Updates in Treatment Options for Asthma and C.O.P.D. Patients
advertisement

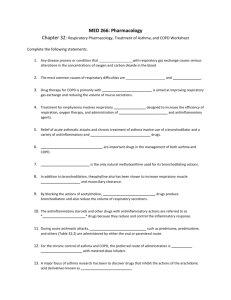
Updates in Treatment Options for Asthma and C.O.P.D. Patients Jim Holliman, M.D., F.A.C.E.P. Program Manager, Afghanistan Healthcare Sector Reconstruction Project Center for Disaster and Humanitarian Assistance Medicine, Uniformed Services University Bethesda, Maryland, U.S.A. Asthma and C.O.P.D. Lecture Objectives ƒ Know presenting signs & symptoms ƒ Be able to assess case severity ƒ Know medication and other treatment options ƒ Be able to formulate appropriate plans of care ƒ Know indications for admission Asthma : Definition & General Demographics ƒ Is a chronic inflammatory disorder of the airways, with airflow obstruction & airway inflammation, & recurring wheezing, dyspnea, & cough ƒ Prevalence, morbidity, & mortality has increased since 1980's ƒ Age - adjusted death rate for ages 5 to 34 increased 40 % from 1982 to 1992 ƒ About 5000 deaths per year in U.S. ƒ However Rowe and Camargo’s editorial in 2006 notes improved control and decreasing mortality in some countries ƒ About 2 million E.D. visits in U.S. per year This prevalence trend is still true Morbidity and mortality aspects of asthma Triggers of asthma Additional triggers of asthma Markers of a Potentially Fatal Asthma Attack ƒ Historical factors : –Hyperacute exacerbation –Lack of steroid use –Non-compliance –Psychiatric illness –> 3 hospital admissions –Prior intubation or barotrauma ƒ Physical findings : –Altered mental status –Diaphoresis –Inability to speak –PEFR < 100 L / min. Diagnostic Assessments to Consider for Asthma ƒ ƒ ƒ ƒ ƒ Peak Expiratory Flow Rate (PEFR) Pulse oximetry Arterial blood gas (ABG) Hematology & chemistry studies Chest X-ray (CXR) PEFR Considerations for Asthma ƒ Probably the single most useful assessment test ƒ Can stratify patients into severity groups : – < 25 % : Severe (impending resp. failure) – 25 to 50 % : moderate to severe – 50 to 70 % : mild to moderate – > 70 % : mild (can be discharged if at this value) ƒ Initial value not highly correlated with admission rate but higher risk if < 100 or improves < 60 with Rx ƒ Should usually not discharge if < 250 L / min. Pulse Oximetry Considerations for Asthma ƒ Trend toward lower initial values correlating with higher chance of admission, but not very sensitive ƒ Especially helpful in patients unable to perform PEFR and in kids ƒ Can be at normal levels in some with severe bronchospasm ABG Considerations for Asthma ƒ Initial ABG is poor predictor of outcome and rarely influences therapy ƒ NOT recommended routinely ƒ Indications : –Suspected respiratory failure –Altered mental status (need to know pCO2) –Pulse oximeter unable to track, & hypoxia is suspected –Worsening despite therapy Hematology and Chemistry Studies for Asthma ƒ Generally are NOT needed for most cases ƒ WBC count NOT reflective of severity or associated infection ƒ Most patients are not dehydrated, and do not have electrolyte abnormalities (except pseudohypokalemia from beta agonists) ƒ Only useful test might be theophylline level if the patient is taking a methylxanthine CXR Considerations for Asthma ƒ NOT routinely needed for "typical" exacerbations ƒ May be needed for : –New onset asthma (especially in kids) –Unclear Dx (e.g., R / O CHF, foreign body, etc.) –Asthma refractory to treatment –Respiratory failure –ETT placement –Strong clinical suspicion for infection –Chest pain (R / O pneumo - thorax or - mediastinum) 26 year old male with asthma and chest pain Same patient with arrows denoting pneumomediastinum General E.D. Management Scheme for Asthma ƒ Triage ƒ Primary treatments : –Beta agonists –Corticosteroids ƒ Secondary (or "refractory") treatments : –Anticholinergics –Magnesium, leukotriene inhibitors, Heliox, antibiotics, ketamine, mucolytics ƒ Disposition Triage Considerations for Asthma ƒ All patients with acute asthma should be quickly taken to a monitored treatment area ƒ Initial nursing interventions : –Pulse oximetry –Oxygen by nasal prongs (or blow-by mask for kids) –Cardiac monitor (if moderate to severe) –PEFR –IV line if severe –Notify physician Main Therapy for Acute Asthma Exacerbations : Inhaled Beta Agonists ƒ MDI-spacer delivery may be equivalent to traditional nebulizer –The patient may think MDI Rx in E.D. will be ineffective since has already tried it at home ƒ Continuous nebulization may be more effective in severe cases, but no difference for moderate cases (although takes less E.D. personnel time) –Albuterol doses are 10 to 30 mg / hr for adults, 5 to 7.5 mg / hr for kids Choices for Short Acting Beta Agonists (SABA’s) • Albuterol (Ventolin, Proventil) – PO 0.1 to 0.2 mg/kg/dose up to 12 mg/day – MDI one to two puffs q 20 minutes X 3 or : – 2.5 mg of 0.5 % solution via nebulizer q 20 minutes X 3 • Levalbuterol (Xopenex) – R isomer of albuterol – MDI 1 to 2 puffs q 4 h – Not shown superior to racemic albuterol (but is more expensive) • Metaproterenol (Alupent) – Same doses for MDI and nebulizer as albuterol – No big comparative studies versus albuterol Considerations for Parenteral Use of Beta Agonists ƒ Subcutaneous may be useful for rare patient not able to receive aerosol –Terbutaline probably safest (0.01 mg/kg, max. 0.3 mg) –Epinephrine (same dose; causes more HBP) ƒ For "crashing" patient, give IV –0.1 mg diluted and via SLOW IV push –then 0.4 mcg/kg/min IV drip ƒ Prior to discharge, can give Susphrine (epi tannate in oil) SQ at 0.005 mg/kg (more useful for allergic reactions) although availability of this med has decreased Long Acting Beta Agonists (LABA’s) ƒ Salmeterol (Serevent) MDI 50 mcg bid ƒ Onset in 10 to 20 minutes & duration 12 hours ƒ Twice as expensive as albuterol ƒ Useful for nocturnal asthma ƒ May be useful prior to E.D. discharge to help prevent early relapse ƒ Formoterol (Oxis, Foradil) MDI 12 to 25 mcg bid ƒ Note FDA black box warning for these Clinical Use Guidelines for the LABA’s ƒ NOT to be used as monotherapy for long term control of asthma ƒ Recommended in combination with Inhaled Corticosteroids (ICS) for long term control in moderate and severe persistent asthma ƒ NOT to be used frequently or chronically before exercise because this may mask poorly controlled asthma Other Medications for Acute Asthma ƒ "Primary" Meds –Corticosteroids –Anticholinergics –Magnesium ƒ "Secondary" Meds –Methylxanthines –Ketamine –Heliox –Halothane –Leukotriene inhibitors Use of Systemic Steroids in Asthma ƒ Clearly shown to decrease admission & relapse rates ƒ Oral route is fine for most –40 to 60 mg prednisone / day for adults –2 mg / kg per day for kids –5 day duration best (typical length of attack) –taper usually not needed ƒ IV only for severe dyspnea, emesis, altered mental status, or intubated (IV versus PO shows same acute effects) ƒ Methylprednisolone, hydrocortisone, dexamethasone Use of Inhaled Steroids for Asthma ƒ Regular use decreases need for beta agonists & relapse rates ƒ Use during an acute attack may just increase cough ƒ Use of spacer and post-Rx mouth rinse decrease side effects (dysphonia, oral Candidiasis) Choices of Inhaled Steroids for Asthma (via MDI’s) ƒ Fluticasone (Flovent) 250 to 500 mcg bid ƒ Budesonide (Pulmicort, Rhinocort) 200 to 800 mcg bid ƒ Triamcinolone (Azmacort) 2 to 4 puffs bid to qid ƒ Beclomethasone (Vanceril, Beclovent) 84 to 840 mcg per day ƒ Virtually all patients should be on one of these after discharge Use of Anticholinergics for Acute Asthma ƒ Inhaled (via MDI or nebulizer) these decrease bronchospasm by reducing vagal tone –Atropine (0.2 to 0.5 mg) –Glycopyrrolate (Robinul) 0.2 to 0.4 mg –Ipratropium (Atrovent) 250 to 500 mcg ƒ Several studies show mild added benefit when added to first three beta agonist nebulizations in E.D. (not helpful after this) ƒ Ipratropium has low rate of side effects ƒ May help undefined subsets of patients Use of Magnesium for Acute Asthma ƒ Acts as smooth muscle relaxer & suppresses neutrophil burst response ƒ Conflicting results of efficacy in different studies ( ? inadequate dosing in some) ƒ Clearly safe & few side effects ƒ 2.0 to 5.0 gm IV dose reasonable to try for : –Severe symptoms –Respiratory failure –Non-response to standard Rx Use of Methylxanthines for Asthma ƒ Problems with aminophylline : –weak bronchodilator –high rate adverse side effects –narrow toxic / therapeutic window –requires monitoring of serum levels (goal 5 to 15 mcg/ml) –many medication interactions ƒ Clearly shown to add no benefit to acute Rx with beta agonists & steroids –However, slow release forms (Slo-Bid, Theo-Dur, Uniphyl) may be useful in some patients for chronic maintenance –5 to 8 mg/kg/day Use of Ketamine for Acute Asthma ƒ Dissociative anesthetic ƒ Relaxes bronchial smooth muscle ƒ Excellent agent for RSI for critically ill asthmatic –2 mg / kg IV or 4 mg / kg IM –Continued infusion 1 to 2.5 mg / kg / hr ƒ May cause : –Laryngospasm –Hypertension –Hallucinations Use of Heliox for Acute Asthma ƒ Is premixed air 20 % and helium 80 % ƒ Gas density is lower than air so flow resistance is less ƒ Somewhat limited usefulness for asthma because as more O2 is blended in, the gas density re-increases (max. O2 is 40 %) ƒ Expensive if used for extended period ƒ No major extended benefits in controlled studies Use of Leukotriene Receptor Antagonists (LTRA’s) for Asthma ƒ Leukotrienes are released from mast cells, eosinophils, and basophils and mediate : –bronchoconstriction –mucus secretion –airway mucosal edema ƒ The LTRA’s are useful for : –Treatment of stable, mild, persistent asthma, and prophylaxis of exercise induced asthma –decrease airway response to cold & allergens –Role in acute asthma not yet clear (IV montelukast is in phase 3 research trials) Choices of LTRA’s for Asthma ƒ Montelukast (Singulair) ƒ 10 mg PO hs or two hours before exercise ƒ Systemic eosinophilia and vasculitis consistent with Churg-Strauss Syndrome rarely reported ƒ Zafirlukast (Accolate) ƒ 20 mg PO bid ƒ Rarely has caused liver failure Another Category of Meds : 5Lipoxygenase Inhibitors ƒ Zileuton (Zyflo, Zyflo CR) ƒ Inhibits leukotriene formation ƒ Dose 600 mg pc and hs for Zyflo ƒ Dose 1200 mg bid for Zyflo CR ƒ Can cause liver failure ƒ Not studied for acute use Still Another Category of Meds : Mast Cell Degranulation Inhibitor • Cromolyn (Intal) – Inhibits degranulation of sensitized mast cells – Attenuates bronchospasm caused by exercise, cold air, aspirin, and environmental pollutants – MDI dose 2 puffs qid or two puffs 15 to 60 minutes prior to exercise – Rarely has caused liver impairment And the Final Category of Asthma Medication : Omalizumab (Xolair) ƒ ƒ ƒ ƒ Recombinant DNA-derived immunoglobulin G monoclonal antibody which binds selectively to human immunoglobulin E on the surface of mast cells and basophils and then reduces mediator release Used when Sx are not controlled by inhaled steroids Dose 150 to 375 mg SQ q 2 to 4 weeks Annual cost $12,000 to $15,000 Can cause anaphylaxis Combination Medications Available for Asthma ƒ Ipratropium and albuterol (Combivent) ƒ Nebulizer 3 ml q 20 min X 3 doses ƒ MDI 4 to 8 puffs q 20 min X 3 ƒ Salmeterol and Fluticasone (Advair Diskus) ƒ 3 dosage forms ; ƒ 100, 250, or 500 mcg fluticasone with 50 mcg salmeterol ƒ One inhalation bid Expert Panel 3 (2007) List of Ineffective Treatments for Asthma ƒ ƒ ƒ ƒ ƒ ƒ ƒ ƒ Methotrexate Cyclosporin Colchicine Acupuncture Chiropractic Homeopathy Breathing techniques Yoga Airway Management in Asthma ƒ Endotracheal intubation should be required in < 5% of admitted pts. ƒ Indications for ETT : –Altered mental status due to hypercarbia or hypoxia –Progressive resp. failure or resp. acidosis despite maximal Rx –Base decision on clinical situation (not a particular value of pCO2 or pO2 or pH) ƒ Always preoxygenate & ETT attempt should be made by most experienced operator Considerations About Nasotracheal Intubation of the Asthmatic Patient ƒ Advantages : –Can leave pt. sitting up ( resp. distress may worsen if forced supine) –Pt.'s resp. effort often makes the procedure easy –Tube may be more comfortable for pt. –Tube less likely to be dislodged ƒ Disadvantages : –May cause epistaxis –Requires smaller tube diameter than oral (so more airflow resistance) –May predispose pt. to sinusitis later Considerations About Orotracheal Intubation of the Asthmatic Patient ƒ Advantages : –Method of choice if pt. apneic or markedly bradypneic –No predisposition to epistaxis or sinusitis –Larger diameter tube can be used (may permit later bronchoscopy) ƒ Disadvantages : –Generally requires "full" Rapid Sequence Intubation (RSI) technique & supine position –May be less comfortable for pt. & more likely to dislodge Options for RSI Meds for the Asthmatic Patient ƒ For nasal ETT may only need etomidate or benzodiazepine IV (after topical anesthesia in nose) ƒ Usual oral ETT sequence : –Preoxygenate –Lidocaine 1.0 to 1.5 mg/kg IV –Ketamine 1.0 to 2.0 mg/kg IV –+/- benzodiazepine 1 to 5 mg IV –Succinylcholine 1.0 to 1.5 mg/kg IV –Perform intubation General Considerations for Mechanical Ventilation of the Asthmatic Patient ƒ Mortality of ventilated pts. prior to 1984 reported as 20 to 40 % ƒ Current mortality < 10 % using "permissive hypercapnia" –uses smaller tidal volumes –goal is to limit barotrauma –does not require normalization of pCO2 or pH Specific Guidelines for Mechanical Ventilation of the Asthmatic Patient ƒ 1. Volume control (A/C or SIMV) preferred over pressure control to avoid overventilation ƒ 2. Tidal volume set at 5 to 8 ml/kg ƒ 3. Initial rate set at 6 to 10 breaths per min. –allows increased time for exhalation & avoids dynamic hyperinflation ("breath stacking") Specific Guidelines for Mechanical Ventilation of the Asthmatic Patient (cont.) ƒ 4. Set FIO2 to keep arterial pO2 > 60 mm Hg –Should be < 50% to avoid O2 toxicity if ventilation prolonged ƒ 5. Set PEEP adjusted to 75 to 80 % of measured auto-PEEP level –Make sure endogenous (auto) PEEP does not exceed the amount dialed on the ventilator ƒ 6. Set Peak Insp. Flow Rate 70 to 90 L/min –Produces rapid inspiration allowing time for exhalation –End-inspiratory plateau pressures should be < 35 mm Hg Specific Guidelines for Mechanical Ventilation of the Asthmatic Patient (cont.) ƒ 7. Sedation to prevent tachypnea & allow pt. to rest ƒ 8. Aerosolized beta agonists should be given via ventilation circuit (continuous Rx can be done) ƒ 9. As wheezing improves, may increase TV & rate ƒ 10. Monitor for barotrauma (risk greater if endinsp. plateau pressure > 35 mm Hg) ƒ 11. Monitor for clinical improvement allowing extubation Complications of Mechanical Ventilation of the Asthmatic Patient ƒ Barotrauma due to alveolar rupture –Pneumomediastinum, pneumothorax, or SQ emphysema –Should usually treat with chest tube –May need to reset ventilation parameters to decrease end-inspiratory plateau pressure ƒ Prolonged muscle weakness –Can be due to prolonged effect of paralytic agent used for intubation (esp. if renal insufficiency) –May be partly due to steroid Rx –Can be a myopathic syndrome with increased muscle enzymes & require ventilation for several weeks Education of the Asthmatic Patient to be Discharged from the E.D. ƒ Consider pt. education regarding the following items prior to D/C : –MDI / spacer use training –Review of medications –Self use of short course oral steroids –Home use of PEFR ƒ Identify PEFR #'s for which pt. should come to E.D. –Arrange F/U with primary care doctor –Asthma diary –Identify avoidable triggers (shoot any cats in the house) Other Considerations for Education of the Asthmatic Patient ƒ Make sure family members are also educated re meds & severity assessment ƒ Emphasize planning & early response to minimize time lost from school or work ƒ Remember it is a chronic recurrent disease, so limit diagnostic tests unless there are atypical features or severity of an attack Asthma Lecture Summary ƒ ƒ ƒ ƒ ƒ Assess severity at presentation Start multiple simultaneous Rx if severe Decide if diagnostic studies needed Monitor for response to Rx Consider second line Rx's & intubation & ventilation for refractory cases ƒ Provide careful education & post - E.D. planning for discharged pts. Chronic Obstructive Pulmonary Disease (COPD) ƒ Refers to triad of disease processes : –Asthma (airway reactivity) –Bronchitis (airway inflammation) –Emphysema (airway collapse) –All 3 coexist to some degree in same pt. ƒ Definitions : –Chronic bronchitis = chronic cough with sputum production for at least 3 months / yr. for at least 2 yrs. –Emphysema = enlargement of distal air passages due to alveolar septal destruction (& obliteration of pulm. capillary bed) COPD Epidemiology ƒ 4th leading cause of death in U.S. ƒ Leading cause of death in smokers > age 55 ƒ 12.5 million in U.S. have chronic bronchitis ƒ 14 million in U.S. have emphysema ƒ 2nd most common cause of permanent disability ƒ Huge economic impact Risk Factors to Develop COPD ƒ Major factor is cigarette smoking ƒ Less common factors : –Inhalation of "second hand" smoke –Occupational exposure –Cystic fibrosis –Alpha 1 antitrypsin deficiency –Intravenous drug abuse Pathophysiologic Features of COPD ƒ airflow ƒ lung volumes, hyperinflation ƒ V/Q mismatch ƒ Arterial hypoxemia & hypercarbia ƒ Often intrinsic airway inflammation ƒ Note typical inflammatory cells in COPD are usually neutrophils, whereas they are usually eosinophils in asthma Sequence of Pathophysiologic Events with COPD ƒ Parenchymal destruction continues ƒ Distal air spaces enlarge ƒ Loss of elastic recoil –Increases lung volumes when resp. rate –Expiratory time then –Hyperinflation results Pathophysiologic Results of Dynamic Hyperinflation in COPD ƒ Inspiratory muscle dysfunction –Acts at stiffer portion of its volume pressure relationship –Muscle fibers forced from vertical to horizontal position –Increased reliance on accessory muscle fibers ƒ Causes increased work of breathing & increased dyspnea Goals of the E.D. Evaluation of the COPD Patient ƒ ƒ ƒ ƒ Rapidly stabilize the pt. in resp. failure Identify precipitating causes Treat complications Rule out or treat concurrent conditions Clinical Presentation of Patients with Exacerbations of COPD ƒ Dyspnea ; most common ; may be severe ƒ Other Sx may or may not be present –Chest pain ; may be : ƒ Diffuse or vague ƒ Pleuritic ƒ Chest wall (from cough injury) –Cough –Fever –Altered mental status –Apprehension Signs Associated with COPD Exacerbations ƒ ƒ ƒ ƒ ƒ ƒ ƒ ƒ ƒ Dyspnea Tachypnea Tachycardia Ashen skin color or cyanosis Diaphoresis Accessory muscle use Intercostal retractions Rales / rhonchi / wheezes / decreased BS Apprehension Signs of Severe or Critical Airflow Obstruction in a COPD Exacerbation ƒ Altered mental status ƒ Inability to speak ƒ "Silent chest" (no or limited audible BS) ƒ Combativeness / seizures Differential Dx of COPD Exacerbation ƒ ƒ ƒ ƒ ƒ ƒ ƒ ƒ ƒ CHF Acute myocardial ischemia Airway obstruction Pneumonia Pneumothorax Pulmonary embolus Pleural effusion Acute aortic dissection Allergic reaction Caveats About Differential Dx of COPD Exacerbation ƒ COPD exacerbation may coexist or be concurrent with any of Dx's on previous slide ƒ Particularly CHF may cause COPD exacerbation & vice versa –PEFR > 150 L/min suggestive of Dx of CHF ƒ Pulm. embolus particularly difficult to Dx in COPD pt. Spirometry Use for COPD Exacerbation ƒ Should be performed on all pts. –Determine initial severity –Determine response to Rx ƒ Clinical eval. alone is unreliable at estimating airflow obstruction ƒ Many pts. with post-Rx FEV1 > 40% can be safely discharged ƒ Another discharge criterion is PEFR > 250 (assuming pt.'s baseline PEFR is > 300 ; need to know pt.'s prior PFT's to determine this) Use of ABG's in COPD Exacerbation ƒ Some recommend on all pts. ƒ I favor using only in pts. who : –Appear critical at presentation –Do not respond well to Rx –Have altered mental status ƒ ALL pts. should have continuous pulse oximetry ƒ Pt. can have hypoxemia even when pulm. function approaches 50% of normal Use of CXR in COPD Exacerbation ƒ CXR should be obtained on all pts. ƒ At least 15 % of CXR's show a directly treatable finding : –Pneumonia –Pleural effusion –Pneumothorax –Atelectasis –Aortic dissection ƒ Also allows R/O CHF E.D. Management of COPD Exacerbations ƒ For ALL Pts. : –Oxygen –Beta agonist aerosol ƒ Consider SQ terbutaline if unable to take aerosol –Anticholinergic aerosols ƒ For some pts. : –Corticosteroids –Antibiotics –Diuretics –CPAP / BiPAP / Intubation / Ventilation Considerations for O2 Therapy for COPD Exacerbations ƒ Risk of eliminating hypoxic drive (& causing further resp. acidosis / failure) is overstated –Only applies to < 5% of COPD population ƒ Venturi mask can be used to give precise regulated O2 concentrations ƒ Pts. that develop resp. acidosis with O2 Rx usually need to be intubated & ventilated anyway Anticholinergic Med Choices & Doses for COPD Exacerbations Medication Dose Ipratropium 0.5 mg Atropine 1 to 2 mg (0.025 mg/kg) Glycopyrrolate 0.2 to 1.0 mg Ipratropium preferred because of less side effects such as tachycardia Considerations in Use of Corticosteroids for Rx of COPD Exacerbation ƒ Not of benefit to all pts. with COPD ƒ Should be considered if : –Pt. on chronic steroid Rx –Wheezing component is prominent –Allergic trigger –Prior response to steroids –IV versus PO is equivalent Considerations in Use of Antibiotics for COPD Exacerbation ƒ Not indicated for all pts. ƒ Usually indicated for COPD exacerbation with : –Fever / chills –Increased sputum production –Change in color of sputum –Persistent increased cough –Atelectasis or infiltrate on CXR ƒ Most common pathogens : –Strep pneumoniae (with increasing rates of PCN resistance) –Hemophilus influenzae –Moraxella (Branhamella) catarrhalis Antibiotic Choices for COPD Exacerbation ƒ Best first line agents : –Azithromycin –Cefuroxime –Trimethoprim - sulfa –? levofloxacin ƒ Problems with other choices : –Doxycycline, amoxicillin : resistance –Erythromycin : no H. flu coverage –Amoxil / clavulanate : cost, side effects –Clarithromycin : cost, drug interactions, taste Ventilatory Assistance Considerations for COPD Exacerbation ƒ 3% of COPD pts. require ETT & ventilation for resp. failure ƒ Indications & complications same as for asthma ƒ Need to be careful to avoid barotrauma ƒ Intubated COPD pts. have higher mortality & longer time on ventilator than asthma pts. ƒ CPAP or BiPAP can be tried prior to ETT Disposition Considerations for COPD Exacerbation ƒ Indications for hospital admission : –Persistent hypoxemia (O2 sat. < 90%) –Persistent hypercarbia / resp. acidosis –Persistent dyspnea –Overt resp. failure –Altered mental status –Usually if associated pneumonia –Pneumothorax ƒ "Borderline " admission candidate may be considered for observation unit first Suggested E.D. Management of COPD Exacerbation ƒ ƒ ƒ ƒ ƒ ƒ Immediate O2 & beta 2 aerosol Rapid CXR to R/O CHF or pneumothorax Evaluate for cardiac ischemia (EKG) Consider other Dx tests Early PEFR & repeat after each Rx Continued Rx (aerosols, +/- steroids, +/antibiotics, etc.) ƒ Monitor for response : –ETT / ventilation if worsening –Admission if not improving satisfactorily Adjunctive Treatments to Consider for COPD Exacerbations ƒ Phosphodiesterase-4 Inhibitors ƒ Reduce inflammation via macrophages and lymphocytes ƒ Cilomilast 15 mg PO bid ƒ Mucolytic agents ƒ N-acetycysteine ƒ Efficacy debatable ƒ Referral for surgical bullectomy, lung volume reduction surgery, or lung transplantation Web Sites with Useful Clinical Guidelines for Asthma and COPD ƒ Expert Panel Report 3 Summary Report 2007 ƒ 440 pages ; summary is 74 pages ƒ http://www.nhlbi.nih.gov/guidelines/asthma/asthgdl n.htm ƒ http://www.medscape.com/viewarticle/564670 , and 564654 ƒ emedicine.com has 4 nice articles under both “emergency medicine” and “pulmonology” : ƒ http://www.emedicine.com/med/topic177.htm , & 373 ƒ http://www.emedicine.com/emerg/topic43.htm , & 99