ENVIRONMENTAL PATHOLOGY
advertisement

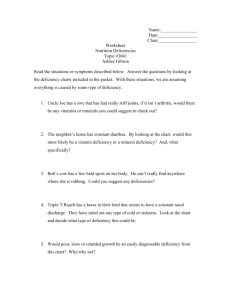
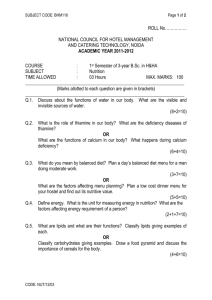
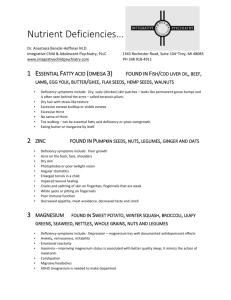
ENVIRONMENTAL PATHOLOGY Chemical and Physical Agents Nutrition David S. Wilkinson, MD, PhD Environmental Pathology Magnitude of the Problem in US • 600,000 cancer cases/year related to chemical carcinogens (est) • 400,000 deaths related to smoking • Reported Chemical Exposures – – – – 2.4 million reported chemical exp/yr (2005) 80% accidental Children <6 yo account for 50% 1261 fatalities, 50% suicides US Government Agencies Regulate Environmental Hazards • Environmental Protection Agency • Food and Drug Administration • Occupational Safety and Health Administration • Consumer Products Safety Commission Sources of Exposure • Environmental – Man-made • Intentional (Hg, Minimata, Japan) • Accidental – methyl isocyanate, Bhopal, India – radiation, Chernobyl – Natural (H2S/CO/CO2, Cameroon) • Occupational (mining, dye, chemical) • Iatrogenic (drugs) • Self-administered (substance abuse, suicide) Mechanisms of Toxicity • Corrosive, tissue destruction (acids, alkali) – desiccation – protein destruction • denaturation • hydrolysis – fat saponification • Inhibition of enzyme activity cyanide: cytochrome oxidase Cyanide Poisoning Mechanisms of Toxicity • Alternate metabolic pathways – ethanol: NAD/NADH • Disturbances of homeostasis – steroids: immune system – aspirin: acidosis • Mutagenesis • Carcinogenesis Clinical Findings • Symptoms-patient complaints • Signs-what you observe • Clinicopathologic correlation – related to mechanism and tissue localization • Acute vs chronic-the signs and symptoms may differ Lung Injury Related to Air Pollution • Acute and chronic inflammation – direct cell injury • Emphysema-enhanced proteolysis • Asthma-allergic or irritant effect • Hypersensitivity pneumonitis – immunologic injury related to organic dusts • Pneumoconiosis-cytokines • Neoplasia – mutagenic/promoting effects Main Constituents of Smog • SO2 respiratory irritant (acid rain) • NO2*, NO respiratory irritant (xs O2) • CO carboxyhemoglobin ( O2) • O3* respiratory irritant • Pb binds sulfhydryl groups *Oxidant pollutants Mostly produced by combustion of fossil fuels Inhalation Toxins Related to Mining and Similar Occupations Pneumoconiosis, characterized by cytokinemediated, progressive fibrotic scarring – coal dust (anthracosis) – silica (silicosis) – asbestos (asbestosis), Ca/Mg silicate • pleural plaques, mesothelioma, bronchogenic ca – beryllium (berylliosis) Macrophages produce cytokines Size matters-0.5 to 5μ Normal Lung Pulmonary Fibrosis Inhalation Toxins Related to Farming • Organic dusts (hypersensitivity pneumonitis) – moldy hay (Farmer’s Lung) – bird droppings (bird breeders lung) • Pesticides – organophosphate (acetycholine esterase inhibitors) – organochlorine (DDT, chlordane) • Herbicides (paraquat, diquat, dioxin) • Fertilizer (ammonia) Tobacco Smoking • 400,000 deaths/yr (21% of all deaths in US) • 50 Million smokers in US • Smoke composition – carcinogens (polycyclic HC, b-naphthylamine, nitrosamines) • Irritants and toxins – ammonia, formaldehyde, oxides of nitrogen • CO • Nicotine Relative Disease Risks Associated with Smoking Lung Ca death Mouth Ca Larynx Ca Esophogus Ca CAD >35 yo Cerebro VD >35 yo COPD Male 22 27 10 8 3 4 10 Female 12 6 18 10 2 5 10 Ill health effects of smoking partially reversible Heavy Metal Toxic Agents • Mercury (HgCl2 , ATN; org Hg, CNS function) • Lead ( inhibits heme synthesis, CNS function, kidneys, GI) – 2-11% of children in US exceed 10 μg/dL • Arsenic • Iron Lead Lines Basophilic Stippling Normal Kidney Acute Tubular Necrosis Organic Alcohols • Ethanol – 1/3 of Americans characterized as heavy drinkers – CNS depressant – legally intoxicated >100 mg/dL – Nearly 50% of fatal MVA • Methanol (toxic metabolites inhibit hexokinase, may cause blindness) • Ethylene glycol (antifreeze, ATN) Fatty Change in Liver Normal Liver Fatty Change in Liver Alcoholic Hepatitis Mallory Body Alcoholic Cirrhosis Alcoholic Cirrhosis Bands of Fibrosis Regenerating Nodules Adverse Drug Events Adverse Drug Reactions + Therapeutic Misadventures Adverse Drug Events • 3-6% of all medical admissions • 160,000 deaths/yr Shapiro et al. JAMA 1971; 216: 467-472. • Most common adverse event in hosp pts Leape et al. NEJM 1991;324: 377-384. • 6.5 ADE/100 admissions, 1% fatal Bates et al. JAMA 1995; 274: 29-34. Major Patterns of ADRs • Blood dyscrasias (Chloramphenicol) – dose related or idiosyncratic – pan or line specific • Skin eruptions (Penicillin) • Hepatic reactions – – – – fatty change (Tetracycline) cholestasis (Chlorpromazine) hepatitis (INH) massive hepatic necrosis (Halothane) Major Patterns of ADRs • Renal reactions – predictable (aminoglycosides) – hypersensitivity (sulfa) • Lung reactions – – – – congestion edema hemorrhage interstitial fibrosis Major Patterns of ADRs • Cardiac reactions – arrhythmias – cardiomyopathy • CNS reactions – respiratory depression • Systemic reactions – anaphylaxis – vasculitis – hormonal effects (HRT, OC) Syndromes Related to Drugs of Abuse • Pulmonary complications (edema, septic emboli, absess, opportunistic infections) • Granulomas (adulterants) • Infectious complications • Kidney disease Often related to diluents, cutting agents, and needle sharing Physical Injuries • Mechanical force – – – – abrasion laceration incision contusion • Gunshot wounds – entry wound – exit wound Contusion/22 hours Laceration with Marginal Abrasion Incision Stab Wound GSW/Contact GSW/Close Range/Stippling GSW/Distant and Contact Radiation Injury • Direct (target) effect-radiation acts directly on target molecules, such as DNA • Indirect effect-free radical intermediary • Cell death, mutations, developmental abnormalities • Tissues have differential radiosensitivity • Oxygen effect • Whole body radiation Radiation Injury Radiation Sensitivity of Biological Tissue • • • • • • Lymphocytes Thrombocytes Granulocytes GI lining Endothelial cells Neural tissue Sensitivity Most Sensitive Cell Division Fastest Least Sensitive Slowest Vitamin Deficiency Vitamin Function A D Vision Immune system Epithelium Deficiency State Diet, malabsorption Night blindness, xerophthalmia, keratomalacia, immune deficiency Blood calcium Diet, malabsorption, and phosphate inadequate sun, liver and renal disease Rickets, osteomalacia Vitamin Deficiency Vitamin Function Deficiency State E Antioxidant Diet, malabsorption tocopherols Free radical Neuromuscular scavenger deficits K Clotting Malabsorption, loss factors of gut flora, II, VII, IX, Coumadin therapy X bleeding Vitamin Deficiency Vitamin Thiamine (B1) TPP Function Enzyme cofactor, nerve conduction Riboflavine Enzyme co(B2) factor FMN, FAD Niacin Enzyme coNAD, factor NADP Deficiency State Diet, EtOH Polyneuropathy, cardiomyopathy, Wernicke-Korsakoff Diet, EtOH Cheilosis, glossitis, dermatitis (atrophy) Diet, EtOH Pellagra, dermitis, diarrhaea, dementia Vitamin Deficiency Vitamin Function Deficiency State Pyridoxine Enzyme co- Drugs (INH), EtOH (B6) factor Similar to riboflavin and niacin deficiency C HydroxylDiet, EtOH ation of Scurvey, weak proteins connective tissue Antioxidant Bleeding, fractures, gingival swelling, peridontal disease, poor wound healing