Malabsorption-lecture
advertisement

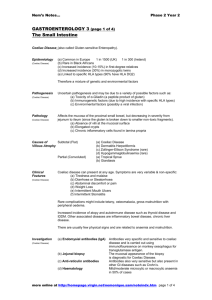
Non-neoplastic intestinal disease Malabsorption Paul L. Crotty Department of Pathology Tallaght Hospital October 2007 Outline of lecture Review normal digestion/absorption How diseases interfere with the process Tests for malabsorption Coeliac disease Chronic pancreatitis Bacterial overgrowth Malabsorption/Maldigestion diverse disease processes final common pathway of interference with normal digestion and absorption of nutrients similar/overlapping clinical presentations understanding normal digestion and absorption is central to understanding diseases that interfere with same Normal digestion and absorption (1) Luminal phase (2) Mucosal phase (3) Removal phase As example: Triglycerides Luminal phase: in small intestine Pancreatic lipase: enzymatic hydrolysis into mono-acyl glycerol and free fatty acids Solubilisation: incorporation into micelles with bile salts Mucosal phase: in enterocyte cytoplasm assembly into chylomicra with apoproteins Removal phase: in lymphatics Normal process of fat digestion and absorption Diseases interfering with luminal phase Pancreatic exocrine insufficiency chronic pancreatitis Bile salt deficiency liver disease, especially cholestatic bacterial overgrowth terminal ileal disease Other: post-gastrectomy, Zollinger-Ellison Diseases interfering with mucosal phase Small bowel disease Coeliac disease Tropical sprue Whipple’s disease Crohn’s disease Post-small bowel resection Specific enzyme deficiency,transport protein defects, abetalipoproteinaemia Diseases interfering with removal phase Lymphatic blockage Primary lymphangiectasia Obstruction Major disease entities Coeliac disease Chronic pancreatitis Bacterial overgrowth Consequences of malabsorption Effects of excess fat in stool Steatorrhoea: bulky, pale, foul-smelling Nutrient deficiencies: global/specific Energy, Protein (failure to thrive, short stature, weight loss) Specific deficiencies esp. fat soluble vitamins A, D, E and K, also iron Quantitation of fat in stool Normal stool fat <6g/day (over range of dietary fat from 60 to 200g) With diarrhoea of any cause: stool fat can rise up to 14g/day With fat malabsorption: stool fat much higher: 50-100g/day range Standard: 3-5 day collection D-xylose test 5 carbon sugar: absorbed by passive diffusion D-xylose test is a measure of functional surface area of small bowel After overnight fast: 25g D-xylose given p.o Measure serum level at 1h (normal >20mg/dl) 5h urine collection (normal >4g) FP: incomplete collection/dehydration/renal disease What do you expect the result of a D-xylose test will be in… Chronic pancreatitis? Coeliac disease? Cholestatic liver disease? Bacterial overgrowth? Key role of duodenal biopsy Biopsy diagnosis of specific diseases Giardia infestation, Whipple’s disease abetalipoproteinaemia, lymphangiectasia Significantly blunted villi or flat mucosa (partial or complete villous atrophy) classically seen in untreated coeliac disease but can also be seen in other food allergies, rarely in viral infection, Crohn’s disease, tropical sprue Normal mucosa Patient with malabsorption with a normal duodenal biopsy Any disease interfering with luminal phase of absorption chronic pancreatitis bile salt deficiency ...but also in any primary small bowel disease with focal involvement Aretaeus: The Greek work "koiliakos" used by Aretaeus had originally meant "suffering in the bowels" when used to describe people. Passing through Latin, 'k' became 'c' and 'oi' became 'oe'. Dropping the Greek adjectival ending 'os' gave us the word coeliac. "The Coeliac Diathesis" [by Aretaeus] describes fatty diarrhoea (steatorrhoea) for the first time and then proceeds to give an account of several other features of the condition including loss of weight, pallor, chronic relapsing and the way in which it affects children as well as adults. "If the stomach be irretentive of the food and if it pass through undigested and crude, and nothing ascends into the body, we call such persons coeliacs". 17 centuries later... 1888: Samuel Gee, using an identical title to Francis Adams' translation of Aretaeus’ writings , "The Coeliac Affection", gave the classic description of the condition. "to regulate the food is the main part of treatment ... The allowance of farinaceous foods must be small ... but if the patient can be cured at all, it must be by means of diet." “a child…was fed upon a quart of Dutch mussels daily, throve wonderfully but relapsed when the season for mussels was over. Next season, he could not be prevailed upon to take them.” 1924: Haas: Popularised the banana diet: Essentially a diet low in carbohydrate except for ripe bananas. 1950: Dicke: In Holland during WW2, severe bread shortage until Swedish airplanes airdropped bread. Coeliacs relapsed in parallel with the bread drops: Dicke systematically showed how coeliac children benefited dramatically when wheat, rye and oats flour were excluded from the diet. As soon as these were excluded, the children's appetite returned and their absorption of fat improved so that the fatty diarrhoea disappeared. 1950: Paulley identified villous abnormality Later shown that the histological abnormality normalised after gluten withdrawal and recurred after gluten challenge Alpha-Gliadin Alpha-GLIADIN PEPTIDES (SYNTHETIC) FOR WHICH THERE IS IN VIVO EVIDENCE OF ACTIVITY 31 L-G-Q-Q-Q-P-F-P-P-Q-Q-P-Y-P-Q-P-Q-P-F 49 31 L-G-Q-Q-Q-P-F-P-P-Q-Q-P-Y 43 44 P-Q-P-Q-P-F-P-S-Q-Q-P-Y 55 Ingestion of gluten (or alpha-gliadin or even synthetic peptides) by a patient with coeliac disease causes symptoms in few hours and villous abnormality in 8-12 hours Why are gliadins toxic in some patients and not in others? Genetic factors First degree relatives: 10% risk MZ twin concordance: 70-90% HLA-identical sibs: 30-50% concordance In Europe: Coeliac patients >95% HLA-DQ2+ (vs. 25% in non-coeliacs) >99% of DQ2+ individuals do not have coeliac disease But significant component of genetic risk is accounted for by other non-HLA genes Immunological factors Increased immunoglobulin production in small intestine Most have circulating antibodies to alpha-gliadin ...but is this cause or an effect of the disease ? Antibodies to alpha-gliadin also seen in other intestinal diseases Other circulating antibodies also found in coeliacs Current hypothesis T-cell-mediated immunity of primary importance in pathogenesis Increased intraepithelial CD8+ T lymphocytes Increased CD4+ T lymphocytes in lamina propria Evidence of T-cell activation Theory of pathogenesis In a patient with a genetic predisposition... Some initial trigger? Adenoviral infection early in life?? Immune response including presence of T cells with specific ability to respond to alpha-gliadin peptides Theory of pathogenesis So later when any gluten-containing food is ingested…. Rapid T cell activation with Th1 pattern of cytokine release causing enterocyte apoptosis Enterocyte apoptosis leads to villous blunting/flattening Loss of surface area for absorption of nutrients clinically reflected as malabsorption Antibodies Sensitivity Specificity IgA 89% 95% IgG 99% 86% EMA >95% >95% tTG (IgA/IgG) >95% >95% AGA IgA tests negative in the 2-3% of coeliacs with IgA deficiency Presentation Any age: failure to thrive/short stature/wt loss Steatorrhoea, fat-soluble vitamin deficiency Diagnosis based on: Clinical suspicion Endoscopy with biopsy Serology: circulating antibodies Response to gluten withdrawal Complications Long term effects of malabsorption: chronic vitamin deficiencies Refractory sprue, ulcerative jejunoileitis, enteropathy-associated T cell lymphoma: all stages in a monoclonal lymphoid proliferation/lymphoma Controversial whether there is a small increase in risk of carcinoma or not dermatitis herpetiformis Dermatitis herpetiformis Chronic pancreatitis Exocrine pancreas Pancreatic secretions: 2-3 litres/day Secretion co-ordinated with presence of food in duodenum (via intestinal CCK) Proteases (trypsin, chymotrypsin, aminpeptidase) Pancreatic amylase Pancreatic lipases How does pancreas protect itself from self-digestion? Secreted as inactive pro-enzymes compartmentalised in granules Activation of pro-enzymes requires presence of activated trypsin Duodenal-derived enterokinase is required to activate trypsin Pancreas also secretes trypsin inhibitors Pancreatitis Acute (mild to severe necrotising/haemorrhagic) Chronic (result of repeated episodes of mild acute pancreatitis) Main causes: Alcohol, Gallstone disease Other: medications, trauma, hypercalcaemia, hyperlipidaemia, post-instrumentation, blockage of duct by parasites or tumour Pathogenesis of pancreatitis Gallstone disease: Duct obstruction Alcohol: ? Directly toxic to pancreas ? Altered secretions: leads to plugging of duct ? Sphincter of Oddi: alternate spasm/relaxation In both: pancreatic self-destruction by enzymes If chronic: scarring and loss of exocrine function Tests of pancreatic function Direct measure of enzymes in duodenal aspirate Indirect tests: Bentiromide test: NBT-PABA bond cleaved by chymotrypsin: measure urinary PABA metabolites Pancrealauryl test: Fluorescein dilaurate cleaved by pancreatic arylesterase: detect fluorescein in urine Malabsorption due to pancreatic dysfunction Clinical diagnosis Exclusion of primary small bowel disease Usually don’t need direct tests of pancreatic exocrine function Treatment: Oral enteric-coated pancreatic enzymes Small bowel bacterial overgrowth Normal small bowel: Low bacterial count Factors maintaining low count: Bacterial input from stomach is low due to stomach acidity Continuous peristaltic activity Secreted IgA Intact ileo-caecal sphincter Small bowel bacterial overgrowth Factors responsible for overgrowth: Stasis: strictures, fistulas, blind loops, dysmotility Achlorhydria Immune defects Small bowel bacterial overgrowth How does overgrowth causes malabsorption? Main mechanism is by inactivation of bile salts by direct deconjugation, dehydroxylation: interferes with micelle formation ? Also by directly inactivating enzymes ?? Competition for nutrients Small bowel bacterial overgrowth Tests for bacterial overgrowth: Jejunal aspirate: bacterial count Hydrogen breath tests: basal or after CHO load 14-C D-xylose: Urine xylose low: breath 14-CO2 Fairly common: Easily treatable Antibiotics: Tetracycline Outline of lecture Review normal digestion/absorption How diseases interfere with the process Tests for malabsorption Coeliac disease Chronic pancreatitis Bacterial overgrowth