PTEP_2 - PT Final Exam
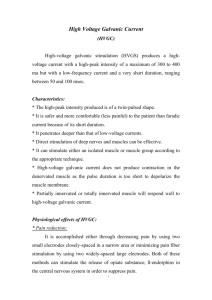
advertisement

Musculoskeletal -> Shoulder 1. 2. 3. 4. 5. 6. 7. -> Special Tests Empty Can => Supraspinatus MUS/T Yergason => Bicipital Tendinitis => ER/Sup Speeds => Bicipital Tendinitis => push down on FA Ludington’s => Bicep Brachelli long head tendinitis => hands on head Drop Arm => Rotator Cuff => 90° ABD Lateral Scapular Slide Test Apley Scratch Test a. Inability to touch opposite shoulder => limited GH ADD, IR, horizontal flexion b. Inability to touch back of neck => limited in GH ABD, ER, upward rotation, elevation c. Inability to touch back of thorax => limited in GH ADD, IR, Retraction, Downward Rotation 8. Hawkins – Kennedy => Shoulder impingement (supraspinatus) forward flex GH 90°/Elbow 90°/IR 9. Sternoclavicular Stress Test => Sternoclavicular/Costoclavicular Lig. Sprain 10. Acromionclavicular Compression/Distraction Test => acromioclavicular/coracoclavicular Lig. Sprain 11. Apprehension Test Posterior/Anterior => dislocation/instability 12. Sulcus SIign => Inferior force/distraction => step inferior to acromion 13. Piano Key Sign => distal clavicle in an inferior direction => instability of acromioclavicular on involved side 14. Posterior Impingement Test => Maximal ER (crank test) => RTC/Posterior Labral Pathology 15. Cross-over impingement test => horizontal flex/ADD => superior sh. Pain => AC joint pathology => Anterior sh. Pain => subscapularis, supraspinatus, Biceps long head => Posterior sh. Pain => intraspinatus, Teres minor, Posterior capsule path. 16. Anterior drawer test => passive ABD GH joint 70 - 80°/forward flex 0° - 10°/ER 0 - 10° Increased anterior translation 17. Posterior drawer test => downward pressure => Increased posterior translation 18. Jobe Relocation Test => supine 90° ABD/full ER => posterior force on head of humerus => in shoulder ER => indicative of anterior instability 19. Feagin Test => 90° ABD rest on PT shoulder => move in atn/inf direction => excessive gliding -> indicative of anterior and/or inferior GH instability 20. Load and shift test=> compression of humeral head + anterior then posterior shift translation => translation greater than 25% of the diameter => instability 21. Grind Test => grinding/clunking => indicative of glenoid labrum tear (overhead) 22. Clunk Test => passive ABD + ER + Anterior force to humerus => grinding clunking => glenoid labrum 23. O’brien test (Active compression) => 90°forward flex + 30 - 45° ADD + max 1R => pain and/or popping present in IR position but absent in ER position is indicative of SLAP lesion. 24. Brachial Plexus Stretch Test => lateral flex subject head + downward pressure => Test if cervical fx or dislocation is suspected => nerve or facet joint impingement 25. Adson Maneuver => palpate radial pulse, rotate arm towards test arm => TDS => Subclavian Artery 26. Allen’s test => 90° ABD and ER, 90° elbow flex, rotate arm towards test arm => TOS 27. Roo’s test => 90° ABD and ER, 90° elbow flex => rapidly open and close hands for 3min => TOS 28. Military Test => arm extended to 30° and hyperextend head and neck => absent radial pulse TOS 29. Pectoralis major contracture test: Arms clasped behind head, PT pushes elbow to table => (+) subject is unable to passively have his elbows reach the table 30. Neer impingment => examine passively and maximally forward reflexes => pain, apprehension => supraspinatus and long head tendons -> Elbow 1. Resistive Tennis Elbow Test (cozens) => Resist pronation, RD, Extension, => ECRL/ECRB => lateral epicondyle 2. Golfer’s Elbow (Medical Epicondyle) => passively Slip FA, extend elbow, extend worst 3. Hyperextension test => passively extend to 0° 4. Elbow Flexion => maximally flex elbow and hold for 3 – 5 min => Radiating pain in median nerve distribution (lateral FA, tip of thumb, index and middle finger, lateral half of index) => indicative of cubital fossa syndrome 5. Varus stress test => pushes laterally => damage radial collateral ligament (LCL) 6. Valgus Stress test => pushes medially => damage UCL/MCL 7. Tinel’s sign => Ulnar notch (btw olecranon process and medial epicondyle) => Ulnar N. compromise 8. Punch Grip => thumb and index finger: pad to pad => anterior interosseous -> median N. (trapped between pronator head) 9. Pronator Teres Syndrome => elbow 90° => Resist FA pronation and elbow extension => median nerve distribution -> Wrist and Hand 1. 2. 3. 4. 5. 6. Tap percussion test => indication of fracture Compression test => Press, stabilize distal phalanynx => fx Long finger flexion test => can’t flex PIP => FDP + FDS + nerve => can’t flex DIP = FDP Finkelstein’s test => identify Dequervain’s (APL/EPB) Phalen’s => Carpal tunnel of Median N. Reverse phalens => Median N. 7. 8. 9. 10. 11. Tinel’s sign => carpal tunnel compression of Median N. Fromets sign => weakness of adductor pollicis of Ulnar N. Wrinkle Test => No wrinkle – dennervated tissue. No peripheral regeneration Allen’s Test => Vascular feeling Bunnel – Littler test => tight capsule vs tight intrinsic muscle => flexion limited in MCP and PIP = capsule. If move PIP with MCP = Intrinsic tight. If move DIP with PIP then retinacular ligament are tight 12. Murphy’s sign: 2nd and 3rd digits are equal when making a fist => dislocated lunate 13. Watson’s test => Ant/post scaphoid while Ulnar and radially => subluxation and reduction of Scaphoid -> TMJ 1. Chvostek => taps over masseter muscle and parotid gland => (+) = twitching facial nerve => hypoparathyroidism => results of low calcium 2. Loading test => Molase => bites down => Anterior dislocated disc 3. Palpation test => 5th digit in subject ear while open and closes mouth => inflammation of synovium of TMJ or TMS pathology Neuromuscular Neuromuscular / w2 1. SCI: partial or complete disruption results In paralysis, i loss, altered autonomic reflex activities - Thiumatic causes: MVA, jumps, falls diving, gunshot wounds - MOI: Flexion (most common lumbar) Flexion-Rotation (most common cenical) Compression Hyperextension - Nonthumatic: disc proplapse, Vascular unsuits, infections - Spinal areas of greatest injury C5, C7, T12 & L1 - Pathophysiology: lack of blood supply Z edme, ischemia, demyelination, Necrosis, scar tissue formation - Lesion level: most distal uninvolved Nerve not at lease 3+/5 or fair + function - Tetbaplegia: C168 - Paraplegla: btwn T1 T12-L1 - ASIA scale: A complete - Byncomplete: sensory, no motor - Ctncomplete: motor presented Muscle and grade < 3 - D=incomplete: motor presented Muscle and grade > 3 E=Normal Syndromes: 1. Anterior cord – loss of motor fxn, motor loss sensation good pain, temp preservation of light touch, proprioception position sense 2. Brown – sequard: UPsilateral awareness Loss of position vibration below The level contralateral loss of P! Temp a few segs below lesion 3. Central: loss of central cenical loss of ventral home loss of UE motor thicks / arm fxn preservation of peripheral located number sacral tracts / leg fxn. Early loss of P! temp 4. Calida equine: below L1, LMN 5. Sachi spanng: spring if tracts to sacral segmenents preservation of penianal sensation , rectal sprincter tone or active toe flexion - Spinal shock loss of fxn resolves btwn 24 hours 6. Poster: B loss of dosal column, sensation of ptro fxn, PI light touch, propnoception, vibration, pressure, deficits of kinesthesia (sterognesis 2 point discrinination) 2. TBI: 10: Diffuse axonal injury: results from shear strain of angular acceleration results in neuronal death petechual hemormages - Focal injury: contusions, lacerators, mass effect from hemomhage edema (hematoma) - Coup-contricoup: injury at point of impact Opposite point - Closed or open injury: fx of skull - Z: hypoxic-ischemic: results from systemic problems (respiration or CV) that compromise cerebral arculation - Swelling / edema: intrcronlal pressure, brain hemuation (uncal, central, or tonsilkr) - Electrolyte imbalance - mass release of damaging neuriot 3. Epilepsy: distunaance of CMS: - Ground mal: tonic-clonic, tongue Biting, arrested breathing; after 2-5 min consuousness is gradually Regrained, full recovery take hours Some attacks preceeded by a brief Aura - Petit-Mai(absence squee) Brief lapse of consousness Followed by immediate full return of conciousnsess posture is maintained,; may occur 100x a day - Status sebure: prolonged sebure (730 mm) very little recovery btwn Attacks, life threatening, medical Emergency - TX: do not restrain patient 4. Vestibular neurontitis: vestibular synd acute infection prolonged attack of symptoms - Caused by vibal or bacterial infection 5. Meniere: vestubular - Recuvent progressive vest. Disease episodes last from min -> hrs - Tinnitus, deafness, fullness Of ear, edema of abrynthis Consistent. -> Symptoms of concussions Loss of consciousness, changes in HR, RR, BP 1. Mild concussion: momentary loss of consciousness or confusion - Retrograde amnesia (loss of memory that goes back in time before injury) 2. Classic: Moderate in severity - Mostly reversible in 24 hours - may be retrograde and posttraumatic amnesia (loss of memory for events after the traumatic event) 3. Severe: loss of consciousness for > 24 hrs - associated with diffuse axonal injury and coma -> Standardized Tests and Measure for TBI 1. Glasgow Coma: Mild (13-15) Mod (9 – 12) Severe (< 8) 2. Rancho Los Amigos (Recovery): 8 general cognitive and behavioral level 3. Rappaport’s Disability Rating Scale levels of disability of functional behavior 4. Glasgow Outcome Scale: Major Disability Categories for outcome assessment -> Symptoms of TBI Increased intracranial pressure, inappropriate physical, verbal, sexual behaviors, poor judgment, iriitability, low frustration tolerance and aggression, impulsivity, safety issues, depressed mood, sensory deficits, paresis, apraxia(dyspraxia), reflective behaviors, balance diets, ataxia, incoordination (cerebellar damage is common) -> Symptoms of CVA 1. ACA Syndrome: Contralateral sensory loss and hemiparesis LE > UE, mental confusion, aphasia 2. MCA Syndrome: contralateral sensory loss and hemi UE > LE, motor speech dysfunction (Broca’s), perceptual dysfunction (parietal sensory cortex), homonymous hemianopsia (optic radiation, internal capsule), loss of conjugate gaze to opposite side (frontal eyelids), sensory ataxia (parietal lobe) 3. Vertebral Artery (medial medullary): ipsilateral paralysis of tongue, contralateral paralysis of arm and leg with impaired sen. 4. Lateral Medullary (Wallenberg: PICA, basilar): ipsilateral symptoms (ataxia, vertigo, N/V, nystagmus, Hornets, dysphagia, impaired speech Contralateral loss of pain and temp of half of body, sometimes face. 5. Basilar Artery: locked in syndrome (occlusion in pons): Quadriplegia and bulbar paralysis: unable to move or speak: full cognitive fxn: sensation may be intact 6. PCA: Contralateral homonymous hemianopsia: contralateral sensory loss, thalamic syndrome, involuntary mvts, paralysis of vertical eye movement => oculomotor CN III -> Standardized Test and Measures for CVA 1. Fugi-Meyer: Objective criteria for scoring of movement (O; cant Z; fully performed) UE, LE fxn, balance, sensation, ROM, pain 2. NIH stroke scale: measures acute cerebral infarction 3. Postural Assessment Scale for stroke (PASS): postural control and balance in patients. 4. Stroke Impact Scale: Brief assessment of physical and social fxn after CVA. 5. Functional Independence Measure (FIM) (Functional mobility and basic ADL, Physical, Psychological, Social Fxns 6. Functional Assessment Measure (FAM) FIM + community access, IADL, Safety, employability and adjustment. -> 10 common disease/congenital conditions 1. ALS: Upper and Lower Motor Neurons Affects muscles of reputation Dysarthria and dysphagia Muscle Atrophy, cramp, fasciculation(LMN) Spasticity and hyperreflexive (UMN) No sensory changes: ALS functional rating scale TX: teach energy conservation 2. Bell’s Palsy: inflammatory response, facial nerve (CN VII) LMN Difficulty wrinkling forehead, close eye lid tight and smoking Loss of control of salivation, one sided facial muscle weakness or paralysis, normal sensation Mouth droops and decrease taste sensation anterior 2/3 tongue Tx: Artificial tears of temp. patching to protect cornea - E-stim - Teach facial muscle exercises - Functional retraining (chew on opposite side) 3. Guillain – Barre (GBS) LMN Polyneuropathy of probable immune – mediated vital organ symmetric motor paralysis and progressive muscular weakness Affects cranial and peripheral N. Stocking/globe sensory loss Paresthesias Progressive weakness from LE -> UE: from distal -> proximal Full tetraplegia with respiratory failure Tachycardia, abnormalities in cardiac rhythm and blood pressure changes Slow recovery 3% mortality rate TX: During Ascending Phase (disease progressing) - Respiratory function - PT PROM with tolerance, positioning to prevent contractures, skin care to prevent breakdown - Stabilized patient - Avoid overuse and fatigue, begin gentle stretching and initiate movement in a controlled environ During Descending Phase - Provide muscle reeducation with moderate exercise program - Improve cardiovascular fitness - Teach energy conservation 4. Multiple Sclerosis UMN - demyelinated disease prevalent in colder climates - sensory disturbances: tigling, numbness, pain - coordination problems and spasticity - Fatigue (in p.m.) - diplopia - B and B problems - Psychosocial problems including euphoria/depression - Adverse rxn to heat - Standardized test - Expanded Disability Status Scale - Minimum Record of Disability - Modified Impact scale TX: Prevention of secondary problems, skin care if sensation is lost or diminished - Breathing exercises - PNF tolerance - Morning treatment preferable Meds: Steroids, ACTH 5. Parkinson’s Disease Progressive disease affecting basal ganglia with a decrease dopamine production TRAP Abnormal gait( festigating or slow shuffling) Behavior changes including memory loss, decubitus ulcers, muscle atrophy, contractures, decreased vital capacity and falls 6. Post-polio (LMN) new form of muscular dystrophy denervation with asymmetrical muscular weakness myalgia joint pain excessive fatigue and decreased endurance TX: Low intensity: never to point of fatigue - Stop exercise with pain or weakness - Energy conservation - 2 – 3 min of exercise to 1 min of rest - Appropriate target => 60 – 80% - 3x/week - Sleep disturbances 7. Cerebral Palsy Non-progressive gestational, perinatal or postanatal CNS damage Voluntary movement impairments Causes: Hemorrhage below lining of ventricles, Hypoxic encephalopathy, Malformations, Trauma to CNS 4 main Syndromes 1. Spastic: UMN (most common) - Hemi, para, or tetraplegia - Increased DTRs, muscle tone - Mass patterns of flexion or extension - Scissors gait and toe walking - Visual, Auditory, Cognitive and Oral-motor deficits may be present 2. Athetoid: - Basal ganglia involvement Slow, writhing, involuntary movement, may affect extremities Decreased tone Poor functional stability in proximal joints, poor visual tracking, speech delay, and oral motor problems ATNR, STNR, TLR, may be persistent blocking functional positions and movement 3. Ataxic: (uncommon) - Results from cerebellar involvement - Weakness, poor coordination, intention tremor produce unsteadiness - Wide base gait - Difficulty with rapid or fine movement 4. Mixed Forms: - Most often: spasticity and athetosis - Less often: ataxia and athetosis TX for ALL: maxima (I) allowed - Motor learning and motor control to facilitate fxn motor skills Adaptive equipment for posture, trunk control, function and socialization 8. Down Syndrome (Trisomy 21) Congenital chromosomal abnormalities: extra chromosome 21 Decreased tone, muscle force, congenital heart defects, visual and hearing losses, laxity of ligs., cognitive defects Difficulty in eating and speech Forceful neck flexion and rotation activities should be limited due to atlantoaxial ligament laxity and potential for a subluxation and/or SCI Tx: Facilitate gross and fine motor via positioning, posture and movement activities o Encourage motor function and avoid hyperextension of elbows and knees during WB activities o Encourage conservation (if congenital heart defects are present) 9. Duchenne’s Musuclar Dystrophy Affects males, destruction of cells Progressive weakness proximal -> distal from ages 3 to 7 Waddling pattern, toe walking, lordosis, frequent falls, difficulty standing up (Gower’s sign) and problems climbing stairs Contractures and deformities for heel cords and TFL As progresses, child develop kyphoscoliosis (after 11 years old) Tx: Maintain mobility o Recreational activities to maintain strength and cardiopulmonary function o Don’t expect at maximal level 10. Myelomeningocele (Spina Bifida) Defect in vertebrae resulting in protrusion of the spinal cord and meninges After surgical closure, hydrocephalus may become a problem and require shunt of the CSF to decrease intracranial pressure A. Ventriculoatrial shunt: cerebral ventricle -> cardiac atrium B. Ventriculoperitoneal: Cerebral Ventricle -> peritoneal cavity Signs: Increased irritability, decreased muscle tone, seizure, vomit, bulging fontanels, HA, redness along shunt tract. Functional problems depending on level of spinal cord defect: Strength deficits Hip flexor and adductor tightness Foot deformities: club foot or talipes equinovarus (club foot) B and B problems Low tone and poor head control Developmental delays Treatment: Proper positioning - Standing frame - Parapodia - Swivel and rollator walker with low thoracic lesion - RGO for lumbar lesion 11. Charcot – Marie – Tooth Disease (Peroneal Muscular Atrophy) Hereditary disorder of peroneal and distal leg M. Foot drop and “stork leg deformity” 12. Legg-Calve – Perthes Disease Idiopathic aseptic necrosis of femoral capital epiphysis Unilateral: boys ages 5 to 10 years Treatment: o Prolonged Bed rest o Mobile traction and slings o Casting o Special hip abduction orthosis Common Reflexes Tested and the Scale o Jaw Reflex: trigeminal CNV o Biceps: C5 – C6 o Triceps: C7 – C8 o Brachioradialis: C5 – C6 o Hamstrings: L5 – S3 o Quads (knee jerk; patellar): L2 – L4 o Achilles (ankle jerk) S1 – S2 Scale(scoring) O: absent 1+: Decreased response 2+: Normal 3+: Exaggerated 4+: Hyperactive DTRs: may be abnormal in CNS lesions (hyporeflexia, hyperreflexia) or PNS lesions (hyporeflexia) Sensory Pathway (White matter) A. Ascending fiber systems: (sensory) 1. Dorsal Columns/Medial lemniscal - sensation of proprioception, vibration and tactile discrimination - fasciculus cuneatus (UE and laterally located) - fasiculus gracelis (LE and medially located) - fibers cross (lemniscal decussation) to form medical lemniscus ascend to thalamus then to somatosensory cortex 2. Spinothalamic: Sensations of pain and temperature (lateral), and crude touch (anterior) – ascend 1 or 2 ipsilateral spinal cord (lissauer) synapse and cross in spinal cord to opposite side 3. Spinocerebellar: proprioception information from muscle spindles, GTO, and touch and pressure receptors to cerebellum for control of voluntary movements - Dorsal spinocerebellar => ipsilateral -> inferior - Ventrospinocerebellar => contralateral and ipsilateral -> superior cerebellar 4. Spinoreticular: Deep and chronic pain to reticular formation of brainstem, polysynaptic pathways. B. Descending Fiber Systems (motor) 1. Corticospinal Tract: Arise from primary motor cortex, descend in brainstem, cross in medulla; important for voluntary motor control. 2. Vestibulospinal: Arise from vestibular nucleus and descend to spinal cord in lateral (uncrossed) and medial (crossed and uncrossed); important for control of muscle tone, antigravity muscles and postural reflexes. 3. Rubrospinal: Arise in contralateral red nucleus and descend in lateral white column: assist in motor function. 4. Reticulospinal: arises in reticular and descends (crossed and uncrossed) in ventral and lateral columns - on dorsal gray: modifies transmission of sensation - on ventral gray: influences gamma motor neurons and spinal reflexes 5. Tectospinal: Arises from superior colliculus (midbrain): assists in head turning response to visual stimuli List of 12 Cranial Nerves and How to Test 1. Olfactory (some): D - Loss of smell 2. Optic (stars): D – Monocular blindness, loss of papillary constriction, absence of blink reflex F – Slight, papillary 3. Oculomotor (make): F – Moves eye and elevates the upper eyelid D – Ptosis (levator palpebrae), dilation of pupil, loss of accommodation of light reflex; Homer’s syndrome 4. Trochlear (money): F – Motor N. for superior oblique muscle D – Diplopia, failure to rotate eye up and out 5. Trigeminal (but): F – Mastication and sensory n. D – Loss of facial sensation, weakness in mastication, deviation of open jaw to ipsilateral side 6. Abducens (my): F – Abducts eye via nerve supply to lateral rectus muscle D – Diplopia, convergent squint (medial strabisumus) and abductor paralysis of ipsilateral eye 7. Facial (brother): F – Facial expression, speech articulation, winking, ingestion of food and drink, taste, salivary and nasal secretions D – Ipsilateral facial paralysis, dry mouth, loss of taste anterior third of tongue (Bell’s palsy) 8. Vestibulocochlear (says): F – maintenance of equilibrium, hearing D – Vertigo, nystagmus, disequilibrium, tinnitus, loss of hearing 9. Glossophareangeal (bugs): F – Elevates pharynx, salivary secretion, taste D – Slight dysphagia, partial dry mouth, loss of taste posterior third of tongue, dysphonia (hoarseness) 10. Vagus (bunny): F – Phonation, visceral sensation and reflexes, cardiac depressor, bronchoconstrictor, GI tract peristalsis and secretion D – Palpitation, tachycardia, vomiting, slowing of respiration, ipsilateral paralysis of soft palate and larynx, hoarseness, anesthia of larynx, gag reflex. 11. Accessory (makes): F – Deglutition and phonation (carotid part), movements of head and shoulder (spinal part) D – Weakness in shrugging ipsilateral shoulder turning head to opposite side scom 12. Hypoglossal (more): F – Movements of tongue D – Unilateral paralysis of tongue, deviation to ipsilateral side with protrusion UMN VS Location Structures LMN CNS Cortex, brainstem, corticospinal tract SC CVA, TBI, SCI Disorders Tone Hypertonia, velocity dependent Increased Muscle spasms, flexor/extensor Weakness/paralysis Reflexes Involuntary Movement Strength Muscle bulk Variable, disuse atrophy Voluntary Movement Impaired/absent dyssynergic pattern PNS SC: anterior horn, CN, peripheral nerve Polio, GB, Peripheral neuropathy Decreased, not velocity dependent Decreased With denervation: fasiculations Limited distribution - segment/focal - root innervated Neurogenic atrophy, rapid focal, severe wasting Weak or absent if nerve interrupted Table 2 – 5 CENTRAL NERVE PD ALS CVA Conditions vs Peripheral Nerve Peripheral nerve injury Trigeminal neuralgia Bulbar palsy TBI SCI Guillain – Barre ALS Postpolio Bell’s Palsy Integumentary Burn Classification 1. Superficial burn (1°) – only involves outer epidermis area, may be red with slight edema. No scarring, spontaneous healing 3 – 7 days, delayed pain. 2. Superficial Partial thickness – epidermis and upper layer of dermis, bright pink, blisters, moist surface, weeping, moderate edema, painful, sensitive to touch, change of temperature, spontaneous healing, discoloration. 3. Deep partial thickness (2°) – damage to epidermis, dermis, nerve endings, hair follicles, and sweat glands, mixed red or waxy white appearance, slow capillary refill, broken blisters, wet surface, marked edema, sensitive to pressure but insensitive to light touch or soft pin prick , slow healing. 4. Full thickness (3°) – destruction of epidermis, dermis, subcutaneous; may extend to muscle. White, gray, charred or black appearance, no blanching; poor distal circulation, dry leathery surface, little pain, nerve endings destroyed, removal of infection, hypertrophic scarring and wound contracture. 5. Subdermal (4°) – destruction of epidermis, dermis, subcutaneous with muscle damage, charred appearance, destruction of vascular system, lead to additional necrosis. From electrical burns; ventricular fibrillation, acute kidney damage, SCI, heals with skin grafting and scarring, requires extensive surgery amputation may be necessary. Staging of Pressure Ulcers (characteristics) - Stage 1: Nonblanchable erythema of intact skin. Skin temperature (warm or cool), tissue consistency (firm or boggy), and/or sensation (pain, itching) changes. Stage 2: Partial-thickness skin loss: involves epidermis dermis, or both ulcer is superficial. Presents clinically as an abrasion, blister, or shallow crater. Stage 3: Full-thickness skin loss: involves damage to or necrosis of subcutaneous tissues. May extend down to, but not through, underlying fascia. Presents clinically as a deep crater. Stage 4: Full-thickness skin loss: involves extensive, destruction, tissue necrosis, or damage to muscle, bone, or supporting structures undermining and sinus tracts may be present. Physical Examination and Documentation Size = Clear film grid superimposed on wound Depth = sterile cotton tip applicator (tunneling) Length = Head to foot Width = Left to Right or Right to Left Ulcers Etiology Artificial Arteriosclerosis obliterans, Artheroembolism Venous Valvular incompet. Of DVT venous HTN Appearance Irregular, smooth edges, minimum to no granulation: deep Location Distal lower leg: toes, feet, lateral malleolus, ant. Tibial area Decreased or absent Painful, especially leg elevated Irregular, dark pigmentation, fibrotic, good granulation, shallow Distal lower leg med. malleolus Pedal Pulses Pain Drainage Gangrene May be present Signs Trophic changes, pallor on foot evelation dusky rubor on dependency Usually present Little pain, comfort with leg elevated Moderate to large amt of exudate Absent Edema status, dermatitis, cyanosis on dependency Diabetic Diabetes with arterial disease and peripheral neuropathy Repetitive trauma or insensitive skin Decubitus Unrelieved pressure Plantar aspect of foot Bony prominence, sacrum, heel, ischial, elbows Present or diminished Not painful, sensory loss Red, brown/ black, yellow Painful if sensation is intact Sepsis: may develop Absent ankle jerks Hypotension, with neuropathy microvascular inflammatory with necrotic tissue, superficial -> deep erosion of deep layers, WBC Physical Examination and Documentation Undermining (circumference) - Deepest area into the wound, document using the face of the clock. Head of the wound is 12. Foot is 6. Ex. 1.7cm at 10 o’clock (clockwise) Tunneling - Deepest area into the wound (depth), document using the face of the clock. Head of the wound is 12. Foot is 6. (clockwise) Ex. 1.8cm at 3 o’clock Types of Exudate 1. Serous (clear): Watery-like serum, normal in inflammatory and proliferative stage 2. Purulent (yellow): Containing pus, infection 3. Sanguineous (Red): Containing blood, normal or disrupt of BV 4. Serosanguineous (pink): Healthy wound Rule of 9s Color and Tissues Involved 1. Clean Red wound: healthy granulating (in need of protection), absence of necrotic tissue 2. Yellow wound: include slough (necrotic or dead tissue), fibrous tissue 3. Black wound: Eschar 4. Indolent ulcer: slow to heal; not painful Genitourinary System Symptoms and Types of Urinary Incontinence Inability to retain urine: result of loss of sphincter control may be acute (due to transient causes e.g. cystitis) or persistent (e.g. stroke dementia) 1. Type: Stress – damage to pudendal nerve Increased intra-abdominal pressure o Coughing, laughing, exercise, straining, obesity Weakness and laxity of pelvic floor musculature o Post-partum incontinence, menopause 2. Type: Urge – inability to delay voiding to reach toilet due to: Detrusor muscle instability or hyporeflexia (stroke) Sensrory instability: hypersensitive bladder 3. Type: Overflow – An overdistended bladder or incomplete emptying of bladder due to: Anatomical obstruction: prostate enlarged Acontractile Bladder: SCI, DM Neurogenic Bladder: MS, Suprasacral Spinal lesion 4. Type: Functional – leakage associated with inability or unwillingness to toilet due to Impaired cognition (dementia): depression e.g. Alzheimer’s Impaired Physical functioning; stroke Environmental barriers Bladder Infections (UTI) Lower UTI (Urethra and Bladder): Cystitis (inflammation and infection of bladder) Urethritis (inflammation and infection of the urethra) - Symptoms of urinary frequency, urgency, burning during urination. Urine may be cloudy and foul smelling. - Pain is noted in suprapubic, lower abdominal, or groin area, depending on site of infection. Upper UTI (Ureter and Kidney): Pyelonephritis (inflammation and infection of one or both kidneys) - Symptoms of systemic involvement: fever, chills, malaise, HA, tenderness and pain over kidneys (back pain), tenderness over the costovertebral angle (Murphy’s sign) - Symptoms: frequent and burning urination; nausea and vomiting may occur - Palpation or percussion over kidney causes pain - Can be acute or chronic; generally more serious than lower UTI Obstructive disorders - Prostatic hyperplasia (incontinence for men) - Renal calculi (kidney stones) => Calcium, Magnesium, Uric Acid, Cystine Extracorporeal Shockwave Lithotripsy (ESWL) is used to break up stones into fragments to allow for easy passage. - Treatment/prevention: increase fluid intake, thiazide diuretics, dietary restriction of foods high in oxalate (vegetables, fruits, nuts, grain, seeds), acidification or alkalinization of urine Renal failure A. Acute: Elevation in serum area and creatinine - Circulatory disruption of kidneys, toxic substances, bacterial toxins, acute obstruction, trauma. B. Chronic: Progressive loss of kidney function leading to end-stage failure - Prolonged acute urinary tract obstruction and infection, DM, SLS, uncontrolled hypertension. - Uremia: end-stage toxic condition resulting from renal insufficiency and retention of nitrogenous waste in blood - Signs and Symptoms: anorexia, nausea, mental confusion Pregnancy - Postural changes: Kyphosis with scapular protraction, cervical lordosis and forward head; lumbar lordosis - Third trimester : limit supine position to avoid inferior vena cava compression bridging - Balance : COG shifts forward and upward - Ligament laxity: Joint hypermobility - Muscle weakness : Stress incontinence - Respiratory: elevation of diaphragm with widening of thoracic cage; hyperventilation, dyspnea with mild exercise - Cardiovascular : Increased blood volume, increased venous pressure in LE, increased HR and CO, decreased BP due to venous distensibility - Altered thermoregulation: Increased basal metabolic rate, heat production Pregnancy-related Pathologies 1. Diastasis Recti Abdominis - separation from midline (linea alba), > 2cm is significant 2. Pelvic floor disorders - Pubococcygeal (PC) muscles - Weakness or laxity of PC can result in partial or total organ prolapsed ex: A. Cystocele: Herniated bladder into vagina B. Rectocele: Herniated rectum into vagina C. Uterine Prolapse: Bulging uterus into vagina * Pain can radiate down the posterior thigh 3. Sacroiliac dysfunction - Posterior pelvic pain - Pain in buttocks, radiate into posterior thigh/knee - Associated with prolonged sitting, standing, walking - Avoid single-limb weight bearing 4. Varicose veins - Elevate extremities - Do not cross legs - Elastic support stockings 5. Preeclampsia - Acute hypertension after the 24th week of gestation - Symptoms of HTN, edema, sudden excessive weight gain, HA, visual disturbances, hyperreflexia - Initiate prompt physical referral 6. Low Back and pelvic pain - Emphasize use of firm mattress - Massage, modalities for pain (no deep heat) 7. Cesarean childbirth - Post-operative TENS can used for incisional pain: electrodes are placed parallel to incision - Assist patient in breathing, coughing - Postural exercises: precautions about heavy lifting for 4-6 weeks - Friction massage Disorders of the Female Reproductive System 1. Endometriosis - Ectopic growth and function of endometrial tissue outside of the uterus - Common sites include ovaries, fallopian tubes, broad ligaments, uterosacral ligaments, pelvis vagina, intestines - Back pain, endometrial implants on muscle (Psoas and pelvic floor M) - Symptoms: dysmenorrheal, dyspareunia (abnormal pain during sexual intercourse) and infertility 2. Pelvic Inflammatory Disease (PID) - Inflammation of upper reproductive tract involving uterus (endometritis), fallopian tubes (salpingitis) or ovaries (oophonitis) - Symptoms: lower abdominal pain, with mesnstrual cycle, purulent cervical discharge and painful cervix - Fever, increased WBC and increased ESR are present Disorders of the Male Reproductive System 1. Erectile Dysfunction (ED) Causes: - Neurogenic: CVA, trauma, SCI, MS, PD Hormonal: decreased androgen level with hypogonadism, hypothyroidism and hypopituitarism Vascular: HTN, CHD, hyperlipidemia, smoking, DM, pelvic irradiation 2. Prostatitis - Inflammation and infection of prostate gland - Dull acting pain may be found in the lower abdominal, rectal, lower back, sacral, or groin regions - Non-bacterial inflammatory prostatitis produces pain in penis, testicles, and scrotum: painful ejaculation, low back pain or pain in inner thigh, decreased libido and impotence - Because the prostate encircles the urethra, obstruction of urinary flow can result. Cardiovascular Page - 1 Week 2 : caradovascular/ Pulmonary/ list 10-15 common diseases 1. COPD : - Abnormal breath sounds - Increased chest size - Dry/ productive cough - Hx of smoking 2. Astma - reactivity of trachea of bronchi - Narrowing of away - Secretions - Dry or productive mucold sputum - Wheezing cough - Chest wall symmetically decreased - Meds ovil or iv stenrds (prednisone) 3. Bronchitis - chronic inflammation of tracheobronchlal tree cough - sputum lasting at least 3 months for Z convective years - Wheezing or Ranchi breath sounds - Productive mucold & infection - May have fever - Tx paced breathing, Endurance, D+ ed about smoking, biancho, pulmonary hygiene 4. Cystic 5. - Thickening secretion of all exocrine gland fibrosis - Respimtory infection C staph and pseudononas aewgunosa - + sweat test - Rales (extrn breath sounds), wheezing - May have hemoptysis (cough up blood) - Large amt of mucold - Tx. Percussion, vibrate, shake endunince exercises - Trypsin precursor of prypsnagen Emphysema - Permanent abnormal enlargement distraction of all spaces distal to - terminal bronchures - barreled chest - assessory mussels of vent - breath sounds wheeze - dyspnea - puzed up breathing during exhalation 6. Alternations to pleura fibrotic changes within pulmonary pleura - Pulmonary filonosis - Asbestosis - Radiation pnamonitis - Oxygen toxicity 7. Aitenatony to chest wall - restricted motion of bory thonix - alkylosug spondylitis - arithiting - scoliosis - pectusexcalatum - chest wall skin louring - scterodorma 8. Alterations un Neuromuscular - muscular strength in an unability to expand no cage - MS - Muscular dystrophy - PD - SCI 9. Teauma - 2 or more fixoures in 2 or more adjacent nibs - Flail chest shallow breathing - Crepitation over fix site - Inspination: flail moves inward - Exhalation: flail moves outward - Tx. gontle breathing, spunt, proper positioning, pain manage 10. Pneumothorix air enters plewal space causing lung to collapse due to loss of negative trauma pressure - Or absent breath sounds - Dry cough - Local or referred pain - Trachear dernation quary from affected side - Hyperresonant tympanic percussion sound - Tx. chest tube, chest precaution 11. Tuberculosis infection spread by droplets - after 2 weeks of meds, host is non-noninfectious - TB in HIV patients - Hemoptysis - Low grade fever - Dyspnea - Chest wall pain 12. Pulmory Edema acute Disease - excessive seepage if flued from pulmonary vascular system unto - interstitial space due to - ventricular failure - Aovtic valvular disease - Mitral valvular disease - Unhalation of toxic fumes - Naracotic overdose - Dyspnea on exertion or paroxysmal noctumal dyspnea - Fatgue - Pink frothy sputum - Circuits - Tx. divietics salt intake bed rest (hob elevtel) 13. Rulmonary Acute disease - thromlals from peripheral venous circulation (ie) - lodges in Embolic pulmonaryarery - infarction chest hemoptysis, ploural friction rub, fever and EXR - 5 infroction pachitinea anxiety restlessness rales wheezing decreasing breath sounds - Tx. low dose hepan alalgesies, rilmory vasodilaturs. Page – 2 4st 10-20 1. 2. 3. 4. 5. 6. Anti-anhythmic : I docaine, Dilantin, Norpace, - Control or prevent cardnic - anthythmias that can be fatal quinidine Anti-arolinergic (atropine) - used & IV for heart block or bbidoavzlia - inhibits ACTH, blocking Vagal effects on SA & AV node - SE Palpitations, HA, ataxia restlessness, dry mouth, blurred vision Beta-adrenergic: Propranolol (indetal) - HR, BP, conthchloty & SV - OZ demand on = in exercise - dent use HR to determine tolerance of ex. use RPE Calcium channel: Vasodilate & relieve coronary antery spasm - could reduce blood flow to al muscel creating iocnemic reponse - diattizem, cardizen - BP, control anthythmias Digitals: Contractility HR - tx of CHF - digoxin Diuretics: myocardial work (Preioad & afferioad) - 7. & Lungmeds Control HTN Nitrate: Vasodilator - BP Preload - OZ demand on 8. 10. 11. Anticoagulants: Coumadin & heparin - blood clotting time - Could result in hemoptysis during percussion & snacking - Pts DVT Branchoduators: Epinephine, vention, Alupent - Relax smooth muscle - open lumen - used prior to ex. to reduce - negative effect (asthma) Corticosteriods: Predntson & contisool - edema & inflammation - COPD - SE .OP muscle wasting - slow wound healing 1. Lymphatic Deceases - Lymonadenopathy: enlargement of nodes or stendoness 2. Lymphedema: Chronic-execrate acamuldar of fund - results from massacres insufficiency A) Primary congenital & alonmalyaph note or lymph vesser (hypoplasia) B) 2 : acquired; injury of 1 or more pane - results from surgery radical mastectomy lymphnode removal radution therapy for beast cancer, - results of panlysis & desuse - tropical & subtropical areas from - filansis (nematode worm) - Chronic venous insufficiency. 3. Acute lymphangtis: bacterial infections spreading throughout lumph system - Streptococcal 4. Initiating factors: inactivity / charges in carbon pressure - fluctuation in weight gain - Hypermia - Hypopotonia Page – 3 Week 2: Musculos kelctal -> Conditions RA: Systemic disorder, unknown etiology Dysfunction of synovial tissues and articular cartilage at hands, wrists, elbows, shoulders, knees, ankles, Ulnar drift and volar subluxation of MCPs X-rays, lab tests (increased WBCs & erythrocyte sedimentation rate. Hemoglobin/hematocrit show anemia elevated RF) Rx: Antireumatic drugs, NSAIDS( side effect fluid retention and Edema), immunosuppressive PT Interventions Joint protection strategies, improve/maintain joint mechanics and CT function Aerobic fitness Osteoporosis Metabolic disease Depletes bone density (=fractures) Senile: Decrease in cell activity (genetic or acquired) Post-menopausal primary: Decrease in estrogen production CT scan (assess bone density) Rx: Calcium, vit D(aids in calcium absorption from the G)I, calcitonin( helps prevent osteoclastic activities and aids reabsorption), estrogen, biophosphates PT Intervention Joint/bone protection strategies, aerobic exercise, improve joint mechanics Osteomalacia Decalcification of bones due to vit D deficiency Severe pain, fractures, weakness, deformities Diagnosis: X-ray, bone scans, possibly a bone biopsy Rx: Calcium, vit D, calciferol (form of vit D (D2) via injection) PT Intervention Joint/bone protection strategies, aerobic exercise, improve joint mechanics Osteomyelitis Inflammatory response within bone due to infection Usually caused by staph aureus More common in children, immunosuppressed, males Diagnosis by: Lab tests for infection, possible bone biopsy Rx: Antibiotics for infection, nutrition, possible surgery PT Intervention Joint/bone protection strategies, cast care, improve joint mechanics Arthrogryposis multiplex congenita Congenital deformity of skeleton and soft tissues Decreased joint ROM, "sausage-like" limbs Blue sclera noted and increased contractures and club foot Diagnosis: X-ray Rx: PT intervention Joint/bone protection strategies, aerobic exercise, improve joint mechanics, education RE adaptive/assistive/orthotic/supportive devices, flexibility exercises Oseogenesis imperfecta Characterized by Abnormal collagen synthesis, imbalance between bone deposition and reabsorption Thinning of bone - fractures/deform Genetic autosomal dominant Bone scan, X-ray, serology Rx: Calcium, vit D, estrogen, calcitonin, biophosphonates Joint/bone protection strategies, aerobic exercise, improve joint mechanics Osteochondritis dissecans Separation of articular cartilage from bone (osteochondral #) Usually medial femoral condyle, occasionally femoral head/talar dome/capitellum Diagnosis: X-ray, CT PT intervention Joint/bone protection strategies, flexibility exercises (for normal joint motion) aerobic exercise, strength, power, and endurance Myofacial pain syndrome Characterized by trigger points Active TP: Tender, referral pattern Latent TP: Not tender, can be converted to active May be due to sudden overload, overstretch, repetitive/sustained muscle activities No diagnostic tests Rx: Dry needling, analgesic/corticosteroid injection (Side effects include infection moon face, striae), flexibility exercises (for normal joint motion) Myositis ossificans Abnormal calcification within muscle belly Usually due to direct trauma (hematoma-calcification) CAN BE CAUSED BY EARLY STRETCHING/MOBILIZATION WITH AGGRESSIVE PT FOLLOWING MUSCLE TRAUMA Usually occurs in quads, brachialis, biceps Diagnosis: X-ray, CT, MRI Acetaminophen( side effects Liver damage), NSAIDS( side effects GI disturbances) Possible surgery (if non-hereditary and after lesion has matured - 6-24 months. Indicated if lesion interferes with joint or impinges nerves) Flexibility (for normal joint motion), massage (reduces guarding/pain), mobilization (correct biomechanical faults), aerobic exercise (AVOID BEING OVERLY AGGRESSIVE WITH ALL ABOVE TECHNIQUES) Complex regional pain syndrome (CRPS) Dysfunction of sympathetic nervous system including pain, circulation and vasomotor disturbances Long term: Muscle wasting, trophic skin changes, decreased bone density, decreased proprioception, contractures Etiology unknown (thought to be related to trauma) Two types: Type 1 1) Triggered by tissue injury; all patients with above symptoms but no underlying nerve injury Type 2 2) Same symptoms but clearly associated with nerve injury Rx: Sympathetic nerve block, sympathectomy, SC stim, intrathecal drug pumps( side effects drowsiness), topical analgesics, antiseizures Side effects, antidepressants( side effects mood swings, orthostatic hypotension)corticosteroids, opioids (side effects drowsiness, respiratory depression). PT interventions Education to prevent injury, desensitization (focus on RTW), flexibility (for normal joint motion), TENS Paget's Metabolic bone disease, abnormal osteoclast/osteoblast activity Etiology unknown (possibly viral) Spinal stenosis, facet arthropathy, possible spine Diagnosis: X-ray, lab tests (look for increased serum alkaline phosphates and urinary hydrogenase) Rx: Acetaminophen, calcitonin and etidronate disodium (limit osteoclast activity) Joint/bone protection strategies, improve mechanics, aerobic Idiopathic scoliosis Two types: Structural: Irreversible lateral curvature with rotation Nonstructural: Reversible lateral curvature without rotation which straightens with flexion X-ray, CT, MRI Rx (Structural): Bracing, possible surgery depending on degree of curve (<25 conservative, 25-45 orthoses, >45 surgery) Flexibility, strength, power, endurance, electrical stimulation (for muscle performance), application and education RE orthoses Torticollis Spasm/tightness of SCM Characterized by Side bend towards, rotation away from affected SCM Rx: Acetominophen, muscle relaxants (side effects Drowsiness), NSAIDS Flexibility, manual therapy - massage, joint oscillations (to decrease muscle guarding/pain), mobilizations (to corrects biomechanics) Glenohumeral subluxation/dislocation Anterior-inferior is the most common direction of dislocation Occurs with abduction and forceful ER Tearing of inferior GH ligament, ant capsule, possibly labrum Posterior: Occurs with horizontal adduction and IR Complications: Hill-Sachs, SLAP, Bankart, bruising of axillary nerve AVOID APPREHENSION POSITION POST SURGERY CT, MRI, apprehension tests Rx: Acetaminophen, NSAIDS, biomechanical correction (especially scapulohumeral rhythm, dynamic stabilization) Thoracic outlet syndrome (TOS) Compression of neurovascular bundle (brachial plexus, subclavian artery and vein, vagus and phrenic nerves, sympathetic trunk) between soft and boney structures Occurs when size or shape of TO is altered Areas of compression: Scalene triangle Superior TO Between clavicle and 1st rib Between pec minor and thoracic wall Rx: Surgery, acetaminophen, NSAIDS, postural reeducation, biomechanical restoration, manipulations/mobs (especially 1st rib) 1. DJD: Artnntic: P!/stuffness upon rising - P! eases through a.m $ c exercise - P! bending - Soreness / nagging - Non theumatic, nonsystemic Diff Dx: Normal ESR Abnormal ft ndiographs Problem in WB - TX: NSAIDS, education…. 2. AAhnogyrposis: non progressive, non genetic congenital - symmetrical Rigid joints - sausage uke - Hip disloc/contric = Frex, ABD,ER - Diff Dx: spina bitfida 3. CRPS: Abnormal sympathetic reflex - P! edema, circulation, OP, slandriynes, propriception atrophy - Tx: modalities, ft mobs, WB, ckc activites 4. Colte’s fx: FOOSH - Distal segment of radius moved dorsal - Tx: cast -> AROM / PROM -> resistance > Mobs -> ckc activities 5. Fibromyalgia: - Tendemess, pl stuffness in mus - Related to stress, anxiety, fatigue, sleeplessness - Achirg burning - Diffuse or tenderpoints\ - Diff Dx: 11 out of 18 tender points Recognition of typical pattern of nonrnoumatic symps + sleep deprivation - Tx: ADL +x, stress management - Meds: analgesics antidoppresants 6. Gout: level of senium uric acid metabolic disease deposition of unite cyystals - Severe ft pain @ night & warmth, enythema extreme tenderness / hypersons - Tx: Anti-inflammatory, use of colcnine daily, diet, weight loss, alcohol, allopurinol to hypeniricamia 7. Hemphilia: Hemownagic disorder (hereditary) - PT converns: Hemanthrosis muscle bleeds 8. ITB_Syndrome: nibbing of ITB over lateral epdicondyle of femur - Ober test - Excessive hupIR - TX: stretch, modalities, mobs, shoe orthosis 9. Myositis ossificans: truma to muscle -> Hematoma -> ossity or calcity - Quads, bnonialis bicepsionchill - Induced ealy mob aggressive PT - Tx: conservative gentle A/AAROM - Passive stretching NOT undicative - No manual stretching over pressure @ end range 10. Osteochondritis dissecans: sopriation of articular cargtibage from bone. - Medical femoral condyle - Less frequently at femoral head talardome - Tx: Gait tx, fxn strengthening, conditioning 11. Osteomalacia: decalcification of bones vitamin D - Tx: pain control, fxn mobility tx 12. Oseomyelitis: Bone infection - Traumatic injury + infection - Child: distal femur, proximal tibla, humens raidus - Adult : Pelvis venebias usually result of containination of related to surger or truma 13. Osteoporosis: Metabolic bone disease - Depletes bone mineral density - Postmenopausal estrogen 14. Pagets: osteitis deformans metabolic bone distease - Intial phase of excessive bone - Reabsorption followed by excessive abnormal bone formation - New bone is weak fagile - Fatal when ass ZCHF bone saroma or giant cell tumore - Heals slowly uncomplete - Vatebral collapse vascular changes -> paraplegia - Osymptomatic = Notx - Symptomatic = dng theraphy 15. Patellofemoral dysfxn: patella fails to trick properly into trochelear groove - Instability / P! first 30 of knee fexion - Stair clumbing, prolonged sitting (moviegoer sign) squal, jump - Diff Dx: Q angle > 18 - + chondromalacia test. - Abnormal tracking of patella - During knee - Tx – Taping - Strengthening - Shoe unserts - TFM Page - 4 16. Pattelar position: Patellaya: Lower than normal - Patella alta: Higher patella “camel sign” “less efficient in knee” - Tx: inferior glide -> patella alta Superior glide -> patella baja 17. Progressive systemic sctorosis (sclenderma) Fibrosis changes in intermalorgan skin - Accompanied by Raynauds phenomenon - Polyarthralgia is a prominent early symptoms - Diff Dx: vneumatold factor 18. Pronator Teres synd: Median N entrap - PTS test: resist pronation from ao of elbow to extension - Tx: nerve glides stretch, AROM, ultrasound, NMES 19. RA: systemic inflammatory disease - symmetrical pattern - eye lessons injection, opare additional manifestations - malaise fatigue - symmetrical numbness -> - myelopathy => refer to MD! 20. JRA: prior to age 16 - Characterized by fever rash - Fatigue, malaise, weight loss, general ms p! - Symmetrical bilateral presentation - Deformities: UD swan neck or boutonniere deformities 21. Scaphold fx: navicular: FOOSH - Poor vascular supply - High risk of a vascular neerosis of proximal fragment - Tx: early AROM of distal proximal jounts while UE is casted - Latee: foral use of wrist hand 22. Scoliosis: structural alonormalities (leg length or HNP) - Diff Dx: postural analysis forward flexion test - Tx: Bracing: Hamington Rodsctural: stretch, shoe unsers - Respiratory care needed if cobb’s angle is > 40 23. Sjogrens syn: meumatold-like by dyness of mucous membrane, inflamm anema - Diff Dx: Dryness of oyos Mouth z jt - Annentis occute - Tx: sipping fluids - Chew sugarless gum - Mouth wash 24. Smiths fx: FOOSHZ hand suppurated - Distal fx of radius volaty - Cast -> A/PROM -> Resistance -> mobs -> ckc 25. Systemic lupus: chronic systemic, Rnematic, unflammatory Disorder. - Diff Dx: malaise, fatigue, anthblge, Fever, skin rash (over nose) anemia, hair loss, Raynauds phenomenon - Vascullitis, lesion undigit necrotic legulce 26. TMJ: synontis capsulitis - P! anterior to ear (preauricular) - Unable to close back teeth - Open less than 40mm z p! - Pan decreases rest - TMJ hpermobility - “My jaw feels like its out of place” - Ft noises, jaw catching in fully opened position - Mandibular depression > 40 mm Derviates toward non involved side - Disc displacement reduction “Jant noises, pops or clicks” - Disc displacement is limited to 20-25 mm Deflection toward unvolved side. - Lateral excursion limited Page - 5 ABI Test of peripheral arterial circulation Ratio of Lower Extremity Pressure Upper Extremity Pressure Significance - > 1.0 = Normal; ankle systolic is at least as high as brachial pressure - 0.8 – 1.0 = Mild peripheral artery disease compression therapy with caution - 0.5 – 0.8 = Moderate: + for intermittent claudication compression therapy is contraindicated - < 0.5 = Severe; Critical limb ischemia, + for rest pain compression therapy contraindicated Intermittent Claudication Examine for coldness, numbness, or pallor in legs or feet; loss of hair over anterior tibial area Leg cramps may also result from diuretic use with hypokalemia Diastolic and Systole Systole - Ventricular contraction - End – systolic volume is the amount of blood in the ventricles after systole; about 50mL Diastole - Ventricular relaxation and filling of the blood - End - diastolic is the amount of blood in ventricles after diastole; about 120mL Heart Sounds Auscultation landmark: 1. Aortic Valve: 2nd Right at Sternal Border 2. Pulmonic Valve: 2nd Left Sternal Border 3. Tricuspid: 4th Left at Sternal Bone 4. Mitral: 5th Left at border(midclavical) 5. Erb’s point: 3rd Left Hear S1 and S2 equal 6. PMI: Same as mitral point of max. impulse S1 sound (lub) - Normal closure of mitral and tricuspid valve - Beginning of systole - Decreased on first degree heart block S2 sound (dub) - Normal closure of mitral and tricuspid valve - Marks end of systole Decreased in aortic stenosis Bruit Indicative of atherosclerosis Common in carotid or femoral artery Gallop S3 (ventricular falling) o Indicative of congestive heart failure (LV) S4 (ventricular filling and atrial contraction) o Indicative of pathology (CHD, MI, Aortic stenosis, or chronic HTN) Right-sided Heart Failure Increased RAP, CVP Jugular distention + Hepatojugular reflex Right ventricle heave Murmur of tricuspid Hepatomegaly Peripheral Edema Nausea/Vomiting Anorexia Weight Gain Ascites Right upper quadrant pain Cystic Fibrosis Exocrine glands Obstructive, resistive, or mixed disease Respiratory infections vs Left-sided Heart Failure Tachycardia S3 gallop Crackles Increased PAP, PAWP, SVR Laterally displaced PMI Left ventricular heave Pulsus Alternans Confusion Decreased Urine Output Cheyne – stokes respiration (advanced failure) Murmur of metal insuff. Fatigue Cough SOB DOE Orthopnea PND Diaphoresis Inability to gain weight Diagnosis by blood test trypsinogen or (+) sweat electrolyte test Heart Attack Caused by occlusion of one or more coronary arteries Factors: atherosclerotic with thrombus function, coronary vasospasm or embolism; cocaine toxicity Zones of infarction 1. Central Zone: Pathological Q wave, electrically inert 2. Zone of injury: electrically unstable, elevated ST segments in leads over injured area 3. Zone of ischemia: electrically unstable, see T wave inversion Infarction sites: o Transmural (Q wave) Full thickness of myocardium o Nontransmural (no Q wave) Subendocardial Subepicardial Intramural infarctions Sites of Coronary A. Occlusion o Inferior MI: Right ventricle infarction = Right coronary artery o Lateral MI: Ventricular ectopy, Circumflex A o Anterior MI: disturbances of lower conduction: Left Anterior descending artery Impaired Ventricular function o Decreased SV o Deacreased CO o Ejection Fraction o Increased end diastolic ventricular pressures Electrical Instability o Arrhythmias present Most Common Restrictive Diseases 1. Atelectasis 2. Sarcoidosis ECG Info about: Rate, rhythm, conduction, areas of infarct, hypertrophy, electrolyte imbalances. PVCs: no P wave, bizarre and wide QRS followed by a long compensatory pause. Serious PVCs: > 6 per minute, paired sequential runs, multifocal, Ron T phenomena Ventricular fibrillation: erratic activity without QRS complexes, no effective CO, clinical death within 4 – 6 minutes. Atrial arrhythmias: Abnormal P-waves o Rhythm may be irregular o Rapid rate with atrial tachycardia o Cardiac output is maintained, may precipitate ventricular failure 2 Types of Stress Tests 1. Treadmill and cycle ergometry (leg or arm) - allow for precise calibration of the exercise workload. 2. Step test (upright or sitting) - used for fitness screening healthy population Diagnostic Imaging for Heart and Lungs 2. Heart a. Chest X-ray: abnormalities of lung fluids, overall cardiac shape and size aneurysm. b. Myocardial perfusion: used for MI and ischemic disease; Thalium – 201 scan, - Radioisotopes concentrate in normal tissue but not in ischemic or infracted tissue, used to identify myocardial blood flow, areas of stressed – induced ischemia. c. ECG: Noninvasive to visualize internal structures (size of chambers, movement of valves, septum, abnormal wall movement) d. Cardiac Catheterization: Tube passes through heart into blood vessels with intro of a contrast medium into coronary arteries and subsequent x-ray - Provides info about anatomy of heart and great vessels, ventricular function, abnormal wall movements - Allows determination of ejection fraction (EF) e. Central line (Swan-Ganz catheter): inserted through vessels into right side of heart - Measures central venous pressure, pulmonary artery pressure, pulmonary capillary wedge pressure. 3. Lungs a. Chest X-ray: 2-dimensional film to detect presence of abnormal material(exudate, blood) or a change in pulmonary parenchymal (fibrosis, collapse) b. CT Scan: Cross-sectional plane of the body c. Ventilation perfusion (v/q): matches the ventilation pattern of the lung to the perfusion pattern to identify the presence of pulmonary emboli. d. Fluoroscopy: Continuous x-ray beam allows observation of diaphragmatic excursion Non-systems Therapeutic Modalities 1. Superficial Thermotherapy - Indications: Joint stiffness Musculoskeletal pain Muscle spasm Prepare for e-stim, passive and active Subacute and chronic traumatic and inflammatory conditions - Contraindications: Acute and subacute traumatic and inflammatory Decreased circulation and/or sensation DVT Impaired cognitive function Malignant tumors Tendency toward hemorrhage or edema Very young and very old patients A. Hot Packs: - Canvass filled with silica gel immersed between 165 -170° - 20 – 30 min B. Paraffin Bath: - Mixture melt (paraffin wax and oil mixture) 125° - 127° - Tx: 15 – 20min - Indications: Painful joints due to arthritis in subacute or chronic phase Joint stiffness of hands and wrist - Contraindications: Allergic rash Open wounds Recent scars and structures Skin infections C. Contrast Bath: - Alternate hot and cold - Decreased pain and swelling - Increased circulation - Water temp around 40°C (104°F) for hot, 15°C (59°F) for the cold - In subacute: 3 – 4 min hot to 1 min cold - Tx: 20-30min end with hot immersion D. Hydrotherapy - Used for debridement and loosening of dressings - Full body immersion (hubbard tank) Water temp < 38°C (100°F) - Chronic conditions: 37.2 - 40°C (99-104°C) If patient has PVD, cardiac problems or open wounds, temp < 38°C (100°F) Indications: Decubitus ulcers Open wounds/burns Post surgical conditions or fracture of hip Subacute and chronic musculoskeletal conditions of neck, shoulder, back RA 2. Cryotherapy - Indications: Acute and chronic traumatic and inflammatory condition Edema Muscle spasm Musculoskeletal pain Thermal burns - Contraindications: Impaired circulation Impaired sensation PVD Neuropraxia Raynaud’s phenomenon Sensitivity/allergy to cold A. Cold Pack - Temp: 0 - 10°F - Tx time: 10 – 20 min B. Ice massage - Tx time: 5-10min 3. Deep Thermotherapy - Indications Joint contractures Musculoskeletal pain Muscle spasm Subacute and chronic traumatic condition - Contraindications acute infections impaired circulation, cognitive function or sensation malignancy thoracic area containing pacemaker very young or old patients A. Ultasound - Deep aching pain = overheating periosteal tissue => reduce intensity immediately - Indications - - Open wounds Neuromas Periarticular condition Contraindications acute inflammatory joint pathology healing fracture thrombophlebitis radioactive isotopes Precautions Metal implants Osteoporosis Plastic implants Primary repair of tendons or ligaments or scar tissue B. Phonophoresis 4. Other Physical Agents A. Mechanical Spinal Traction - Indications Degenerative disc Discogenic pain HNP (disc protrusion) Joint stiffness or disease Meniscoid blocking muscle spasm Nerve root impingement Subacute or chronic joint pain - Contraindications impaired cognitive function spinal tumors and infections Spondylolisthesis RA OP Very young and very old patients Vascular compromise (verterbral artery syndrome) - Precautions Acute inflammation aggravated by traction Acute strain and sprains Claustrophobia Hiatal hernia Joint instability Pregnancy TMJ problems with use of halter, remove dentures use mouth piece B. Cervical traction - 20 – 30 pounds =distraction of vertebral bodies C. Lumbar Traction - 25 – 65 punds = effect change at spinal segments - Neck position 0 - 5° to increase space at C1 – C4 20 - 30° for C5 – C7 0° for disc dysfunction - Lumbar position Spinal stenosis Hip/knee (90/90) position Posterior HNP Prone without pillow preferred Intermittent Compression - Indications Chronic Edema Lymphedema (postmastectomy) Stasis ulcer Traumatic edema Venous insufficiency Amputation - Contraindications Acute or infected treatment area Acute DVT or pulmonary edema Arterial insufficiency Cancer Decreased skin sensation Kidney, cardiac insufficiency HTN Cognitive dysfunction Obstructed lymph channels Very young and frail elderly 5. Electrotherapy - Indications Pain modulation Muscle spasm Impaired ROM Muscle re-ed Disuse atrophy (muscle weakness) Soft tissue repair (wound healing) Edema reduction Spasticity (reduce hypertonicity) Denervated muscle - Contraindications Healing fractures - Areas of active bleeding Malignancies or phlebitis treatment area Superficial metal implants Pharyngeal or laryngeal muscles Demand-type pacemaker Myocardial disease Precautions Impaired sensation Severe Edema A. Iontophoresis - Therapeutic ion must be placed under electrode of similar charge to “push” chemical past the skin into deeper tissue - Contraindications Impaired skin sensation Allergy or sensitivity to therapeutic agent or direct current Recent scars, cuts, bruises, broken skin Metal in or near treatment area. - Negative Salicylate (pain relief) Acetic acid (calcium deposits) Dexamethasone (anti-inflammatory) - Positive Calcium (muscle spasm) Lidocaine (pain relief) Magnesium (muscle spasm) Zinc (dermal ulcers) Copper (fungal infections) B. TENS (Transcutaneous Electrical Nerve Stimulation) - Impulses stimulating large A-fiber afferents, can act to blcok the pain impulses (gate control theory) - Body’s own endorphins/enkephalins to inhibit pain or pain transmission - Contraindications Demand type pacemakers (anywhere on body) Over chest area of patients with cardiac dysfunction Over eyes, laryngeal, pharyngeal muscles, head and neck of patient after CVA or epilepsy. Application to mucosal membrane =Physiological effects of general heat Increased: CO, metabolic rate, HR, RR, vasodilation Decreased: BP, muscle activity, blood to internal organs, blood to resting muscle, SV Physiological effects of local heat Increased: Blood flow, capillary permeability, elasticity of non-elastic tissues, metabolism, vasodilation, edema (capillary permeability). Decreased: Joint stiffness, muscle strength, muscle spasm, pain. Indications for superficial thermotherapy Modulate pain, increase CT extensibility, reduce/eliminate ST inflammation/swelling, accelerate rate of healing, reduce joint restriction/muscle spasm Precautions for superficial thermotherapy Cardiac insufficiency, edema, impaired circulation, impaired thermal regulation, metal in treatment site, open wounds Contraindications for superficial thermotherapy Acute/early-subacute trauma/inflammation, decreased circulation/sensation, DVT, impaired cognition, malignancy, tendancy towards hemorrhage or edema, very young/old Parameters: Hot packs Immersed in water heated at 165-170 degrees F Eight layers of toweling between pack and patient Treatment time: 20-30 mins Parameters: Paraffin bath Paraffin wax/oil mix at ~6:1 ration Melts at 118-130 deg F Rx temp: ~125 deg F Self-sterilizing at 175-180 deg F Treatment time: 15-20 mins Remove/cover jewlery Wash part, check for infection and open areas 6-12 layers of paraffin Wrapped in plastic/wax paper after it solidifies Covered with several layers of toweling Place in comfortable or elevated position for 15-20 mins Alternative part can remain in the bath Paraffin contraindications Allergic rash, open wounds, recent scars and sutures, skin infections Parameters: Hydrotherapy Temp - Whirlpool: 103-110 Hubbard tank: 100 PVD: 95-100 Open wounds: 92-96 Treatment time: 20 mins (up to 30 if other procedures also being performed) Hydro precautions Use liners for patients with burns/wounds/blood-borne pathogens Add disinfectant and if open wounds are present Standard precautions in infected environment (goggles, gown etc. - splashing) Decreased temp sensation, impaired cognition, incontinence, confusion/disorientation, deconditioned state, hydrophobia Hydro indications Pressure ulcers, open burns/wounds, post-hip #, post-surgical hip conditions, subacute/chronic conditions of neck/shoulders/ back, RA Hydro contraindications Bleeding, wound maceration, cardiac instability, profound epilepsy Water pick parameters 4-8 psi - can be increased in presence of large amounts of necrotic tissue or tough eschar Decrease pressure if bleeding occurs, near a major vessel, or if pt complains of pain Treatment time usually 5-15 mins Aquatic therapy parameters Temp: 92-98 deg F Treatment time varies with pt. tolerance Open wounds and skin infections must be covered Aquatic therapy contraindications Incontinence, UTIs, severe epilepsy, unprotected open wounds, unstable BP, severe cardiopulmonary dysfunction Physiological effects of general cold application Decreased: Metabolic rate, HR, RR, venous BP Increased: Blood flow to internal organs, CO, SV, arterial BP, shivering (when core temp drops) Physiological effects of local cold Decreased: Blood flow, capillary permeability, elasticity of non-elastic tissues, metabolism, muscle spasm, muscle strength (after 5-10 mins), spasticity, vasoactive agents Increased: Joint stiffness, pain threshold, blood viscosity, muscle strength (in first 5 mins) Vasoconstriction causes skin blanching at center with hyperemia due to histamine reaction around edge of the contact area. "Hunting reaction" Cyclic vasodilation/vasoconstriction following prolonged cold exposure (>15 mins). Occurs mostly in hands, feet and face where atriovenous anastomoses are found. Cold urticaria Cold hypersensitivity Erythema of the skin with wheal formation associated with severe itching due to histamine reaction. Other adverse effects of cold due to hypersensitivity Facial flush, eyelid puffiness, respiratory problems, anaphylaxis (decreased BP, increased HR), with syncope Related to histamine release Indications for cryotherapy: Modulate pain, reduce/eliminate inflammation/swelling, reduce muscle spasm, and reduce spasticity. Cryotherapy precautions: HTN, impaired temperature sensation, open sound, over a superficial nerve, very old/young Cryotherapy contraindications: Cold hypersensitivity, cold intolerance, cryoglobulinemia, PVD, impaired temp sensation, Raynaud's Cold/ice pack parameters Wrap pack in damp towel Packs maintained at 0-10 deg F Treatment time: 10-20 mins If using ice towel replace towel every 45-60 secs Ice massage parameters Apply to area no larger than 4x6" Apply slowly (2" sec), overlapping circles or long strokes Do not massage over bony prominences or superficial nerves Treatment time: 5-10 mins or until anagesia occurs Vapocoolant spray parameters Indications: Reduce spasm, desensitize trigger points Invert container, hold ~18-24" from treatment area Spray at 30 deg angle and sweep at 4" per sec Allow liquid to completely dry before next sweep Muscle should be passively stretched before and during application Treatment time: 10-15 mins Contrast bath parameters Indications: Pain modulation, PVD, sprains, strains, trauma (after acute phase ends) effectiveness at raising deep temperature is questioned Begin in 80-110 deg F water - 4 mins Cold water (55-65) for 1 min Continue in sequence of 1:4 End in warm water - ending in cold water may be more beneficial if goal is to reduce edema Treatment time: 20-30 mins Contrast bath contraindications Advanced atherosclerosis, arterial insufficiency, loss of sensation to heat and cold. Ultrasound: Transducer head size, Range from 1-10 cm 5cm most common Should be relative to treatment area size: wrist- 1cm, shoulder/leg - 5cm Ultrasound: Spatial average intensity Total power (watts) divided by area (cm2) of transducer head Typically the measurement used in documenting US treatments (0.25 w/cm2 - 2.0 w/cm2) (measure of intensity) Ultrasound: Beam non-uniformity ratio Ratio of spatial peak intensity to average intensity Lower BNR = more uniform energy distribution and less risk of tissue damage Should be between 2:1 and 6:1 Ideal 1:1 is not technically feasible Ultrasound: Duty cycle the fraction of time the US is on over one pulse period Time on/time on+time off Duty cycle of 50% or less is considered pulsed Ultrasound: Structures with high attenuation High protein and collagen content - muscles, tendons, ligaments, capsules Ultrasound: Depth of penetration 3-5 cm At 3 MHz - greater attenuation in superficial tissues (e.g. TMJ) At 1MHz - increased heat production in deep layers due to less superficial scatter Ultrasound: Thermal effects Produced by continuous US at 0.5-3 W/cm2 (intensity will vary depending on tissue type and pathology) Increased: Tissue temp, pain threshold, collagen extensibility, enzyme activity, tissue perfusion, temp at tissue interfaces. Alteration of nerve conduction velocity. Excessively high temps may produce sudden, strong ache due to overheating periosteal tissue - reduce intensity or increase surface area. Ultrasound: Non-thermal effects Generated by very low intensity or pulsed US. Typically duty cycles of 20-50% Cavitation: Alternating compression and expansion of small gas bubbles caused by mechanical pressure waves. Stable cavitation: Bubbles resonate but no tissue damage. May be responsible for diffusional changes in cell membranes. Unstable cavitation: Secure collapse of gas bubbles - can result in local tissue destruction due to high temps. Acoustic streaming: Movement of fluids along the boundaries of cell membranes resulting from mechanical pressure wave. May produce: Alterations in cell membrane activity increase: cell wall permeability, intracellular calcium, macrophage response, protein synthesis. May be of some value in tissue healing. Ultrasound: Goals/indications Modulate pain - increase CT extensibility, reduce inflammation, accelerate healing rate, reduce joint restriction/muscle spasm. Ultrasound: Precautions Acute inflammation, breast implants, open epiphyses, healing fractures. Ultrasound: Contraindications Impaired circulation/cognition/sensation Thrombophlebitis, joint cement, plastic components, over vital areas (ear, brain, heart, eye, cervical ganglia, carotid sinuses, reproductive organs, SC, pacemakers, pregnant uterus) Ultrasound: Procedures - Direct content Apply generous amount of coupling medium Move head slowly in overlapping circles or long strokes Do not cover an area greater than 2-3x size of the ERA per five minutes of treatment While head is moving turn up intensity to desired level - lower intensities for acute conditions or thin tissue; higher intensities for chronic conditions or thick tissue. Treatment time: 3-10 mins depending area, intensity, condition and frequency Ultrasound: Procedures - indirect contact (water immersion) Use with irregular bod parts Plastic container preferred to decrease reflection Place part in water Place sound head in water, 0.5-1" from skin surface at right angle to body part Move head slowly - if using stationary technique decrease intensity or use pulsed US Turn up intensity to desired level Periodically wipe off any air bubbles that form on sound head or body part during treatment Ultrasound: Procedures - indirect contact (fluid-filled bag) Thin-walled bag over irregular bony surface Not widely used Place sound head inside bag, apply coupling agent to skin and place bag over treatment area Move head slowly within the bag, do not slide bag on skin Increase intensity to desired level Ultrasound: Phonophoresis Use of US to drive medications through the skin into deeper tissues Local analgesics (lidocaine) Anti-inflammatory (dexamethasone, salicylates) Method is similar to direct contact except medicine is used as part of coupling agent Intensity: 1-3 W/cm2 Treatment time: 5-10mins Low intensities and longer time is more effective to introduce drug to skin Traction: Goals/indications Decrease: Joint stiffness, meniscoid blocking, muscle spasm, DJD, disc protrusion Modulate disc pain, sub-acute/chronic pain, reduced nerve root impingement Traction: Precautions Acute inflammation aggravated by traction, acute strains/sprains, claustrophobia, hiatus hernia, joint instability, osteoporosis, pregnancy, TMJ problems with halter use. Traction: Contraindications Impaired cognition, RA, spinal tumors, spinal infections, spondylolysthesis, vascular compromise, very old/young. Traction: Cervical halter Pull of ~7% of body weight Seated or supine Head halter under occiput and mandible, attached to cord or spreader bar Slack is removed 0-5 deg flxn to increase IV space at C1-C5 25-30 deg flxn to increase IV space at C5-C7 0 for disc dysfunction Facet joint separation may require 15 degrees of neck extension Traction applied to occiput, not chin If pt. experiences discomfort at TMJ, stop and adjust halter Traction: Cervical sliding device Head placed on padded headrest which positions the neck in 20-30 deg flxn Adjustable neck yoke tightened to firmly grip below mastoid Head strap across forehead Device attached to spreader bar Acute phase: Disc protrusion, elongation of soft tissue, muscle spasm: 10-15 lbs or 7-10% of BW Joint distraction ~20-30 lbs 5-10 mins for acute conditions and 15-30 mins for other conditions. Duty cycle 1:1 - except joint distraction best at 3:1 Traction: Lumbar Split table (minimize friction) Supine, pillow under knee or small bench under lower leg Prone may be preferable in case of posterior herniated disc 45-60 deg hip flxn for L5-S1 75-90 deg hip flxn for L3-4 Apply pelvic harness with top edge above iliac crest Attach thoracic harness with inferior margin slightly below ribs Thoracic harness counteracts pull of pelvic harness Acute: 25-40 lbs Disc protrusion, spasm, elongation of soft tissues: 25% BW Joint distraction: 50 lbs or 50% of BW 5-10 mins for herniated disc; 10-30 mins for other conditions Intermittent Mechanical Compression Pneumatic Applies pressure to limb via inflatable sleeve Single compartment=uniform circumferential pressure Multiple compartments =Applies pressure sequentially (greater pressure in distal compartments) Cold can be applied simultaneously - coolant pumped through sleeve Intermittent Mechanical Compression: Physiological effects Increased interstitial fluid pressure - fluids forced into lymphatic and venous return systems = reduced fluid volume in limb Intermittent Mechanical Compression: Goals/indications Amputation, arterial insufficiency, decrease chronic edema, Post mastectomy lymphedema, stasis ulcer, venous insufficiency. Intermittent Mechanical Compression: Precautions Impaired sensation, malignancy, uncontrolled HTN, Obstructed lymph/venous return Intermittent Mechanical Compression: Contraindications Acute inflammation, DVT, acute pulmonary edema, diminished sensation, cancer, edema with cardiac or renal impairment, impaired cognition, infection in treatment area. Obstructed lymph channels, very old/young patients Intermittent Mechanical Compression: Procedures Check BP Comfortable position with limb at ~45deg elevation, abd 20-70 Apply stocking, no wrinkles Apply appliance Edema reduction: Inflation/deflation ratio ~3:1 (45:15) Shape stump: 4:1 often used Power on, slowly increase pressure to desired level Usually an elastic bandage/compression stocking used to retain reduction before dependant position allowed Intermittent Mechanical Compression: Pressure Pt.’s BP determines setting Some manufacturers recommend the pressure never exceed diastolic Others advise pressure should fall between diastolic and systolic. Numbness, tingling, pain, pulse should not be felt by pt. during treatment Intermittent Mechanical Compression: Treatment time depends on tolerance Minimum daily treatment: Lymphedema - 2 hrs to two 3 hr sessions Traumatic edema - 2 hrs Venous ulcers - 2.5 hrs/3x/week to two 1 hr periods Stump reduction - 1 hr to 3 hr sessions totalling 4 hrs Intermittent Mechanical Compression: Indications Chronic edema, lymphedema, stasis ulcer, traumatic edema, venous insufficiency, amputation. CPM: Physiological effects Accelerate rate of intra-articular cartilage regeneration, tendon and ligament healing Decrease edema and joint effusion Minimize contractures, decrease post-op pain, increase synovial fluid lubrication of joint, Improve circulation, prevent adhesions, improve nutrition to articular cartilage and periarticular tissues, and increase ROM CPM: Indications Post-immobilization #, tendon/ligament repair, total knee/hip replacement CPM: Precaution Intracompartmental hematoma from anticoagulants CPM: Contraindications Increases in pain, edema of inflammation following treatment CPM: Procedure (post-op knee) Applied immediately Set at 1-4 minute cycles At knee ROM may be 20-40 deg flxn initially, increased 5-10 as tolerated Usually goal of 110-120 flxn Treatment time: 1 hr 3x daily to 24 hr continuous Duration: 1-3 weeks or until goals achieved Tilt Table: Physiological effects Stimulate postural reflexes to counteract orthostatic hypotension Facilitate postural drainage Gradual loading of one or both LLs Begin active head/trunk control Provide positioning for stech of hip flexors, knee flexors PFs Tilt Table: Indications Prolonged bed rest, immobilization, SCI, TBI, orthostatic hypotension, spasticity Tilt Table: Procedure Supine Abdominal binder, long elastic stockings or tensor bandaging to counteract orthostatic hypotension may be used Secured by straps - Proximal to patella, pelvis, chest under axilla Table gradually raised Can be maintained as long as 30-60 mins - initially no longer than 45 mins 1-2x daily Monitor vitals Massage: Physiological effects Increased venous and lymph flow, stretching and loosening of adhesions, edema reduction, sedation, muscle relaxation, modulate pain. Massage: Contraindications Acute inflammation in area, acute febrile condition, severe atherosclerosis, severe varicose veins, phlebitis, areas of recent surgery, thrombophlebitis, arrhythmia, malignancy, hypersensitivity, severe RA, hemorrhage to area, edema due to kidney dysfunction, heart failure and venous insufficiency. Electrical Stimulation: Characteristics of nerve/muscles cells Duration of 1 ms is enough to depolarize a nerve cell, too short to stimulate a muscle cell <0.05 ms with low intensities can depolarize sensory nerves <1 ms required for motor nerves >10 ms with high intensities needed for denervated muscle Rate of rise must be rapid enough to prevent accommodation (square wave = instantaneous rise) Electrical Stimulation: Rheobase Intensity of the current (have a long duration) required to produce a minimum muscle contraction Electrical Stimulation: Chronaxie Pulse duration of stimulus at twice rheobase intensity. Chronaxie of a denervated muscle is greater than 1 ms Electrical Stimulation: Motor point: Area of greatest excitability on skin Small current generates a muscle response In innervated muscle - located at/near where motor nerve enters muscle, usually over belly denervated muscle - located over muscle distally towards insertion Electrical Stimulation: Types of muscle contraction Low freq pulse (1-10/sec) produces brief twitch with each stim Increasing number of stim progressively fuses twitches to tetanic contraction Asynchronous/worm-like (vermicular) muscle response is noted in denervated muscle Electrical Stimulation: Amperage Rate of flow of electrons Electrical Stimulation: Voltage Force driving electrons Electrical Stimulation: Ohm's law Current is directly proportional to voltage and inversely proportional to resistance. Electrical Stimulation: Monophasic waveform, Direct/galvanic Unidirectional flow Has either positive or negative charge Electrical Stimulation: Biphasic waveform Alternating current Bidirectional flow Half cycle above baseline, half below Two phases = one cycle Zero net charge if symmetrical Electrical Stimulation: Polyphasic waveform Russian current or interferential current Biphasic current modified to produce three or more phases in a single pulse Electrical Stimulation: Surge mode Gradual increase in decrease in intensity over finite period of time Electrical Stimulation: Ramped mode Gradual rise in intensity with maintenance of intensity at a selected lever for a given period of time, then gradual or abrupt decline. Electrical Stimulation: Indications Pain modulation (gate control or descending inhibition), Decrease muscle spasm, Impaired ROM, Edema, Muscle re-education (assistive, feedback, coordiation), disuse atrophy, wound-healing, decrease spasticity, stimulate denervate muscle Electrical Stimulation: Methods to Decrease muscle spasm Muscle fatigue - tetanic contraction Muscle pump - interrupted/surge modulation, increase circulation Muscle pump and heat - Combination of electric stim and US to increase tissue temp and produce muscle pump at same time Electrical Stimulation: Methods to increase ROM mechanical stretching - used when muscle strength in deficient of dysfunction (e.g. spasticity) prevents adequate joint movement Electrical Stimulation: Wound healing - Pulsed currents Interrupted modulations Improved circulation (muscle pump) - improved tissue nutrition and waste metabolism Electrical Stimulation: Wound healing - Monophasic Low volt continuous, high volt pulsed Low amp for 30-60 mins -Restores electrical charges at wound -Disruption of bacterial DNA, RNA synthesis, cell transport -Increased ATP concentration, amino acid uptake, protein and DNA synthesis -Attraction of cells: Inflammation - Macrophages (+ve), mast cells (-ve), neutrophils (+ve/-ve) Proliferation - Fibroblasts (+ve) Wound contraction - Alternating (+ve/-ve) Epithelialization - Epithelial cells (+ve) Electrical Stimulation: Edema reduction Muscle pump - increase lymph and venous flow Electrical field phenomenon - Effect of electrical charge in interstitial proteins increase lymph and venous flow. Electrical Stimulation: Spasticity Fatigue of agonist Reciprocal inhibition - stimulate antagonist, inhibit agonist Electrical Stimulation: Stimulate denervated muscle Goal is to decrease effects of disuse and shorten recovery time May be deleterious to denervated muscle by: Interfering with regeneration of NMJ and subsequent reinnervation Traumatizing hypersensitive denervated muscle Financial cost and prolonged treatment time required until reinnervation are additional factors to consider. Electrical Stimulation: Contraindications Healing fractures, areas of active bleeding, malignancies or phlebitis in area, superficial metal implants, pharyngeal/laryngeal muscles, demand-type pacemaker, myocardial disease Electrical Stimulation: Precautions Areas of impaired sensation and severe edema Electrical Stimulation: Electrodes Two required - one active (stimulating), one dispersive Active placed on motor point Dispersive placed on treatment site or at a remote site Current density is relative to electrode size (small size, high density, strong stim) Electrode size should be relative to size of treatment site Electrical Stimulation: Electrode placement Unipolar/monopolar: Single or bifurcated active electrodes placed over treatment area. Usually larger size dispersive electrode placed ipsilaterally away from treatment area. Bipolar: Equal sized active and dispersive electrodes in same treatment area. Space between A and D electrodes should be at least the diameter of the active electrode and as far as practically possible. Greater space = less current density in intervening tissue - less risk of burns and skin irritation. Electrical Stimulation: Muscle strength/spasm/edema (muscle pump) Slowly increase intensity until muscle response observed 10-25 contractions may be sufficient depending on goal Muscle re-education sessions may last 10-30 mins Interrupted/ramped allows muscles to recover Ratio of 1:3 or more minimizes fatigue Use continuous to induce fatigue for spasm Electrical Stimulation: Iontophoresis Transport medications through skin Continuous, direct, monophasic Like charges repel like +ve ions move towards cathode where secondary alkaline reaction occurs (NaOH) -ve ions move towards annode where acid is produce (HCl) The number of ions transferred is directly related to the treatment duration, current density and ion concentration Electrical Stimulation: Iontophoresis ions Analgesia: Lidocaine, xylocaine (+ve) ; Salicylate (-ve) Calcium deposits: Acetate (-ve) Dermal ulcers: Zinc (+ve) Edema reduction: Hyaluronidase (+ve) Fungal infections: Copper (+ve) Hyperhidrosis: Water (+ve-ve) Muscle spasm: Calcium, magnesium (+ve) Musculo inflam: Hydrocortisone (+ve) ; Dexamethasone (-ve) Electrical stimulation: Iontophoresis Procedure To reduce alkaline effect the -ve electrode should be 2x size of +ve, regardless of which is the active electrode Dispersive electrode placed at either proximal or distal distant site, ~4-6" away Dosage = time x intensity Anode safe limit = 1.0mA/cm2; Cathode safe limit = 0.5mA/cm2 Duration is 10-40 mins Turn intensity up slowly Observe treatment area every 3-5 minutes Electrical stimulation: Iontophoresis contraindications As per general for elec stim Impaired skin sensation Allergy/sensitivity to therapeutic agent or direct current Denuded area or recent scars Cuts, bruises, broken skin Metal in or near treatment area Electrical stimulation: TENS: Physiological effects Pain inhibition through gate-control therory: Large A-beta fibers activate inhibitory interneurons in dorsal horn, inhibiting smaller A-delta and C fibers. Also enkephalin release which combines with opiate receptors to depress release of substance P. Pain modulation through descending pathways Noxious stim generates endorphin production. Efferents from PAG and other areas travel through dorsal SC and synapse with enkephalinergic interneurons in SC to presynaptically inhibit release of substance P from A-delta and C fibers. Electrical stimulation: TENS: Wave form Typically assymetrical biphasic Zero net direct current Pulsed monophasic sometimes used Electrical stimulation: TENS: ModulationContinuous or burst Electrical stimulation: TENS: Conventional (high-rate) Most common mode For acute or chronic pain Pain modulated via gate mechanism Onset of relief is fast with short duration of relief. Amplitude: Comfortable tingling, no muscle response Pulse rate: 50-80 pps Pulse duration: 50-100 microsec Duration: 20-60min Electrical stimulation: TENS: Acupuncture-like (strong low-rate) Chronic pain Endogenous opiate mechanism Onset of relief may take 20-40 mins Duration is long-lasting, 1+ hrs Amplitude: Strong, comfortable rhythmic twitches Pulse rate: 1-5 pps Pulse duration: 150-300 microsec Duration: 30-40 min Electrical stimulation: TENS: Brief, intense Used to provide rapid onset, short-term pain relief during painful procedures (debridement, deep frictions, mobs etc) Relief lasts ~30min-1 hour Amplitude: To tolerance Pulse rate: 80-150 pps Pulse duration: 50-250 microsec Duration: 15 min Electrical stimulation: TENS: Burst mode Combines characteristics of high and low rate TENS Stimulation of endogenous opiates but current is more tolerable than low-rate TENS Long-lasting pain relief (hours) Amplitude: Comfortable, intermittent paresthesia Pulse rate: 50-100 pps delivered in burst of 1-4 pps Pulse duration: 50-200 microsec Duration: 20-30 min Electrical stimulation: TENS: Hyper stimulation Point stimulation Use small probe to locate and stimulate acupuncture or trigger points. Multiple sites may be stimulated per treatment. Onset of pain relief is similar to acupuncture-like TENS. Long-lasting relief Amplitude: Strong, to pt's tolerance Pulse rate: 1-5 pps Pulse duration: 150-300 microsec Duration: 15-30 sec increments Electrical stimulation: TENS: Modulation mode Modulate other TENS modes to prevent neural/perceptual adaptation. Can change frequencies, intensities or pulse durations by 10+ % 1-2 times per second Electrical stimulation: TENS: Electrode placement several options: Acupuncture site, dermatome distribution of involved nerve, over painful site, proximal or distal to pain site, segmentally related myotomes, trigger points. Electrical stimulation: TENS: Contraindications Demand-type pacemaker Over chest of pt. with cardiac disease Over eyes, larynx, pharynx Head/neck of pt. following CVA or with epilepsy Mucosal membranes Electrical stimulation: High Voltage Pulsed Galvanic Stimulation Passage of HVPC decreases skin resistance due to current flowing toward skin capacitors rather than resistors. Thermal effects are negligible (little resistance to the current). Electrical stimulation: High Voltage Pulsed Galvanic Stimulation – Parameters Paired monophasic waveform Instantaneous rise and exponential fall of current Continuous, surged or pulsed Typically twin-peaked pulses of short duration Electrical stimulation: High Voltage Pulsed Galvanic Stimulation - Wound healing concept intact skin surface -ve with respect to deeper epidermal layers Injury to skin develops +ve potentials initially and -ve potentials during healing Absent or insufficient +ve potentials retard tissue regeneration Addition of +ve potentials initially through anode may promote or accelerate healing Electrical stimulation: High Voltage Pulsed Galvanic Stimulation - Wound healing parameters Amplitude: Comfortable tingling, paresthesia, no muscle response Pulse rate: 50-200 pps Pulse duration: 20-100 microsec Duration: 20-60 min\Both high volt pulse and low volt continuous can be used Clean and debride wound first and pack with sterile saline-soaked gauze. Place active electrode over gauze For bactericidal effect active electrode should be -ve For culture-free wound, AE should be +ve Electrical stimulation: High Voltage Pulsed Galvanic Stimulation - Indications Inflammation phase: Free from necrosis and exudates, promote granulation Proliferation phase: Reduce wound size (depth, diameter, tunneling) Epithelialization phase: Stimulate epidermal proliferation and capillary growth Electrical stimulation: Functional electrical stimulation (FES) Also called neuromuscular stimulation (NMES) Used as an alternative or supplement to orthotic devices Electrical stimulation: Functional electrical stimulation (FES) - parameters for shoulder subluxation Asymmetrical biphasic square Interrupted modulation Bipolar electrodes on supraspinatus and deltoid Amplitude: Tetanic contraction to tolerance Pulse rate: 12-25 pps Duration of treatment: 15-30 mins. 3x daily up to 6-7 hours. Duty cycle (on:off): 1:3 (2sec:6sec) progressing to 12:1 (24sec:2sec) Electrical stimulation: Functional electrical stimulation (FES) - parameters for DF assists Asymmetric biphasic square Pulse duration: 20-250 microsec Modulation: Interrupted by foot switch Amplitude: Tetanic contraction sufficient to decrease PF Pulse Rate: 30-300 pps Bipolar electrodes on peroneal nerve near head of fibula or on tibialis anterior Heel-switch contains pressure-sensitive contact which stops stimulation during stance phase and activates stimulation during swing phase. Hand switch also allows therapist to control stim during gait. Electrical stimulation: (EMG) Instrument used to measure motor unit action potentials (MUAP) generated by active muscles (measured in microvolts) Reinforces voluntary control Electrical stimulation: Electromyographic feedback (EMG) - electrodes Small electrodes for specific muscles, large for large muscles or muscle groups Two active and a single reference electrode (may be placed adjacent to active electrodes to minimize cross-talk) Active electrodes placed near motor point ~1-5cm apart, parallel to muscle fibers Active electrodes placed close together minimizes cross-talk, yields smaller, more precise signals. Active electrodes placed further apart detects from more than one muscle. Electrical stimulation: Electromyography feedback (EMG) - Procedure Quiet setting For weak muscles begin with electrodes widely spaced and instrument sensitivity high As pt's motor ability improves make it harder Use facilitation techniques Progress from simple to complex, functional movements Treatment time depends on pt tolerance For spastic muscle begin with electrodes close together and instrument sensitivity low to minimize cross-talk Progress to high sensitivity as pt gains ability to relax and perform functional activities Use relaxation techniques, imagery etc Electrical stimulation: (EMG) Criteria for pt selection Good vision, hearing, communication Good comprehension of simple commands Good concentration Good motor planning skills No profound sensory or proprioceptive loss