Psychosocial Needs Distress of AYA Oncology Patients
advertisement

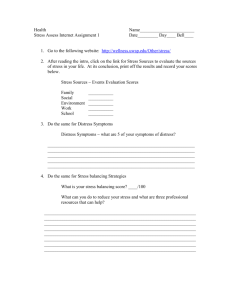
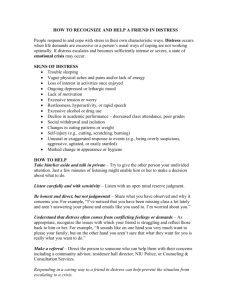
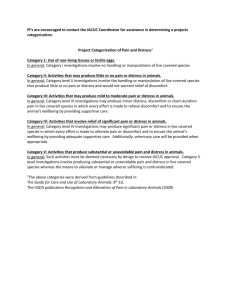
Psychosocial Needs/ Distress of AYA Oncology Patients Andrea Johnson, MSW, RSW PhD Student- UBC Why Adolescents? Significant physical, psychological, emotional, social, vocational growth during AYA years (Abrams, Hazen, & Penson, 2007; Hollis & Morgan, 2001; Woodgate, 2006). Dichotomy of care (Fernandez, C., Fraser, G., Freeman, C., Grunfeld, E., Gupta, A., Mery, L.S.,…Schacter, B., 2011; Bleyer, W.A. & Barr, R.D, 2007). The ‘Lost Tribe’ (Fernandez & Barr, 2006). Can be a complex population to care for Psychosocial Challenges Independence and autonomy Peer relationships/dependence on family Changes in physical appearance Self-Esteem; Identity Sexuality and Fertility Future-planning Fears and difficult events within cancer (Hedstrom, 2007) But positive experiences too! (Bellizi et al, 2012; Karian et al, 1995) Identity Development “You’re no longer that person you used to be. The day you’re told that you have cancer, you’re no longer that person you were a second ago.” Body Image & Self-Esteem “Before treatment, I was a cool kid in high school. I had friends, everything was good. . . And then coming back, I had this thin hair, I was pale, I was overweight. I was walking with 2 canes and limping and hunched over. I was different.” Interrupted Lives I find I matured beyond my years but I’m 2 years younger than everyone else in a sense. I can’t drive yet, I don’t have a job, I haven’t graduated school yet. All my friends are working, going to school, driving, they have boyfriends. I mean they’re having sex and I just can’t relate to any of this.” Adolescent Oncology Narratives “Teens definitely need different care than kids… we’re struggling severely with our identity already, you throw cancer in the mix… and that just messes it up even more.” “Sometimes we want to cry… we are not showing it.” “Sometimes doctors and nurses don’t get it… our world is very small…we need friends around us who understand.” “It’s the smaller picture we care about (how this is affecting my life right now!) as opposed to the bigger picture.” “Get to know me outside of my cancer.” “You can’t treat me like a kid but you also can’t treat me like an adult… cancer is a very scary thing to go through.” Distress: Distress: ‘a multifactorial, unpleasant emotional experience of a psychological (cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment.’ (NCCN, 2012) Distress- Adolescents with Cancer Adolescents and young adults with cancer may be at greater risk for distress Argued that adolescents experience greater distress as compared to children or adults (Kwak et al, 2013b) Inconsistent significant distress levels of AYA reported in literature- ranging from 6-41% (Kwak et al., 2013). Adolescent distress is under-reported and under-addressed Distress is often not recognized by clinicians Distress can occur at any point along the cancer trajectory Why Screen for Distress?? Psychosocial screening and intervention can reduce levels of cancer-related distress and improve QOL (Anderson, 2002; Carlson & Bultz, 2004) Early identification of patients at risk for significant psychosocial distress. Triaging psychosocial distress is not always accurate. Theory should be used to guide screening practice- developmental theory provides good rationale Distress- ‘vital sign’ Canadian Strategy for Cancer Control (2004) added ‘distress’ as a new vital sign to accompany temperature, respiration, heart rate, blood pressure, and pain Challenges to Screening Psychosocial screening for adults with cancer- late 80’s (Zabora, 2012) Screening practices not yet widely adopted for adolescents with cancer (despite extensive use in adult oncology) Lack of standardized screening measures for adolescent distress Does the measure actually measure what it is supposed to? How can we best assess AYA distress? Effectiveness of measures to screen for distress- previous studies focused on distress measures regardless whether measures were accurately identifying AYA distress (Zebrack et al., 2012) Barriers to implementation Research Findings- Distress Adults: 20-40% of survivors experienced high levels of distress throughout their illness- 30% at clinically significant levels of distress (Carlson et al, 2004; Gao, Bennett, Stark, Murray, & Higginson, 2010). AYA: Within 4 months and 12 months since diagnosis, 28% of AYA oncology patients experienced distress that exceeded population norms; improved at 6 months (Kwak et al., 2013a.). Levels of distress equally distributed regardless of diagnosis type, severity or survival rate (Kwak et al., 2013a.). At 6 and 12 months, 39 % and 44%, of patients reported moderate to severe levels of PTSS; 29% had PTSS levels of PTSD (Kwak et al., 2013b.) Higher rates of PTSS were found in AYAs with higher-survival rates (Kwak et al., 2013b) 12% of AYAs reported clinically significant choronic distress throughout 12 months since diagnosis; 15% reported delayed distress. 41% of patients reported un-met counseling needs- this was significantly related to distress over time (Zebrack, Burg, & Vaitones, 2012) Adolescents often have un-met psychosocial needs (Kent et al., 2012) Context for Developing Standardized Distress Guidelines… No standardized screening practice for AYAs Lack of validated distress screening measures for adolescents with cancer Adolescents are experiencing distress that is not being screened and resulting in unmet needs Adolescents are an under-researched population- we simply don’t know much about their unique distress Recent studies have demonstrated that AYA distress exceeds population norms National AYA Distress Sub-Committee Sub-committee of the Canadian National Adolescent and Young Adult Cancer Task Force Developed to address the gaps in the current context of distress screening National psychosocial clinician committee member representation Pediatric and adult oncology clinician committee representation Research Project/Goal: AYA Distress Screening Tool Validation PIs: Dr. Anne Klassen (McMaster); Dr. Norma D’Agostino (PMH) AYA Distress Screening Tool Validation To assess the only validated distress screening tools for AYAs with cancer (AUS) To adapt these screening tools (for on-treatment and off-treatment) for use in Canada with AYAs 15-29 years old; English and French versions Australian AYA Oncology Distress Screening Tool: Distress Thermometer (modified for AYA specific areas of distress); separate versions for treatment and survivorship. Pilot-tested in AUS and found to be valid. Clinical Assessment Questions Demographics Funding has been received from C17 for adaptation of this AUS distress screening tool for AYAs 15-29 in Canada Current phase of the project: content validation Face validity qualitative interviews currently being conducted in English and French (ON & QC) Next phase of project: field validation. Once completed and analyzed, large-scale field validation study will be extended to sites across Canada The field test-data will be analyzed to identify items that represent best indicators of distress based on performance against a standardized set of psychometric criteria. Goal is to have a valid measure of AYA oncology distress. AYA oncology specific screening tool can enhance both research and clinical practice with cancer. Will assist in development of a national screening program for adolescents and young adults with cancer. Where to from here? Distress is being under-screened yet many adolescents are experiencing significant distress How best to screen for distress?? Goal of this project… Screening practice at your local adult oncology centre? BCCA (PSSCAN-R) Strengths/weaknesses of different screening measures Ask questions of this population…