Benzodiazepines
advertisement

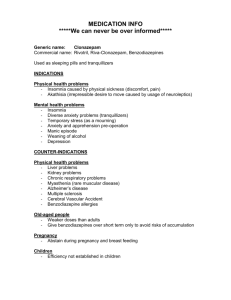
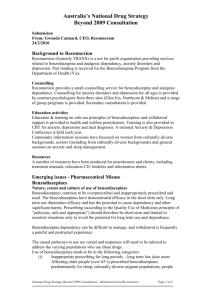
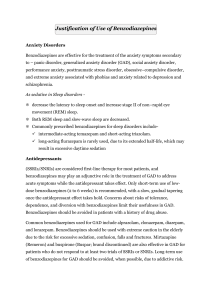
Anxiolytic Works on the CNS by acting selectively on gamma-aminobutyric acid-A (GABA-A) receptors in the brain by making the neuron negatively charged and resistant to excitation They are used as sedatives, hypnotics, anxiolytics, anticonvulsants, and muscle relaxants Examples: Xanax, Ativan, Klonopin, Valium, Versed Introduced around 1960 with the marketing of chlordiazepoxide (Librium) and followed by its derivative diazepam (Valium) Replaced older more unsafe sedatives like barbiturates It is a chemical compound made in laboratories of pharmaceutical companies Acute toxicity of benzodiazepines are extremely low, even in large doses Acute toxicity symptoms: confusion, dizziness, poor judgment and decision making, lack of coordination, slurred speech, difficulty breathing, weakness, Chronic toxicity will change a person’s appearance and behavior which affects their relationships and work performance Chronic abuse symptoms: anxiety, insomnia, anorexia, tremors, headaches, weakness, and memory problems Symptoms of overdose – dizziness, confusion, drowsiness, blurred vision, unresponsiveness, anxiety, and agitation Physical exam findings for overdose nystagmus, hallucinations, slurred speech, ataxia, hypotonia, weakness, altered mental status, amnesia, respiratory depression, paradoxical agitation, hypotension, coma Antidote is flumazenil (Romazicon) – specific for benzodiazepine poisoning and acute overdose; controversial because the risk usually out weight the possible benefits The best treatment for benzodiazepine overdose is good supportive care and monitoring of patient Very rarely fatal for benzodiazepine overdose but biggest concern is aspiration with altered mental status May begin 12-24 hours after the last dose received, reaches peak intensity between 24 and 72 hours Signs and symptoms: Autonomic hyperactivity (sweating, HR >100), hand tremors, N/V, illusions, hallucinations, anxiety, grand mal seizures, fear, rapid mood changes, insomnia, hand tremors, and constipation Hospitalization is usually not required unless rare, but severe symptoms such as seizures occur Medications are usually not used for the withdrawal from benzodiazepines. Slowly lowering the doses of the substance is best to decrease the amount and severity of symptoms. References: Benzodiazepines. (2015). Retrieved from http://www.drugs.com/drugclass/benzodiazepines.html. Benzo Withdrawal: The Ultimate Guide to Symptom Relief. (2015). Retrieved from https://www.discoveryplace.info/benzo-withdrawal-ultimate-guidesymptom-relief?gclid=CIvEotWH1MgCFQUGaQodLIkD5Q Dryden-Edwards, Roxanne. Benzodiazepine Abuse. (2014, December 12). Retrieved from http://www.emedicinehealth.com/benzodiazepine_abuse/article_em. htm. Townsend, M. C. (2015). Psychiatric mental health nursing: Concepts of care in evidence-based practice (8th ed.). Philadelphia, PA: F. A. Davis. Withdrawal syndrome: Benzodiazepines. Reconnection- Treating Panic, Anxiety, Depression, and Tranquilizer dependency. (2013). Retrieved from http://www.reconnextion.org.au/withdrawalsyndrome/w1/i023219/.