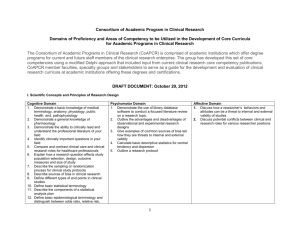
Investigator
advertisement

Responsibilities of Investigator Kamila Novak Investigator’s Responsibilities Medical Care of Trial Subjects Communication with IRB/IEC Safety Reporting Essential documents Adequate Resources Compliance to GCP and reg. requirements IP Protocol Compliance Informed Consent Site Noncompliance Source documents Records and reports Adequate Resources Adequate resources Adequate number of qualified staff, adequately informed about the protocol, IP and their duties Sufficient Time (competing trials) Motivation Adequate facilities Adequate equipment and support functions ICH GCP Chapter 4.2 Potential for recruiting the required number of suitable subjects Medical Care Medical care • A qualified physician (or dentist), who is an investigator or a sub-investigator, should be responsible for all trial related medical (dental) decisions • Investigator should ensure that adequate medical care is provided to a subject for ANY adverse events, including clinically significant laboratory values • With subject’s agreement it is recommended for the investigator to inform the subject’s primary physician about the subject’s participation in the trial • Investigator should make a reasonable effort to ascertain the reason for subject’s withdrawing prematurely from a trial ICH GCP Chapter 4.3 Сompliance with GCP Compliance with GCP Investigator should: Be aware of and should comply with GCP and the applicable regulatory requirements ICH GCP Chapter 4.1.3 Сompliance with Protocol Compliance with protocol Investigator should: Review the protocol Be thoroughly familiar with the IP as described in the protocol, current Investigator’s Brochure, and the product information ICH GCP Chapter 4.1.2 Two Roles: Physician and Investigator Routine Medical Care Conduct of a Clinical Trial Person with symptoms is looking for physician to diagnose and treat the illness Investigator is looking for subjects with diagnosis eligible for the clinical trial Physician collects and reviews, per medical practice, relevant information to make a diagnosis Investigator collects and reviews, per protocol, relevant info to select eligible subjects Physician makes diagnosis and gives standard treatment/therapy of choice Investigator enters eligible subject into trial and is obliged to give IP per protocol Two Roles: Physician and Investigator Routine Medical Care Conduct of a Clinical Trial Physician may change dose, route, administration of drug or drug itself and allow concomitant medication according to standard treatment Investigator follows protocol for dose, route and administration of IP and use of concomitant medication may be restricted Physician performs examinations and procedures to determine Diagnosis and evaluates outcome of treatment Investigator performs examinations and procedures per protocol to obtain data for efficacy and safety evaluation of IP Physician determines schedule of events for each patient Investigator follows schedule of events per protocol Treatment ends when satisfactory outcome is achieved Subject participation in trial is complete per protocol Compliance with Protocol Compliance with protocol The Investigator should sign the protocol (signature page) to confirm his/her agreement to conduct the trial in compliance with the approved protocol The Investigator should not implement any deviation from the protocol without agreement of the sponsor and prior review and approval/favourable opinion of the IRB/IEC ICH GCP Chapter 4.5.1, 4.5.2 Compliance with Protocol • Where necessary to eliminate an immediate hazard to trial subjects • When changes involve only logistical or administrative aspects The investigator should • document and explain any deviation from the protocol • document, explain and report such deviation to IRB/IEC for review and approval to sponsor for review ICH GCP Chapter 4.5.2, 4.5.3 Noncompliance Noncompliance Noncompliance with protocol, SOPs, GCP and/or applicable regulatory requirements If serious and/or persistent Noncompliance is identified by auditors and/or monitor Sponsor should act promptly to secure compliance (e.g. corrective action plan) Sponsor should terminate investigator’s participation Sponsor should notify RA promptly ICH GCP Chapter 5.20 Deviations from Protocol Reports to IRB/IEC Deviations from, or changes of the protocol to eliminate immediate hazards to trial subjects Changes increasing the risk to subjects and/or affecting significantly study conduct All adverse drug reactions that are both serious and unexpected New information that may affect No deviation from, or change of protocol without sponsor’s agreement, IEC/IRB approval *** except when necessary to eliminate an immediate hazard(s) to subjects or in case of administrative changes adversely the safety of subjects ICH GCP Chapter 3.3.8, 4.5.4 Informed Consent (IC) of Trial Subjects The voluntary confirmation of a subject’s Informed Consent willingness to participate in a particular trial, after having been informed of all aspects of the trial relevant to his/her decision to participate in the trial Documented by means of a written, signed and dated informed consent form (by subject and investigator) Informed Consent Form Signature ICH GCP Chapter 1.28 Date Investigator’s Responsibilities • • • • Consent the subject prior to participation in a trial and before ANY trial procedure, including blood tests for screening unless it’s part of normal clinical practice Ensure the subject is fully informed Ample time and opportunity to ask questions must be given Should not unduly influence a subject to participate ICH GCP Chapters 4.8.8, 4.8.5, 4.8.7, 4.8.3 Investigator’s Responsibilities • • • • Document the consent procedure in source documents Give the subject a copy of the signed and dated ICF Obtain written approval from IEC/IRB on ICF and all changes to ICF Ensure the language is understandable to the subjects ICH GCP Chapter 4.8.11, 4.8.1, 4.8.2, 4.8.6 “Special” ICF Procedures • Witnessed consent by impartial witness ◦ e.g., if subject is unable to read • Legally acceptable representative ◦ e.g., pediatric trials, mentally ill subjects • Emergency situations ◦ e.g., unconscious subjects ICH GCP Chapter 4.8.9, 4.8.15 Vulnerable subjects Individuals whose willingness to volunteer is influenced by the expectation of benefits of participation, or of response from senior members of hierarchy: * medical students disease * hospital/laboratory personnel homes * armed forces * people under detention * patients in emergency cases * ethnic minorities * patients with incurable * persons of nursing * unemployed/homeless * pharmaceutical industry employees * incapable to give IC ICH GCP Chapter 1.61 Investigational Product IP A pharmaceutical form of an active ingredient or placebo being tested or used as a reference in a clinical trial, including a product with a marketing authorization when used or assembled (formulated or packaged) in a way different from the approved form, or when used for an unapproved indication, or when used to gain further information about an approved use ICH GCP Chapter 1.33 IP – Investigator Responsibilities • Receipt of IP only by authorised staff IP IP • Dispensing, handling and appropriate use of IP according to protocol • IP given only to trial subjects, used package and unused IP returned • Explanation of the correct use of IP to each subject to ensure compliance with protocol • Storage as specified by the sponsor (temperature regimen, proper conditions/times) • Secure, safe and appropriate storage with limited access by investigator and authorised staff ICH GCP Chapter 4.6.2, 4.6.6, 4.6.4, 4.6.3 IP – Records at the Site Maintain records of IP delivery, inventory, use by IP IP each subject and the return to sponsor/destruction Dates and amounts received from sponsor Confirmation IP received by authorised person Dates and amounts dispensed to/used by patients Dates and amounts returned to sponsor Expiry dates (if applicable) Unique code numbers assigned Doses used by subjects IP accountability - RECEIVED = USED + UNUSED ICH GCP Chapter 4.6.3 IP – Randomization & Unblinding IP Investigator should: IP follow the trial’s randomization procedures ensure that the code is broken only in accordance with the protocol promptly document and explain to the sponsor any premature unblinding ICH GCP Chapter 4.7 IP - Flow of Events Investigational Product Q/sponsor/vendor Received at Site IP receipt docs IP dispensed to subjects IP accountability docs IP returned by patient IP returned to sender Destruction of IP IP Reconciliation docs Adverse Event Safety reporting Any untoward medical occurrence in a patients or clinical investigation subject administered a pharmaceutical product that does not necessarily have a causal relationship with this treatment ICH GCP Chapter1.2 Why Are AEs Important? Medical Reasons Regulatory Reasons Adverse Event-Recording Adverse Event Page in the CRF ! All AEs must be assessed by investigators and documented in the source documents first and then transferred to CRF ! ICH GCP Chapter 4.9.2 Adverse Event Page Protocol: Site Nr: Subject Initials: Visit Nr: Subject Nr: Visit Date: Adverse Duration Intensity/ Causality Event Severity Investigator: Randomisation Nr: Trial Drug Treatm. given Outcome Seriousness Investigator Signature ____________________ Date ___________________ Recording AEs What information is generally collected: - Adverse Event - Dates of Onset and Resolution - Severity: Mild = aware but tolerable Moderate = interferes with activities Severe = unable to do normal activities - Causality: Not related Unlikely Possible Probable (AE stops when drug stopped) Highly probable (AE stops when drug stopped and restarts when drug is reintroduced) Recording AEs What information is generally collected: - Outcome Resolved Resolved with sequelae Ongoing Death - Action Taken with Study Drug (dose) None Reduced or increased Interrupted (means temporarily) Discontinued (means permanently) - Requirement for Treatment – Concomitant Medication - Seriousness Adverse Drug Reaction (ADR) New medicinal product Marketed medicinal product A causal relationship between a medicinal product and an adverse event is at least a reasonable possibility, i.e. the relationship cannot be ruled out May occur at ANY DOSE! A response to a drug which is noxious and unintended and which occurs at doses normally used in man for prophylaxis, diagnosis, or treating diseases or for modification of a physiological function ICH GCP Chapter1.1 Unexpected Adverse Drug Reaction (UADR) An adverse reaction, the nature and severity of which is not consistent with the applicable product information ICH GCP Chapter1.60 Serious Adverse Event (SAE) Any untoward medical occurrence that at any dose results in: death life-threatening inpatient hospitalization or prolongation of existing hospitalization persistent or significant disability/incapacity congenital anomaly/birth defect ICH GCP Chapter 1.50 Planned Hospitalization • Per project requirements, a hospitalization planned prior to a subject’s inclusion in the trial might not be considered an SAE • If a hospitalized subject has an AE that prolongs that hospitalization, then that AE would become an SAE Pregnancy and Subjects Most sponsor companies will request that all pregnancies are reported in the same way as serious adverse events i.e., immediately, and using the SAE report form or Pregnancy Notification Form Upon consent pregnancies are followed until delivery of the child Child is assessed at birth for any congenital anomaly/birth defect and possibly longer What is what? AEs ADRs UADRs SAEs Serious Adverse Event - Flowchart Episode of Myocardial Infarction Is it an Adverse Event ? YES Is it a Serious Adverse Event ? NO Y E S Notify the Sponsor/CRO Complete SAE Report Form Notify IRB/IEC and RA Complete AE Page Immediately may mean 24 hours Communication with IRB/IEC Communication with IRB/IEC Written, dated approval/favourable opinion (before initiating) Ongoing applications of trial documents (during the trial) Ongoing Safety Reporting (during the trial) Progress/annual reports (during the trial Notification about trial completion, early termination (end of the trial) ICH GCP Chapter 3.1.2, 3.1.4, 3.3.8, 4.4.1, 4.4.3, 4.10.1, 4.10.2, 4.12.1, 4.13 Prompt Reports to IRB/IEC Progress Reports • Deviations from, or changes of, the protocol to eliminate immediate hazards to the trial subjects • Changes increasing the risk to subjects and/or affecting significantly the conduct of the trial • All adverse drug reactions (ADRs) that are both serious and unexpected • New information that may affect adversely the safety of the subjects or the conduct of the trial ICH GCP Chapter 3.3.8 What are Source Documents (SD)? SDs Original documents, data and certified copies of original records necessary for trial evaluation and reconstruction ICH GCP Chapter 1.52 Source Documents Include, But Are Not Limited To.... Medical records/clinical charts/subject's file Laboratory results Subject diaries/cards Pharmacy drug dispensing records Recorded data from automated instruments ICH GCP Chapter 1.52 Source Documents Include, But Are Not Limited To.... Microfilm or magnetic media, x-rays, etc Records kept at pharmacy, at labs and medicotechnical departments Electronic records Electronic signatures ICH GCP Chapter 1.52 Case Report Form (CRF) A printed, optical, or electronic document designed to record all of the protocol required information to be reported to the sponsor on each trial subject ICH GCP Chapter 1.11 Minimum Requirements for SD Signed and dated Informed Consent form ◦ source notes indicating that the subject has signed and dated the consent prior to any study procedure Subject Identification/Demographic data ◦ Unique study identifier (screening/randomization number) Medical history including diagnosis of the condition under study Physical examination Minimum Requirements for SD (cont.) Entries for each visit including screening, scheduled, and unscheduled, to include: ◦ ◦ ◦ ◦ ◦ ◦ ◦ ◦ Dates Health status Medical observations Changes to medications with reasons IP dispensing and accountability Adverse events Efficacy measures Study procedures (both done and not done with reasons) Minimum Requirements for SD (cont.) Concomitant medication Concurrent medical conditions Reports and printouts, radiology, x-ray, laboratory, ECG, MRI, EEG, etc. Date of completion or withdrawal from study with reasons stated Follow-up Contacts with patients Investigator’s Responsibilities Consistency of CRFs with SDs Up-to-date Source Documents maintained Accuracy, completeness, legibility and timeliness of data collected, recorded and reported Source documents Follow minimum requirements for recording data in Medical Records must not be altered to match the CRF Direct access to all trial documents for monitor, auditor, IRB/IEC, RA Changes/corrections to CRFs dated, initialed Discrepancies explained (if necessary) ICH GCP Chapter 4.9.1, 4.9.2, 4.9.3 Data Correction Proper procedure for correcting CRFs ◦ Single line through error ◦ Legibly print correct data adjacent to error ◦ Initial and date correction ◦ Never back date ◦ Avoid pencil use ◦ Never use correction fluid or tape ICH GCP Chapter 4.9.3 Source Document Verification (SDV) Process of checking data consistency in the CRF with source data, performed to maintain subject safety Requirements for data consist ency: accuracy completeness explanation and documentation of discrepancies ICH GCP Chapter 5.18.4k, 5.18.4m, 5.18.4n General Reminders Source documents/data must be maintained individually for each subject and identifiable to the subject Only authorised personnel are to make entries into source documents All entries should be signed and dated by the personnel responsible for entries Essential Documents Documents which individually and Records collectively permit evaluation of the conduct of a trial and the quality of the data produced May include: • CRFs • Patients Medical Notes • SDs • Investigator Site File ICH GCP Chapter 1.23, 8.1 Retention of Essential Documents Records • At least 2 years after last Marketing Application approval in an ICH region and there are no pending or contemplated MAs in ICH regions • At least 2 years after discontinuation of clinical development • Sponsor responsible for informing investigator when no longer required ICH GCP Chapter 4.9.5