DJChapter_05
advertisement
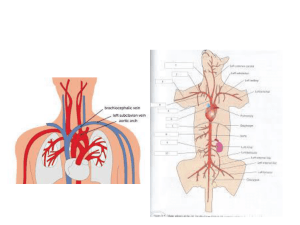
CHAPTER 5 The Anatomy and Physiology of the Circulatory System Copyright © 2008 Thomson Delmar Learning The Circulatory System • Blood • Heart • Vascular System Copyright © 2008 Thomson Delmar Learning THE BLOOD Copyright © 2008 Thomson Delmar Learning Formed Elements of Blood Table 5-1 Copyright © 2008 Thomson Delmar Learning Cell Type Erythrocytes (Red Blood Cells, RBCs) ) Description # of Cells/mm3 D & LS Biconcave, 4-6 million anucleate disc; salmon-colored; diameter 7-8 microns D: 5-7 days DL: 100-120 days Table 5-1 Function Transport O2 & CO2 Copyright © 2008 Thomson Delmar Learning Cell Type—Neutrophils ) Description # of Cells/mm3 D & LS Function Nucleus multilobed; inconspicuous; cytoplasmic; diameter 10-14 microns 3000-7000 Phagocytize bacteria D: 6-9 days LS: 6 hours to a few days Table 5-1 Copyright © 2008 Thomson Delmar Learning Cell Type—Eosinophils ) Description # of Cells/mm3 D & LS Nucleus multilobed; 100-400 red cytoplasmic granules; diameter 10-14 microns Table 5-1 Function D: 6-9 days Kills parasitic worms DL: 8-12 days destroy antigenantibody complexes; inactivate some inflammatory chemical of allergy Copyright © 2008 Thomson Delmar Learning Cell Type—Basophils ) Description # of Cells/mm3 D & LS Function Nucleus lobed; large blue-purple cytoplasmic granules 20-50 Release histamine and other mediators of inflammation; contains heparin, an anticoagulant D: 3-7 days DL: a few hours to a few days Table 5-1 Copyright © 2008 Thomson Delmar Learning Cell Type—Lymphocytes ) Description # of Cells/mm3 D & LS Function Nucleus spherical or indented; pale blue cytoplasm 1500-3000 Mount immune response by direct cell attack or via antibodies D: days-wks DL: hrs-yrs Table 5-1 Copyright © 2008 Thomson Delmar Learning Cell Type—Monocytes Table 5-1 ) Description # of Cells/mm3 D & LS Function Nucleus U- or kidney-shaped; gray-blue cytoplasm; diameter 14-24 microns 100-700 D: 2-3 days DL: months Phagocytosis; develop into macrophages in tissues Copyright © 2008 Thomson Delmar Learning Cell Type—Platelets Table 5-1 ) Description # of Cells/mm3 D & LS Function Discoid cytoplasmic fragments containing granules stain deep purple; diameter 2-4 microns 250,000500,000 D: 4-5 days DL: 5-10 days Seals small tears in blood vessels; instrumental in blood clotting Copyright © 2008 Thomson Delmar Learning Centrifuged Blood-Filled Capillary Tube Fig. 5-1. A centrifuged bloodfilled capillary tube. Copyright © 2008 Thomson Delmar Learning Normal Differential Count Table 5-2 Copyright © 2008 Thomson Delmar Learning Chemical Composition of Plasma Water 93% of plasma weight Proteins Albumins Globulins Fibrinogen Electrolytes Cations Na+ K+ Ca2+ Mg2+ Anions Cl– PO43– SO42– HCO3– Food Substance Amino acids Glucose/carbohydrates Lipids Individual vitamins Table 5-3 Respiratory Gases O2 CO2 N2 Individual Hormones Waste Products Urea Creatinine Uric Acid Bilirubin Copyright © 2008 Thomson Delmar Learning THE HEART Copyright © 2008 Thomson Delmar Learning The Heart Fig. 5-2. (A) anterior view of the heart. (B) posterior view of the heart. Copyright © 2008 Thomson Delmar Learning Anterior View of Heart Fig. 5-2. (A) Anterior view of the heart. Copyright © 2008 Thomson Delmar Learning Posterior View of Heart Fig. 5-2. (B) posterior view of the heart. Copyright © 2008 Thomson Delmar Learning Relationship of Heart to Other Body Parts Fig. 5-3. (A) the relationship of the heart to the sternum, ribs, and diaphragm. (B) Cross-sectional view showing the relationship of the heart to the thorax. (C) Relationship of the heart to the lungs great vessels. Copyright © 2008 Thomson Delmar Learning Layers of the Pericardium and Heart Wall Fig. 5-4. The layers of the pericardium and the heart wall. Copyright © 2008 Thomson Delmar Learning Cardiac Muscle Bundles Fig. 5-5. View of the spiral and circular arrangement of the cardiac muscle bundles. Copyright © 2008 Thomson Delmar Learning Coronary Circulation Fig. 5-6. Coronary circulation. (A) Arterial vessels. (B) Venous vessels. Copyright © 2008 Thomson Delmar Learning BLOOD FLOW THROUGH THE HEART Copyright © 2008 Thomson Delmar Learning Chambers and Valves of the Heart Fig. 5-7. Internal chambers and valves of the heart. Copyright © 2008 Thomson Delmar Learning THE PULMONARY AND SYSTEMIC VASCULAR SYSTEM Copyright © 2008 Thomson Delmar Learning Pulmonary and Systemic Circulation Fig. 5-8. Pulmonary and systemic circulation. Copyright © 2008 Thomson Delmar Learning Neural Control and the Vascular System Fig. 5-9. Neural control of the vascular system. Sympathetic neural fibers to the arterioles are especially abundant. Copyright © 2008 Thomson Delmar Learning Components of the Pulmonary Blood Vessels Fig. 1-29. Components of the pulmonary blood vessels. Copyright © 2008 Thomson Delmar Learning THE BARORECEPTOR REFLEX Copyright © 2008 Thomson Delmar Learning Location of the Arterial Baroreceptors Fig. 5-10. Location of the arterial baroreceptors. Copyright © 2008 Thomson Delmar Learning Arterial Blood Pressure • When arterial blood pressure decreases, the baroreceptor reflex causes the following to increase: – – – – Heart Rate Myocardial Force of Contraction Arterial Constriction Venous Constriction Copyright © 2008 Thomson Delmar Learning The Net Result • Increased cardiac output • Increase in total peripheral resistance • Return of blood pressure to normal Copyright © 2008 Thomson Delmar Learning PRESSURES IN THE PULMONARY AND SYSTEMIC VASCULAR SYSTEMS Copyright © 2008 Thomson Delmar Learning Types of Pressures Used to Study Blood Flow • Intravascular • Transmural • Driving Copyright © 2008 Thomson Delmar Learning Intravascular Pressure • The actual blood pressure in the lumen of any vessel at any point, relative to the barometric pressure • Also known as “intraluminal pressure” Copyright © 2008 Thomson Delmar Learning Transmural Pressure • The difference between intravascular pressure of a vessel and pressure surrounding the vessel Copyright © 2008 Thomson Delmar Learning Transmural Pressure • Transmural pressure is positive when the pressure inside the vessel exceeds pressure outside the vessel, and • Negative when the pressure inside the vessel is less than the pressure surrounding the vessel Copyright © 2008 Thomson Delmar Learning Driving Pressure • The pressure difference between the pressure at one point in a vessel and the pressure at any other point downstream in the vessel Copyright © 2008 Thomson Delmar Learning Blood Pressures Fig. 5-11. Types of blood pressures used to study blood flow. Copyright © 2008 Thomson Delmar Learning THE CARDIAC CYCLE AND ITS EFFECT ON BLOOD PRESSURE Copyright © 2008 Thomson Delmar Learning Sequence of Cardiac Contraction Fig. 5-12. Sequence of cardiac contraction. (A) ventricular diastole and atrial systole. (B) ventricular systole and atrial diastole. Copyright © 2008 Thomson Delmar Learning Systemic Circulation Fig. 5-13. Summary of diastolic and systolic pressures in various segments of the circulatory system. Red vessels: oxygenated blood. Blue vessels: deoxygenated blood. Copyright © 2008 Thomson Delmar Learning Mean Arterial Blood Pressure (MAP) • MAP can be estimated by measuring the systolic blood pressure (SBP) and the diastolic blood pressure (DBP) and using the following formula: Copyright © 2008 Thomson Delmar Learning Mean Arterial Blood Pressure (MAP) • For example, the mean arterial blood pressure of the systemic system, which has a SBP of 120 mm Hg and a DBP of 80 mm Hg, would be calculated as follows: MAP = SBP + (2 x DBP) 3 = 120 + (2 x 80) 3 = 280 3 = 93 mm Hg Copyright © 2008 Thomson Delmar Learning Mean Intraluminal Blood Pressure Fig. 5-14. Mean intraluminal blood pressure at various points in the pulmonary and systemic vascular systems. Copyright © 2008 Thomson Delmar Learning Major Arterial Pulse Sites Fig. 5-15. Major sites where an arterial pulse can be detected. Copyright © 2008 Thomson Delmar Learning The Blood Volume and Its Effect on Blood Pressure • Stroke Volume • Cardiac Output Copyright © 2008 Thomson Delmar Learning Cardiac Output • Cardiac output (CO) is calculated by multiplying the stroke volume (SV) by the heart rate (HR) Copyright © 2008 Thomson Delmar Learning Example • If the stroke volume is 70 mL, and the heart rate is 72 bpm, the cardiac output is: Copyright © 2008 Thomson Delmar Learning Cardiac Output and Blood Pressure • Cardiac output directly influences blood pressure. Thus, – When either SV or HR increase, blood pressure increases – When either SV or HR decrease, blood pressure decreases Copyright © 2008 Thomson Delmar Learning Distribution of Pulmonary Blood Flow • Gravity • Cardiac output • Pulmonary vascular resistance Copyright © 2008 Thomson Delmar Learning GRAVITY Copyright © 2008 Thomson Delmar Learning Distribution of Pulmonary Blood Flow Fig. 5-16. Distribution of pulmonary blood flow. In the upright lung, blood flow steadily increases from the apex to the base. Copyright © 2008 Thomson Delmar Learning Distribution of Pulmonary Blood Flow Fig. 5-17. Blood flow normally moves into the gravity-dependent areas of the lungs. Erect (A), supine (B), lateral (C), upside-down (D). Copyright © 2008 Thomson Delmar Learning Distribution of Pulmonary Blood Flow Fig. 5-18. Relationship between gravity, alveolar pressure, pulmonary arterial pressure, and pulmonary venous pressure in different zones. Copyright © 2008 Thomson Delmar Learning Determinants of Cardiac Output • Ventricular Preload • Ventricular Afterload • Myocardial Contractility Copyright © 2008 Thomson Delmar Learning Ventricular Preload • Ventricular preload – Degree to which the myocardial fiber is stretched prior to contraction (end-diastole) • Within limits, the more myocardial fiber is stretched during diastole (preload), the more strongly it will contract during systole – Thus, the greater myocardial contractility Copyright © 2008 Thomson Delmar Learning Ventricular Preload Reflected In . . . • Ventricular end-diastolic pressure (VEDP) – which, in essence, reflects the . . . • Ventricular end-diastolic volume (VEDV) Copyright © 2008 Thomson Delmar Learning Ventricular Preload • As the VEDV increases or decreases . . . the VEDP . . . and, therefore, the cardiac output . . . increases or decreases, respectively. Copyright © 2008 Thomson Delmar Learning Frank-Starling Curve Fig. 5-19. Frank-Starling curve. Copyright © 2008 Thomson Delmar Learning Appendix V—Cardiopulmonary Profile Copyright © 2008 Thomson Delmar Learning Ventricular Afterload • Ventricular afterload is defined as the force against which the ventricles must work to pump blood Copyright © 2008 Thomson Delmar Learning Ventricular Afterload Directly Influenced By: • Volume and viscosity of blood ejected • Peripheral vascular resistance • Total cross-sectional areas of the vascular space into which blood is ejected Copyright © 2008 Thomson Delmar Learning Ventricular Afterload • Arterial systolic blood pressure best reflects the ventricular afterload Copyright © 2008 Thomson Delmar Learning Ventricular Afterload • Blood pressure (BP) is a function of cardiac output (CO) times the systemic vascular resistance (SVR) Copyright © 2008 Thomson Delmar Learning Myocardial Contractility • Regarded as the force generated by the myocardium when the ventricular muscle fibers shorten Copyright © 2008 Thomson Delmar Learning Myocardial Contractility • In general, when the contractility of the heart increases or decreases – Cardiac output increases or decreases respectively Copyright © 2008 Thomson Delmar Learning Myocardial Contractility • Positive inotropism – Increase in myocardial contractility • Negative inotropism – Decrease in myocardial contractility Copyright © 2008 Thomson Delmar Learning Vascular Resistance • Circulatory resistance is approximated by dividing the mean arterial pressure (MAP) by the cardiac output (CO) Copyright © 2008 Thomson Delmar Learning Vascular Resistance • In general, when the vascular resistance increases: – Blood pressure increases – In turn increases ventricular afterload Copyright © 2008 Thomson Delmar Learning ACTIVE AND PASSIVE MECHANISMS Copyright © 2008 Thomson Delmar Learning ACTIVE MECHANISMS AFFECTING VASCULAR RESISTANCE Copyright © 2008 Thomson Delmar Learning Active Mechanisms—Vascular Constriction (↑ Resistance) • Abnormal Blood Gases – ↓ PO2 (Hypoxia) – ↑ PCO2 (Hypercapnia) – ↓ pH (Acidemia) Copyright © 2008 Thomson Delmar Learning Active Mechanisms—Vascular Constriction (↑ Resistance) • Pharmacologic Stimulation – Epinephrine – Norepinephrine – Dobutamine – Dopamine – Phenylephrine Copyright © 2008 Thomson Delmar Learning Active Mechanisms—Vascular Dilation (↑ Resistance) • Pharmacologic Stimulation – Oxygen – Isoproterenol – Aminophylline – Calcium-channel blocking Copyright © 2008 Thomson Delmar Learning Active Mechanisms—Vascular Dilation (↑ Resistance) • Pathologic Conditions – Vessel blockage/obstruction – Vessel wall disease – Vessel destruction – Vessel compression Copyright © 2008 Thomson Delmar Learning PASSIVE MECHANISMS AFFECTING VASCULAR RESISTANCE Copyright © 2008 Thomson Delmar Learning Passive Mechanisms—Vascular Dilation (↑ Resistance) • ↑ Pulmonary arterial pressure • ↑ Left atrial pressure Copyright © 2008 Thomson Delmar Learning Pulmonary Arterial Pressure Fig. 5-20. Increased mean pulmonary arterial pressure decreases pulmonary vascular resistance. Copyright © 2008 Thomson Delmar Learning Pulmonary Vascular Resistance Fig. 5-21. Schematic drawing of the mechanisms that may be activated to decrease pulmonary vascular resistance when the mean pulmonary artery pressure increases. Copyright © 2008 Thomson Delmar Learning Passive Mechanisms—Vascular Constriction (↑ Resistance) • ↑ Lung volume (extreme) • ↓ Lung volume Copyright © 2008 Thomson Delmar Learning Pulmonary Vessels During Inspiration Fig. 5-22. Schematic illustration of pulmonary vessels during inspiration. Copyright © 2008 Thomson Delmar Learning Pulmonary Vascular Resistance Fig. 5-23. Schematic drawing of the extra-alveolar “corner vessels” found at the junction of the alveolar septa. Copyright © 2008 Thomson Delmar Learning Pulmonary Vascular Resistance Fig. 5-24. PVR is lowest near the FRC and increases at both high and low lung volumes. Copyright © 2008 Thomson Delmar Learning Passive Mechanisms—Vascular Dilation (↑ Resistance) • ↑ Blood volume Copyright © 2008 Thomson Delmar Learning Passive Mechanisms—Vascular Constriction (↑ Resistance) • ↑ Blood viscosity Copyright © 2008 Thomson Delmar Learning Effects of Active and Passive Mechanisms on Vascular Resistance Table 5-4. Copyright © 2008 Thomson Delmar Learning Effects of Active and Passive Mechanisms on Vascular Resistance Table 5-4. ↑ RESISTANCE (VASCULAR CONSTRICTION) ACTIVE MECHANISMS Pharmacologic Stimulations Epinephrine Norepinephrine Dobutamine Dopamine Phenylephrine Oxygen Isoproterenol Aminophylline Calcium-channel blocking agents ↓ RESISTANCE (VASCULAR DILATION) X X X X X X X X Copyright © 2008 Thomson Delmar Learning Effects of Active and Passive Mechanisms on Vascular Resistance Table 5-4. ↑ RESISTANCE (VASCULAR CONSTRICTION) ACTIVE MECHANISMS Pathologic Conditions Vessel blockage/obstruction Vessel wall disease Vessel destruction Vessel compression ↓ RESISTANCE (VASCULAR DILATION) X X X X Copyright © 2008 Thomson Delmar Learning Effects of Active and Passive Mechanisms on Vascular Resistance Table 5-4. ↑ RESISTANCE (VASCULAR CONSTRICTION) PASSIVE MECHANISMS Pathologic Conditions ↑ Pulmonary arterial pressure ↑ Left atrial pressure ↑ Lung volume (extreme) ↓ Lung volume ↑ Blood volume ↑ Blood viscosity ↓ RESISTANCE (VASCULAR DILATION) X X X X X X Copyright © 2008 Thomson Delmar Learning Clinical Application 1 Discussion • How did this case illustrate … – Activation of the baroreceptor reflex? – Hypovolemia and how it relates to preload? – Negative transmural pressure? – Effects of gravity on blood flow? Copyright © 2008 Thomson Delmar Learning Clinical Application 2 Discussion • How did this case illustrate … – Ventricular afterload? – Ventricular contractility? – Ventricular preload? – Transmural pressure? Copyright © 2008 Thomson Delmar Learning