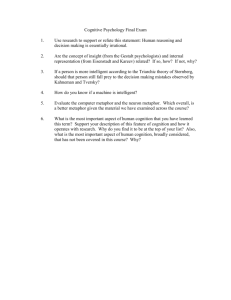
The Mental Status Exam
advertisement

The Mental Status Exam John Wurzel MD Outline and Objectives 1. To review the major points of the mental status examination and learn a little vocabulary. 2. To understand the role of the mental status exam in in diagnostic, prognostic, and therapeutic thinking. 3. To understand how to use mental status exam findings in context to assess a patient. 4. To practice performing various elements of the mental status exam. What is the Mental Status Exam? • Let’s start with a caveat: I’m teaching you my (and most of my colleagues’) interpretation of what a mental status exam is and what purpose it serves. However, other interpretations exist, and are also valid. • That said…what is a mental status exam? – It is a medical examination; an extension of the physical exam. – Like a physical exam it includes both objective and subjective evidence gathered about the patient. • And, what purpose does a medical examination serve? – To aid in diagnostic, prognostic, and therapeutic thinking. • Therefore, the elements of the mental status exam should all provide pertinent positive or negative information. What are the elements of the MSE? • Well? – – – – – – – – – Appearance Behavior Speech Mood Affect Thought process Thought content Cognition Insight/Judgment Appearance • What sorts of things should you note when describing appearance that help us determine diagnosis or choose treatment? – Clothing (casual, work-appropriate, formal, dirty or clean, torn, stained, etc.) • A well dressed psychotic person likely has a strong social network; this is useful information for treatment planning. • A professional in grossly inappropriate dress might make you concerned for psychosis or mania. – Grooming (cleanliness, pertinent comments on make-up or hair, dentition) • Depression often produces poor grooming, mania or psychosis bizarre grooming, and these also speak to level of social support. More Appearance – Body habitus • Very thin patients should raise diagnostic concern for anorexia, end stage dementia, severe decompensations in psychosis, etc. • Obese patients are often obese because of medications that we are prescribing for them. • Our medications can cause gynecomastia – Scars • Raise possibility of previous self harm (suicidal or nonsuicidal) More Appearance – Acute or chronic injuries • Perhaps due to recent self-harm attempt, but also useful in terms of psychosocial thinking and treatment planning • May be complications of mediations that we are prescribing (i.e. amputation from diabetes secondary to an antipsychotic). – Patient’s posture and or location in the hospital room • More relevant in consult work, this again speaks to functionality – Odors (alcohol, feces, urine, etc.) – Track marks Appearance continued…It’s all about context • What about tattoos or piercings? Well, what does a tattoo tell you diagnostically? – I usually don’t mention them unless they are truly remarkable. – But…If I worked with Jehovah's Witnesses, or the president of the anti-tattoo league, I certainly would. • Religious symbols or attire? – If your patient comes in wearing a Habib or a yarmulke, or a cross, what does it really tell you about them? – However, if my conservative Islamic patient in a Hijab tells me that she’s taken up drinking and has slept with eight different men in as many days, I’m going to comment on the Hijab (and the rest of it, obviously). • Anything that seems out of place, or anything that represents a change deserves comment. – I’m usually not very excited if my patient, who is a successful lawyer, comes in in a pant suit. But after six weeks of seeing her in sweat pants, the change makes the pant suit pertinent. Appearance Continued Here’s a couple examples: 1. Dress casual clothing, fair and appropriate grooming, well-healing scar on right forearm and multiple healed and faded similar scars over both forearms. 2. Obese man in a wheelchair missing left leg below the knee as well as right foot, in clean sweat pants and sweat shirt. 3. Lying in hospital bed in hospital gown, in five point restraints, poor but appropriate grooming. Bandages over left side of skull, intubated. Examples: Let’s practice describing appearance… Behavior • Again, what sorts of things should you note when describing behavior that help us determine diagnosis or choose treatment? – What is their level of agitation? • Are they calm and cooperative, irritable, impatient, angry, falling asleep? – This may help inform me of how to structure my interview, how to suggest interventions, whether to believe their answers to questions, and may speak to various diagnoses. For example, pseudodementia is classically characterized by poor effort and cooperation, while true dementia is not. – Psychomotor agitation or retardation; what might it tell you? • ADHD, manic or anxious patients (or those high on stimulants) are classically activated, depressed patients are classically retarded. Behavior – Motor tics; why would your patient have motor tics? • Perhaps Tourette’s syndrome, perhaps a medication side effect from an antipsychotic (tardive dyskinesia). – Tremor; what is the psychiatric differential? • Parkinson’s disease, antipsychotic-induced parkinsonism, lithium tremor (possibly lithium toxicity), alcohol or benzodiazepine withdrawal, stimulant intoxication, etc. Behavior – Eye contact; what kinds of patients have what kinds of eye contact? • • • Depressed patients typically have poor eye contact Anxious patients also have poor eye contact, though for different reasons Psychotic patients often have unusually intense eye contact because they don’t pick up on social cues (and an increased blink rate). – What might gait findings tell you? • Acute intoxication can cause ataxia, Parkinson’s or parkinsonism cause shuffling gait, etc. So how would you describe the following behaviors? This is tardive dyskinesia, in a case of antipsychotic withdrawal dyskinesia. This, however, is psychomotor agitation during (probably) methamphetamine intoxication… Speech What are the four descriptors for speech? • Rate; purely a comment on speed. Who speaks fast? – Anxious, manic, stimulant intoxicated, etc. Who speaks slow? – Depressed, patients with parkinsonism, etc. • Rhythm; the articulation, prosody, any slurring, latency, and I consider pressured speech to be a rhythm. – Pressured speech refers not to the rate, but to whether the speech is interruptible. • Classically, pressured speech is also rapid and is coming from a manic patient or someone on stimulants • However, you will rarely meet someone with slow, pressured speech. If you’re anything like me, it will be intensely frustrating. Speech • Volume; self-explanatory. • Content; this refers mostly to neurologic findings like aphasias, perseveration, etc. However, it can also refer to findings like monosyllabic responses, very poor vocabulary, etc. Let’s try describing this woman’s speech… I would describe this woman’s speech as rapid and bordering on pressured. Mood • The prevalent emotional state the patient tells you they feel. • Often placed in quotes since it is what the patient tells you. • Examples “Fantastic, elated, depressed, anxious, sad, angry, irritable, good.” Affect: The radio dials… • I think of affect like a radio; it has a dial for volume, and one for station. – The station dial: what emotional state are you observing? It can pretty much be anything… • Dysphoric (sad), euthymic (neutral), euphoric (happy), anxious, irritable, excited, annoyed, frustrated, plethoric...don’t be limited by “psychiatric terms”, just describe it accurately. Affect – The volume dial: how much range does the patient’s affect display? Or, how much does their affect vary from the state you described? • Patients whose affect varies little might be called blunted, restricted, constricted. • Patients with normal variation (i.e. they can smile at jokes or at happy thoughts, but they can look sad or cry at sad thoughts) I typically describe as having “normal range.” • Patient’s whose affect seems to vary out of proportion to the conversation have “labile” affect. Sometimes a labile affect is so labile that you can’t identify a core mood state. • Flat affect is the physical inability to convey emotion. You might see it in severe parkinsonism, supranuclear palsy, amyotrophic lateral sclerosis, comatose patients, etc. It is essentially a neurological condition. A patient cannot have “dysphoric, flat” affect. It can only be “flat” if it is truly flat. Affect: Other Considerations • Congruity: Does the observed affect match the mood that the patient describes? • Appropriateness: Is the affect appropriate to the subject of conversation? Every time I describe affect, I use at least two words: the “station” or emotional state, and the “volume” or the emotional range. If congruity or appropriateness seem important, then I comment on them, too. If a picture is worth a thousand words, how many is a video worth? And what affect do you see here? I would describe Data as having a highly restricted, euthymic affect. It is also incongruous relative to his stated mood and somewhat inappropriate to the subject matter (a joke). You might call it flat if you ignore the fake laughing. And what about in this video? This woman has a labile affect. It’s actually so labile that I can’t tell if she is fundamentally happy or sad. To really stretch my analogy, you might say that the radio volume is turned up so high that you can’t make out the words anymore. Thought Process: How organized are their thoughts? First, I’ll need a volunteer… How does one describe a normal thought process? • Linear, logical, goal oriented. Tangential: Li/Lo Circumstantial: Li/Lo/~GO Q Normal Thought Process: Li/Lo/GO A Word salad Loosening of associations (a string of loosely related tangents): ~Li/~Lo Flight of Ideas (a string of unconnected tangents): ~Li (Clanging) Video! What is this man’s thought process like? I would say his thought process is characterized by loose associations, frequent flights of ideas, and even occasional clanging. • For bonus credit, what about his speech? • Rapid and truly pressured Thought Content • What thought content abnormalities do we ask about? – Hallucinations: seeing or hearing things that aren’t really there (typically auditory of visual) – Illusions: misinterpreting sights or sounds that actually are there (for example, seeing a coat rack as a person, or hearing radio static as a voice) Thought Content – Delusions: fixed, false beliefs firmly held in spite of contradictory evidence • Control: outside forces are controlling actions • Erotomanic: a person, usually of higher status, is in love with the patient • Grandiose: inflated sense of self-worth, power or wealth • Somatic: patient has a physical defect • Reference: unrelated events apply to them • Persecutory: others are trying to cause harm More Thought Content Abnormalities – Ideas of reference: the idea that something refers to you when it does not (for example, the idea that a TV show or radio program has special messages just for you, or that two strangers across the street are having a conversation about you when they have no reason to) – Thought insertion (mind reading) or thought broadcasting (other people reading your mind) Even More Thought Content Abnormalities – Paranoia: believing that people or organizations are out to get you – Thought blocking: the sense that you can’t finish your thoughts – Suicidal or homicidal ideation, intent, and plan are usually mentioned here. Let’s discuss this man’s thought process and content… He is displaying loose associations, with paranoid delusions and possible ideas of reference. And this woman’s thought content… She is describing tactile hallucinations, has clear ideas of reference, and also displays paranoia. She may have thought broadcasting as well. Cognition • Think about cognition diagnostically: – What are core cognitive domains that fail in dementia? • Executive function – Includes planning, visuospatial, etc. • Language (covered in speech) • Memory • Recognition (or naming) • Coordination – And what are the primary diagnostic clues for delirium? • Level of attention (alert, appropriate vs. waxing, inconsistent, drowsing off) • Disorientation Cognition Continued • If you tested these domains, then provide the test and the results (i.e. “Short term recall 3/3”, or “Able to perform serial 7’s”, “MOCA 28/30” etc.) • Don’t say that you assessed cognitive domains unless you actually did. • Every MSE should include some comment on memory, orientation, and level of attention. Other domains should be discussed if pertinent. The Mini-Cog: A Useful Screening Tool • Clock draw: – Shape of contour must be correct – Numbers must be in the correct places – Hands must be accurate (you should always ask for a time that places the hands in two different quadrants) • Three item recall after five minutes. • Scoring: – If they pass the three item recall, they pass – If they get 0/3, they fail – If they get 1-2/3, they pass if the clock is right and fail if the clock is wrong. – If they pass, the patient is quite unlikely to have dementia (up to 99% sensitivity in some studies). – If they fail, they merit further evaluation (MOCA, Mini-Mental, SLUMS, etc.) Insight and Judgment • Insight and judgment are not the same things. • What is insight? – An awareness of one’s own situation or condition. • On a superficial level, it refers to a patient understanding the medical elements of their condition • On a deeper level, it refers to a patient understanding the social and even psychological contributions to their situation. Insight and Judgment • What is judgment? – The ability to anticipate the consequences of one’s behavior and make decisions that protect oneself and others in the context of one’s own moral compass • Functionally, it usually boils down to whether the patient is doing what their providers are recommending, regardless of why they are doing it. • Who can give me some examples of insight and judgment? Now a couple full practice assessments… Write your own MSE for a couple minutes, then we’ll all compare notes. Practice #1 • Appearance: Appropriately though casually dressed, fair grooming. Appears to be bleeding at the mouth. • Behavior: Calm, though confused. Repeatedly tries to put hands in mouth. No gross psychomotor agitation or retardation. • Speech: Somewhat slurred, with labile volume. • Mood: “I feel funny” Practice 1 Continued • Affect: Mildly dysphoric and clearly confused. Somewhat labile. • Thought process: Linear and logical in general but at times displays disorganization in that he loses the thread of conversation. • Thought content: Some evidence of responding to internal stimuli. SI, HI not assessed. • Cognition: Not formally assessed, but cognition appears impaired. Memory grossly impaired to recent events. Attention waxing and waning during interview. • Insight/Judgment: Poor/Poor. More practice.. Write your own MSE for a couple minutes, then we’ll all compare notes. Practice #2 • Appearance: Dressed and groomed casually but appropriately. Notable bilateral facial scars. • Behavior: Generally calm, though with a violent outburst toward the end. Tearful throughout. No psychomotor agitation or retardation noted. • Speech: Limited by tears, but characterized by stutter, brief statements, and quiet volume. • Mood: “I always thought I was funshine bear…” Practice #2 Continued • Affect: Restricted to dysphoria. Tearful. • Thought process: Linear and logical on a superficial level. • Thought content: No evidence of responding to internal stimuli. Clear HI, with intent, plan, and access to means. • Cognition: Not formally assessed, but cognition appears superficially intact. Memory grossly intact. Attention appropriate throughout. Orientation not formally assessed. • Insight/Judgment: Fair/Fair?