Chapter 5: Integument System
advertisement
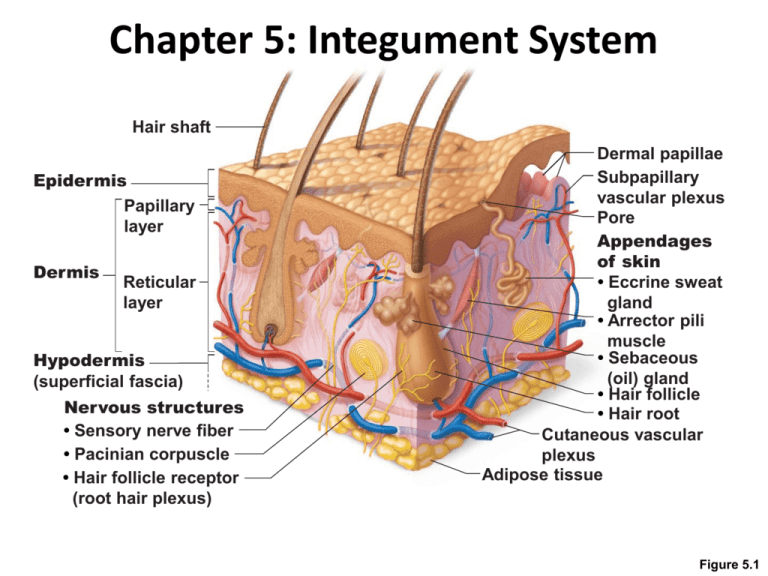
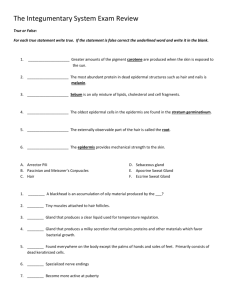
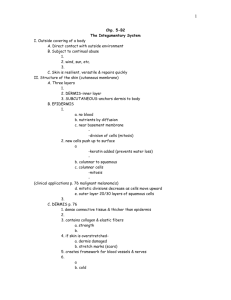
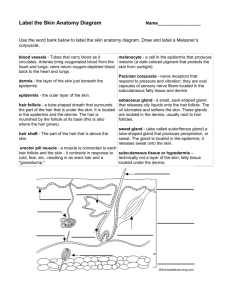
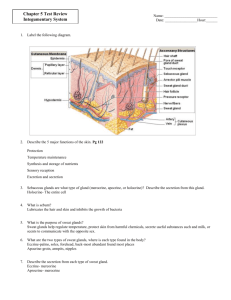
Chapter 5: Integument System Hair shaft Epidermis Papillary layer Dermis Reticular layer Hypodermis (superficial fascia) Nervous structures • Sensory nerve fiber • Pacinian corpuscle • Hair follicle receptor (root hair plexus) Dermal papillae Subpapillary vascular plexus Pore Appendages of skin • Eccrine sweat gland • Arrector pili muscle • Sebaceous (oil) gland • Hair follicle • Hair root Cutaneous vascular plexus Adipose tissue Figure 5.1 Integument System • Skin and its derivatives – sweat and oil glands, hair, and nails • Skin – – – – – – Covers entire body 1.2 2.2 square meters ~4 – 5 kg, 9-11 lbs ~ 75 of total body weight Thickness varies – 1.5 4.0 mm thick 2 regions – • dermis – tough, leathery material, vascularized fibrous connective tissue • Epidermis – epithelial cells, outermost protective shield Skin • Epidermis • Dermis • Hypodermis – – – – – – – – – – Also called superficial fascia Not part of skin But same protective feature Mostly adipose tissue Anchors skin to underlying structures Loosely so that skin can slide freely over structures Shock absorber/insulator Thickens when gain weight Women – accumulates in thighs and breasts first Men – anterior abdomen “beer belly” Hair shaft Epidermis Papillary layer Dermis Reticular layer Hypodermis (superficial fascia) Nervous structures • Sensory nerve fiber • Pacinian corpuscle • Hair follicle receptor (root hair plexus) Dermal papillae Subpapillary vascular plexus Pore Appendages of skin • Eccrine sweat gland • Arrector pili muscle • Sebaceous (oil) gland • Hair follicle • Hair root Cutaneous vascular plexus Adipose tissue Figure 5.1 Epidermis • • • • Keratinized stratified squamous 4 distinct cell types 4 or 5 layers Cells: 1. 2. 3. 4. Keratinocytes Melanocytes Epidermal dendritic cells Tactile cells Keratinocytes • Most common • Produce keratin – fibrous protein that helps give epidermis its protective function • Arise from cell layer – stratum basale • Continuous mitosis – epidermal growth factor • Push cells upward by production of new cells • By the time they reach the surface – dead, scale like structures with a keratin filled plasma membrane Keratinocytes • • • • Millions of dead cells rub off everyday Totally new epidermis every 25 – 45 days Friction – hands and feet – accelerated Persistent friction – causes thickening of epidermis - callus Melanocytes • Spider shaped epithelial ells that synthesize melanin • Found in deepest layer of epidermis • Melanin – made and accumulated in membranous granules • Melanosomes – moved to ends of melanocyte processes, then taken up by keratinocytes • Pigment – protects nucleus from damaging effects of UV radiation Epidermal Dendritic Cells • Also called Langerhorn cells • Arise from bone marrow and migrate to epidermis • Ingest foreign substances • Key activators of the immune system • Slender processes extend around keratinocytes – forming continuous network Tactile (Merkel) Cells • • • • Present in epidermal junction Shaped like spiky hemisphere Associated with disk like sensory nerve ending Sensory receptor for touch Layers of Epidermis • Variation – thick or thin skin • Thick skin – covers – palms, fingers, soles • 5 layers or strata – Stratum basale – DEEP – Stratum spinosum – Stratum granulosum – Stratum lucidum – Stratum corneum – superficial (a) Dermis Stratum corneum Most superficial layer; 20–30 layers of dead cells represented only by flat membranous sacs filled with keratin. Glycolipids in extracellular space. Stratum granulosum Three to five layers of flattened cells, organelles deteriorating; cytoplasm full of lamellated granules (release lipids) and keratohyaline granules. Stratum spinosum Several layers of keratinocytes unified by desmosomes. Cells contain thick bundles of intermediate filaments made of pre-keratin. Stratum basale Deepest epidermal layer; one row of actively mitotic stem cells; some newly formed cells become part of the more superficial layers. See occasional melanocytes and epidermal dendritic cells. Figure 5.2a Layers of Epidermis • Thin Skin – covers rest of body • Stratum lucidum – absent • Outer strata thinner Stratum corneum Most superficial layer; 20–30 layers of dead cells represented only by flat membranous sacs filled with keratin. Glycolipids in extracellular space. Stratum granulosum Three to five layers of flattened cells, organelles deteriorating; cytoplasm full of lamellated granules (release lipids) and keratohyaline granules. Stratum spinosum Several layers of keratinocytes unified by desmosomes. Cells contain thick bundles of intermediate filaments made of pre-keratin. Stratum basale Deepest epidermal layer; one row of actively mitotic stem cells; some newly formed cells become part of the more superficial layers. See occasional melanocytes and epidermal dendritic cells. Desmosomes Melanin granule Melanocyte (b) Keratinocytes Dermis Sensory nerve ending Epidermal Tactile dendritic cell (Merkel) cell Figure 5.2b 1. Stratum Basale • Basal layer • Also called stratum germinative ‘germinating layer” • Deepest epidermal layer • Attached by wavy borderline • Single row of stem cells • Many mitotic nuclei • 10- 25 % of cells – melanocytes • Occasional tactile cells 2. Stratum Spinosum • • • • • • • • Prickle layer Several cell layers thick Web like system of intermediate filaments Tension resisting bundles of pre-keratin filaments Span cytosol and attach to desomones Keratinocytes – have spines – called prickle cells Artifacts that arise during tissue prep Scattered are melanin granules and epidermal dendritic cells 3. Stratum Granulosum • Granular layer • 3 to 5 cell layers in which keratinocytes – appearance changes • Keratinization – cells fill with protein keratin • Cells flatten, nuclei and organelles begin to disinigrate • Accumulate 2 types of granules: – Keratohylane granules – help to form granules – Lamellated granules – water resistant glycolipids, slow water loss across epidermis • Plasma membrane thickens as cytosol proteins bind • Lipids released – coat outer surface • Make more resistant to destruction 4. Stratum Lucidum • Clear layer • Appears – thin translucent • 2 or 3 rows of clear, flat, dead keratinocytes with distinct boundaries • Arrogate in large, cable like parallel arrays • Visible in only thick skin 5. Stratum Corneum • • • • • • • • • • • Horney layer Broad zone of 20-30 cell layers thick ¾ of total thickness Keratin and thickened plasma membrane of cells – protect skin against abrasion and penetration Glycolipids – water proof Durable overcoat Protects deeper cells from – air, water-loss, and chemical, biological, and physiological assaults Layer of dead cells – play many roles Remnants – cornified or horney cells Average person – sheds 18 kg in lifetime Outer skin we see - DEAD Dermis • 2nd major skin region • Strong, flexible connective tissue • Connective tissue proper cells – fibroblasts, macrophages, mast cells, and WBCs • Semi fluid matrix – binds together like a stocking • “hide” – like animal hide • Richly supplied with nerve fibers, blood, and lymphatic vessels • Major portion of hair follicles, sweat, and oil glands found here Dermis • 2 layers – 1. Papillary layer – - thin, superficial areolar connective tissue - Fine, interlacing collagen and elastic fibers from loosely woven mat - Numerous small blood vessels - Dermal papillae – superior surface - Peg like projections - Indent overlying epidermis - House fee nerve endings - pain receptors - touch receptors – Meissner’s Corpuscles Dermis • • • • • • • • Papillary layer – cont Palms of the hands and soles of the feet Papillae lie atop larger mounds – dermal ridges Turn overlying epidermis into epidermal ridged (mounds) Friction ridges – increased friction and enhanced gripping ability Genetically determined and unique to each Sweat pores – open at crest Sweat = fingerprints Friction ridges Openings of sweat gland ducts (a) Figure 5.4a Dermis 2. Reticular Layer – deeper - 80 % of thickness of dermis - Coarse, irregularly arranged - Dense fibrous connective tissue - Cutaneous plexus – network of blood vessels - Extracellular matrix – adipose cells - Thick bundles of collagen fibers Dermis 2. Reticular Layer – deeper (cont) - Less dense regions – cleavage or tension lines - Incisions made parallel to lines – skin gapes less and heals better - Gives skin strength - Keeps skin hydrated - Stretch recoil properties - Flexure lines – dermal folds – occur near joints Skin Color • • • • • 3 pigments – melanin, carotene, and hemoglobin Only melanin – made in skin Melanin – polymer of tyrosine amino acids 2 forms Range in color from yellow tan and reddish brown black • Synthesis depends on enzyme – tyrosine • Pigment found only in deeper layer of epidermis Melanin • Humans – differ in skin color • Not random – – Darker – near equator, need greater amount of protection from the sun – Lighter – closer to poles, need less protection • Melanocytes of darker skinned people produce more and darker melanocytes • Freckles and pigmented nevu (moles) – local accumulation of melanin Melanin • Prolonged sun exposure – substantial melanin buildup • Protects skin from UV radiation • Excessive sun – damages skin – – – – Clumping of elastic fibers – leathery skin Temporary depresses immune system Alters DNA of skin cells – leads to skin cancer UV radiation – also destroys folic acid stores – can be harmful if pregnant – impaired development of fetal NS Carotine • Yellowish – orange pigment • Found in certain plant products – carrots • Accumulates in stratum corneum and fatty tissue of hypodermis • Converted to vitamin A – essential for normal vision • Infants - orangey Hemoglobin • Pinkish hew • Caucasian – small amounts of melanin – hemoglobin color shows through • Cyanosis – blue skin – hemoglobin poorly oxygenated – Heart failure and severe respiratory disorders – Darker skin – melanin masks, but can be seen in mucus membranes and nail beds Alterations in Skin Color • Redness – erythema – embarrassment, fever, hypertension, inflammation or allergy • Pallor – blanching – fear, anger, also signifies anemia or a decrease in BP • Jaundice – yellow – liver disorder, yellow bile pigments accumulate in blood, deposited in body tissues • Bronzing – Addison's Disease, adrenal cortex – inadequate amounts of steroid hormones, sign of pituitary gland tumor • Black and Blue – burses, blood escaped circulation and clotted beneath skin, hematomas – blood swelling Appendages of Skin • Nails, sweat glands, sebaceous (oil) glands, hair follicles and hair • Forming – appendages • Epithelial bud – formation • Stimulated by reduced production of cell adhesion factor (cadherin) • Cell-cell attractions – broken, cells move and rearrange themselves Sweat (Sudoriferous) Glands • Distributed over entire skin surface except nipples, and parts of external genitalia (tip of penis) • Up to 3 million per person • 2 types – eccrine and apocrine • Myoepithelial cells – specialized cells – contract when stimulated by NS • Contraction forces sweat into and through duct system to surface Eccrine Sweat Glands • Merocrine sweat glands • Numerous • Most abundant in palms, soles of feet, and forehead • Simple coiled tubular gland • Secretory part in dermis • Duct –open in a funnel shaped pore on skin surface Sweat pore Eccrine gland Sebaceous gland Duct Dermal connective tissue Secretory cells (b) Photomicrograph of a sectioned eccrine gland (220x) Figure 5.5b Eccrine Sweat Glands • Secretion – sweat • Hypertonic filtrate of the blood • Released by exocytosis – – – – – – – 99 % water Some salts (NaCl) Vitamin C Antibodies Microbe killing peptide – dermcidin Metabolic wastes (urea, uric acid, and ammonia) Small amounts of ingested drugs • Acidic pH 4.0-6.0 Eccrine Sweat Glands • Sweating – • Regulated by sympathetic part of Autonomic NS • Major role – prevent from overheating • Heat induced sweat begins at head and spreads • Emotionally induced stress – begins at palms, soles, and armpits Sweat pore Eccrine gland Sebaceous gland Duct Dermal connective tissue Secretory cells (b) Photomicrograph of a sectioned eccrine gland (220x) Figure 5.5b Apocrine Sweat Glands • • • • • • • Approximately – 2000 of them Confined to auxiliary asnd anogential areas Exocytosis Larger than eccrine Lie deeper in dermis and sometimes hypodermis Ducts empty into hair follicles Same basic components of sweat plus some fatty substances and proteins • Viscous • Milky/yellowish color • When organic molecules are decomposed by bacteria – body odor Apocrine Sweat Glands • Begin functioning at puberty • Little role in thermoregulation, function not yet known • Through of as the human equivalent of scent glands • Increased activity during foreplay • Enlarge and recede with menstrual cycle Apocrine Sweat Glands • Ceruminous glands – modified apocrine glands • Lining of internal ear canal • Secretion mixes with sebum • Sticky bitter substance – cerumen – earwax • Thought to deter insects and block entry of foreign material Apocrine Sweat Glands • Mammary Glands – specialized sweat glands • Secret milk Sebaceous (oil) Glands • Oil glands • Simple branched alveolar glands • Found all over body except thick skin of palms and soles • Small amounts on body trunk and limbs • Numerous on face, neck, and upper chest • Secrete – sebum- oily substances Sweat pore Dermal connective tissue Sebaceous gland Sebaceous gland duct Eccrine gland Hair in hair follicle Secretory cells (a) Photomicrograph of a sectioned sebaceous gland (220x) Figure 5.5a Sebaceous (oil) Glands • • • • • Central cells – accumulate oil lipids Engorged – burst Holocrine glands Develop from hair follicles Sebum secreted into follicle – softens and lubricates hair and skin – Slows water loss from skin – Bactericidal- bacteria killing • Secretion - stimulated by hormones (androgens) activated during puberty Sebaceous (oil) Glands • When blocked – white head • When material inside oxidizes – becomes a blackhead • Acne – active inflammation of sebaceous glands • Bacterial infection – staphylococcus • Cradle cap – infants – seborrhea – fast flowing sebum Hair and Hair Follicles • Millions on skin except – palms, soles, nipples, and external genitalia (some parts) • Warmth – mammals - ours less luxuriant and useful • Main function – sense insects • Hair on scalp – prevent physical trauma, heat loss, and sunlight • Eyelashes – shield eyes • Nose Hairs – filter large particles Structure • • • • • Hair (pili) Flexible strands Produced by hair follicles Consist largely of dead keratinized cells Hard keratin – 2 advantages 1. Tougher and more durables 2. Individual cells do not flake off Follicle wall Hair shaft Arrector pili Sebaceous gland Hair root • Connective tissue root sheath • Glassy membrane • External epithelial root sheath • Internal epithelial root sheath Hair • Cuticle • Cortex • Medulla (a) Diagram of a cross section of a hair within its follicle Hair bulb Figure 5.6a Follicle wall • Connective tissue root sheath • Glassy membrane • External epithelial root sheath • Internal epithelial root sheath Hair Hair shaft Arrector pili Sebaceous gland Hair root • Cuticle • Cortex • Medulla (b) Photomicrograph of a cross section of a hair and hair follicle (250x) Hair bulb Figure 5.6b Structure - Hair • Regions 1. Shaft – portion in which keratinization is complete, extends halfway into skin 2. Root – keratinization ongoing, portion of hair deep in follicle - Shape - Flat ribbon-like – hair kinky Oval – silky and wavy Perfectly round – straight and coarse Structure - Hairs • 3 layers – 1. Medulla– central core - Large cells, air spaces Contains soft keratin 2. Cortex – bulky layer - Surrounding medulla Several layers of flattened cells 3. Cuticle – outer layer - Single layer of cells that overlap each other Most heavily keratinized Tends to wear away at tip – keratin fibrils – frizz out, spilt ends Hair Pigment • • • • Made by melanocytes Transferred to cortical cells Different colors – yellow, rust, brown, black Red hair – colored by iron containing pigment – trichosiderin • Gray or white – decrease in melanin in production Structure of Hair Follicle • • • • • • • • • • • Folded down from epithelial surface into dermis May extend to hypodermis ~ 4 mm below skin Hair – bulb – expanded region at base Hair follicle receptor – (hair plexus) Wraps around bulb Hair papilla – dermal tissue that protruded into hair bulb Knots of capillaries – supply blood Wall – connective tissue root sheath Thickened basement membrane – glassy membrane Epithelial root sheath – invagination of epidermis Hair shaft Arrector pili Sebaceous gland Hair root Hair bulb Follicle wall • Connective tissue root sheath • Glassy membrane • External epithelial root sheath • Internal epithelial root sheath Hair root • Cuticle • Cortex • Medulla Hair matrix Hair papilla Melanocyte Subcutaneous adipose tissue (c) Diagram of a longitudinal view of the expanded hair bulb of the follicle, which encloses the matrix Figure 5.6c Structure of Hair Follicle • Hair Matrix – actively dividing area of hair bulb • Originate in hair bulb • New cells produced, older cells pushed out • Arrector pili – smooth muscle • Contraction pulls hair upright • Dimples skin – goose bumps Follicle wall • Connective tissue root sheath • Glassy membrane • External epithelial root sheath • Internal epithelial root sheath Hair root • Cuticle • Cortex • Medulla Hair matrix Hair papilla Subcutaneous adipose tissue Hair shaft Arrector pili Sebaceous gland Hair root Hair bulb (d) Photomicrograph of longitudinal view of the hair bulb in the follicle (160x) Figure 5.6d Types of Hair • Vellus hair – pale, fine hair – body hair of children and women • Terminal Hair – coarse, long hair – Eyebrows and scalp – Puberty – terminal appear is auxiliary and pubic regions (both sexes), face and chest (male) Hair Growth • Dependent on - Nutrition and hormones • Poor nutrition = poor hair growth • Increased dermal blood flow – chronic physical irritation = increased hair growth • Undesired Hair growth – eliminated by electrolysis • Excessive hairiness in women – Hirsutism – can be from adrenal gland or ovarian tumor that secretes large amounts of androgens Rate of Growth • Varies • Average ~ 2.5 mm/week • Growth cycles – 1. Active phase 2. Regressive phase 3. Resting phase Rate of Growth • Scalp – active 6 – 10 years before inactive for a few months • Average – 90 hairs lost a day • Eyebrows are only active for ~ 3-4 months Hair Thinning/Baldness • Growth fastest – teens 40 years old - then slows • Hairs not replaced as fast as they are shed – Alopecia • True or frank baldness – Male pattern baldness – genetically determined, sex influenced condition • Delayed action gene and changes in response of hair follicles to DHT • Follicular growth very short • Minoxidial – drug that reduces BP, found to stimulate hair growth • Finasteride – pill – must take everyday or new hair falls out Hair Thinning/Baldness • Thinning – can be caused by: – – – – High fever Surgery Emotional trauma Drugs – excessive vitamin A • Antidepressants • Anabolic steroids • Chemotherapy drugs – Also protein deficiency or lactation – Alopecia Areata – condition where immune system attaches follicles and hair falls out – Burns and radiation – can also cause permanent hair loss Nails • • • • • • Scale like modification of epidermis Clear protective covering Correspond to hooves/claws of other animals Tools – pick up and scratch Hard keratin Free edge, body, and root Lateral nail fold Lunule (a) Free edge Body of nail of nail Eponychium (cuticle) Nail bed Proximal nail fold Root of nail Nail matrix (b) Hyponychium Phalanx (bone of fingertip) Figure 5.7 Nails • Nail bed – epidermis below nail • Nail Matrix – proximal part of nail bed, responsible for nail growth • Pink – because of capillaries under dermis • Lunule – little moon – white crescent • Borders – overlapped by skin folds • Cuticle (eponychium) – proximal fold • Hyponychium – region below free nail, accumulates dirt Nails • Yellow nails – indicate a respiratory or thyroid disorder • Thickening and yellow – fungal infection • Outward concavity – iron deficiency • Horizontal lines – beaus lines – malnutrction Functions of Integument System • Protection • 3 types 1. Chemical Barrier – skin secretions and melanin - Low pH – acid mantle – retards bacteria growth - Seat/bacterialcide substances kill bacteria - Defensins – natural antibiotics secreted by skin - Cathelicidins – wounded skin secretes to prevent infection - Melanin – protects against UV radiation Functions of Integument System • Protection 2. Physical/Mechanical barriers – continuity of skin - Hardness of keratinized cells - Water resistant – glycolipids – block diffusion of water Functions of Integument System • Protection 2. Physical/Mechanical barriers (cont) - Some substances can penetrate skin – 1. 2. 3. 4. 5. 6. - Lipid soluble – oxygen, carbon dioxide, vitamin A, D, E, & K. and steroids Oleoresins - poison ivy/poison oak Organic solvents – acetone, paint thinner, etc. Salts of heavy metals – lead and mercury Selected drugs – nitroglycerine and nicotine Drug agents – penetration enhancers, ferry other drugs into body Enhanced by alcoholic drinks Metals and organic solvents – can be lethal and can cause kidneys to shut down Also brain damage Lead – anemia and neurological affects Functions of Integument System • • • • • Protection Biological Barriers – Dendritic cells – present antigens to WBCs Macrophages – attack viruses and bacteria DNA – chemical sunscreen, electrons absorb UV radiation, convert it to harmless heat Functions of Integument System • Body temperature Regulation – • 31- 32 C – external – Sweat glands will produce ~ 500 ml of sweat a day - Insensible perspiration • Body temperature increase – NS stimulates blood vessels to dilate and sweat glands to secrete – Loss can be up to 12 L/day – sensible perspiration Functions of Integument System • Cutaneous Secretion – • Cutaneous sensory receptors – • Exteroceptors – respond to stimuli outside the body • Meissners Corpsules and tactile discs – feel of clothing • Pacinian or purcles – bumps/contact involving deeper pressure • Free nerve endings – painful stimuli, irritating chemicals or extreme heat or cold Functions of Integument System • Metabolic Functions – • Sunlight – vitamin D precursor – converted to vitamin D, role in calcium metabolism • Keratinocyte Enzymes – 1. ‘disarm” cancer causing chemicals 2. Convert chemicals to carcinogens 3. Activate steroid hormones: cortisol hydroxycortisone - Skin makes biologically important proteins collagenase Functions of Integument System • • • • Blood reservoir – Extensive and can hold large amounts of blood ~ 5% of total blood volume Constriction – moves blood to other organs that need it Functions of Integument System • Excretion – • Limited amounts of nitrogen containing wastes – ammonia, uric acid, urea • Perfect sweating – water and salt Homeostatic Imbalances • More than 1000 different conditions and aliments • Bacterial, viral or yeast infections • Cancer and burns Homeostatic Imbalances • • • • • Skin Cancer – 1 in 5 Americans Most are benign and do not spread Wart – neoplasm caused by a virus UV light – another risk factor – Damages DNA bases – Adjacent bases fuse, forming lesions – dimers – Also disables tumor suppressor gene p 53 • Sunburn – increases production of Fas – a protein that causes genetically damaged skin cells to commit suicide, skin pealing after sunburn – Damages DNA bases – Adjacent bases fuse, forming lesions – dimers – Also disables tumor suppressor gene p 53 Homeostatic Imbalances – Skin Cancer • Skin lotions – fix damaged DNA before cells develop into cancer cells • Contain oily vesicles – liposomes – enzymes that initiate repair of DNA mutation Homeostatic Imbalances – Skin Cancer • • • • • • • • • • Basal Cell Carcinoma – Least malignant Most common 80 % of skin cancers Stratum basal cells proliferate – invade dermis and hypodermis Lesions occur most often in face Shinny dome shaped nodules Later develop an ulcer Slow growing Surgical excision Homeostatic Imbalances – Skin Cancer • Squamous Cell Carcinoma • 2nd most common • Arises from keratinocytes of stratum spinosium • Scaly red papule • Small, rounded elevation • Most often on head and hands • Grows rapidly and metastasize if not removed Homeostatic Imbalances – Skin Cancer • • • • • • • • • • • • • Melanoma – Cancer of melanocytes Most dangerous Highly metastatic Resistant to chemo 2 – 3 5 of all skin cancer Increase rapidly Most occur spontaneously 1/3 develop in persisting moles Spreading brown to black patch Early detection needed If over 4 mm thick – survival poor Surgical removal and immunotherapy Homeostatic Imbalances – Skin Cancer • ABCD Rule – • A. Asymmetry – 2 sides don’t match • B. Border irregularity – borders exhibit indentations • C. Color – several colors – blacks, browns, tans, blues, reds • D. Diameter – larger than 6 mm in diameter – pencil eraser • Some want to add • E. elevation – elevation above skin Homeostatic Imbalances – Burns • Burns – • Tissue damage, inflicted by intense heat, electricity, radiation, or certain chemicals • Denatures cell proteins • Causes cell death • Immediate threat – loss of body fluids renal shut down shock • Rules of 9s – body divided into 11 areas – Each 9% of total area – Genitals – remaining 1 % Totals 4 1 /2 % Anterior and posterior head and neck, 9% Anterior 4 1 /2 % trunk, 18% Anterior and posterior upper limbs, 18% 4 1 /2 % Anterior and posterior trunk, 36% 9% 9% (Perineum, 1%) Anterior and posterior lower limbs, 36% 100% Figure 5.9 Homeostatic Imbalances – Burns • Supplement nutrients – extra calories to replace damaged tissue • After initial crisis passed – infection and sepsis next threats • Bacterial, viral, and fungal infections Homeostatic Imbalances – Burns • Classified according to severity: 1st degree burn – only epidermis is damaged. - Localized redness, swelling, and pain 2nd degree burn – epidermis and upper regions of dermis - blisters, red painful 3rd degree burn – full thickness of skin - Gray white/cherry red/blackened - Not painful – nerve endings destroyed - Skin graft needed – living bandage - Graft takes – extensive scar tissue 1st degree burn 3rd degree burn 2nd degree burn (a) Skin bearing partial thickness burn (1st and 2nd degree burns) Skin bearing full thickness burn (3rd degree burn) Homeostatic Imbalances – Burns • • • • Critical if – Over 25 % of body – 2nd degree burns Over 10 % - 3rd degree burns 3rd degree burns on head, face, and feet Developmental Aspects of Integumentary System • • • • • • • • Epidermis develops from embryonic ectoderm Dermis and hypodermis develop from mesoderm By the end of the 4th month – skin fairly well formed During 5th and 6th month fetus is covered with delicate colorless hairs – lanugo coat Shed by the 7th month, vellus hairs make appearance Baby born – vernix caseosa – white substance produced by sebaceous glands Infancy and childhood – skin thickens Older – skin thins