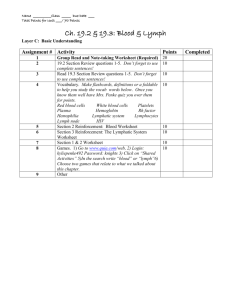
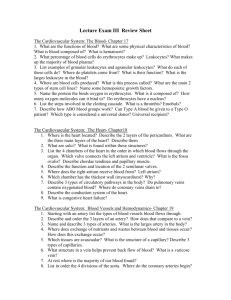
The Lymphatic System and the Blood

Overview
Why needed?
Origin:
Blood vessels form from mesoderm
Blood produced 2 wks after vessels are formed, during the 5 th week of life
What is blood?
Connective tissue?
Different from others
Matrix not a solid or semi-solid material
Matrix of blood is plasma
watery substance
○
○
Yellowish
○ 90% Water
7% protein
1% minerals
○ 2% other materials incl. atmospheric gases, chem signals, and nutrients
More on plasma
Contains:
Atmospheric gases:
oxygen , carbon dioxide, and nitrogen
Comprises 55% of blood volume
Formed elements
(= Cellular components)
Remaining 45% of blood volume:
Erythrocytes (RBCs)
Leukocytes (WBCs)
Thrombocytes (platelets)
Hematocrit
Calculates the volume of red blood cells making up the blood
Included in a CBC
FYI: CBC (on medical shows) = complete blood count
Complete Blood Count includes…
Hematocrit
The number of RBCs
The number of WBCs
The total amount of hemoglobin in the blood
Also provides information about the following measurements:
Average red blood cell size (MCV)
Hemoglobin amount per red blood cell (MCH)
The amount of hemoglobin relative to the size of the cell (hemoglobin concentration) per red blood cell
(MCHC)
The platelet count is also usually included in the
CBC.
Can you answer these questions?
What is the blood composed of?
Why is the blood unlike any other connective tissue?
What does a hematocrit tell you?
Red Blood Cells
No mature nucleus (lost in dev.)
No DNA, so ….
○ Use enzymes to carry out their tasks
Reticulocytes (immature RBC) – have mesh-like network of rRNA … become mature in ~24 hours
○ Live max 120 days
○ No way to repair & replace damaged cellular components
Appear red b/c of hemoglobin
○ Contains iron facilitates transport of
O
2
and CO
2
4.8 million RBC/mm 3 in women
5.4 million RBC/mm 3 in men
Blood Type
Genetic
Determined by the antigens on the surface of the
RBC membrane
A,B,O blood group system most common (30 possible in full blood type classification!)
Blood will attack “non-self”
Important to match blood types for transfusions
Therefore …
AB universal acceptor
O universal donor-has no proteins on the membrane
Rh Factor
The “D” protein
Most are positive (depends on geography)
If a woman is negative and conceives with a positive man, problems can arise — erythroblastosis fetalis
This can lead to anemia, a condition marked by weakness and fatigue. Severe anemia can lead to heart failure and death. The breakdown of RBC leads to the buildup of bilirubin which can lead to jaundice and brain damage.
Prevention of erythroblastosis fetalis
Treat negative mothers with Rhogam , a preventative measure
Prevents formation of antibodies to Rh molecule
Given whenever there is a possibility of fetal blood mixing with maternal blood following childbirth, abortion, miscarriage, prenatal testing.
Once sensitized the woman will always react against Rh+ cells
Can you answer these questions?
3.
4.
5.
1.
2.
6.
How are RBCs different from most other cells?
How does the lack of a nucleus affect
RBCs lifespan?
What is hemoglobin and what does it do?
Why are RBCs red?
What is blood type? What do the different blood types mean?
Why is it dangerous for an Rh- woman to have an Rh+ baby?
White Blood Cells
WBC : RBC ratio = 1 : 500 or 1000
Use blood, lymph to move from bone marrow to the tissues
5 types (differential WBC count measures them)
Neutrophils (Most abundant)
Lymphocytes
Eosinophils
Monocytes
Basophils (Least abundant)
Agranulocytes
AKA : Mononuclear
Lack visible granules in cytoplasm
Monocytes Lymphocytes
T & B cells
Granulocytes
Noticeable granules that produce specialized secretions for fighting infection
Nucleus is polymorphic , lobed, unusually shaped
Eosinophils, basophils, neutrophils
Neutrophils
Granulocyte
Most common WBC
Nucleus = 2-5 lobes
Found in the blood
First responders in the inflammation response due to environmental exposure, some cancers, bacterial infection
Predominant cell in pus
Eosinophils
Granulocyte
5% of WBCs
Bi-lobed nucleus
Combats parasitic infections (protists, worms)
Secretions produced related to allergies
Normally in thymus GI, ovaries, testes, spleen, uterus, lymph nodes
NOT in lungs, esophagus, or skin if found here, indicates disease/pathology
Basophils
Granulocyte (least common)
Susceptible to basic dyes
Large, bi-lobed nucleus (similar to mast cells)
Granules obscure the nucleus
“ Bas-ically all granules ”
Involved in allergies .
Stores, secrete histamine & heparin
(anticoagulant)
Found where allergic reactions are taking place
Agranulocytes
Lymphocytes
“Immune” cells:
NK (natural killer) cells (no prior activation needed)
T lymphocytes (mature in thymus)
○ Helper: direct immune response
○ Cytotoxic: release cytotoxin to kill pathogen infected cells
B lymphocytes (mature in bone marrow): Use antibodies to neutralize pathogens
Monocytes
Agranulocyte
Largest of WBCs
- shaped nucleus
Mono = kissing = Love = heart
Many vesicles in cytoplasm for processing pathogens
Perform phagocytosis - uptake & digestion of pathogens
Fragments of “eaten” pathogen signal Tlymphocytes to the area
Platelets
Cell fragments derived from larger cells called megakaryocytes.
Have “sticky” proteins
Reduce blood flow to an affected area.
Reduce blood loss
Sensitive to many types of hazardous chemicals and pollutants
Can you answer these questions?
Describe the characteristics & functions of all granulocytes, agranulocytes, and platelets.
Compare and contrast the structure & function of RBCs and WBCs
Why are platelets called the “Band-Aids” of the blood?
Carry oxygen from the lungs to the body
Carry carbon dioxide from the body to the lungs
Alveoli-where gas exchange happens in the lungs
RBC in the capillaries that surround the alveoli oxygen enters
Only if the partial pressure of oxygen outside is higher than inside
In cytoplasm of RBC oxygen binds to
Hemoglobin
Four oxygen molecules bind to hemoglobin (w/ the iron)
Carries CO
2 also; binds to a different area than O
2
Percent saturation :
amount of oxygen that is dissolved in a solution of hemoglobin molecules
O
2 sats = 98% or above
Similar to with myoglobin in muscle
Greater affinity for oxygen
Hemoglobin collects oxygen a low partial pressures
In the tissues the oxygen is released and carbon dioxide enters the RBC, binds to
Hemoglobin.
Partial pressures of the gases must appropriate
Some cellular wastes stimulate the release of the oxygen from the hemoglobin
○ Allows RBC to give more O
2 metabolic needs to tissues w/ high
Carried 3 ways in the blood
1. Carried in the blood as a gas (10%)
2. Binds to empty hemoglobin: carbaminohemoglobin
3. As a bicarbonate ion (HCO
3
)
○ CO
2 can dissolve in water, forming bicarbonate ion
○ Dissolves in the blood plasma
Carbonic anhydrase : enzyme in RBC that stim’s the formation of carbonic anhydrase, which dissociates to form bicarbonate ions and H+ ions
Eventually excreted
Diffusion: High concentration low concentration
For Oxygen:
Partial pressure is higher in blood than in tissues
For Carbon Dioxide:
Partial pressure is higher in tissues than in blood
Occurs when the CO
2 is extremely high in the environment or the blood
Acute: high levels in the air
Subacute : toxicity caused by the body’s failure to eliminate carbon dioxide
Decreases blood’s pH (what kind of acid does CO
2 form when it dissolves in water?)
○ Carbonic acid!
What is the purpose of RBCs?
Where does oxygen bind to the Hb molecule?
Where does Hb collect oxygen? Then what happens?
Describe the partial pressures that must be present for oxygen to diffuse from
RBC to tissues and for carbon dioxide to move to the cells?
In general:
Fight infections & disease
Granulocytes :
○ granules of toxic chemicals that kill microorganisms
○ regulate reactions to foreign materials in the body
Pass through capillaries to tissues to with infections.
Attracted to affected areas by factors secreted by damaged cells/tissues
Stick to injured tissues, use phagocytosis to engulf remains of bacteria and damaged cells
Secretes antibiotics-harms/kills bacteria
Secretes other chemicals that stim.
Inflammation ↑ blood flow to the area & ↑ WBC concentration
Secretions defend against parasitic infections esp. protists
& worms
↑ in eosinophils = parasitic infection
Granules contain major basic protein to kill the parasites
Secrete chemicals associated w/ allergies
Secrete histamine stim the immune response
Overproduction of histamine runny nose, sneezing, watery eyes
Mast cells (special kind of basophil)
Cause inflammation of tissues
Secrete chemical that attract neutrophils
Found in walls of small bl. vessels
Clear granules give cytoplasm a grey appearance
When they leave the bone marrow they become either:
Circulating monocytes
○ Detect infections in blood
○ Bone growth & maintenance
Tissue monocytes (macrophages)
○ Remove dead cells
○ Attack microorganisms that are difficult to kill (fungi)
Stay tuned! We’ll talk about it later….for now, they carry out most of the duties of the immune system
Which WBC is in charge of engulfing bacteria?
Which WBC is in charge of protecting us from parasites?
Which WBC differentiates into cells that assist in bone growth and maintenance or are macrophages that protect against fungal infections?
Which WBC secretes major basic protein?
Blood clotting
Platelets adhere to injured area
Activation of blood clot formation
Important that clot forms by injury only
Intact cells secrete prostacyclin (prevents platelet activation)
1.) BV damaged, releases “distress chemicals”
2.) Clotting factors stim. other factors that indicates presence of damaged tissues a.) platelets stick to damaged tissues & each other b.) Platelets secrete prothrombin activator & Ca 2+
Catalyze conversion of prothrombin to thrombin c.) Thrombin causes fibrinogen fibrin d.) Fibrin forms a sticky mesh that adheres to thrombocytes and other blood components (clot)
Clot forms a barrier that prevents blood loss & impedes the passage of microorganisms into tissues
Calcium ions = catalyze PT to T
Vitamin K = synthesis of clotting factors
Prothrombin Thrombin Fibrinogen Fibrin
So the blood doesn’t clot unintentionally!
They aren’t permanent
Plasminogen plasmin (digests fibrin and dissolves a clot)
Healthy cells near the clot secrete TPA
(tissue plasminogen activator) dissolves fibrin as well.
Can you answer these questions?
1.) What is the purpose of prostacyclin?
2.) What is the purpose of a clot?
3.) What are the steps of the clotting cascade?
4.) What is the role of calcium and vitamin K in clot formation?
5.) Why is the clot cascade so complex?
6.) What do plasmin and tissue plasminogen have in common? What’s the difference?
Adults: bone marrow
Embryo: Liver
Different forms of Hb throughout development allow fetus to adapt to varying metabolic needs for oxygen
11 million/sec in an adult
1 WBC produced for every ~500 RBCs
Adults: bone marrow
Embryo: Liver
11 million/sec in an adult
1 WBC produced for every 700 RBCs
GF
Hematopoietic stem cell
Or
Multipotent stem cell
Or
Pluripotent stem cell
Myeloid stem cell
(progenitor)
GF
Lymphoid stem cell
(progenitor)
The life history of erythrocytes
(RBCs)
Blood oxygen decreases
Stimulates erythropoietin production from kidneys and liver
Erythropoietin Erythropoiesis in red bone marrow (where is this found?)
Immature erythrocytes have a large nucleus
Hb production begins in basophilic erythroblasts
Reticulocytes: lose nucleus, after 1-2 days in circulation lose organelles
If the need for oxygen is great, erythropoiesis will occur at an increased rate.
This means an increased amount of polychromatic erythroblasts will enter the blood stream
Erythropoiesis of a single erythrocyte takes approximately 4 days
Normal bone marrow has an abundance of newly formed RBCs and megakaryocytes (which produce platelets)
Removed by macrophages
Globin (protein) is broken into individual amino acids & recycled
Iron is recycled
Parts of the molecule are converted to bilirubin
Processed in liver, secreted in bile in small intestine
○
○
Bacteria convert into pigments feces color
Some excreted in urine yellow color
Lifespan = 13-20 days
Destroyed in lymphatic system
When released from bone marrow called stabs or bands
Esp. neutrophils b/c their nuclei aren’t lobed, yet, and look like a rod (stab = German for rod) or bands
Functions of Lymphatic System
1.) Maintain fluid balance in the tissues
○
○
30L fluid from capillaries to interstitial and only
27L pass from interstitial back into capillaries qd (every day)
If fluid left in the body tissue damage
○ 3L fluid enter lymph capillaries, called lymph
Then to lymph vessels & return to blood
2.) Absorb fats & other substances from digestive tract (chyle)
3.) Defense
○ Nodes filter lymph & spleen filters blood of microorganisms & foreign substances
Lymphatic System Structures
Lymph
Like plasma: ions, nutrients, wastes from interstitial spaces
Hormones, enzymes from cells in tissues
Lymphocytes
Lymph vessels
○ Flow of lymph produced by gravity
○ or skeletal muscle, passively drains to lower body from upper
Valves-no backflow
○ Lymphatic trunks drain lymph from larger areas of body
Clusters of lymphatic tissue
Lymphatic System Structures
Lymph nodes
Collections of lymphatic tissue covered by connective-tissue capsules
Eliminate antigens from lymph as lymph flows thru the node.
In groups along the larger lymphatic vessels
Lymph node structure
2 divisions: Cortex (outer) & Medulla (inner)
Cortex
○ Has “compartments” called lymphatic nodules
○
○
2 layers: inner layer called germinal center where Blymphocytes are found. In the “wall” surrounding the germinal center is where T-lymphocytes are found.
Nodules are sep’d by trabeculae—extensions of the capsule
—fibrous covering of the node
○ Cortical sinus: spaces where lymph flows through
Medulla
○ Medullary sinus = space where lymph flows throught he center of the node, contains macrophages
○ Medullary cord = contains lymphocytes
Lymphatic System Structures
Tonsils
Swollen cluster of lymphatic tissue in throat
Form protective ring of lymphatic tissue around the openings between the nasal and oral cavities & pharynx
Provide protection against bac and other harmful material
Eventually disappear in adults
Spleen
Detects and responds to foreign substances in the blood
Destroys worn out red blood cells
Acts as a blood reservoir
Structure
○ Left side of the extreme superior, posterior corner of ab cavity
○ White pulp: Contains T & B lymphocytes
Assist body with infections that require a large immune response
○ Red pulp: removes old/damaged RBCs
Lymphatic System Structure
Thymus
Deep to manubrium
In newborn, extends length of thorax & grows until puberty, then decreases in size
Function
○ Produce lymphocytes that move to other lymph tissues, but most degenerate before moving on
○ Produces secretions that mature T-lymphocytes
Can’t destroy normal body cells (Self-tolerance)
Immunity words to know:
Antigen : a substance that can induce an immune response.
Hapten : A molecule that can cause an immune response when attached to blood proteins.
Two ways the immune system can respond to disease:
Innate immunity
Acquired immunity
Why an immune system?
We are outnumbered! Viruses and bacteria are everywhere!
Humans offer limitless resources for pathogens
Energy
Reproductive potential
Getting into the body isn’t easy!
Meet the enemy
Bacteria
Free-living
Not all are bad!
Pathogenic ones produce toxins that damage human tissue
Viruses
Obligate parasites
Hijack human cells; convert to virusproducers, killing host cell in the process
(And fungi, protozoa too…)
A human fortress: Prevention
Skin is thick – hard to penetrate
Produces substances that deter invasion:
Skin pH (not favorable)
Mucus (sticky trap)
Lysozymes (digest bacteria)
Specialized traps around vulnerable areas
(Eyes, nose, mouth)
Cilia sweep away invaders that are trapped
Stomach acid kills ingested invaders
…but we
do
get sick!
Enter through weak points:
Food
Nose
Break in skin/scrapes
Cells are damaged/destroyed
Dying cells release distress chemicals
( histamine )
○ Triggers inflammation (blood vessel dilation, increased blood flow)
○ Draws defensive cells to area (generalized white blood cells)
How do we tell “friend” from
“foe”?
All cells present antigens – surface protein molecules that identify identity
(antigen = antibody generator)
Immune system reacts to foreign antigens
A complex system!
Several “lines” of defense:
1.
2.
3.
Barriers (First line of defense)
Generalized defenders (Second line of defense)
Specific defenders AND memory (Third line of defense)
Consist of:
Several types of cells
Proteins
The Complement System
Part of second line of defense
Free-flowing proteins found in blood
Quickly reach site of invasion
React to antigens
When activated, can
Trigger inflammation
Attract “eater cells” ( macrophages )
Coat pathogen (make macrophages’ job easier)
Kill intruder directly
Phagocytes
Find and “eat” bacteria, viruses, dead/injured body cells by phagocytosis
3 types:
Neutrophils
Macrophages
Dendritic cells
Neutrophils
Often first to site of infection
Numerous
Short lifespan
“Pus” in infected wounds chiefly composed of neutrophils
Macrophage
“Big eaters”
Slower to respond to invader than neutrophil
Larger, longer-lived, more capable
Help alert rest of immune system to invader
Start as monocytes; become macrophages when entering bloodstream
Dendritic cells
“Eater” cells
Help with immune system activation – act as antigen-presenting cells
Filter bodily fluids to clear foreign organisms and particles
Lymphocytes: Third Line of
Defense
T and B cells
Originate in bone marrow
Migrate to lymph nodes, spleen, thymus to mature
Lymph vessels
transport, store lymphocytes
Feeds cells into body
Filter out dead cells/invading organisms
Receptors
Each lymphatic cell contains surface receptors
Recognize foreign antigens
Specialized for a particular antigen
T cells
Two types: helper and killer
T = thymus
Mature here
Helper T cell
Main regulator of third line of defense
Primary task: activate B cells and killer T cells
Activated by macrophages/dendritic cells
( antigen presentation )
Killer T cell
Attacks body cells infected by pathogen, cancer cells
Receptors used to determine if each cell encountered is self/non-self ( compare to accepted receptors, MHC)
B lymphocyte cell
Searches for antigens matching receptor
If a match is found…
Connects to antigen
Triggering signal set off…
○ T helper proteins help fully activate B cell
Produces 1000’s of clones : differentiate into plasma cells or B memory cells
Plasma Cell
Produces antibodies
Responds to same antigen matched by
B cell receptor
Seek out intruders, help destroy them
Release tens of thousands/second
Antibodies
Y-shaped
Attach to matching antigens
Enhance phagocytosis of macrophages (label for capture)
Neutralize toxins
Incapacitate viruses (coat surface proteins)
Group pathogens by linking ( agglutination )
Immunoglobins
Ig G : most common, fight general infections, pass from mom to child in pregnancy ( G= mom’s gift )
Ig A : in mucous membranes of the digestive system, milk, tears, saliva ( A= a lot of mucus )
Ig M : natural defenses against general bacterial infections ( M=most bacteria )
Ig E : stim basophils and mast cells to defend against parasites fungi and worms ( E=eeww!
)
Ig D : on membranes of B-lymphocytes, form plasma and memory cells ( D=defend blood )
Memory cells
Prolonged lifespan
“Remember” specific intruders
Both B and T cells have memory cells
Helps trigger immune system to respond more quickly if invader reappears
Inflammation
Outcome of acquired immune response
Increases blood circulation to affected area
Bv’s dialate to increase blood flow
Immune cells go to injured area
Immune resp. takes place at the site it’s needed
Tissues = red and warm b/c of the blood that enters the area, ↑ in temp = anti-microbial
Pain from pressure of swollen tissues on nerve endings
Normal functions return when the tissue is fully recovered
Natural Immunity
Natural : exposed to foreign antigens as a part of everyday life.
Active immunity – body responds to foreign antigens and develops immunity using B and T lymphocytes
Passive immunity –
○ Embryological development when antibodies (Ig’s) from the mother’s blood stream are passed to the fetus
○ Breastfeeding – baby receives antibodies via milk
Artificial Immunity
Active: Immunization
Therapeutic exposure to antigens
Stimulates the primary response by introducing pathogenic material (inactivated, attenuated, or partial) into the body
Vaccines are typically used for viruses! Antibiotics are
only for bacteria
Passive: Antibody Transfer
Patient receives (via injection) large amounts of antibodies to fight disease
○ Globulin injections can remove certain microorganisms from the body.