Risk Assessment Project
advertisement
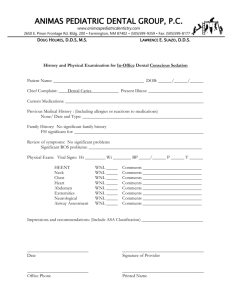
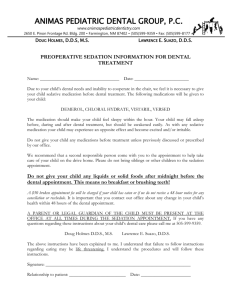
Risk Assessment Project JENNIFER KUO #1211 DH 88 Personal History Age: 31 years old Sex: Male Race: Caucasian Marital Status: Single Occupation: Air Traffic Controller Medical History Past Medical History Patient has a history of childhood asthma that is no longer observed. Past medication or drug use: None Family History Patient has a family history of diabetes from both parents. A positive history of diabetes doubles an offspring's risk of developing the disease (Franks, 2010). General Health Patient reports he is in good health. Review of Systems Head and Neck: None reported Neuromuscular System: None reported Respiratory: None reported Cardiovascular: None reported Gastrointestinal/Genito-urinary: None reported Allergies: None reported Hematological: None reported Behavioral: No disorders reported Current Medications Patient is not currently under any medications. Hospitalizations/Emergency Room visits: None reported Baseline Vital Signs: BP: 118/78 Pulse: 76 bpm Respiration: 16 breaths/min ASA Status with rationale: The patient is classified as ASA I due to the fact that he presents without any systemic disorders, not currently under any medications, and presents with a normal baseline blood pressure. Dental History Last dental exam 11/13/2010 Last hygiene appt 11/13/2010 Last radiographs FMX: 11/15/2010 Panoramic: 03/18/2011 Past treatments Orthodontic treatment for 18 months from 1992-1993 Extraction of third molars from all quadrants Present status Patient currently has no need for restorative treatment Currently on a six months interval for his recare appts (due May 13,2011) The patient is not compliant with his recare appts. Prior to his most recent hygiene visit, his last hygiene appt was over two years ago. Clinical Examination (Pre-treatment) Extra-oral examination Symmetry & Skin 3x4 mm macule on the labium inferius The macule developed within this past year Lymph nodes: WNL Thyroid & Trachea: WNL TMJ Slight crepitus on the right Deviation to the right upon closing Maximum opening 50mm Clinical Examination (Pre-treatment) Intra-oral Examination Occlusal relationship Overjet, overbite, underjet, crossbite: None Right side relationship - Molar: class I, Canine: class I Left Side relationship - Molar: class I, Canine: class I Clinical Examination (Pre-treatment) Intra-oral Examination (Con’t) Labial & Buccal mucosa: WNL Frenums: WNL Alveolar bone: WNL Tori: None present Floor of mouth: WNL Salivary glands/flow: WNL Tongue: WNL Tonsils: WNL Uvula: WNL Oropharynx: WNL Common deviations: Macroglossia **photo was not enlarged Gingival Description Maxillary Free Pink, firm, stippled, knifeedged Localized rolling on the buccal and lingual surfaces of #5 Attached: Pink, firm, stippled, smooth Mandibular Free Pink, blunted, firm, stippled Slight bulbous between #26,27 Rolled on the lingual of #23,24,25, 26 Attached Pink, smooth, stippled, firm Baseline Periodontal Record Generalized 2-3mm pocket, with localized 4mm pockets on distobuccal surface of #3, #4, distolingual surface of #3, mesiobuccal of #31, distolingual of #31. BOP: noted on #3M, 14M, 24F. MBI: 0%, PI: 100%, PFI: 0% Furcation: Class I on the buccal aspect of #2, 3, 14, 15, 19, 30. And Class I on the lingual aspect of #19. Mobility: none Recession 1mm- #2B, 14L, 15L, 20L, 21L, 29L, 28B, 2mm- #3B, 5B, 12B, 13B, 14B, 30L Calculus code: WLAC code light 2 AAP: Generalized moderate chronic periodontitis Areas of Concern: existing caries watch on the occlusal of #2 Perpetuating factor: Patient does not present with any restorations or malocclusion but his inadequate oral hygiene perpetuates his periodontitis Etiology: Patient is not compliant with his six month recare intervals his current homecare techniques demonstrate inadequate biofilm control as evidenced by his PI score and caries watch. Patient flosses occasionally Before Disclosing After Disclosing – Baseline Results PI: 100%, PFI: 0% Oral Hygiene Evaluation (Pre-treatment) Patient’s skill level Poor, as evidenced by his baseline PI score Patient demonstrates good dexterity but his current vertical and horizontal scrubbing method is less effective in removing biofilm Patient’s knowledge and awareness of dental and periodontal disease Patient possesses basic knowledge of dental diseases such as cavity development, but was unfamiliar with the cause and effects of periodontal diseases. Oral Hygiene Instruction Educated the patient on the modified bass technique. The patient presents with type I gingival embrasures and it is recommended that the patient continue using dental floss with the spool method, but increase its frequency The Tell-Show-Do method was employed for both techniques Caries Examination Existing caries and quality of restorations Caries watch on the occlusal surface of #2 which has been monitored by his dentist for the last three years. Caries Index The patient has a DMFS score of 21. This is determined by the following information: 1 decayed surface 20 surfaces from 4 missing/extracted teeth 0 filled/crowned teeth A DMFS score of 21 indicates that there are 21 affected surfaces and 107 out of a total of 128 surfaces are still intact. Evaluation of radiographs for caries and restorative needs Radiographs reveal no restorations The caries watch is not detectable radiographically Panoramic Radiograph •Per Dr. Liewen’s Assessment: •Generalized 2-3mm horizontal bone loss •Caries watch is not detectable on the radiographs, but is clinically visible. Nutritional Analysis Three day dietary analysis Patient has a tendency to skip breakfast Frequently consumes fast food meals high in fat and carbohydrates ex: McDonald's, Popeye’s, etc. Frequently snacks between meals and has a fondness for sugary sweets such as candy and brownies Commonly deficient in vegetables and dairy which consequently affected the patient's intake of essential vitamins such as Vitamin E The patient frequently does not meet the RDAs for many food groups Research Correlations According to Imamura, Lichtenstein, Dallal, Meigs, & Jacques (2009), specific dietary patterns such as the habitual consumption of “soft drinks, particularly caloric soft drinks, meat and processed meat, eggs, refined grains, and French fried potatoes were positive contributors to the dietary patterns associated with type II diabetes”. These same foods also appear within the patient’s dietary diary The nutritional habits coupled with the patient’s familial history of type II diabetes, increases the patient’s risk of developing the disease even more Nutritional counseling will focus on addressing these issues and offer healthy alternatives Analysis of Carbohydrate Intake 1st day – 120 minutes of exposure 2nd day – 120 minutes of exposure 3rd day – 140 minutes of exposure Avg total exposure for all three days – 126.67 mins. The high value is attributed to the frequent sugary snacks and carbohydrate rich foods at each meal Nutritional Food Pyramid Results – Day 1 Nutritional Food Pyramid Results – Day 2 Nutritional Food Pyramid Results – Day 3 Caries Risk Assessment Recommendations based on the patient’s need CAMBRA Assessment Based on CAMBRA, the patient is considered to be at high caries risk. He has an existing caries watch on the occlusal of #2 as evidenced clinically and diagnosed by his dentist. Furthermore, the patient presents with deep grooves and pits as well as exposed roots due to gingival recession Prognosis Poor - Although the status of the patient’s caries watch has not changed over the last three years, his current nutritional habits coupled with his ineffective tooth brushing technique and sporadic flossing regimen, categorizes the caries risk prognosis as poor. Emphasis will be placed on encouraging a healthier diet and OHI to raise the prognosis to an acceptable and good level. Brush 2x/day with fluoridated toothpaste (Prevident 5000 is also recommended) Floss regularly with dental floss Reduce the frequent consumption of sugary snacks and sodas; continue consumption of tap water (0.7ppm) Incorporate more fruits and vegetable in the diet Fluoride rinse (0.05% NaF, ACT, or Fluorigard) 2x/day Xylitol – after snacks and as a mint 3-5 times/day In-office fluoride varnish or tray Antibacterial rinse - Chlorhexine gluconate for 1 week/month Dental Hygiene Treatment Plan Rationale for tx plan and patient needs Patient demonstrates inadequate biofilm control as evident by his PI score of 100%. Patient also presents with an existing caries watch as well. Goal of dental hygiene tx Decrease patient’s caries risk and increase the prognosis level Encourage the development of oral hygiene habits to improve oral health Increase the patient’s understanding and awareness of the cause and effects of periodontal disease, as well as its sequence Dental Hygiene Treatment Plan First Appointment Interpretation of PI results, explanation of the role of carbohydrates and tooth decay, what periodontal disease is, sequence of periodontal disease development Because the patient demonstrates good dexterity, the modified bass technique will be introduced to the patient. Daily flossing with the spool method will be reinforced and encouraged. Employment of the tell-show-do method to ensure proper application of the techniques demonstrated. A goal of 25% plaque reduction was established to encourage the patient to improve their overall oral hygiene and practice the new techniques taught. Sealant recommendation for his deep grooves and pits on all mandibular molars 5% NaF in-office varnish is recommended due to the patient’s caries risk and recession. In addition to the in-office treatment, Prevident 5000 will also be recommended. Antibacterial rinse – 0.12% Chlorhexidine gluconate is recommended for 1 week/month for patient’s caries watch and prevention of future caries. Nutrition recommendation: Encourage the reduction of frequent in-between snacking Increase consumption of fruits and vegetables, and decrease consumption of sodas and retentive sweets Introduction of xylitol and healthier snack options Encourage the consumption of breakfast to reduce snacking habits. Dental Hygiene Treatment Plan Second Appointment – 3 Week Re-evaluation Analysis of the patient’s compliance with the aid of a second PI score Review and reinforced OHI provided at the first appointment. Modified bass technique Spool method of flossing Clinical Examination (Post Treatment) Extra-oral Examination Symmetry & Skin 3x4 mm macule on the labium inferius The macule remained unchanged and the same size Lymph nodes: WNL Thyroid & Trachea: WNL TMJ Slight crepitus on the right Deviation to the right upon closing Maximum opening 50mm Clinical Examination (Post Treatment) Intra-oral Examination Occlusal relationship Overjet, overbite, underjet, crossbite: None Right and Left side relationship Molar: class I, Canine: class I Labial & Buccal mucosa: WNL Frenums: WNL Alveolar bone: WNL Tori: None present Floor of mouth: WNL Salivary glands/flow: WNL Tongue: WNL Tonsils: WNL Uvula: WNL Oropharynx: WNL Common deviations: Macroglossia Gingival Description Max Free: Pink firm, stippled, blunted, localized rolling on the buccal and lingual surfaces of #5 Max attached: Pink, firm stippled, smooth Mand Free: Pink, blunted firm, slight bulbous between #26,27, rolled on the lingual of #23,24,25, 26 Mand attached: Pink, smooth, stippled, firm Clinical Examination (Post Treatment) Intra-oral Examination (con’t) Periodontal Record Generalized 2-3mm, with localized 4mm pockets on distobuccal surface of #3, #4, distolingual surface of #3, mesiobuccal of #31, distolingual of #31. BOP: noted on #2B, 12D, 30L MBI: 0% Furcation: Class I on the buccal aspect of #2, 3, 14, 15, 19, 30. And Class I on the lingual aspect of #19. Mobility: none Recession 1mm- #2B, 14L, 15L, 20L, 21L, 29L, 28B, 2mm- #3B, 5B, 12B, 13B, 14B, 30L After Disclosing – Post Treatment Results PI: 68%, PFI: 32% Post Instructions Status Patients compliance resulted in a 32% reduction in biofilm. Patient exceeded the improvement goal established during the first appointment. Based on the areas where biofilm remained, I recommend the patient continue his homecare regimen Recommended the use of an electric toothbrush “electric brushes are significantly more effective at maintaining low plaque levels compared to a manual brush with or without the daily use of floss” (Rosema et al., 2008) “Provides long-term biofilm control and improve gingival condition for more than 6 months compared to manual brushes with or without the use of floss”. (Rosema et al., 2008) Recommended the additional use of mouthrinses to aid with interproximal biofilm control as these are the areas the patient is missing “twice daily rinsing reduced P.gingivalis (64.5%), Veillonella sp. (56.6%, F. nucleatum (76.6%), and total anaerobes (74.9%) within the interproximal regions” (Teles & Teles, 2009) Even single 30 second rinses demonstrated a significant reduction (43.8%) 5 minutes later (Teles & Teles, 2009) Essential oil containing mouthrinses are “as effective as daily flossing in reducing interproximal plaque and gingivitis” (Teles & Teles, 2009) Referrals Patient was referred to his dental hygienist for hygiene services as dictated by his six month recare interval; Due May 13, 2011 Patient is also referred to a specialist for the macule present on his labium inferius Research First article Periodontal Disease and diabetes – review of the literature – BasconesMartinez et al. (2011) Analyzes the interrelationship between periondotitis and diabetes. Second Article: Diabetes family history: a metabolic storm you should not sit out – Franks (2010) Analyzes the contribution of family history to the development of diabetes and the mechanism of various genetic risk factors. Third Article: Generalizability of dietary patterns associated with incidence of type 2 diabetes mellitus – Imamura, Lichtenstein, Dallal, Meigs, & Jacques (2009) Analysis of the dietary patterns associated with type 2 diabetes Fourth Article: Comparison of the use of different modes of mechanical oral hygiene in prevention of plaque and gingivitis – Nanning et al. (2008) A study that analyzed the efficacy of powered toothbrush to their manual counterparts over a 9 month period. Research Con’t Fifth Article Comparison of the use of different modes of mechanical oral hygiene in prevention of plaque and gingivitis – Rosema et al. (2010) Analyzes the efficacy of the modified bass method Sixth Article Antimicrobial agents used in the control of periodontal biofilms: effective adjuncts to mechanical plaque control? – Teles & Teles (2009) Analyzed the efficacy of antimicrobial rinses