Tissue Repair Regeneration
advertisement

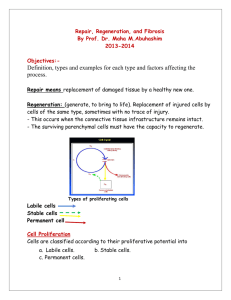
TISSUE REPAIR REGENERATION / HEALING DEFINITIONS: REPAIR: Restoration of normal structure and function of tissues. • For parenchymal and connective tissue. HEALING: For surface epithelium. REPAIR • Repair of damaged tissue occurs by • 1- regeneration by proliferation of uninjured cells and maturation of stem cells. • 2-deposition of connective tissue to form scar. REGENERATION • Replacement of lost structures • Is dependent on the type of normal turnover the original tissue has, skin, intestine. • Mammals have limited ability to regenerate. Scar/ CT deposit • If the tissue damage is severe: Connective tissue(fibrous) is laid down to end in scar formation. • Fibrosis, as one of the 3 possible outcomes of inflammation, follows “healing” • Fibrosis + inflammation= organization. Both regeneration and Fibrosis occur simultaneously. Cell Population Fates • PROLIFERATION – Hormonal, especially steroid hormones – eg., EPO, CSF * • DIFFERENTIATION – UNIDIRECTIONAL, GAIN (specialization) and LOSS (versatility) • APOPTOSIS *One of the most KEY concepts in neoplasia CELL TYPES • Labile/dividing: eg., marrow, GI • Stable/Quiescent: liver, kidney • NON-mitotic/permanant: neuron, striated muscle ADULT STEM CELLS • MARROW (HEMOCYTOBLAST) (hematopoetic stem cells) • NON-MARROW (RESERVE) MARROW STROMAL CELL Growth Factors (GFs) • Polypeptides • Cytokines • LOCOMOTION • CONTRACTILITY • DIFFERENTIATION • ANGIOGENESIS Growth Factors (GFs) • • • • • • • • Epidermal Transforming (alpha, beta) Hepatocyte Vascular Endothelial Platelet Derived Fibroblast Keratinocyte Cytokines (TNF, IL-1, Interferons) CELL PLAYERS (source AND targets) • • • • • • • • Lymphocytes, especially T-cells Macrophages Platelets Endothelial cells Fibroblasts Keratinocytes “Mesenchymal” cells Smooth muscle cells E (Epidermal) GF • • • • Made in platelets, macrophages Present in saliva, milk, urine, plasma Acts on keratinocytes to migrate, divide Acts on fibroblasts to produce “granulation” tissue T (Transforming) GF-alpha • Made in macrophages, T-cells, keratinocytes • Similar to EGF, also effect on hepatocytes H (Hepatocyte) GF • Made in “mesenchymal” cells • Proliferation of epithelium, endothelium, hepatocytes • Effect on cell “motility” VE (Vascular Endothelial) GF • • • • • Made in mesenchymal cells Triggered by HYPOXIA Increases vascular permeability Mitogenic for endothelial cells KEY substance in promoting “granulation” tissue PD (Platelet Derived) GF • Made in platelets, but also MANY other cell types • Chemotactic for MANY cells • Mitogen for fibroblasts • Angiogenesis • Another KEY player in granulation tissue F (Fibroblast) GF • Made in MANY cells • Chemotactic and mitogenic, for fibroblasts and keratinocytes • Re-epithelialization • Angiogenesis, wound contraction • Hematopoesis • Cardiac/Skeletal (striated) muscle T (Transforming) GF-beta • Made in MANY CELLS • Chemotactic for PMNs and MANY other types of cells • Inhibits epithelial cells • Fibrogenic • Anti-Inflammatory K (Keratinocyte) GF • Made in fibroblasts • Stimulates keratinocytes: –Migration –Proliferation –Differentiation I (Insulin-like) GF-1 • Made in macrophages, fibroblasts • Stimulates: – Sulfated proteoglycans – Collagen – Keratinocyte migration – Fibroblast proliferation • Action similar to GH (Pituitary Growth Hormone) TNF (Tumor Necrosis Factor) • Made in macrophages, mast cells, T-cells • Activates macrophages (cachexin) • KEY influence on other cytokines • The MAJOR TNF is TNF-alpha Interleukins • Made in macrophages, mast cells, T-cells, but also MANY other cells • MANY functions: – Chemotaxis – Angiogenesis – REGULATION of other cytokines INTERFERONS • Made by lymphocytes, fibroblasts • Activates MACROPHAGES • Inhibits FIBROBLASTS • REGULATES other cytokines SIGNALING • Autocrine (same cell) • Paracrine (next door neighbor) (many GFs) • Endocrine (far away, delivered by blood, steroid hormones) ExtraCellular Matrix (ECM) • • • • Collagen(s) I-XXVII Elastin Fibrillin CAMs (Cell Adhesion Molecules) – Immunoglobulins, cadherins, integrins, selectins • Proteoglycans • Hyaluronic Acid ECM • • • • Maintain cell differentiation “Scaffolding” Establish microenvironment Storage of GF’s Collagen One - bONE (main component of bone) Collagen Two - car TWOlage (main component of cartilage) Collagen Three - reTHREEculate (main component of reticular fibers) Collagen Four - FLOOR - forms the basement membrane DEFINITIONS: •REGENERATION: Growth of cells to replace lost tissues •HEALING: A reparative tissue response to a wound, inflammation or necrosis Tissue regeneration • Labile tissues contain stem cells that differentiate to replenish lost cells and maintain homeostasis. • Cell proliferation is controlled by cell cycle and is stimulated by growth factors and interaction of cells with ECM. • Regeneration of liver is classic example of regeneration. Prometheus, Zeus. Liver regeneration. • After resection, IL-6 primes hepatocytes to receive new cells. • Growth factors and cytokines push hepatocytes into cell cycle and later divide kupffer cells, endothelial and stellate cells. • In last termination phase, hepatocytes return to quiescent phase. TRANSCRIPTION FACTORS HEPATIC REGENERATION TNF IL6 HGF HEALING/REPAIR • FOLLOWS INFLAMMATION • PROLIFERATION and MIGRATION of connective tissue cells • ANGIOGENESIS (Neovascularization) • Collagen, other ECM protein synthesis • Tissue Remodeling • Wound contraction • Increase in wound strength (scar = fibrosis) ANGIOGENESIS (NEOVASCULARIZATION) • From endothelial precursor cells • From PRE-existing vessels • Stimulated/Regulated by GF’s, especially VEGF • Also regulated by ECM proteins • aka, “GRANULATION”, “GRANULATION TISSUE”, “ORGANIZATION”, “ORGANIZING INFLAMMATION” ANGIOGENESIS GRANULATION TISSUE, TRICHROME STAIN. WOUND HEALING • 1st INTENTION • 2nd INTENTION • Edges lined up • Edges NOT lined up • More granulation • More epithelialization • MORE FIBROSIS TWO TYPES OF WOUND Difference • • • • • • • • FIRST INTENTION Wound contraction Inflammation Scar Healing rapid Function loss Oedema Granulation tissue • • • • • • • • SECOND INTENTION Present More More Slow More More More “HEALTHY” Granulation Tissue FIBROSIS/SCARRING • DEPOSITION OF COLLAGEN by FIBROBLASTS • With time (weeks, months, years?) the collagen becomes more dense and the tissue becomes “STRONGER”. However function and appendages might be lost. COLLAGEN DEPOSITION • TGF-Beta is most important cytokine for CT deposition. • Produced by GT and macrophages • Changes fibroblasts to myofibroblasts. • Remodelling/degradation of collagen is done by MMP. • ADAM (a disintegrin and MP) is also related to MMP. Wound RETARDING factors (LOCAL) • DECREASED Blood supply • Denervation • Local Infection • FB • Hematoma • Mechanical stress(Cough) • Necrotic tissue Wound RETARDING factors (SYSTEMIC) • DECREASED Blood supply • Age(Arteriosclerosis) • Anemia • Malignancy • Malnutrition • Obesity • Infection • Steroids inhibit TGF exception cornea. Abnormalities of repair • Inadequate / less GT or scar: wound dehiscence or rupture (cough/vomiting) • Excessive GT: Protrudes above the surrounding skin and blocks approximation of edges (proud flesh). • Excessive Collagen: Hypertrophic scar/ Keloid. • Excessive contraction: Contractures. THANK YOU