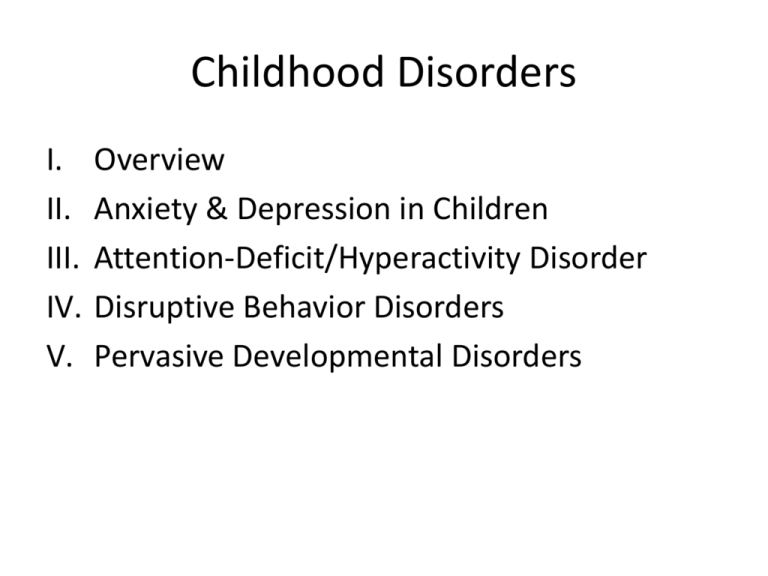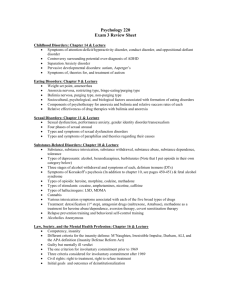
Childhood Disorders
I.
II.
III.
IV.
V.
Overview
Anxiety & Depression in Children
Attention-Deficit/Hyperactivity Disorder
Disruptive Behavior Disorders
Pervasive Developmental Disorders
I. Overview
II. Anxiety & Depression in Children
• Separation anxiety disorder
III. Attention-Deficit/Hyperactivity
Disorder
Symptoms
Symptoms (continued)
IV. Disruptive Behavior Disorders
• Oppositional Defiant Disorder
• Conduct Disorder
Conduct Disorder Symptoms
• A repetitive and persistent pattern of behavior
in which the basic rights of others or major
age-appropriate society norms or rules are
violated, with at least three of the following
present in the past twelve months (and at
least one in the past six months):
Conduct Disorder Symptoms
• Frequent bullying or
threatening of others
• Frequent provoking of physical
fights
• Using dangerous weapons
• Physical cruelty to people
• Physical cruelty to animals
• Stealing while confronting a
victim
• Forcing someone into sexual
activity
• Fire-setting
• Deliberately destroying other’s
property
• Breaking into a house, building
or car
• Frequent manipulation of
others
• Stealing items of non-trivial
value without a victim
• Frequent staying out beyond
curfews, beginning before age
13
• Running away from home at
least twice
• Frequent truancy from school,
beginning before age 13
ODD Symptoms
• The symptoms of ODD are not as severe as the
symptoms of conduct disorder but have their
onset at an earlier age, and ODD often
develops into conduct disorder.
• A pattern of negativistic, hostile, and defiant
behavior lasting at least 6 months, during
which four (or more) of the following are
present:
ODD Symptoms
• Often loses temper
• Often argues with adults
• Often actively defies or refuses to comply with
adult requests or rules
• Often deliberately annoys people
• Often blames others for his/her mistakes or
misbehavior
• Is often touchy or easily annoyed by others
• Is often angry and resentful
• Is often spiteful or vindictive
V. Pervasive Developmental Disorders
Autistic Disorder/Autism
• Lack of social interaction
• Lack of communication
• Restricted repetitive and stereotyped
behaviors, interests, and activities
Other Pervasive Developmental
Disorders
• Asperger’s disorder
• Rett’s disorder
• Childhood disintegrative disorder
• Institute for Attachment & Child Development
Eating Disorders
I.
II.
III.
IV.
V.
VI.
Introduction
Anorexia Nervosa
Bulimia Nervosa
Binge-Eating Disorder
Theories
Treatments
I. Introduction
II. Anorexia Nervosa
Symptoms
III. Bulimia Nervosa
Symptoms
IV. Binge Eating Disorder
Symptoms
• Recurrent episodes of binge eating
• Symptoms continuing, on average, at least
twice a week for 6 months
• The binge eating is not associated with
recurrent inappropriate compensatory
behavior
V. Theories
Women with
High EAT score
Women with
Low EAT score
Men
Sexual Disorders & Gender Identity
Disorder
I.
II.
III.
IV.
V.
The Sexual Response Cycle
Frequency of Sexual Behaviors
Sexual Dysfunction Disorders
Paraphilias
Gender Identity Disorder (GID)
I. The Sexual Response Cycle
II. Frequency of Sexual Behaviors
Frequency of Sexual Behaviors
Michael et al. (1994)
Learned about sex primarily from
the home
Has a sexually transmitted disease
Purchased erotic material during
the past year
Females
Thinks about sex every day
Males
Lived with spouse before marriage
Had much sexual experience
before marriage
0
10
20 30
40
50 60
Percentage who report behavior
70
What Kinds of Sexual Practices Do
People Find “Very Appealing?”
Michael et al. (1994)
Practice
Men
Women
Vaginal Intercourse
83%
78%
Watching partner undress
50%
30%
Receiving oral sex
50%
33%
Giving oral sex
37%
19%
Group sex
14%
1%
Anus stimulated by partner’s finger
6%
4%
Using dildos/vibrators
5%
3%
Watching others do sexual things
6%
2%
Having a same-gender sex partner
4%
3%
Having sex with a stranger
5%
1%
Percentage of People Who Have Had a
Sexual Difficulty in the Past Year
Michael et al. (1994)
Lacked interest in sex
Unable to orgasm
Sex not pleasurable
Experienced pain during sex
Women
Anxiety about performance
Men
Climax too early
Unable to keep an erection
Had trouble lubricating
0
5
10
15
20
25
30
35
III. Sexual Dysfunction Disorders
Disorders Involving Sexual Desire
Disorders Involving Sexual Arousal
Disorders Involving Orgasm
Disorders Involving Orgasm
Disorders Involving Sexual Pain
Causes of Sexual Disorders:
Sociocultural
• Relationship problems:
– lack of communication
– differences in sexual expectations
– conflicts unrelated to sex
• Trauma
• Cultural taboos against sex
Causes of Sexual Disorders:
Psychological
• Psychological Disorders
– Depression
– Anxiety disorders
– Schizophrenia
• Attitudes & cognitions
– Beliefs that sex is “dirty” or “disgusting”
– Performance anxiety
Causes of Sexual Disorders:
Biological
• Medical Conditions
– Diabetes
– Cardiovascular disease
– Multiple Sclerosis
– Renal failure
– Vascular disease
– Spinal cord injury
• Prescription Drugs
– Antihypertensive medications
IV. Paraphilias
Paraphilias
(Greek word for “besides love”)
• Atypical sexual activity that involves at least
one of the following:
– Non-human objects
– Non-consenting adults
– Suffering or humiliation of self or partner
– Young children
Types of Paraphilias
• Fetishism
– Tranvestism or transvestic fetishism
• Sexual Sadism and Sexual Masochism
• Voyerism*
• Exhibitionism*
• Frotteurism*
• Pedophilia*
* Diagnosed if symptoms cause significant
distress/dysfunction OR person acts on these sexual
urges
Cognitive Causes
Category
Pedophilia
Exhibitionism
Misattributing blame
“She started it by being too
cuddly.”
“She would always run
around half dressed.”
“She kept looking at me
like she was expecting it.”
The way she was dressed,
she was asking for it.”
Minimizing or denying
sexual intent
“I was teaching her about
sex… better from her
father than some one
else.”
“I was just looking for a
place to pee.”
“My pants just slipped
down.”
Debasing the victim
“She’d had sex before with
her boyfriend.”
“She always lies.”
“She was just a slut
anyway.”
Cognitive Causes
Category
Pedophilia
Exhibitionism
Minimizing consequences
“She’s always been real
friendly towards me, even
afterward.”
“She was messed up even
before it happened.”
“I never touched her so I
couldn’t have hurt her.”
“She smiled, so she must
have liked it.”
Deflecting blame
“This happened years
ago… why can’t everyone
forget about it.”
“It’s not like I raped
anyone.”
Justifying the cause
“If I wasn’t molested as a
child, I’d never have done
this.”
“If I knew how to gets
dates, I wouldn’t have to
expose.”
V. Gender Identity Disorder (GID)
Substance Related Disorders
I.
II.
III.
IV.
V.
Introduction
Diagnoses
Types of Psychoactive Substances
More on Alcohol
Treatment
I. Introduction
1848
1876
II. Diagnoses
Substance Intoxication
• Significant maladaptive behavior
• Show some of a specific list of symptoms
(which are specific to each substance)
Substance Withdrawal
• Set of physiological and behavioral symptoms
that occur when people stop using a
substance that they have been using for a
period of time (symptoms are usually the
opposite of what the substance does)
• Significant distress or dysfunction
Substance Abuse
• Repeated problems as a result of the using the
substance
• 1 or more of the following in a 1 year period:
– Failure to fulfill important obligations at work, home,
or school
– Repeated use of the substance in hazardous situations
– Repeated legal problems
– Continued use of the substance despite repeated
social and legal problems
Substance Dependence
• Closest thing in the DSM to “addiction”
• Often involves tolerance & withdrawal (if so,
often referred to as physical/physiological
dependence)
• But can be dependent without tolerance &
withdrawal (if so, often referred to as
psychological/psychic dependence)
III. Types of Psychoactive Substances
• Depressants: Alcohol, benzodiazepines, barbiturates,
inhalants (gasoline, paint thinner)
• Opioids: morphine, heroin, codeine, methadone
• Stimulants: cocaine, amphetamines, nicotine,
caffeine
• Hallucinogens: LSD, MDMA (Ecstasy), peyote (PCP
has similar effects)
• Cannabis: a.k.a. marijuana
IV. More on Alcohol
Alcohol Intoxication
• Recent ingestion of alcohol
• Clinically significant maladaptive behavior or
psychological changes (inappropriate sexual or
aggressive behavior, mood lability, impaired judgment)
• One or more of the following
–
–
–
–
–
–
Slurred speech
Incoordination
Unsteady gait
Nystagmus
Impairment in attention or memory
Stupor or coma
Alcohol Withdrawal
• Cessation of alcohol use that has been heavy and
prolonged
• Two or more of the following (within a few hours to a few
days after cessation):
–
–
–
–
–
–
–
–
Autonomic hyperactivity (sweating, HR over 100 BPM)
Hand tremor
Insomnia
Nausea or vomiting
Transient visual, tactile, or auditory hallucinations
Psychomotor agitation
Anxiety
Grand mal seizures
• Significant distress or dysfunction
Long-Term Effects of Alcoholism
• Korsakoff’s psychosis
• Wernicke’s encephalopathy
Fetal Alcohol Syndrome
Lifetime Prevalence of Alcohol
Dependence in Various Cultures
(Helzer et al., 1992)
Culture
South Korea
New Zealand
Canada
Germany
Puerto Rico
Mainland United States
Taiwan
China
Percentage
22%
19%
18%
13%
13%
8%
6%
.45%
V. Treatment
Law, Society, & the Mental Health
Profession
I.
II.
III.
IV.
Introduction
Judgments about People Accused of Crimes
Involuntary Commitment
Clinicians’ Duties to Clients & Society
I. Introduction
II. Judgments of People Accused of
Crimes
• Competency
– Mental state at time of the trial
• Insanity
– Mental state at the time of the alleged criminal
act
Insanity Defense Rules
M’Naghten rule
Irresistible
impulse rule
Durham rule
The individual is not held responsible for a
crime if…
At the time of the crime, the individual was
so affected by a disease of the mind that he
or she did not know the nature of the act he
or she was committing or did not know it was
wrong.
At the time of the crime, the individual was
driven by an irresistible impulse to perform
that act or had a diminished capacity to resist
performing the act.
The crime was a product of a mental disease
or defect.
Insanity Defense Rules
The individual is not held responsible for a
crime if…
American Law
At the time of the crime, as a result of a
Institute (ALI)
mental disease or defect, the person lacked
rule
capacity either to appreciate the criminality
(wrongfulness) of the act or conform his or
her conduct to the law.
American
At the time of the crime, as a result of a
Psychiatric
mental disease or retardation, the person was
Association (APA) unable to appreciate the wrongfulness of his
rule (IDRA)
or her conduct.
III. Involuntary Commitment
• Prior to 1969: need for treatment
• After 1969, consider the following:
– Grave disability
– Danger to self
– Danger to others
– Immanence of harm
• Patients civil rights
– Right to treatment and the right to refuse
treatment
IV. Clinicians’ Duties to Clients and
Society
• Dual relationships
• Confidentiality
– Tarasoff ruling
• Cultural competency