Pneumonia - BobSheppard.com
advertisement

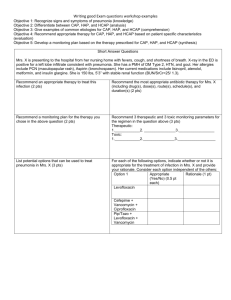
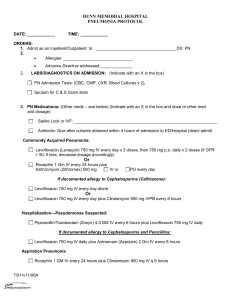
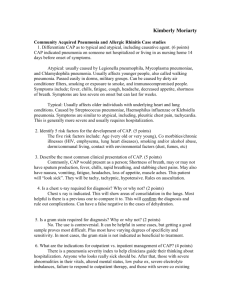
Pneumonia Charles B. Lehman, MD College of Community Health Sciences University of Alabama Diagnosing pneumonia Clinical evaluation Chest x-ray with or without microbial testing Clinical evaluation Common clinical features: Cough Fever Pleuritic chest pain Dyspnea Sputum production GI: nausea, vomiting, diarrhea Mental status changes Clinical evaluation Physical exam: 80% will be febrile Tachypnea, especially in elderly patients Tachycardia Audible crackles Evidence of consolidation Lab findings: Leukocytosis with left shift Leukopenia can occur and is an ominous sign Clinical evaluation: chest x-ray Radiologic evaluation Presence of infiltrate on plain chest x-ray is gold standard for diagnosis Should be obtained whenever diagnosis is suspected Recommendations less clear when viral infection suspected but should be obtained in patients with an abnormal vital sign, especially tachypnea. Lobar consolidation Left lower lobe opacity in patient with pneumococcal pneumonia. Interstitial infiltrates Nodular opacities in the right lower lobe in patient with mycoplasma pneumonia. Cavitation Lung abscess with air-fluid level in right lung in first image. Next image is of necrotizing pneumonia in the left lung Clinical evaluation: chest x-ray Considerable variation in reading between different radiologists Even more between ED physicians and radiologists High-resolution CT is a much better test but generally not necessary to make a diagnosis. Clinical evaluation: chest x-ray Other causes for chest x-ray which can look like pneumonia Malignancy Hemorrhage Pulmonary edema Pulmonary embolism with infarction Inflammation due to non-infectious causes CT can be used to clarify cases when clinical picture is consistent with pneumonia but chest x-ray is negative. Clinical evaluation: microbial testing Outpatients: testing is optional Hospitalized patients with specific indications should have blood cultures and sputum Gram stain and culture. Severe CAP requiring ICU admission should have blood cultures, Legionella and pneumococcus urinary antigen tests and sputum culture. Other tests indicated with specific findings Clinical evaluation: microbial testing Blood cultures Blood cultures are positive in 7 to 16% of hospitalized patients with S. pneumococcus accounting for 2/3 of positive cultures. Arguments to obtain blood cultures: Establishes a diagnosis when likely pathogen found In many cases is the only test done and is primary source for microbiologic data for many hospitals Isolates are an important resource for tracking resistance patterns in S. pneumoniae which provide data for evaluating vaccines. Arguments against: Relatively low rate of positives Rarely lead to modification of therapy Clinical evaluation: microbial testing Sputum cultures Sputum cultures ICU admission Failure of antibiotic therapy Cavitary lesions Active alcohol abuse Severe obstructive of structural lung disease Immunocompromised host Pleural effusion Epidemic pneumonia Clinical evaluation Predisposing conditions Altered mental status which can lead to micro/macro aspiration (stroke, seizure, intoxication, anesthesia) Smoking Alcohol Hypoxemia Acidosis Toxic inhalations Pulmonary edema Uremia Malnutrition Clinical evaluation: predisposing conditions Immunosuppresive agents Mechanical obstruction of a bronchus Advanced age Cystic fibrosis Bronchiectasis COPD HIV Viral respiratory tract infection, especially influenza Lung cancer Microbiology: bacteria S. pneumoniae: most common cause H. influenzae: more common in elderly and patients with underlying pulmonary disease (COPD, cystic fibrosis) M. pneumoniae: most common atypical cause, highest rates in school-aged children, military recruits and college students. C. pneumoniae Legionella: transmitted by aerosols containing the bacteria such as showers, grocery store misters, cooling towers, whirlpool spas and fountains. Microbiology: bacteria Gram negative bacilli E. coli Serratia K. pneumoniae Acinetobacter P. aeruginosa Enterobacter Uncommon in CAP except in patients with severe disease requiring ICU admission Microbiology: bacteria S. aureus Usually in older adults or younger patients who are recovering from influenza Associated with severe necrotizing pneumonia Group A streptococcus Can cause fulminant pneumonia with early empyema even in young competent hosts. Anaerobes (aspiration and lung abscess) Neisseria meningitidis M. tuberculosis Microbiology: viruses Influenza Can cause primary pneumonia, more likely to cause secondary bacterial pneumonia Parainfluenza viruses RSV Adenovirus Human metapneumovirus Severe acute respiratory syndrome (SARS) Middle East respiratory syndrome coronavirus (MERS-CoV) Other coronaviruses Microbiology: viruses Hantavirus (ARDS) Avian influenza: considered a possible source for next global influenza pandemic. Varicella Microbiology: fungi Usually occur in immunocompromised hosts Neutropenia Immunosuppressive therapy HIV Usually endemic to particular areas Microbiology: fungi Cryptococcus Found world-wide Infection often asymptomatic in immunocompetent hosts Histoplasma Most common in Ohio and Mississippi River valleys Less than 5% develop symptoms with low-level exposure Coccidioides (Sonoran desert regions) Aspergillosis P. jirovecii Microbiology: bioterrorism Bacillus anthracis (anthrax) Yersinia pestis (plague) Francisella tularensis (tularemia) C. burnetti (Q fever) Inpatient vs. outpatient treatment Hospital admission rates vary widely Rates often are not related to local disease severity Physicians often overestimate patient risk of short-term mortality Many unnecessary admissions as a result Inpatient vs. outpatient treatment Pneumonia Severity Index Step 1 risk factors: Age > 50 Coexisting conditions: cancer, CHF, cerebrovascular disease, renal disease or liver disease Physical exam: AMS, heart rate >= 125, respiratory rate >= 30, SBP < 90, temperature < 35 (95) or > 40 (104) If one or more Step 1 risk factors are present then evaluation proceeds to Step 2. Inpatient vs. outpatient treatment Pneumonia Severity Index Class I: no predictors Class II: <= 70 Class III: 71–90 Class IV: 91-130 Class V: > 130 PSI and mortality by class Class Points Mortality I No predictors 0.1 II <= 70 0.6 III 71-90 0.9 IV 91-130 9.3 V > 130 27.0 Inpatient vs. outpatient treatment Pneumonia Severity Index Measuring impact using Pneumonia PORT cohort Strategy 1: outpatient therapy for class I or II, brief observation for class III and admission for class IV or V: 31% fewer admissions 19% more would have been assigned to observation 4.3% admitted to ICU < 1% mortality Inpatient vs. outpatient treatment Pneumonia Severity Index Measuring impact using Pneumonia PORT cohort Strategy 2: same as strategy 1 except that all patients with hypoxemia were admitted: 26% reduction in admissions 13% assigned to observation 1.6% admitted to ICU Mortality < 1% Either set of recommendations would have recommended inpatient therapy for 5 of the 6 patients who died following an initial course of outpatient therapy. Inpatient vs. outpatient treatment Pneumonia Severity Index CAPITAL trial (Canada) Admission rate for low risk (class I, II or III) patients dropped from 49 to 31% No negative effects on patient quality of life or adverse medical outcomes (ICU admission, mortality, readmission or complications). EDCAP (US) Increased proportion of low-risk patients treated in outpatient setting No statistically significant difference in safety outcomes Inpatient vs. outpatient treatment CURB-65 score Confusion Urea (BUN > 20) Respiratory rate (>30) Blood pressure (SBP < 90 or DBP < 60) Age > 65 0-1: outpatient treatment 2: admission >= 3 should be assessed for ICU admission Inpatient vs. outpatient treatment Severe CAP score Major criteria: pH < 7.30 (13 points) SBP < 90 (11 points) Minor criteria: RR > 30 (9) PaO2/FiO2 < 250 (6) BUN > 30 (5) Age > 80 (5) Multilobar/bilateral infiltrates (5) Score > 10 predicts progression to severe CAP CAP: outpatient treatment Empiric therapy Chest x-ray which demonstrates pneumonia Risk stratification with CURB-65 or PSI Distinguish CAP from HCAP Microbiologic testing is optional Blood cultures Sputum if quality sample can be obtained CAP: outpatient treatment Empiric therapy Co-morbidity Alcoholism COPD Post-CVA aspiration Post-obstruction of bronchi Influenza Local resistance of S. pneumoniae to macrolides > 25% CAP: outpatient treatment Empiric therapy No co-morbidities, local macrolide resistance < 25% Azithromycin 500 x 1 dose then 250 mg/day Clarithromycin 500 mg BID for 7 days If patient had antibiotics within 3 months: Above plus amoxicillin 1 gm TID or Augmentin 1000/62.5 2 tabs BID Levofloxacin 750 mg qD If co-morbidity present: Levofloxacin 750 mg qD x 5 days CAP: inpatient treatment Non-ICU patients S. pneumoniae most common pathogen Respiratory viruses Less common: M. pneumoniae H. influenzae C. pneumoniae Legionella CAP: inpatient treatment Non-ICU patients Primary regimens: Ceftriaxone 1 gm q24 + azithromycin 500 mg q24 Ertapenem 1 gm q24 + azithromycin 500 mg q24 Alternative regimens: Levofloxacin 750 mg q24 Moxifloxacin 400 mg q24 CAP: inpatient treatment Non-ICU patients with COPD Primary regimens: Levofloxacin 750 mg q24 Moxifloxacin 400 mg q24 Alternative regimens: Ceftriaxone 1 gm q24 + azithromycin 500 mg q24 Ertapenem 1 gm q24 + azithromycin 500 mg q24 CAP: inpatient treatment Empiric therapy, ICU patients Patients admitted to an ICU are more likely to have resistant pathogens including community-associated MRSA and Legionella Suspicion for P. aeruginosa Chronic or structural lung disease Known prior colonization Suspicion for CA-MRSA Post-influenza IV drug use Gram (+) cocci in clusters on Gram stain CAP: inpatient treatment Empiric therapy, ICU patients Primary regimens: (Ceftriaxone 1-2 gm q24 or Unasyn 3 gm q6) + azithromycin 500 q24 Levofloxacin 750 mg q24 Moxifloxacin 400 q24 If CA-MRSA suspected add: Vancomycin 15-20 mg/kg q8-12 Linezolid 600 IV q12 CAP: inpatient treatment Empiric therapy, ICU patients If P. aeruginosa suspected: Beta-lactam (Cefepime 2 gm q12 or Zosyn 3.375 gm q4 or ceftazidime 2 gm q8 or meropenem 1 gm q8) Fluoroquinolone (levofloxacin 750 q24 or ciprofloxacin 400 q8) or tobramycin 5 mg/kg q24 and azithromycin 500 q24 CAP: inpatient treatment Response to therapy Some improvement usually seen within 48 to 72 hours Resolution of symptoms and radiographic findings takes longer Crackles can persist for weeks As many as 87% of patients continue to report at least one symptom at 39 days Takes 6-8 weeks for a chest x-ray to clear and can take up to 12 weeks in patients with underlying lung disease CAP: inpatient treatment Change to oral therapy Clinical improvement Hemodynamically stable Normally functioning GI tract CAP: inpatient treatment Choice of oral therapy Base on culture results if possible Use oral medications from same drug class No need to cover for S. aureus or gram (-) bacilli unless isolated from a good quality sputum specimen Choice depends on risk of resistant S. pneumoniae and the initial IV regimen CAP: inpatient treatment Duration of hospitalization Can go home when: On oral medications No other active medical problems Appropriate environment for discharge Not necessary to keep patient for observation after changing to oral antibiotics. CAP: inpatient treatment Duration of therapy Minimum of 5 days Should be afebrile for 48 hours No more than 1 clinical instability factor Heart rate > 100 Respiratory rate > 24 SBP < 90 CAP: inpatient treatment Duration of therapy Longer duration needed if: Initial therapy was not active against a subsequently identified pathogen Extrapulmonary infection identified (meningitis, endocarditis) P. aeruginosa, S. aureus or Legionella infections Necrotizing pneumonia, empyema or lung abscess CAP: inpatient treatment Non-responding patients Progressive pneumonia or clinical deterioration Requirement of ventilator support Development of septic shock Absence of delay of achieving clinical stability after 72 hours CAP: inpatient treatment Non-responding patients Unusual organisms not covered by empiric therapy Patient-related factors Severity of illness Neoplasia Aspiration pneumonia Neurologic disease Infectious complications Empyema Superimposed nosocomial pneumonia HAP, VAP and HCAP Hospital-acquired (nosocomial) pneumonia Ventilator-associated pneumonia 48 hours or more after admission, did not appear present on admission 48-72 hours after endotracheal intubation Healthcare-associated pneumonia IV therapy, wound care or IV chemotherapy within 30 days Residence in a nursing home or other long-term care facility Hospitalization in an acute care hospital for 2 or more days within the last 90 days Attendance at a hospital or hemodialysis clinic within 30 days HAP, VAP and HCAP Drug selection should be based on risk factors for multi-drug resistant organisms Recent antibiotic therapy Resident flora in the hospital or ICU Presence of underlying diseases Available culture data HAP, VAP and HCAP MRSA Vancomycin or linezolid should be added Should be discontinued if not isolated in cultures If MSSA later isolated should replace above with nafcillin or oxacillin HAP, VAP and HCAP Other considerations Combination therapy for Gram (-) organisms often used but no conclusive evidence to support this practice Legionella should be covered, especially if known to be present in the hospital water supply Anaerobes in patients with recent abdominal surgery or aspiration HCAP Etiologies S. aureus (often MRSA) Gram (-) enterics which may be MDR (E. coli, K. pneumoniae, enterobacter, Serratia) P. aeruginosa Acinetobacter HCAP Empiric treatment Vancomycin 15-20 mg/kg q8-12 Cefepime 2 gm 12 or Zosyn 4.5 gm q6 or meropenem 1 gm q8 Doripenem should not be used Linezolid 600 IV q12 can be substituted for vancomycin If Legionella suspected should use a fluoroquinolone or add azithromycin 500 mg q24 HCAP Empiric treatment Controversy exists regarding uniqueness of HCAP Duration of therapy is not well-defined Therapy should be streamlined once culture results area available HAP/VAP Subtypes Early-onset: no other risk factors for MDR, < 5 days in the hospital S. pneumoniae, S. aureus, H. influenzae, enteric Gram (-) bacilli Late onset: >= 5 days in the hospital, risk factors for MDR organisms S. aureus, often MRSA Gram (-) enterics ESKAPE organisms (E. coli, Serratia, Klebsiella, acinetobacter, pseudomonas and enterobacter) etiology in about 80% of patients HAP/VAP Early-onset Ceftriaxone 1 gm q24 or Unasyn 3 gm q6 or Ertapenem 1 gm q24 or Levofloxacin 750 q 24 HAP/VAP Late-onset Meropenem 1 gm q8, Zosyn 4.5 gm q6 or cefepime 2 gm q12 Add vancomycin 15-20 mg q8-12 if MRSA suspected Imipenem preferred over meropenem if acinetobacter is suspected Add levofloxacin if Legionella suspected