Staff training presentation, example 1
advertisement

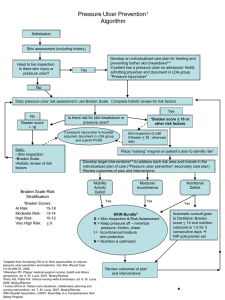
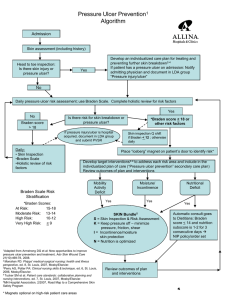
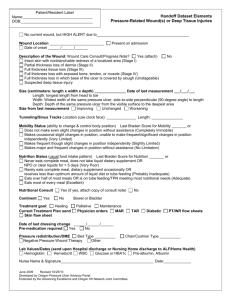
Braden Score + Skin Inspection + Interventions + Critical Thinking Pressure Ulcer Prevention Objectives: Identify risks of pressure ulcer development Differentiate between skin assessment and skin inspection Discuss interventions for pressure ulcer prevention Test your accuracy at scoring a Braden Scale Most pressure ulcers are preventable if patient risk is recognized in time for preventive actions to be initiated. Maklebust J., Sieggreen M.Y, (2001) Pressure Ulcers: Guidelines for Prevention and Mangement, 3rd ed. “Determining patient risk for pressure ulceration is greatly assisted by the availability of research-based instruments such as the Braden Scale” Maklebust, J., Sieggreen, M.Y., Sidor, D., Gerlach, M.A., Mauer, C., Anderson, C., (2005). Computer-based testing of the Braden scale for predicting pressure sore risk. Ostomy/Wound Management; 51(4):40-52 The Evidence • Detroit Medical Center nursing audits raised concern whether staff nurses accurately used the Braden Scale to calculate pressure sore risk. • In 2002 a learning/assessment module was instituted • 2,500 nurses at the facility were tested regarding their knowledge of pressure ulcer risk assessment and prevention using this module. Case Study: Mr. W.G. • • • • • • • • • 75-year-old male with Non-Hodgkins lymphoma, Alert and oriented Height 5’9”, Weight 160 lbs. Spends most of the day in bed. Makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently. Occasionally slides down to foot of bed, requiring some assistance to move back to the top. Able to walk a short distance to the chair with assistance Incontinent of stool Continent of urine – uses urinal as needed Skin occasionally moist from incontinence Hgb = 8.5, Serum Albumin 3.1 Admitting Orders: – Tube feeding formula 400cc q 4 hours per PEG – Dietician consult for tube feeding recommendations – Up in chair daily Test Question Using the Braden Scale, what is Mr. W.G.’s sensory perception score? A. B. C. D. 1 (Completely Limited) 2 (Very Limited) 3 (Slightly Limited) 4 (No Impairment) Test Question Using the Braden Scale, what is Mr. W.G.’s sensory perception score? A. B. C. D. 1 (Completely Limited) 2 (Very Limited) 3 (Slightly Limited) 4 (No Impairment) Test Question Using the Braden Scale, what is Mr. W.G.’s moisture score? A. B. C. D. 1 (Constantly Moist) 2 (Very Moist) 3 (Occasionally Moist) 4 (Rarely Moist) Test Question Using the Braden Scale, what is Mr. W.G.’s moisture score? A. B. C. D. 1 (Constantly Moist) 2 (Very Moist) 3 (Occasionally Moist) 4 (Rarely Moist) Test Question Using the Braden Scale, what is Mr. W.G.’s activity score? A. B. C. D. 1 (Bedfast) 2 (Chairfast) 3 (Walks Occasionally) 4 (Walks Frequently) Test Question Using the Braden Scale, what is Mr. W.G.’s activity score? A. B. C. D. 1 (Bedfast) 2 (Chairfast) 3 (Walks Occasionally) 4 (Walks Frequently) Test Question Using the Braden Scale, what is Mr. W.G.’s mobility score? A. B. C. D. 1 (Completely Immobile) 2 (Very Limited) 3 (Slightly Limited) 4 (No Limitations) Test Question Using the Braden Scale, what is Mr. W.G.’s mobility score? A. B. C. D. 1 (Completely Immobile) 2 (Very Limited) 3 (Slightly Limited) 4 (No Limitations) Test Question Using the Braden Scale, what is Mr. W.G.’s nutrition score? A. B. C. D. 1 (Very Poor) 2 (Probably Inadequate) 3 (Adequate) 4 (Excellent) Test Question Using the Braden Scale, what is Mr. W.G.’s nutrition score? A. B. C. D. 1 (Very Poor) 2 (Probably Inadequate) 3 (Adequate) 4 (Excellent) Test Question Using the Braden Scale, what is Mr. W.G.’s friction and shear score? A. 1 (Problem) B. 2 (Potential Problem) C. 3 (No Apparent Problem) Test Question Using the Braden Scale, what is Mr. W.G.’s friction and shear score? A. 1 (Problem) B. 2 (Potential Problem) C. 3 (No Apparent Problem) Test Question Based on Mr. W.G.’s total Braden Scale Score, indicate his level of risk for developing a pressure ulcer. A. B. C. D. E. 9 or less = Very high risk 10-12 = High risk 13-14 = Moderate risk 15-18 = Mild risk 19-23 = Generally not at risk Test Question Based on Mr. W.G.’s total Braden Scale Score, indicate his level of risk for developing a pressure ulcer. A. B. C. D. E. 9 or less = Very high risk 10-12 = High risk 13-14 = Moderate risk 15-18 = Mild risk 19-23 = Generally not at risk Detroit Medical Center Results • • • • • • • >2,500 nurses completed the computer-based Braden Scale learning module during the third quarter 2002 Each of the 5 case studies took nurses between 6 and 10 minutes to complete 75.5% of the nurses correctly rated the Braden Scale level “Not at risk” and “severe risk” levels were rated correctly more often than “mild risk”, “moderate risk”, and “high risk” levels Subscales with the lowest percentage of correct answers were moisture and sensory perception Moisture: Nurses had a difficult time differentiating between a score of 3 (extra linen change once a day) and 2 (linen must be changed at least once a shift) Sensory perception: This subscale is based on patient communication of discomfort and the ability to feel pain over “half of the body”. Unless these description were spelled out exactly in the case studies nurses tended to score the patient higher (with less risk) than the test writer did. “In addition to the Braden Scale pressure ulcer risk factors, evaluation of patients’ skin is an important concept for evaluating risk for pressure ulcers. Even if patients are rated “not at risk” according to the Braden Scale score, Braden recommends placing them in an “at risk” category if they have actual pressure ulcers, healed pressure ulcers, or persistently reddened areas of skin over bony prominences.” Maklebust, J., Sieggreen, M.Y., Sidor, D., Gerlach, M.A., Mauer, C., Anderson, C., (2005). Computer-based testing of the Braden scale for predicting pressure sore risk. Ostomy/Wound Management; 51(4):40-52 Skin Assessment • Performed every shift • Included documentation of skin: – – – – Condition Color Turgor Mucous Membranes Skin Inspection • Performed at least daily, more often if indicated • Physical examination of the intactness of the skin, specifically on bony prominences. Includes identification of the following abnormal skin conditions: – – – – – – – – – – – Abrasion Blister Bruising (due to pressure) Burn Denuded (missing the top layer of the skin) Erythema (redness) Hematoma Laceration Rash Skin Tear Wound PU Management Goals: • Identify individuals at risk for developing pressure ulcers and initiate early prevention programs • Implement appropriate strategies/plans to – – – – Attain/maintain intact skin Prevent complications Promptly identify or manage complications Involve patient and caregiver in self-management • Implement cost-effective strategies/plans that prevent and treat pressure ulcers WOCN Guideline for Prevention and Management of Pressure Ulcers (2003) PU Assessment 1. Evaluate individual risk for developing pressure ulcers. • • Risk assessment is more than determining an individual’s numerical score. It involves identifying the risk factors that contributed to the score and minimizing those specific deficits. Risk assessment should be performed on entry to a healthcare setting and repeated on a regularly scheduled basis or when there is a significant change in the individual’s condition, such as surgery or other decline in health status. PU Assessment 2. Identify high-risk settings, and groups to target prevention efforts to minimize risk. Settings o o Pressure ulcers usually develop within the first 2 weeks of hospitalization (Langemo et at., 1989) 15% of elderly patients will develop pressure ulcers within the first week of hospitalization (Lyder et al., 2001) Groups o o Seniors (>65) and children (<5) are at highest risk Individuals with SCI are considered high risk PU Assessment 3. Inspect the skin regularly. • Assess all bony prominences of “at-risk” individuals at least on a daily basis (Bergstrom & Braden, 1992). o o o • Supine position: Occiput, sacrum, heels Sitting position: Ischial tuberosities, coccyx Side-lying position: trochanters Special garments, shoes, heel and elbow protectors, orthotic devices, restraints, and protective wear should be removed for skin inspection. PU Assessment 4. Assess for immobility. • • Immobility is the MOST significant risk factor for pressure ulcer development Patients who have ANY degree of immobility should be carefully monitored for pressure ulcer development: • • • • • Non-ambulatory Confined to bed, wheelchairs, recliners and couches Have paralysis or contractures Wear orthopedic devices that limit function and range of motion Require assistance in ambulating, moving, turning, repositioning, getting out of bed or chairs PU Assessment 5. Assess for friction and shearing. • Friction: the mechanical force of two surfaces moving across each other; it damages surface tissues, causing blisters and abrasions • • Individuals who cannot lift themselves with repositioning are at high risk for friction injuries. Shear: the mechanical force that is parallel rather than perpendicular to the skin, which can damage deep tissue such as muscle • Occurs when the head of the bed is elevated and the individual slides downward (Makelbust & Sieggreen, 2001) PU Assessment 6. Assess for incontinence. • • • Moisture from incontinence contributes to pressure ulcer development by macerating the skin. Fecal incontinence is a greater risk because the stool contains bacteria and enzymes that are caustic to the skin. In the presence of both urinary and fecal incontinence, fecal enzymes convert urea to ammonia, raising the skin pH. With a more alkaline skin pH, the skin becomes more permeable to other irritants (Ratcliff & Rodeheaver, 1999). PU Assessment 7. Assess nutritional status. • • • • • Malnutrition is associated with overall morbidity and mortality. Inadequate caloric intake causes weight loss and a decrease in subcutaneous tissue, allowing bony prominences to compress and restrict circulation. Stage III-IV sacral ulcers in the elderly have been found to be associated with low body weight, low pre-albumin, and inadequate nutritional intake relative to needs Patients with pressure ulcers have been found to have lower serum albumin and Hgb compared to those without pressure ulcers Serum albumin levels < 3.5g/dL. have been associated with increased pressure ulcer incidence in individuals with spinal cord injury PU Assessment 8. Assess laboratory parameters for nutritional status. • • No single measurement or combination of nutritional measurements has been determined to accurately predict the risk of developing pressure ulcers Standard measurements of protein: • • • • • Albumin (20 day half-life) Pre-albumin (2-3 day half-life) Transferrin Low serum albumin may reflect a chronic disease state rather than represent overall nutritional status. Total lymphocyte count is decreased in individuals with proteincalorie malnutrion. PU Assessment 9. Assess for history of prior ulcer and/or presence of current ulcer, previous treatments, or surgical interventions. • Presence of an ulcer or history of a prior ulcer puts a person at risk for additional pressure ulcers (Bergstrom & Braden, 1992; Berlowitz & Wilking, 1989). 10. Assess and monitor pressure ulcer(s) at each dressing change (van Rijswijk & Braden, 1989) • • • • Description: location, tissue type, drainage Condition of periwound skin Pain at ulcer site Patient/caregiver’s ability and willingness to adhere to prevention and treatment program. PU Assessment 11. Assess factors that impede healing status. • Comorbid conditions that complicate wound healing: o o o o o o • • • Malignancy Diabetes Cerebral vascular accident Heart failure Renal failure Pneumonia Limited or inaccessible resources may affect prevention and treatment Lack of compliance with pressure ulcer prevention measures complicates pressure ulcer healing Some medications interfere with wound healing: o o o Steroids Immunosuppressive agents Anti-cancer drugs PU Assessment 12. Assess/evaluate healing. • • • • Partial thickness ulcers (Stage II) should show evidence of healing within 1-2 weeks. Reduction of wound size following 2 weeks of therapy for Stage II-IV pressure ulcers has also been found to predict healing. If the condition of the patient or the wound deteriorates, reevaluate the treatment plan as soon as evidence of deterioration is noted. Routinely reassess wound dimensions, type of exudate, and tissue type when monitoring for wound healing. PU Assessment 13. Assess for the following potential complications associated with pressure ulcer(s): • • • • • • • Heterotopic bone formation Fistula Abscess Osteomyelitis Bacteremia Cellulitis Squamous cell carcinoma (Marjolin’s ulcer) Interventions for PU Prevention • • • • • • • • • Mattress overlay Low air loss bed Fluid air bed Boot/Splint Heels off bed HOB 30 deg or < Bed trapeze OOB/walk PROM • • • • • • • • • • Chair reposition Bed reposition RD assess Given supplement Condom catheter Barrier ointment Rectal pouch Flexi-Seal FMS Moisturize skin Turning Prompt Critical Thinking The key component needed to individualize a Pressure Ulcer Prevention Protocol so as to incorporate the possible interventions into a patient’s plan of care QUESTIONS????