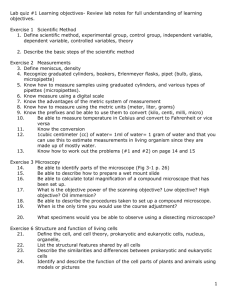
Phospholipid structure
advertisement

Intracellular vs. extracellular concentrations Note: Na+, K+, Cl-, phosphate,- & protein- 1 [IC] vs. [EC] important points *Intracellular cations = Intracellular anions (mEq/L) *Extracelluar cations = Extracellular anions (mEq/L) *miniscule, unmeasurable differences Intracellular particles = Extracellular particles i.e. IC osmolality = EC osmolality 2 Membrane transport overview No carrier: simple diffusion (lipid soluble substances) diffusion through ion channels diffusion through water channels Carrier mediated transport facilitated diffusion (passive) primary active transport (active, uses ATP) secondary active transport (active, uses ion gradient) Endocytosis & exocytosis 3 Simple diffusion Through phospholipid bilayer Lipid soluble substances e.g. O2, CO2, NH3, N2, fatty acids, steroids, ethanol, Passive (down concentration gradient) No carrier ( no saturation, competition) 4 Simple diffusion fig 4-2 5 Simple diffusion (flux) fig 4-3 At equilibrium: compartment 1 concentration = compartment 2 concentration one-way flux (left right) = one-way flux (right left) net flux = 0 6 Simple diffusion (graph of Ci vs. time) fig 4-4 Graph shows that transport is passive i.e. over time Ci will reach, but never exceed Co 7 Simple diffusion (graph of rate vs. concentration) Graph shows that transport is not carrier mediated; because no saturation of transport rate 8 Transport through ion channels fig 4-7 9 Properties of ion channels Usually (not always) highly specific for the ion Ion transport is passive ions are charged therefore, gradient depends on concentration & charge combination is “electrochemical gradient” Channels open and close spontaneously Percentage of “open time” can be regulated (gating) Open time regulated by: binding of ligands to the channels (ligand gating) voltage difference across membrane (voltage gating) stretch of membrane (mechanical gating) covalent alteration of channel protein 10 Facilitated diffusion fig 4-8 11 Facilitated diffusion (properties) Passive, carrier mediated Examples: glucose into most cells (not luminal membrane of kidney or intestine), urea, some amino acids Kinetics: shows: passive shows: carrier mediated 12 Non-mediated vs. mediated transport fig 4-9 13 Primary active transport (Na+/K+ ATPase pump) 3 Na+’s out, 2 K+’s in, 1 ATP hydrolyzed fig 4-11 14 Primary active transport properties Active (energy from direct hydrolysis of ATP) Carrier mediated Used when: many ions moved (e.g. 5 for Na+/K+ ATPase pump) ions moved against steep gradient (Ca++ ATPase in muscle, H+/K+ ATPase in stomach, H+ ATPase in kidney) 15 Primary active transport kinetics shows active transport shows carrier mediated 16 Effect of Na+/K+ ATPase pump fig 4-12 17 Secondary active transport fig 4-13 18 Secondary active transport properties Active (energy from ion gradient, usually Na+) Carrier mediated Can be cotransport (symport) or countertransport (antiport) Examples (many): Na+/amino acids, Na+/glucose (luminal membrane kidney, GI tract), *Na+/H+ kidney, *Ca++/3Na+ muscle, *Cl-/HCO3- red cell. (* = countertransport) Kinetics see primary active transport graphs 19 Transport, the big picture fig 4-15 20 Table 4-2 21 Water transport (aka osmosis) Water moves through aquaporin channels Water moves passively down its own concentration gradient Dissolving solute in water reduces the water concentration Water therefore moves from a dilute solution to a more concentrated solution The “solute concentration” depends on the number of particles The number of particles is called “osmolarity” (?osmolality?) The units of osmolarity are milliosmoles/L (mOsm/L) 22 Calculation of osmolarity The osmolarity of a 100 mM glucose solution is 100 mOsm/L A 100 mM NaCl solution dissociates into 100 mM Na+ and 100 mM Cl-; its osmolarity is therefore 200 mOsm/L Assuming complete dissociation, calculate the osmolarity of the following solutions: 1. 100 mM NaCl, 50 mM urea Answer: 250 mOsm/L 2. 200 mM glucose, 30 mM CaCl2 Answer: 290 mOsm/L 23 Red cells in solution Notes: nonpenetrating solutes, cell osmolarity ~300 mOsm/L fig 4-19 24 Crenated red cells 25 Osmolarity and tonicity Osmolarity is a measure of the total number of particles Tonicity is a measure of the solute particles which do not cross the cell membrane “non-penetrating solutes” Tonicity therefore depends on the properties of the solute and the cell membrane For example, urea crosses most cell membranes, and will enter the cell down its concentration gradient A solution of 300 mM urea is isosmotic to red cells but is hypotonic 26 Osmolarity and tonicity problems 1. Consider a solution of 100 mM NaCl and 200 mM urea. How does its osmolarity and tonicity compare with red cells having an osmolarity of 300 mOsm/L? Answer: hyperosmolar and hypotonic 2. Consider a solution of 125 mM NaCl and 50 mM urea. How does its osmolarity and tonicity compare with red cells having an osmolarity of 300 mOsm/L? Answer: isosmolar and hypotonic 27 Osmolarity (important concept) Because cells contain abundant aquaporin channels, water rapidly equilibrates across the cell membrane Therefore, the osmolarity of virtually all body cells is equal, and equal to the osmolality of extracellular fluid 28 Drinking water 29 Endocytosis and exocytosis fig 4-20 30 Endocytosis and exocytosis properties Endocytosis: pinocytosis, phagocytosis specificity conferred by receptor mediated endocytosis route: see next slide Exocytosis: release of neurotransmitters, hormones, digestive enzymes route: rough er Golgi secretory vesicles release usually triggered by cytosolic [Ca++] insertion of glucose transporters (insulin), insertion of water channels (ADH) 31 Endocytosis route fig 4-21 32 Epithelial transport (Na+) fig 4-22 33 Epithelial transport (water) fig 4-24 34 Epithelial transport (glucose in kidney, GI tract) fig 4-23 35