Dermis - FTHS Wiki
advertisement

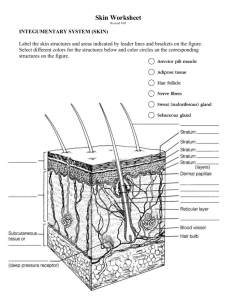
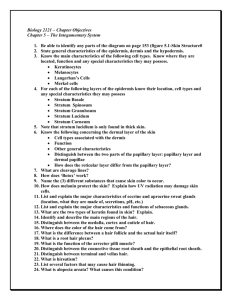
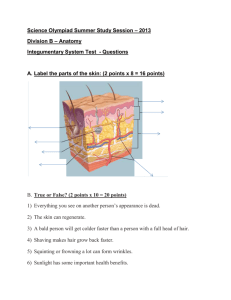
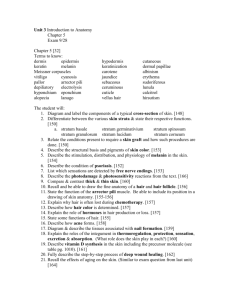
Unit 4: Structure of Integument and its Appendages Regions of Integument (skin) Epidermis – outermost region •Keratinized stratified squamous epithelium •Non-vascular •4 cell types •4 - 5 layers 4 Epidermal Cell Types Keratinocytes – make keratin fibrous protein •Protective •Hardens and waterproofs skin. •Cells connected by desmosomes: •prevent tearing and cell separation from mechanical stress •Arise from hightly mitotic stratum basale •Cells dead at free surface 4 Epidermal Cell Types Keratinocytes – make keratin fibrous protein Langerhans’ Cells – star shaped, epidermal dendritic phagocytic cells •activate the immune system •ingest foreign material 4 Epidermal Cell Types Keratinocytes – make keratin fibrous protein Langerhans’ Cells – star shaped, epidermal dendritic phagocytic cells Merkel Cells – half-sun touch receptors •associated w/ sensory nerve endings 4 Epidermal Cell Types Keratinocytes – make keratin fibrous protein Langerhans’ Cells – star shaped, epidermal dendritic phagocytic cells Merkel Cells – half-sun touch receptors •associated w/ sensory nerve endings melanin Melanocytes – makes brown pigment melanin •shields keratinocyte DNA from UV damage Layers of the Epidermis Stratum corneum Stratum lucidum (absent in thin skin) Stratum granulosum Stratum Spinosum Stratum basale Stratum Basale (Basal Layer) • • • • • AKA stratum germinativum Deepest epidermal layer, attached to the dermis Single row of the youngest keratinocytes Rapidly mitotic, making new cells daily Melanocytes and Merkel cells found here Stratum basale dermis Stratum Spinosum (Prickly Layer) Stratum Spinosum • Cells filled with filaments connected to desmosomes. (gives prickly look) • Melanin granules filling cells in response to UV or genetics • Langerhans’ cells found here Stratum basale dermis Stratum Granulosum (Granular) • • Stratum granulosum Stratum Spinosum • • Stratum basale• dermis 3-5 cell layers Keratinocytes change, flatten, lose nuclei Keratin granules accumulate in the cells of this layer Lamellated granules release extracellular glycolipids in intercellular space that waterproof skin Too far from nutrient rich dermal blood, cells begin to die Stratum Lucidum (Clear Layer) Stratum lucidum would be here, if present Stratum granulosum • Stratum Spinosum • – Sole of feet, palms, calluses • Stratum basale dermis Transparent band of flat, dead keratinocytes Only in thick skin Reduces friction between the granulosum (inferior) and the corneum (superior) Stratum Corneum (Horny Layer) Stratum corneum Stratum lucidum would be here, if present Stratum • 20-30 granulosum Stratum Spinosum • Stratum basale dermis layers of DEAD keratinized cells; ¾ of epidermal thickness Functions include: – Waterproofing (due to glycolipids) – Protection from: • Abrasion • Penetration • biological, chemical, and physical assaults Stratum Corneum (Horny Layer) Stratum Corneum Stratum Lucidum Can Little Stratum Granulosum Girls Stratum Spinosum Stratum Basale dermis Smell Bad? Let’s take a break from lecture to draw the difference between thick and thin skin. • Use appropriate drawing and coloring methods. • Horizontal labeling with leader lines http://www.lab.anhb.uwa.edu.au/mb140/corepages/integumentary/integum.htm #labepidermis Regions of Integument (skin) Epidermis – outermost region •Keratinized stratified squamous epithelium •Non-vascular •4 cell types •4 - 5 layers Dermis – middle region • Vascularized • 80% dense irregular connective tissue • 20% areolar connective tissue Overview of the Dermis • Cell types: fibroblasts, phagocytes, mast cells and white blood cells • 2 layers – papillary (upper) and – reticular (lower) • Rich with nerves, blood and lymph vessels • Most hair follicles, oil and sweat glands derived here Papillary Layer of Dermis •Dermal papillae •Areolar connective with: tissue with collagen •capillary loops and elastic fibers (thin blood •Superior surface vessels) with• Meissner’s dermal papillae: peg-like corpuscles (touch), (reason for projections fingerprints) •and free nerve endings (pain) Papillary Layer of Dermis •Krause’s end bulb: (cold) •Ruffini end organs: (heat and sustained pressure) In Reticular Layer: Pacinian corpuscle: (touch, deep vibrations, transient pressure) Reticular Layer of the Dermis • 80% of the thickness of the dermis (dense –irregular CT) • Collagen fibers: – add strength and resiliency – Binds water, keeping skin hydrated • Elastin fibers: – stretch-recoil properties • Rich in blood vessels: – dilate or constrict in response to emotions or temperature changes Name the epidermal and dermal layers (review) 5. Stratum Corneum (Epidermis) 4. Stratum Lucidum (Epidermis) 3. Stratum Granulosum (Epidermis) 2. Stratum Spinosum (Epidermis) 1. Stratum Basale (Epidermis) 6. Papillary Layer (Dermis) 7. Reticular Layer (Dermis) Regions of Integument (skin) Epidermis – outermost region •Keratinized stratified squamous epithelium •Non-vascular •4 cell types •4 - 5 layers Dermis – middle region • Vascularized • 80% dense irregular connective tissue • 20% areolar connective tissue Hypodermis (superficial fascia) •deepest region •Mostly adipose (fat storage), some areolar •Vascularized Hypodermis (superficial or subcutaneous fascia) • Composed mostly of adipose and some areolar connective tissue • Adipose cells swell and thicken with fatty droplets during weight gain • Connects skin to underlying muscle • Absorbs shock • Insulates Skin Color Three pigments contribute to skin color 1. Melanin: yellow to reddish-brown to black – only pigment made in skin by melanocytes and passed onto keratinocytes – Freckles and pigmented moles – result from local accumulations of melanin 2. Carotene: yellow to orange pigment – Pigment incorporated into skin due to diet – Accumulates in stratum corneum and in adipose 3. Hemoglobin: reddish pigment, gives pink hue to skin – Due to oxygenation of red blood cells Skin “Appendages” Epidermal Derivatives include: hair Sebaceous Oil Glands hair follicles 6 Sudoriferous Sweat Glands Sudoriferous Sweat Glands (2 types: Eccrine and Apocrine) Eccrine glands • • • • • Covers entire body (3 million p/person) – Most abundant on palms, soles of the feet, and forehead Coiled in dermis Duct opens on skin’s surface (pore) “sweat” = hypotonic blood filtrate released by exocytosis: – 99% water, salts, antibodies, anti-biotic proteins, and Nwastes, vitamin C Evaporation of sweat cools the body Sudoriferous Sweat Glands (2 types: Eccrine and Apocrine) Apocrine glands • Only 2000 p/person • Found in axillary and anogenital areas with pheromone secretions • Ducts empty into hair follicles • Odorless initially. – – Secretions contains lipids and protein that bacteria feed on. Decomposition of secretions by bacteria produce “body odor” Sweat glands modified Ceruminous glands – modified apocrine glands in external ear canal that secrete cerumen (ear wax) Mammary glands – specialized sweat glands that secrete milk Sebaceous “Oil” Glands • Simple branched alveolar glands • Holocrine: glandular cells rupture to release secretions • Sebum Secretions: – – – – Oils + ruptured cell fragments moisturize hair and skin Slows water-loss bactericidal • Released onto hair within follicle then flows onto skin surface. • Acne due to blockage of hair follicle w/ infected sebum Video Summary You tube: What is skin? The Layers of Human Skin Hair (Pili) • Strands of dead, hard-keratinized cells made by follicles – Softer keratin in epidermal cells • Shaft projects from skin; Root embeded within dermis and hypodermis •3 concentric layers: - Medulla: absent in fine hair - Cortex: gives hair color - Cuticle: overlapping keratin •Split ends: cuticle worn away, exposing cortex Structure of Hair Follicle Basement membrane medulla Follicle created by in-vagination of epidermal surface (epithelial root sheath) into dermis and hypodermis to create a “bag” or “sac” that builds hair Structure of Hair Follicle Deep end of follicle: expanded forming a hair bulb Hair papilla supplies nutrients to hair (via capillaries) and signals growth Melanocytes on superior surface of papilla pigments hair by creating melanin Hair papilla created from in-folding of dermal tissue into hair bulb Structure of Hair Follicle Arrector pili muscle – attached to hair follicle and skin. When contracted, holds hair erect •Root hair plexus wraps around each hair bulb •Bending hair stimulates these endings, hence our hairs act as sensitive touch receptors Hair Shape • Internal shape of shaft and follicle determines hair shape – Round shaft: straight hair – Oval shaft: wavy hair – Flat or ribbon like shaft: kinky, curly hair ** One head can have many shaft shapes resulting in interesting hair textures. Hair Types • Vellus – pale, fine body hair found in children and the adult female (immature) • Terminal – coarse, long hair of eyebrows, scalp, axillary, and pubic regions • Hair growth influenced by: – Nutrition – Blood flow: reduced blood flow hair loss Ex. Brick layer shoulders: increased blood flow to area because of carrying heavy objects results in hair growth Hair Growth Cycles • Hair has a life cycle: – Period of Active Growth (AG) – Regressive Phase: hair bulb shrivels and matrix dies – Resting Phase – Cycle repeats: Older hair falls out, replaced by new hair • Length of AG period determine length of hair Ex: Scalp: AG of 6-10 years Brows AG: of 3 – 4 months Balding or thinning hair: short AG Hair Thinning and Baldness • Alopecia – hair thinning in both sexes – Rate of hair shed > Rate of hair growth • Hirsutism: excessive hair growth in women. Caused by excessive sex hormones usually from an ovarian tumor. • True, or frank, baldness – Genetic – Sex-influenced condition • Male pattern baldness – caused by follicular response to DHT (Dihydrotestosterone) • Growth cycle is so short that hairs never emerge from follicles before shedding – Sex linked trait – carried on X chromosome, inherited from mother Hair Function Functions of hair include: – maintaining warmth – Alerting the body to insects on skin – Guarding the scalp against trauma, heat loss, and sunlight – Eyelashes and nose hairs act as barriers against foreign substances Hair Distribution • Hair is distributed over the entire skin surface except: – Palms, soles, and lips – Nipples and portions of external genitalia Structure of a Nail • Scale-like epidermal modification on the distal, dorsal surface of fingers and toes • w/ hard keratin Figure 5.6 Back to Regions of Skin 20% Areolar Connective Tissue Back to Regions of Skin 80% Dense Irregular Connective Tissue Collagen fibers organized in irregular patterns •Strong and flexible Back to Regions of Skin Adipose Tissue of Hypodermis Mostly fat droplets Dense irregular connective tissue of reticular layer of dermis Adipose tissue of hypodermis