Trauma Nursing - Faculty Sites - Metropolitan Community College
advertisement

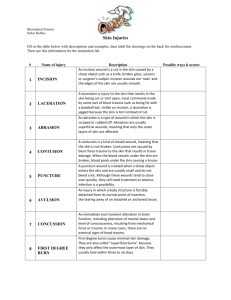
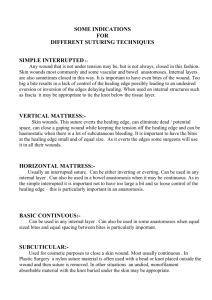
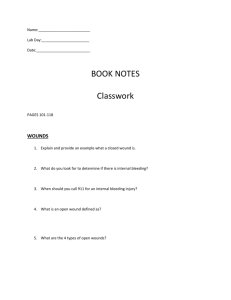
TRAUMA NURSING By: Diana Blum RN MSN Metropolitan Community College PRIORITY EMERGENCY MEASURES FOR ALL PATIENTS Make safety the first priority Preplan to ensure security and a safe environment Closely observe patient and family members in the event that they respond to stress with physical violence Assess the patient and family for psychological function Patient and family-focused interventions Relieve anxiety and provide a sense of security Allow family to stay with patient, if possible, to alleviate anxiety Provide explanations and information Provide additional interventions depending upon the stage of crisis COMMON TRAUMA Heat Bites Cold Electrical Altitude Near drowning Spinal Head Musculoskeletal Stab/gunshot wounds rape HYPERTHERMIA Acute Medical Emergency Failure of heat regulating mechanisms Elderly and young at risk Exceptional heat exhaustion Stems from heavy perspiration Need to stay hydrated! Causes thermal injury at cellular level TREATMENT Lower temp as quickly as possible(102 and lower) How can this be done? Mortality =duration of hyperthermia ABC’s Give 02, Start large bore IV Insert foley Labs: Lytes, CBC, myoglobin. Cardiac enzymes ASSESSMENT status…Seizure may occur Monitor vitals frequently Renal status Mental Monitor temp continuously EKG, Neuro status Hypermetabolism due to increased body temp Increases 02 demand Hyperthermia may recur in 3 to 4 hours; avoid hypothermia HEAT Exhaustion Stroke HEAT EXHAUSTION Caused by dehydration Stems from heavy perspiration Poor electrolyte consumption Signs/Symptoms Normal mental status Flu like Headache Weakness N/V Orthostatic hypotension Tachycardia HEAT EXHAUSTION Treatment Outside hospital Stop activity Move to cool place Cold packs Remove constrictive clothing Re-hydrate (water, sports drinks) If remains call 911 In hospital IV 0.9% saline Frequent vitals Draw serum electrolyte level HEAT STROKE Leads to organ failure and death Mortality rate up to 80% 2 types: Exertional Sudden onset Too heavy clothes Classic Occurs over period of time Chronic exposure to heat Example (no air conditioning) HEAT STROKE Assessment Monitor mental status Monitor vitals Monitor renal status Treatment At site ensure patent airway Move to cool environment Pour water on scalp and body Fan the client Ice the client Call 911 At hospital O2 Start IV Administer normal saline Use cooling blanket DO NOT give ASA Monitor rectal temp q15 minutes Insert foley to monitor I/Os closely and measure specific gravity of urine Check CBC, Cardiac enzymes, serum electrolytes, liver enzymes ASAP Assess ABGs Monitor vitals q 15 minutes Administer muscle relaxants if the client shivers Slow interventions when core temp is 102 degrees or less MANAGEMENT OF PATIENTS WITH HEAT STROKE Remember ABCs (decrease temp to 39° C as quickly as possible Cooling methods Cooling blankets, cool sheets, towels, or sponging with cool water Apply ice to neck, groin, chest, and axillae Iced lavage of the stomach or colon Immersion in cold water bath Monitor temp, VS, ECG, CVP, LOC, urine output Use IVs to replace fluid losses – Hyperthermia may recur in 3 to 4 hours; avoid hypothermia PATIENT TEACHING Ensure adequate fluid and foods intake Prevent overexposure to sun Use sunscreen with at least SPF 30 Rest frequently when in hot environment Gradually expose self to heat Wear light weight, light colored, loose clothing Pay attention to personal limitations: modify accordingly HYPOTHERMIA COLD Most common Hypothermia Frostbite Synthetic clothing is best because it wicks away moisture and dries fast “cotton kills” it holds moisture and promotes frostbite A hat is essential to prevent heat loss though head Keep water, extra clothing, and food in car in case of break down HYPOTHERMIA Internal core temperate is 35° C or less Elderly, infants, persons with concurrent illness, the homeless, and trauma victims are at risk Alcohol ingestion increases susceptibility Hypothermia may be seen with frostbite; treatment of hypothermia takes precedence Physiologic changes in all organ systems Monitor continuously ASSESSMENT Apathy, drowsiness, pulmonary edema, coagulopathies Weak HR and BP Hypoxemia Continuous temperature and EKG Watch for dysrhythmias REWARMING Warm fluids, blankets Cardiopulmonary bypass Warm lavage FROST BITE Inadequate insulation is the culprit 3 stages Superficial (frost nip) Mild Severe Frostnip produces mild pain, numbness,pallor of affected skin Graded like burns-partial thick or full thick 1st degree- hyperemia, edema 2nd degree- fluid blisters with partial thick necrosis 3rd degree- dark fluid blisters, sub cutaneous necrosis 4th degree- no blisters, no edema, necrosis to muscle and bone SNAKE BITES SNAKE BITES Most species non venomous and harmless Poisonous snakes found in each state except Maine, Alaska, and Hawaii Fatalities are few Children 1-9 yrs old victims during daylight hours AWARENESS is KEY Most bites between April and October Peak in July and August 2 main types in North America are pit vipers (look for warm blooded prey) Water moccasins, copperheads, rattlesnakes Most of bites Coral snakes From North Carolina to Florida and in the Gulf states, Arizona, and Texas SNAKE BITES Pit Vipers Depression between eye and nostril Triangular head indicative of venom Venom function is to immbolize, kill and aid in digestion of prey (systemic effects happen with in 8 hours of puncture) impairs blood clotting Breaks down tissue protein Alters membrane integrity Necrosis of tissues Swelling Hypovolemic shock Pulmonary edema, renal failure DIC 2 retractable curved fangs with canals Rattlers have horny rings in tail that vibrates as a warning SNAKE BITES Treatment At site Move person to safe area Encourage rest to decrease venom circulation Remove jewelry and restrictive clothing Splint limb below level of heart Be calm and reassuring No alcohol or caffeine 2nd to speed of venom absorption At hospital Constrict extremity but not to tight Do NOT incise or suck wound Do NOT apply ice Use Sawyer extractor if available if used within 3 minutes of bite and leave for 30 minutes in place At hospital continued O2 2 large bore IV sites Crystalloid fluids (NS or LR) Continuous tele and bp monitoring Opiod pain management Tetanus shot Broad spectrum antibx Lab draw (coagulation studies, CBC, creatinine kinase, T and C, UA) ECG Obtain history of wound and pre-hospital tx measure circumference of bite every 15-30 minutes Possibly give antivenom if ordered (see page 177) Monitor for anaphylaxis Notify poison control SNAKE BITES Coral Snakes Corals burrow in the ground Bands of black, red, yellow “red on yellow can kill a fellow” “red on black venom lack” Are generally non aggressive Ability to inject venom is less efficient Maxillary fangs are small and fixed Use chewing motion to inject Venom is neurotoxic and myotoxic Enough in adult coral to kill human SNAKE BITES Action of venom Blocks binding of acetylcholine at post synaptic junction S/S pain mild and transient Fang marks may be hard to see Effects may be delayed 12 hours but then act rapidly after N/V Headache Pallor, abd pain Late stage: parathesias, numbness, mental status change, crainal and peripheral nerve deficit , flaccid, difficulty speaking, swallowing, breathing elevated creatinine kinase SNAKE BITES Coral Treatment At site Try to ID snake Same as pit viper without concern of necrosis At Hospital Continuous tele Continuous bp and pulse ox Provide airway management (possible ET tube) Provide antivenom treatment as ordered Monitor for anaphylaxis from antivenom Notify poison control http://www.expotv.com/videos/reviews/19/169/Coghlan27sSnakeBiteKit/ 156505 PATIENT TEACHING Avoid venomous snakes as pets Be cautious in areas that harbour snakes like tall grass, rock piles, ledges, crevices, caaves, swamps Don protective attire like boots, heavy pants and leather gloves. Use a walking stick Inspect areas before placing hands or feet in them Do not harass snakes….striking distance is the length of the snake Snakes can bite even 20—60 minutes after death due to bite reflex Use caution when transporting snake with victim to hospital…make sure it is in a sealed container. ARTHROPOD BITES AND STINGS Spiders: carnivorous Almost all are venomous Most not harmful to humans Brown recluse, black widow, and tarantula are dangerous for example Scorpions: England Sting with tail Bark scorpion is most dangerous Bees not in Midwest or New and Wasps Wide range of reactions African or killer bees are very aggressive found in southwest states http://www.videojug.com/film/how-to-treat-an-insect-bite BROWN RECLUSE SPIDER Bites result in ulcerative lesions Cytotoxic effect to tissue Medium in size Light brown color with dark brown fiddle shaped mark from eyes Shy in nature..hide in boxes, closets, basements, sheds, garages, luggage, shoes, clothing, bedsheets, clothes Over 1-3 days lesion becomes dark and necrotic…eschar even forms, and sloughs Surgery is often needed Skin grafting Rare: Malaise, Joint pain, Petechaie, N/V Fever, Chills Pruritis Erythema Extreme: hemolytic, renal failure, death Treatment At site Cold compress initially and intermittently over 4 days (may limit necrosis) Rest Elevation of extremity NEVER use heat At hospital Topical antiseptic Sterile dressing changes Antibx Dapsone: polymorphonuclear leukocyte inhibitor: 50mg twice/day Monitor lab work closely Surgery consult Debridment and skin grafting BLACK WIDOW Found in every state but Alaska Prefers cool, damp, environment Black in color with red hourglass pattern on abd Male are smaller and lighter color that females Carry neurotoxic venom Bites to humans are defensive in nature Main prey other bugs, snakes, and lizards Bite is can be painful, local reactions Systemic reactions can happen in 1 hour and involve the neuromuscular system Causes lactrodectism Venom causes neurotransmitters to release from nerve terminals s/s Abd pain Peritonitis like symptoms N/V Hypertension Muscle rigidity Muscle spasms Facial edema Pytosis Diaphoresis Weakness Increased salavation Priapism Respiratory difficulty Faciculations parathesias At site Apply an ice pack Monitor for systemic involvement ABCs At hospital Monitor vitals Pain meds Muscle relaxants Tentanus Monitor for seizures Antihypertensives Anti venom if needed Call poison control TARANTULAS Largest spider Found mostly in tropical and subtropical parts of USA Some are in dry arid states like New Mexico and Arizona Can live 25 years Venom paralyzes prey and causes muscle necrosis Most human bites have local effects Have urticating hairs in dorsal abd area that can be launched for a defensive technique landing in skin and causing an inflammatory response USA trantulas don’t produce systemic reactions Worldly ones do S/S Pain at site Swelling Redness Numbness Lymphangitis Intense pruritis Severe ophthalmic reactions if hairs come in contact with eyes Treatment Pain meds Immobolize extremity Elevate site Remove hairs with sticky tape followed by irrigation For eyes: irrigation with saline Antihistamines and steroids for pruritis SCORPIONS Found in many states Not usual in midwest or new england unless pet, or transported in baggage Venom in stinger located on the tail s/s Localized pain Inflammation Mild symptoms Treatment: pain meds, wound care, supportive management BARK SCORPION Deadly Has a fatal sting Found in tress, wood piles, and around debris Humans stung when it gets in clothing, shoes, blankets, and items left on ground Solid yellow, brown, or tan in color Have thin pinchers, thin tail, and a tubercle Found in Arizona, New Mexico, Texas, Nevada, and California Has neurotoxic venom s/s Involve cranial nerves May be symptom free Pain Respiratory failure Pancreatitis Musculoskeletal dysfunction Gentle tap at possible sting site while client not looking greatly increases pain, and is confirmation of bite Symptoms begin immediately and reach maximum intensity in 5 hours Most symptoms resolve in 9- 30 hours Pain and parathesia can last 2 weeks Treatment Monitor vitals May need intubation Supply O2 IV Fluids Ice pack to sting site Pain meds and sedatives with caution in non intubated client Wound care Call poison control Atropine gtts to help with hypersalavation Antivenom if needed BEES/WASPS Stings cause wide array of reactions S/S Anaphylaxis most severe Respiratory failure Hypotension Decrease in LOC Dysrhythmias Cardiac arrest Pain Local reaction Swelling N/V Diarrhea Pruritis Urticaria Lip swelling TREATMENT At site Remove stinger Ice pack Epipen if allergy to bees Call 911 if needed In hospital ABCs Check history for allergy Epinephrine Antihistamine O2 NS 0.9% corticosteroids PATIENT EDUCATION Wear protective clothing when working in areas with known venomous athropods (bees, scorpions, wasps) Cover garbage cans Use screens in windows and doors Inspect clothing and, shoes and gear before putting on Shake out clothing and gear that is on ground Exterminate the exterior house Do not place hands where eyes can not see Do not keep insects as pets Epi pen if allergy to bee/wasp POISONING OVERDOSE POISONING According to your book, Poison is any substance that when ingested, inhaled, absorbed, applied to the skin, or produced within the body in relativity small amounts injures the body by its chemical action Treatment goals: Remove or inactivate the poison before it is absorbed Provide supportive care in maintaining vital organ systems Administer specific antidotes Implement treatment to hasten the elimination of the poison ASSESSMENT OF PATIENTS WITH INGESTED POISONS Remember ABCs Monitor VS, LOC, ECG, and UO Assess lab values Determine what, when, and how much substance was ingested Assess signs and symptoms of poisoning and tissue damage Assess health history Determine age and weight INTERVENTIONS FOR THOSE WITH INGESTED POISONS remove the toxin or decrease its absorption Use emetics Gastric lavage Activated charcoal Cathartic when appropriate Administration of specific antagonist as early as possible Other measures may include diuresis, dialysis, or hemoperfusion Corrosive agents such as acids and alkalis cause destruction of tissues by contact DO NOT induce vomiting with corrosive agents MANAGEMENT OF CARBON MONOXIDE POISONING Inhaled carbon monoxide binds to hemoglobin as carboxyhemoglobin, which does not transport oxygen Manifestations: CNS symptoms predominate Skin color is not a reliable sign pulse oximetry is not valid Treatment Get to fresh air immediately Perform CPR as necessary Administer oxygen: 100% or oxygen under hyperbaric pressure Monitor patient continuously Draw blood levels May need HBO MANAGEMENT OF FOOD POISONING A sudden illness due to the ingestion of contaminated food or drink Food poisoning has the ability to result in respiratory paralysis and death depending on the cause ABCs and supportive measures are key Treatment correct fluid and electrolyte imbalances Control nausea and vomiting Provide clear liquid diet and progression of diet after nausea and vomiting subside PATIENTS WITH SUBSTANCE ABUSE Acute alcohol intoxication Alcohol poisoning may result in death Maintain airway Observe for CNS depression and hypotension Rule out other potential causes of the behaviors before it is assumed the patient is intoxicated Use a nonjudgmental, calm manner Patient may need sedation if noisy or belligerent Examine for withdrawal delirium, injuries, and evidence of other disorders Commonly abused substances: ??? see Table 71-1 LIGHTNING LIGHTNING Year round problem Most common in summer Caused by electrical charge in cloud Large energy with small duration High voltage is 1000 volts Lighting is 1 million volts Cloud to ground is most dangerous Flash over phenomenon: force powerful enough to blow off or damage the victims clothing Injury is by: Direct strike Spashing or side flash off of near by structure Through the ground LIGHTNING Best remedy: AVOIDANCE Education Observe forecasts Seek shelter when your hear thunder DO NOT stand under tree DO NOT stand in an open area Isolated sheds and caves are dangerous Leave water immediately Avoid metal objects If camping stay away from metal tent poles and wet walls Stay away from open doors, windows, fireplaces Turn off electrical equipment Stay off of telephone Move to valley area and huddle in ball if in open area (this minimizes target area) LIGHTNING Most lethal effect is asystole or Vfib Most victims suffer cardiac injury S/S Mottled skin Cardiac arrest Respiratory arrest Decreased or absent peripheral pulses Temporary paralysis Loss of Consciousness Amnesia, confusion, disorientation Photophobia Seizures Fatigue and PTSD Ruptured tympanic membranes Blindness, cataracts, retinal detachment Skin burns Ferning marks: branching on the skin INTERVENTIONS At site Spinal immobilization Monitor ABCs CPR Sterile dressings for burns Hospital care ACLS Telemetry ABC support Ventilator prn Creatinine kinase level to determine muscle damage Monitor for kidney failure Monitor for rhabdomyolosis (muscle destruction) Burn precautions Tetanus Xfer to burn center ALTITUDE RELATED ILLNESS High altitude is elevations above 5000 feet most ski resorts As altitude increasesbarametric pressure decrease This means less o2 the higher you go Oxygen is 21% of the barametric pressure Acclimatizationthe process of adapting to high altitudes Increased RR Decrease in CO2 Respiratory alkalosis Impaired REM Excess bicarb excretion through the kidneys Cerebral blood flow increases 3 most common altitude illnesses Acute Mountain Sickness (AMS) Precursor for HACE/HAPE Throbbing headache, anorexia, N/V Chilled, irritable Similar symptoms to alcohol hangover VS variable DOE or at rest High altitude cerebral edema (HACE) Unable to perform ADLs Ataxia w/o focal signs (decreased motor coordination) Confusion, impaired judgment , seizures Stupor, Coma, Death from brain swelling Increased ICP over 1-3 days High altitude pulmonary edema (HAPE) Most frequent cause of death Poor exercise intolerance and recovery Fatigue and weakness Tachycardia and tachypnea, rales, pneumonia Increased pulmonary artery pressure ALTITUDE ILLNESS Site Descent to lower altitude Monitor for symptom progression Rest O2 if available Hospital Acetazolamide Acts as bicarb diuretic Sulfa drug Take 24 hours before ascent and take for 1st 2 days of the trip 125mg-250mg po BID or 500mg SR cap daily Dexamethazone: 4mg – 8mg po or IM initially then 4mg q6hours during descent O2 Monitor airway Lasix Critical care ALTITUDE EDUCATION Plan a slow descent Avoid overexertion and over exposure to cold Avoid alcohol and sleeping pills Stay hydrated and have adequate nutrition If symptoms develop descend immediately O2 if able Wear protective gear Wear sunscreen DROWNING NEAR DROWNING Rip currents are powerful currents of water moving away from shore. More people die every year from rip currents than from shark attacks, tornadoes, lightning or hurricanes. According to the United States Lifesaving Association, 80 percent of surf beach rescues are attributed to rip currents, and more than 100 people die annually from drowning when they are unable to escape a rip current. Rip currents can attain speeds as high as 8 feet per second Some rip currents last for a few hours; others are permanent. Rip currents range from 50 to 100 feet or more in width. They can extend up to 1000 feet offshore. If caught in a rip current: •Remain calm to conserve energy and think clearly. •Never fight against the current. •Think of it like a treadmill that cannot be turned off, which you need to step to the side of. •Swim out of the current in a direction following the shoreline. When out of the current, swim at an angle--away from the current--towards shore. •If you are unable to swim out of the rip current, float or calmly tread water. When out of the current, swim towards shore. •If you are still unable to reach shore, draw attention to yourself by waving your arm and yelling for help. 6,000 to 8,000 people drown in the U.S. each year. Most drownings occur within a short distance of safety. Immediate action and first aid can prevent death. A person who is drowning usually can NOT shout for help. Be alert for signs of drowning. Suspect an accident if you see someone in the water fully clothed. Watch for uneven swimming motions, which indicate a swimmer is getting tired. Often the body sinks, and only the head shows above the water. Children can drown in only a few inches of water. It may be possible to revive a drowning victim even after a prolonged period of submersion, especially if the person was in very cold water. Causes Leaving small children unattended around bathtubs and pools Drinking alcohol while boating or swimming Inability to swim or panic while swimming Falling through thin ice Blows to the head or seizures while in the water Attempted suicide Symptoms Symptoms can vary, but may include: Abdominal distention Bluish skin of the face, especially around the lips Cold skin and pale appearance Confusion Cough with pink, frothy sputum Irritability Lethargy No breathing Restlessness Shallow or gasping respirations Chest pain Unconsciousness Vomiting First Aid When someone is drowning: Extend a long pole or branch to the person, or use a throw rope attached to a buoyant object, such as a life ring or life jacket. Toss it to the person, then pull him or her to shore. People who have fallen through ice may not be able to grasp objects within their reach or hold on while being pulled to safety. Do not place yourself in danger. Do NOT get into the water or go out onto ice unless your are absolutely sure it is safe. If you are trained in rescuing people, do so immediately if you are absolutely sure it will not cause you harm. If the victim's breathing has stopped, begin rescue breaths as soon as you can. This often means starting the breathing process while still in the water. Continue to breathe for the person every few seconds while moving them to dry land. Once on land, give CPR if needed. Always use caution when moving a drowning victim. Assume that the person may have a neck or spine injury, and avoid turning or bending the neck. Keep the head and neck very still during CPR and while moving the person. You can tape the head to a backboard or stretcher, or secure the neck by placing rolled towels or other objects around it. Follow these additional steps: Keep the person calm and still. Seek medical help immediately. Remove any cold, wet clothes from the person and cover with something warm to prevent hypothermia. Give first aid for any other serious injuries. The person may cough and have difficulty breathing once breathing re-starts. Keep Reassuring the person without providing false hope. DO NOT DO NOT go out on the ice to rescue a drowning person that you can reach with your arm or an extended object. DO NOT attempt a swimming rescue yourself unless you are trained in water rescue. DO NOT go into rough or turbulent water that may endanger you. Do not perform the Heimlich maneuver unless repeated attempts to position the airway to use rescue breathes failed and you suspect the person’s airway is blocked. It increases the chances that an unconscious victim will vomit and subsequently choke When to Contact a Medical Professional If you cannot rescue the drowning person without endangering yourself, call for emergency medical assistance immediately. If you are trained and able to rescue the person, do so and then call for medical help. All possible drownings should be checked by a doctor. Prevention Avoid drinking alcohol whenever swimming or boating. Observe water safety rules. Take a water safety course. Never allow children to swim alone or unsupervised regardless of their ability to swim. Never leave children alone for any period of time, or let them leave your line of sight around any pool or body of water. Drowning can occur in any container of water. Do not leave any standing water (in empty basins, buckets, ice chests, kiddy pools, or bathtubs). Secure the toilet seat cover with a child safety device. Fence all pools and spas. Secure all the doors to the outside, and install pool and door alarms. If your child is missing, check the pool immediately. MULTISYSTEM TRAUMA SPINAL CORD INJURIES (SCI) tetraplegia (quadriplegia): paralysis from neck down Loss of bowel and bladder control Loss of motor function Loss of reflex activity Loss of sensation Coping issues *Christopher Reeve is example of this injury* Complete: spinal cord severed and no nerve impulses below level of injury Incomplete: allow some function and movement below level of injury CAUSES OF SCI Primary Hyperflexion (moved forward excessively) Hyperextension (MVA) Axial loading (blow at top of head causes shattering) Excessive rotation (turning beyond normal range) Penetrating (knife, bullet) Secondary Neurogenic shock Vascular insult Hemorrhage Ischemia Electrolyte imbalance CERVICAL INJURIES Anterior cord syndrome Damage to anterior portion of gray and white matter as a result of decreased blood supply..pt will have a loss of motor function, pain, and temperature sensation but touch, vibration, and position remain intact Posterior cord lesion Damage to posterior white and gray matter..pt has intact motor function but loss of vibratory sense, crude touch, and position sensation Brown Sequard syndrome Result of penetrating injury that causes hemisection of spinal cord. Motor function , proprioseption, vibration, and deep touch are lost on the same side as injury (ipsilateral) On the other side (contralateral) the sensation of pain, temperature and light touch are affected Central cord syndrome Loss of motor function in upper extremities and varying degrees of sensation remain ASSESSMENT OF SCI 1st assess respiratory status ET tube may be necessary if compromised 2nd assess for intra-abdominal hemorrhage (hypotension, tachycardia, weak and thready pulse) 3rd assess motor function C4-5 apply downward pressure while the client shrugs C5-6 apply resistance while client pulls up arms C7 apply resistance while pt straightens flexed arms C8 check hand grasp L2-4 apply resistance while the client lifts legs from bed L5 apply resistance while client dorsiflexes feet S1 apply resistance while client plantar flexes feet EMERGENCY CARE OF SCI Observe for signs of autonomic dysreflexia Sever HTN, bradycardia, sever headache, nasal stuffiness, and flushing Caused by noxious stimuli like distended bladder or constipation Immediate interventions Place in sitting position Call doctor Loosen tight clothes Check foley tubing if present Check for impaction Check room temp Monitor BP q10-15 minutes Give nitrates or hydralazine per md order NRSG DX Ineffective tissue perfusion r/t interruption of arterial flow Ineffective airway clearance r/t SCI Ineffective breathing pattern r/t SCI Impaired gas exchange r/t SCI TREATMENT OF SCI Immobilize fx Proper body alignment Traction is possible Monitor vs q4 hours or more Neuro checks q4 hours or more Monitor for neurogenic shock (hypotension and bradycardia) Prepare for possible surgery Teach skin care, ADLs, wound prevention techniques, bowel and bladder training, medications, and sexuality BRAIN INJURIES (TBI) Open- skull fx or when skull is pierced by penetrating object Linear fx- simple clean break Depressed fx- bone pressed in towards tissue Open fx-lacerated scalp that creates opening to brain tissue Comminuted fx- bone fragments and depresses into brain tissue Basilar- unique fx at base of skull with CSF leaking though the ear or nose Closed- blunt trauma Mild concussion-brief LOC Diffuse axonal injury- usually from MVA May go into coma Contusion-bruising of brain Site of impact (coupe) Opposite side of impact (contrecoupe) Laceration-tearing of cortical surface vessels that leads to hemorrhage edema and inflammation Always assume c-spine injury ABC highest priority Control bleeding right away MOTOR VEHICLE COLLISIONS Frontal Front of car stops and driver keeps going Injuries: Seatbelt, Steering wheel, TBI, cspine, flail chest, myocardial contusion Side Rear Injuries: Cspine, flail chest, pneumothorax Hyperextension, cspine Rollover Multiple injuries FIGURE 74.2 UNRESTRAINED FRONTAL IMPACT. OTHER TYPES OF MULTIPLE INJURIES Motorcyle Pedestrian Tib/fib, chest, abd, TBI, cspine, femur Femur, chest, lower extremities Falls Calcaneous, compression, wrist, TBI Battles sign Raccoon eyes Flail chest Tension Pneumothorax Hemothorax BLUNT TRAUMA BY FORCE Acceleration-caused by external force contacting head Deceleration- when head suddenly stops or hits a stationary object INCREASED ICP Normal ICP is 10-15mmHg Normal increases occur with coughing, sneezing, defecation Leading cause of death for head trauma As ICP increases cerebral perfusion decreases causing tissue hypoxia, decrease serum pH, and increase in CO2 ICP CONTINUED 3 types of edema Vasogenic: increase in brain tissue volume Cytotoxic: result of hypoxia Interstitial: occurs with brain swelling HEMATOMA Epidural- bleed b/w dura and inner table Subdural-bleed below dura and above arachoid Intracerebral-accumulation of blood in brain tissue HYDROCEPHALUS abnormal increase in CSF volume Causes: impaired reabsorption from subarachnoid hemorrhage or meningitis may be congenital or acquired Acquired hydrocephalus= develops at the time of birth or at some point afterward. It can affect individuals of all ages and may be caused by injury or disease. Symptoms vary with age, disease progression, and individual differences in tolerance to the condition BRAIN HERNIATION Increased ICP will shift and move brain tissue downward Central Herniation Downward shift to brainstem S/S Cheyne stokes , pinpoint pupils, hemodynamic instability The most life threatening is Uncal because it causes pressure on the 3rd cranial nerve S/S Dilated, nonreactive pupils, ptosis, rapidly decreased LOC INTERVENTIONS FOR MUSCULOSKELETAL TRAUMA Fractures Open Closed Spontaneous Stress Compression Greenstick Spiral Oblique Impacted Displaced Non-displaced fragmented STAGES OF HEALING 48-72 hours after injury hematoma forms at break site Area of bone necrosis forms secondary to diminished blood flow Fibroblasts and osteoblasts come to site Fibrocartilage forms =new foundation Callus forms 2-6 weeks after initial break 3 weeks to 6 months later new bone is formed FACTORS THAT AFFECT HEALING Age Severity of trauma Bone injured Inadequate immobilization Infection Avascular necrosis MUSCULOSKELETAL ASSESSMENT Assess for life threatening complications Skin color and temp Movement Sensation Pulses especially distal to the injury Cap refill Pain Listen for crepitation-grating sound Look for ecchymosis Assess for subcutaneous emphysema-bubbles under skin (like bubble wrap when pushed) Assess clients feeling of situation Some fractures can causes internal injuryhemorrhage DIAGNOSTICS No special lab tests except maybe D-Dimer for clots H/H could be low due to bleeding CT Bone scan MRI X-rays Affected extremity NURSING DIAGNOSIS Acute pain Risk for infection Impaired physical mobility Etc. INTERVENTIONS Inspect fx site Palpate area lightly Assess motor function Immobilize extremity Realignment Cast Traction Surgery open reduction with internal fixation EDUCATION Provide education regarding medication Instruct the client on s/s of infection (foul discharge, purulent drainage, fever, lethargy, etc) Instruct on dressing changes and importance of them Instruct about pressure ulcer prevention Instruct on use of crutches or walker if needed Instruct about HHC and other available resources Fx of clavicle usually from a fall Fx of scapula not common and caused by direct impact Fx of humerus common in older adult Fx of olecrenon usually from fall directly onto elbow Fx of radius and ulna usually Fx together Fx of wrist and hand most common site is the carpal scaphoid bone in young adult men..one of the most misdiagnosed Fx b/c of poor visibility on x-ray Fx of hip caused by falls Fx of femur caused from trauma Fx of patella result from direct impact Fx of tibia and fibula usually break together Fx of ankle and foot difficult to heal because of instability of ankle bone Fx of ribs and sternum caused by chest trauma and potentially can puncture lungs, heart and arteries Fx of pelvis can also cause major internal damage because of the vascular structure present Compression Fx of the spine usually caused by osteoporosis. This causes pain, deformity, neurologic compromise FEMUR AND PELVIC FRACTURES High incidence of hemmorage Femur fx-cast, brace, splint, traction Fat embolism: fat from bone released into blood and into heart, lungs, etc Pelvic- girdle, assess for stability Large amount of force Rectal exam FIGURE 56.10 VASCULAR ANATOMY OF THE PELVIS. DISLOCATIONS Painful Needs to be reduced ASAP Can cause nerve damage Avascular Necrosis Dislocation occludes blood supply OTHER SURGERIES Vertebroplasty Kyphoplasty Both are minimally invasive Both use a bone cement to provide immediate relief of pain COMPLICATIONS Acute compartment syndrome: increase pressure compromises circulation to are. Most common in lower leg and forearm. Fat embolism: fat from bone released into blood and into heart, lungs, etc. Most common with long bone fx DVT PE INFECTION: from break or from implanted hardware..bone infection most common with open fx Fracture blisters: associated with twisting injury..fluid moves into vacant spaces..leads to infection Ischemic necrosis: blood flow to bone is disrupted Delayed union: unhealed after 6 months Nonunion:never completely heal Malunion: heal incorrectly CRUSH SYNDROME CAUSES Wringer type injuries Natural disasters Work related injuries Drug or alcohol overdose CHARACTERISTICS Acute compartment syndrome Hyperkalemia Rhabdomyolosis – myoglobin released into blood S/S Hypovolemia, hyperkalemia, compartment syndrome TX IVF, diuretics, low dose dopamine, sodium bicarb, kayexelate, hemodialysis is possible. COMPLEX REGIONAL PAIN SYNDROME s/s: debilitating pain, atrophy, autonomic dysfunction (excessive sweating, vascular changes), and motor impairment (muscle paresis) Caused by hyperactive sympathetic nervous system Results from trauma Common in feet and hands 3 stages: 1: lasts 1-3 months; local severe burning pain, edema, vasospasm, muscle spasms 2: 3-6 months; pain, edema, muscle atrophy, spotty osteoporosis 3: marked muscle atrophy, intractable pain, severely limited mobility, contractures, osteoporosis TX Pain control PT OT ROM Gentle skin care Support groups, etc SPORTS RELATED INJURIES Tears Lock knee Torn ACL Tendon rupture Dislocation Subluxation Strains Sprains Torn rotator cuff INTERVENTIONS FOR MUSCULOSKELETAL TRAUMA Casts Braces Splints Traction Surgery Reduction (realignment) AMPUTATIONS Removal of part of the body Types Surgical-example digit Traumatic- example digit Levels Lower extremity: digits, bka, aka, midfoot Upper extremity: hands, fingers, arms Complications Hemorrhage Infection Phantom limb pain: perceive pain in the amputated limb Immobility Neuroma: sensitive tumor consisting of nerve cells found at several nerve endings Contractures ASSESSMENTS Skin color Temp Sensation Pulses Cap refill Assess feelings r/t amputation Young: bitter, hostile, uncooperative, loss of job, loss of hobbies, altered self concept, feeling a loss of independence Assess families perceptions also Routine preop xrays done BP done in all extremities Angiography to look at layout of vessels STAB WOUNDS 4 types of wounds Incised = Sharp cut like injuries (knives, glass) Slash wounds= more longer than deep Stab wound= depth longer than length Defense wound= warding wounds (like on hand) Defense Wound Stab Wound w/ single edge blade GUN SHOT WOUNDS 4 types Close contact= illustrates a patternized abrasion around the wound Contact= barrel has contacted the skin and the gases have passed into SQ tissues faint abrasion ring and sone grey/black discoloration Intermediate wound= powder tatooing Exit wound= slit like exit wound…no powder or soot Wound Care Treatment (at Site) Bleeding can usually be stopped by applying direct pressure to the wound. Very large foreign objects stuck in a wound should be stabilized. Do not remove them. All wounds require immediate thorough cleansing with fresh tap water. Gently scrub the wound with soap and water to remove foreign material. If a syringe is available, it should be used to provide high-pressure irrigation. Remove dead tissue from the wound with a sterile scissors or scalpel. After cleaning the wound, a topical antibiotic ointment (bacitracin) should be applied 3 times per day. Wounded extremities should be immobilized and elevated. Puncture wounds are usually not sutured (stitched) unless they involve the face. If the wound is clean, the edges can be drawn together with tape. (Do not cover wounds inflicted by animals or that occurred in seawater with tape.) Oral antibiotics are usually recommended to prevent infection. If infection develops, continue antibiotics for at least 5 days after all signs of infection have cleared. Inform the doctor of any drug allergy prior to starting any antibiotic Some may cause sensitivity to the sun, so sunscreen (at least SPF 15) is mandatory while taking these antibiotics. Pain may be relieved with Tylenol or ibuprofen IN HOSPITAL TREATMENT •Stay Safe. If you are not the victim, practice Universal precautions and wear PPE. •Try to control bleeding before anything else. •Putting pressure directly on the puncture wound while holding it above the level of the heart for 15 minutes should be enough to stop bleeding. •Avoid Tourniquets unless medical care will be delayed for several hours. •Call 911 if any Deep puncture wounds (or those of unknown depth) to the abdomen, back, pelvis, thigh, chest, or if bleeding will not stop •Holes in the chest can collapse the lungs • Deep puncture wounds to the chest should be immediately sealed by hand or with a dressing that does not allow air to flow ( 3 sided). • IF complaints of SOB occur or victim gets worse after sealing the chest puncture wound then unseal it. •Once bleeding has been controlled, wash the puncture wound with warm water and mild soap SEXUAL ABUSE SEXUAL ABUSE Sexual abuse (also referred to as molestation) is defined as the forcing of undesired sexual acts by one person to another. Incest is defined as sexual abuse between family members Different types of sexual abuse involve: Acquaintance rape - forced sexual intercourse between individuals who know each other. Non-consensual, forced physical sexual behavior Psychological forms of abuse, such as verbal, sexual behavior, or stalking The use of a position of trust for sexual purposes. Usually related to drinking http://www.youtube.com/watch?v=PvXxzZUuIn0 SEXUAL ABUSE Signs of sexual abuse Unexplained injuries (especially to parts of the female body that can be covered by a two-piece swimsuit) Torn or stained clothing or underwear Pregnancy Sexually transmitted diseases (STDs) Unexplained behavioral problems Depression Self abuse and/or suicidal behavior Drug and/or alcohol abuse Sudden loss of interest in sexual activity Sudden increase of sexual behavior The doctor in the emergency room will examine the victim for injuries and collect evidence. The attacker may have left behind pieces of evidence such as clothing fibers, hairs, saliva or semen that may help identify him. In most hospitals, a "rape kit" is used to help collect evidence. Samples of evidence may be used in court. blood tests are done to check for pregnancy and diseases that can be passed through sex. Cultures of the cervix may be sent to a lab to check for disease, too. The results will come back in several days or a few weeks. Follow up with PCP is important. If any of the tests are positive, treatment options will be discussed. If a birth control pill or intrauterine device (IUD) the chance of pregnancy is small. If no birth control is taken the victim may consider pregnancy prevention treatment. Pregnancy prevention consists of taking 2 estrogen pills when you first get to the hospital and 2 more pills 12 hours later. This treatment reduces the risk of pregnancy by 60% to 90%. (The treatment may make you feel sick to your stomach.) If not already vaccinated for hepatitis B, the victim should get that vaccination followed by one after 1 month and a third in 6 months. The doctor will also discuss (HIV) infection. you can take 2 medicines– Retrovir and Epivir -- for 4 weeks to aid in prevention RAPE Classified as assault Primary cause is an aggressive desire to dominate according to experts Difficult to prosecute b/c of lack of evidence Statistics Women by men: 90-91% most frequent Male by male: 9-10% less common Little to no research on women offenders Definition Intercourse , is attempted or happens without consent of one of the parties involved (penetration with penis or objects etc) TYPES OF RAPE Gang Multiple offenders, one victim Date Custodial Serial Marital Prison Acquaintance Wartime Statuatory EFFECTS OF RAPE Unpredictable emotions Feeling numb and detached Memory problems Avoidance of things anxiety PTSD can occur Relive the rape over and over Disturbed sleeping patterns Eating habits affected MORE STATS If reported to police 50% chance an arrest will be made If arrest made, 80% chance of prosecution If prosecuted, 58% chance of felony conviction If felony conviction, 69% chance of jail time MANDATORY REPORTING If abuse suspected Child Domestic Any type