Document
advertisement
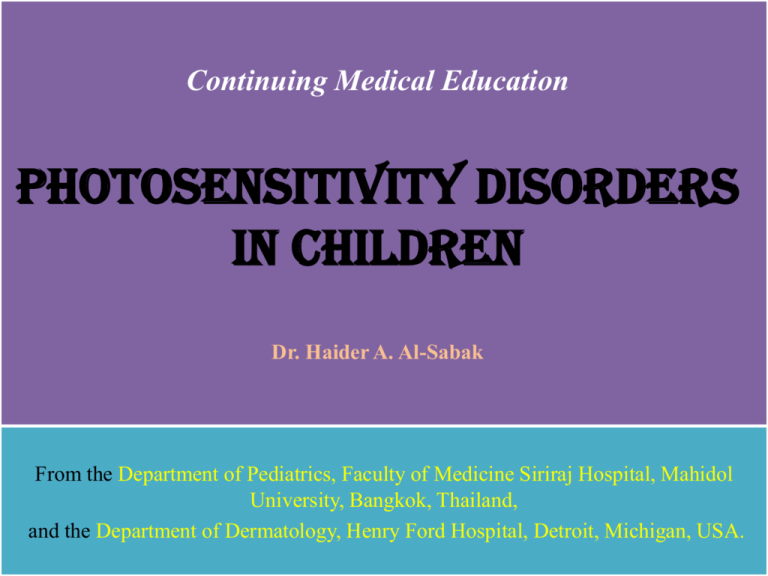
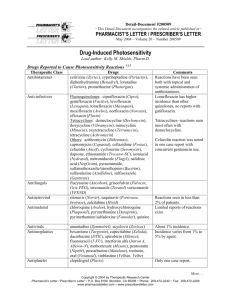
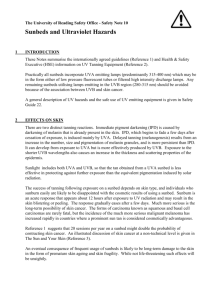
Continuing Medical Education Photosensitivity Disorders in Children Dr. Haider A. Al-Sabak From the Department of Pediatrics, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand, and the Department of Dermatology, Henry Ford Hospital, Detroit, Michigan, USA. Elecromagnetic Radiation Spectrum (EMR) Waveband Wavelength range (nm) X-ray 0.1 – 1 Vaccum UV 10 – 200 UV C 200 – 290 UV B 290 – 320 UV A 320 – 400 UV A II 320 – 340 UV A I 340 – 400 Visible Light 400 – 760 Near IR 760 – 1000 Far IR 1000 - 100000 Microwaves and Radiowaves > 1000000 The depth of penetration of UV to skin depends on WL Longer WL UVA easily reaches the reticular dermis; Shorter WL UVB absorbed in the epidermis Only 2% - 3% of UV radiation from the sun reaches earth’s surface UVB the major spectrum responsible for cutaneous erythema or Sunburn response, While UVA elicits a tanning response Recently, visible light induce a tanning response that is more persistent Both UVA & UVB exposures generate metalloproteinases & induce immunosuppression, & they therefore play a role in photoaging and photocarcinogenesis. Photodermatoses have their action spectrum in the UVA &/or UVB &/or visible light range Photosensitivity: defined as an abnormal or adverse reaction of the skin to UV or visible radiation, & rarely artificial light sources Genetic or metabolic defects, or underlying systemic dis. Child develops a sunburn reaction, swelling, or intense pruritus after limited sun exposure or develops an eruption, skin fragility, or scarring predominantly in sun-exposed areas The incidence of photodermatoses in the pediatric population is much lower than in adults Classification of pediatric photodermatoses I. Immunologically mediated photodermatoses Polymorphous light eruption Juvenile spring eruption Actinic prurigo Hydroa vacciniforme Solar urticaria II. Drug- and chemical-induced photosensitivity Exogenous Phototoxicity: systemic and topical Photoallergy: systemic and topical Endogenous cutaneous porphyrias III. Hereditary photodermatoses Caused by defects in nucleotide excision repair Xeroderma pigmentosum Cockayne syndrome, including cerebro-oculo-facio-skeletal syndrome Trichothiodystrophy Ultraviolet light sensitive syndrome Caused by double strand break repair defects RothmundeThomson syndrome Bloom syndrome Caused by abnormal chemical stubstances Smith-Lemli-Opitz syndrome Hartnup disease Others Kindler syndrome IV. Photoaggravated dermatoses Atopic dermatitis Darier - White disease Dermatitis herpetiformis Herpes simplex infection Lupus erythematosus and neonatal lupus erythematosus Juvenile dermatomyositis Pellagra Psoriasis Seborrheic dermatitis Diagnosis: • careful History taking and Physical examination • Hx: Age of onset , season, timing after sun exposure, the nature, duration, exposure to potential photosensitizers (both topical or systemic), systemic, suggestive of autoimmune dis., family history & consanguinity. • Eruption after exposure to window glass-filtered sunlight indicate action spectra in the UVA and/or visible light. • Exam: distribution of lesions, areas of sparing, photoprotected sites (upper eyelids, postauricular area (Wilkinson’s triangle), submental area, nasolabial folds and neck folds, the volar aspect of the wrist, and the antecubital fossae), & morphology. • Invest: CBC, Autoimm. profile, Screening plasma porphyrin level, Skin biopsy, Phototesting, Evaluation of growth parameters, developmental milestones, systemic involvement, and neurologic abnormalities, Chromosomal analysis and molecular genetic studies. • Polymorphous Light Eruption (PMLE): Prevalence: most com. type in children affects both adults and children +ve family history is reported in 3% to 56% of patients inverse relation to latitude C/F: few hrs (20-30 mint. or 1-2 days) Hardening. Symp. Non-scarring pruritic eruption on a sun-exposed area (common papular type to the relatively rare large papules, vesicular, plaque-like, urticarial, hemorrhagic, insect bite like, and even EM like). In skin of color pt. pinhead pap. Resolve comp. in absence of sun exposure in days. Rare sympt. Chills, headache, fever & nausea Polymorphous light eruption. A, A young white boy with widespread eruptions on the face. Note the erythema on the malar area and the bridge of the nose and sparing of the upper eyelid. B, A 10-year-old boy of Mexican and white descent with erythematous papules and excoriation on extensor forearms and wrists after sun exposure. Diagnosis: Histopathology: Phototesting: Most PMLE pts have normal (MEDs) to UVA & UVB However, reports showing decreased MED values to UVA or UVB. Dx. can be confirmed by evaluating the patient after exposure to sunlight or by performing provocative phototesting in the clinic, by exposing the skin either to multiples of MEDs or to suberythemogenic UV doses for 3 to 4 days followed by evaluation 1 to 2 days later for the development of characteristic PMLE lesions. Pathogenesis: Delayed HR to endogenous, cut. UV induced Ag. PMLE pt. less likely to be photoimmunosuppressed, but repeated UV exposure, photoimmunosuppression occurs; this explains why patients tend to improve as the sunny season progresses. D.Dx: AD, SLE, EPP, SU, HV & photosensitivity induced by exogenous agents Treatment: Proper photoprotection Symp. Rx topical steroid Pophylaxis 5-7 days prednisone, 0.6-1 mg/kg/day or if reccurant NBUVB or PUVA (3 times/wk for 5 wks) in early spring Other antimalarial agents, beta-carotene & nicotineamide. • Juvenile Spring Eruption (JSE): C/F: localized form of PMLE Boys > girls, age 5-12 yrs, spring season Pruritic erythematous papules usually confined to the helix of the ears & evolve into vesicles & crusts & heal with minimal or no scarring. Histopathology & Phototesting Pathogenesis: remain unknown, similar to PMLE Treatment: Proper photo protection & Symp. Rx • Solar Urticaria (SU): Prevalence: uncommon form of physical urticaria and is also a rare subtype of IMP, age (1st wk – 8th decade) C/F: urticaria, headache, nausea, wheeze….etc & anaphylaxis Diagnosis: Phototesting , caution……anaphylactic reaction Com. UVA & visible, less UVB, IR….heat urticaria Pathogenesis: immediate type HR. D.Dx: PMLE, EPP, drug induced photos. Treatment: Proper photo protection & Symp. Rx Hardening NB-UVB with caution Beta-carotene, antimalarial drugs, plasmapheresis (removal of a circulating serum factor/photoallergen), systemic immunosuppressive agents, & IVIG have been reported to be effective in adults. • Hydroa Vacciniforme (HV): C/F: boy > girls, mean age 8 yrs, resole spont. in adulthood Recurrent crops of discrete 2-3mm erythematous macules evolve into blisters hrs to a 1-2 days after sun exposure. Healing occurs within days, with umbilication followed by crusting & pitted, varioliform scarring. Adverse effect on quality of life. Rare presentations ocular involvement (keratoconjunctivitis & uveitis) & blistering of the lips. Histopathology: Phototesting: UVA in monochromatic phototesting…papulovesicular Pathophysiology: not clarified. (Latent EBV infection), some cases reported in adult (fatal) different from that of children. D.Dx: EPP, vesicular PMLE, bullous SLE, & PCT. Treatment: Photoprotection, Chloroquine, beta-carotene & PUVA. In severe cases, systemic corticosteroid. Hydroa vacciniforme. A, A 7-year-old boy with vesicles and crusts on the malar area a few days after sun exposure. B, A boy with pox-like scars on the left cheek. • Actinic Prurigo (AP): Prevalence: Indian and Mestizo (mixed ancestry), Mexico & Central & South America, living at high altitudes. strong association with HLA DRB1*0407 C/F: age 2-43 yrs. (mean <10yr) intensely itchy papules, plaques, & nodules, excoriations and scars on sun-exposed area, 2ndry eczematization & lichenification. Very shallow linear, flat, or punctate scars may occur on the face. Other: bach & buttock, cheilitis, conjunctivitis, pseudopterygium & eyebrows alopecia. Diagnosis: Histopath., Phototesting, D.Dx Treatment: Photoprotection (sunglass, lip balms), topical steroid, antihistamin, emollients, others (Chloroquine, beta-carotene, Vit.E, pentoxyphillin), PUVA & NB-UVB effective. Thalidomide (50-100mg/day……50mg) most effective Rx S/E teratogenic, peripheral neuropathy Actinic prurigo: Note the erythematous papules that have coalesced to form a plaque on the right cheek, V of the neck, and extensor surfaces of both distal arms and forearms of an 8-year-old girl • Chronic Actinic Dermatitis (CAD): replaced the terms persistent light reactivity, actinic reticuloid, photosensitive eczema, & chronic photosensitivity dermatitis. a persistent, chronic, eczematous eruption in the absence of exposure to known photosensitizers usually broad-spectrum photosensitivity with decreased MED to UVA &/or UVB, and at times visible light histology consistent with a chronic dermatitis, with or without features of lymphoma C/F: middle-aged or elderly men, edematous, scaling, thickened patches & plaques that tend to be confluent, involvement of unexposed sites, progressing to erythroderma in the most severe cases. Marked depigmentation (vitiligo). Patients may not realize their condition is exacerbated by light. It may persist in all seasons. Pathogenesis: unknown. In some patients a preceding topical or oral photosensitizer. Dx established by histologic evaluation and phototesting The finding of photosensitivity to UVA and UVB helps to differentiate chronic actinic dermatitis from drug-induced photosensitivity D.Dx: PMLE, photoallergic CD, airborne CD, & MF or Sézary syndrome Treatment: includes identifying & avoiding possible topical photosensitizers by photopatch testing. Maximum sun avoidance & broad-spectrum sunscreens. • Topical tacrolimus is useful in some patients. Top. & sys. steroids. • Azathioprine, 50–200 mg/day, is the most effective Rx & may be required annually during periods of increased sun intensity. • Low dose PUVA, but is often not tolerated, even with steroid • Hydroxyurea, 500 mg twice a day. Cyclosporine A, thalidomide, & mycophenolate mofetil may also be utilized. Immunosuppressive agents may allow patients to tolerate PUVA therapy. DRUG & CHEMICAL-INDUCED PHOTOSENS. Photosensitivity by Exogenous Sensitizers: Rare in children, eiher phototoxic or photoallergic (next table) Almost all induced by UVA bec. Pentrate window glass, in lamp of tanning booth, nail salon, dentist office, photocopy machine…etc NB-UVB safe Phytophotodermatitis: Plant-induced photosens. most common phototoxic reaction of children, Citrus fruit (lemons & limes)…etc UV-induced eruption in day after exposure to the furocoumarin & sunlight, severity from erythema to blistering & characteristic hyperpigmentation. Linear streaks of hyperpigmentation, face, chest, hands, and lower legs of children, over 1-2 wks & persist 6-12 months. Differentiating features of phototoxic and photoallergic reactions Feature Phototoxic Clinical manifestations Occurrence after first exposure Yes Onset of eruption after exposure Minutes to hours Dose of agents needed for reaction Large Cross reactivity with other agents None Clinical changes Similar to sunburn reaction Distribution Histologic findings Pathophysiology Diagnosis Topical agent Systemic agent Photoallergic No 24-48 hrs Small Common Varied morphology, usually eczematous lesions Exposed skin only Exposed skin, may spread to unexposed area Necrotic keratinocytes, epidermal Spongiotic dermatitis degeneration, & dermal inflammation Direct tissue injury Cell-mediated immune response Clinical Clinical and phototest Photopatch test Clinical and phototest; possibly photopatch test Phytophotodermatitis: A 9-year-old boy with a linear hyperpigmented streak on the right arm a few days after exposure to lime and sunlight Most com. Drug Antibiotics (sulfonamides, quinolones, & tetracyclines). Systemic phototoxic agents, Antibiotics (doxycycline, tetracyclines, sulfonamides, nalidixic acid, and fluoroquinolones), Antifungal (griseofulvin), sulfonylurea hypoglycemic agents, furosemide, NSAID, amiodarone, quinine, isoniazid, & thiazide diuretics. Photoallergic agent: com. UV filter octocrylene, benzophenone-3, & butyl methoxydibenzoylmethane. Treatment: The 1st line is removal of photosensitizer; restriction of UV radiation exposure. Good broad spectrum sunscreens need to be used because the action spectrum is in the UVA range. Endogenous Chemical-induced Photosensitivity: Cutaneous Porphyrias (CPs) They are a group of inherited & acquired disorders that are caused by a specific enzymatic defect in the heme biosynthesis pathway. Heme is assembled from simple precursors in an 8-step pathway Each step is catalyzed by a different enzyme, represent partial def., bec. complete enzyme def. in the pathway is not compatible with life. Heme produced in RBC for Hb synthesis & in hepatocytes for synthesis of cytochromes & hemoproteins. So (hepatic or cutaneous) Porphyrins, are potent photosensitizers in CPs, major action spectrum (400-405 nm) (the Sorbet band), minor (600-650 nm) (visible red); Dihydroxyacetone, sunless tanning, blocking longer UVA & visible light. It can provide excellent protection in cases of CPs. Differences in water solubility reflect the clinical features. Heme biosysthetic pathway and sites of enzymatic defect in cutaneous porphyrias. ALA,Aminolevulinic acid; CEP, congenital erythropoietic porphyria; CP III oxidase, coproporphyrinogen oxidase; EPP, erythropoietic protoporphyria; HC, hereditary coproporphyria; HEP, hepatoerythropoietic porphyria; PBG, porphobilinogen; PCT, porphyria cutanea tarda; PP III oxidase, protoporphyrinogen oxidase; URO decarboxylase, uroporphyrinogen decarboxylase; URO III synthetase, uroporphyrinogen III synthase; VP, variegate porphyria Congenital Erythropoietic Porphyria (CEP): Gunther dis., autosomal recessive dis.most disfiguring form caused by def. of UROS III, results in a shift from production of III to I isomers of uroporphyrinogen & coproporphyrinogen . C/F: dark colored urine during infancy, fluoresces red (Wood’s lamp), severe photosensitivity in 1st 2 or 3 yrs of life, splenomegaly, & hemolytic anemia. Patients show signs of discomfort after sun exposure, although they cannot verbally communicate. Phototherapy during the neonatal period for hyperbilirubinemia may lead to generalized blistering. When teeth erupt, they are dark colored, & Wood’s lamp +ve bec. porphyrins bind to dental calcium phosphate. Hypertrichosis & hyperpigmentation of the face & extremities, Ocular involvement, photophobia, corneal scarring, ulceration, ulcerative keratoconjunctivitis, & cataracts. Hemolytic anemia with hypersplenism. Bony involvements include osteodystrophia, combining osteolysis & osteoporosis; hypercellular bone marrow is present. These changes may lead to bone fragility and fracture Congenital erythropoietic porphyria: A, Teeth showing pink to brown color. B, The teeth fluoresce pink under examination with a Wood’s lamp because porphyrins bind to dental calcium phosphate (erythrodontia). Congenital erythropoietic porphyria: A, Urine stained on diaper from an infant with congenital erythropoietic porphyria. B, Urine fluoresced pink under examination with a Wood’s lamp Congenital erythropoietic porphyria: A, A 10-month-old white female with mutilating ulceration and scarring secondary to recurrent eruption of vesicles and bullae. B, Hypertrichosis on the face when the same patient was 28 months old (after bone marrow transplantation) Diagnosis: Biochemical changes: uroporphyrin I & coproporphyrin I in RBC, BM cell, plasma, urine & feces Wood’s lump: reddish orange porphyrin fluorescence in urine or aqueous suspension of feces Hematological changes: normochromic anemia, reticulocyte count Skin biopsy Prenatal Dx. Treatment: rigorous sun avoidance, protective clothing, use of opaque sunscreens containing nonmicronized titanium dioxide or zinc oxide that block in the visible spectrum. Beta-carotene, Hypertransfusion and splenectomy, Bone marrow and allogeneic stem cell transplantation The prognosis of the severe form is poor. Death---hemolytic anemia Erythropoietic Protoporphyria (EPP): Most com. in childhood CPs, partial def. in FECH enz. when only <50% of normal action. Mode of inheritance is complex, autosomal recessive EPP less com. & ass. With severe liver disease. C/F: Accumulation of free protoporphyrin, in RBC & 2ndly in tissue (skin & liver) or biologic specimens (serum, bile, &feces), leads to painful photosensitivity & potential liver complications. EPP usually becomes symptomatic between 1 & 6 years of age because of the photosensitivity. The average age is 4 years Immediate painful reaction within mint. of sun exposure. Severe burning pain in hands & feet & the face---cold air & cold water. Crying upon exposure to sunlight occurs in young children. Chronic lesions are common, thickening of skin on the knuckles & subtle scarring on the bridge of the nose, increased rugosity of the upper cutaneous lip. Erytropoietic protoporphyria: A 12-year-old boy with vesicles and thickening of the skin over the knuckles. Hypochromic & microcytic anemia. Liver dysfunction in 10% to 20% of EPP patients. Incidence of cholelithiasis in 2% ---irreversible cholestatic liver failure develops Biochemical changes: free protoporphyrin in RBC, plasma, bone marrow cells, and feces. It is highly lipophillic, urinary porphyrin levels are normal, unless the patient is in hepatic failure. Examination under a fluorescence microscope--- +ve in RBC. Plasma fluorescence emission spectroscopy shows a ccc peak at 634 nm Treatment: photoprotection, opaque sunscreen, beta-carotene (30-150 mg in children), cholestyramine (4g/day), chenodeoxycholic acid (15 mg/kg/day), Recently, subcutaneous implants of alfa MSH analog Liver transplantation Porphyria Cutanea Tarda (PCT) & Hepatoerythropoietic Porphyria (HEP): PCT most common form of porphyria in adults & the 2nd most common form in children. Heterozygous deficiency in uroporphyrinogen decarboxylase causes PCT, whereas homozygous deficiency in this enzyme results in HEP. PCT Age 3rd-4th decade o Type I: sporadic PCT o Type II: familial form o Type III: C/F: Skin fragility most common, erosions, vesicles, or bullae on sunexposed cutaneous surfaces, esp. the dorsal aspects of the hands & forearms, The blisters vary in size from 1 mm-3 cm., milia, infection. The lesions heal with hyperpigmentation; Periorbital hypertrichosis & mottled hypo & hyperpigmentation are frequently present Rarely sclerodermoid changes only finding in sun-exposed & protected sites, ocular pain, photophobia, scleral perforation. In adult PCT ass. with, iron overload, hepatitis C, alcoholic cirrhosis, hemodialysis, administration of estrogens, hydantoins, or griseofulvin, HIV infections, & hemochromatosis. Dx: levels of plasma, urinary & fecal porphyrins, with predominance of uroporphyrin (8-carboxyl porphyrin) & 7 carboxyl porphyrin in plasma & urine, & isocoproporphyrin in feces. Fluorescence emission spectroscopy of plasma shows a ccc peak at 620 nm. Treatment: like other porphyria…….. low-dose hydroxychloroquine treatment (3 mg/kg twice a week) Clinical improvement, which precedes biochemical improvement, is observed in 4-6 months. Urinary & plasma concentration of porphyrin monitored every 3 months. Phlebotomy is the treatment of choice in adult cases Prognosis: 5-16% of untreated pt.------hepatocellular CA HEREDITARY PHOTODERMATOSES Caused by defects in nucleotide excision repair (NER): The NER pathway serves to repair DNA damaged by UV radiation, chemical carcinogens, & other non UV-induced oxidative damage. 28 proteins in the NER pathway. NER-------normal development, (the nervous system). Complex relationship between clinical phenotypes and the molecular defects in NER. Different defects in 1 gene may lead to different C/F. Xeroderma Pigmentosum (XP): autosomal recessive dis. ccc by marked photosensitivity, ocular, & increased risk of cutaneous malignancy. Patients with XP have defects in NER causing decreased ability to repair DNA damage induced by UV radiation Prevalence is increased in communities of common consanguinity. The disease is categorized into 7 complementation groups, A through G, & a variant subtype Each group has a specific genomic deficit. C/F: Onset, 1 & 2 years of age. The most common is photosensitivity. 50% of affected pts have a history of acute sunburn reaction with blistering or persistent erythema after minimal UV exposure. more severe photosensitivity later develop neurologic abnormalities. The other 50% of the pts tan normally without excessive erythema. Marked freckling of sun-exposed areas presents in most pts before 2 yrs of age, continued sun exposure causes actinic damage, such as dry & parchment like skin with hyperpig., poikiloderma, & AK. XP is an example of accelerated photoaging, with pts developing non-melanoma skin cancers at a mean age of 10 years. Patients who are <20 years of age have a greater than 1000 fold increased risk of cutaneous BCC, SCC, or melanoma. Multiple primary cutaneous neoplasms are common. Fig 1. XP. A 10 month-old boy presenting with developmental delay and marked freckling on the face and sun-exposed area. Fig 2. XP. An 8 year-old girl presenting with dry and parchment-like skin with hyperpigmentation, and multiple pigmented BCC on the face. Both eyes showed corneal opacification. o Eye features in XP is almost as common as the cut. C/F, onset median age of 4 years, anterior portion of the eye (exposed to sunlight). o Chronic UV-induced conjunctivitis and keratitis leading to corneal opacification and vascularization…inflammatory lesions (pingueculae and ptergyia). o Atrophy of the skin of the eyelids (ectropion, entropion &, in severe cases, complete loss of the lids). o Epithelioma, SCC, & melanoma of UV-exposed portions of the eye o About 30% of XP patients have a progressive neurologic deg., especially, pts with XP/CS complex, onset may be early in infancy or delayed until the 2nd decade of life. The earliest C/F are diminished or absent deep tendon reflexes & high frequency hearing loss. o Others, microcephaly, progressive intellectual deterioration, spasticity, ataxia, or seizure. Swallowing difficulties, leading to aspiration of food. o 10-20 fold increase in internal CA, (brain, lungs, hematopoietic system, kidney,& gastrointestinal tract). -----die 20 years of age. o A small no. of XP pts have C/F of XP & other dis. with NER defects, Patients with the XP/CS complex have skin and eye disease of XP and the somatic and neurologic abnormalities of CS. o In XP/TTD syndrome, previously known as photosensitivity, ichthyosis, brittle hair, intellectual impairment, decreased fertility, and short stature (PIBIDS) syndrome, they do not show an increased risk of developing skin cancer. o XP variant have skin & eye C/F identical to other forms of XP (high rate of skin cancer) but don’t have a defect in NER. Most XP variant pts don’t have XP neurologic abnormalities. Dx: by C/F, • Functional tests on living cell, to screen for abnormalities in DNA repair. Cells from individuals with XP with defective NER are hypersensitive to killing by UV in comparison to normal cells; cells from individuals with the XP variant may have normal or near normal post-UV cell survival. Management: • All patients with XP require strict life-long sun protection with UVblocking protective clothing, high SPF broad spectrum sunscreens, UV-absorbing glasses with side shields, & hats. • Vitamin D (age 0-1 year, 400 IU/day; age>1 year, 600 IU/day) is recommended to prevent deficiency from sun avoidance. • Methylcellulose eye drops should be applied to keep the corneas moist, & soft contact lenses should be worn to protect against mechanical trauma in individuals whose eyelids are severely deformed. • Corneal transplantation may be required for patients with severe keratitis & corneal opacity. • Premalignant & malignant skin dis. should be treated. Oral isotretinoin, 0.25 to 2 mg/kg has been used for prevention of non melanoma skin CA. In order to reduce the occurrence of side effects that are dose dependent, initiating low doses of retinoids & gradually increasing according to the patient’s response. • Cockayne syndrome (CS): a rare autosomal recessive disorder with ccc facies, extremely short stature, immature sexual development, & multisystemic degeneration. It results in a reduced lifespan but NO increased incidence of CA. CS is caused by defects in the repair of actively transcribed DNA; 2 genes responsible for CS (ERCC8 & ERCC6). Mutations in ERCC8 cause CS type A (CSA, 25%) & mutations in ERCC6 cause CS type B (CSB, 75%); both CSA and CSB have identical phenotypes. CS spans a wide spectrum of diseases, & classified into 3 groups: They are type I (classic CS), type II (early-onset CS), & type III (mild or atypical CS). Recently, a fourth newly documented group, UV sensitivity only/adult onset. Pts with CS are normal at birth but experience postnatal failure of brain growth. They have a ccc facies with deep set eyes, prominent ears, & a wizened facial appearance. The major C/F of CS are postnatal growth failure, neurologic deg., photosensitivity, pigmentary ‘‘salt and pepper’’ retinopathy, cataracts, sensorineural hearing loss, cachectic dwarfism, & immature sexual development. photosensitive but without pigmentary changes or increased skin CA frequencies as seen in XP, premature aging & results in early death. Others: dental (absent or hypoplastic teeth & delayed teeth eruption); renal (abnormal renal function & pathologic abnormalities); endocrine (undescended testes); cutaneous (anhidrosis and malar rash); & GI abnormalities (abnormal liver function & hepatosplenomegaly). The average lifespan in CS is 12 years. Dx: C/F & Sequence analysis for both genes is clinically available. Treatment: no effective Rx, most patients die by the 3rd decade of life as a result of arteriosclerotic vascular disease, profound neurologic deterioration, or both. Physical therapy prevents contractures & maintains ambulation, while gastrostomy tube placement prevents malnutrition. Spasticity may be alleviated by medication. Hearing loss, cataracts, other eye dis. & dental caries are treated as in the general population. The use of sunscreens & sunglasses & avoidance of excessive sun exposure are helpful. Surveillance includes yearly assessment for complications, including HTN, renal or hepatic dysfunction, & declining vision & hearing. Trichothiodystrophy (TTD): Heterogeneous group of autosomal recessive disorders ccc by sulfurdeficient brittle hair with neuroectodermal manifestations. To date, 4 genes responsible for TTD: XPD, XPB, p8/TTDA, & TTDN1 (TTD nonphotosensitive 1). Approx. 110 patients have been reported to date. C/F: remarkably varied, ranging from only hair involvement to severe neurologic & somatic developmental abnormalities. The hairs sparse, short, dry, & brittle (Next fig); break easily with trauma. Light microscopy reveals hairs with a wavy, irregular outline & a flattened shaft that twists like a folded ribbon. Polarizing microscopy shows ccc alternating light and dark bands,‘‘tiger-tail’’ appearance. 50% of pts (XP/TTD syndrome), also known as PIBIDS syndrome. Pts may born premature or small for their gestational age, & they have a high frequency of cong. cataracts & of multiple infections. Skeletal abnormalities, peripheral osteopenia & central osteosclerosis Neurologic manifestations, (developmental defects, microcephaly, intellectual impairment, & ataxia). Nail abnormalities, such as onychodystrophy, splitting, ridging or thickening, decreased fertility, & features of premature aging may be observed; no specific treatment is available. Ultraviolet-sensitive syndrome UV(S)S: • was first described by Itoh et al in 1994. They reported 2 DNA repairdefective siblings with mild C/F similar those of XP; • defective transcription-coupled repair (TC-NER), the subpathway of NER. & it is genetically heterogeneous, with mutations in (ERCC6). • C/F: photosensitivity, dryness with freckling and pigmentation anomalies of sun-exposed areas, & telangiectasia. • Unlike other photosensitive dis., no neuro. Or developmental signs, & no tendency to skin CA. Trichothiodystrophy. Note the sparse, short, dry, brittle hairs. Trichothiodystrophy. A, Light microscopy shows hairs with irregular outline and a flattened shaft. B, Under polarizing microscopy, the characteristic alternating light and dark bands, the ‘‘tiger-tail’’ appearance, is evident Hereditary photodermatoses caused by double strand break repair defects (DSBR): This pathway is implicated in maintaining genomic stability. DNA double-strand breaks (DSBs) can promote genomic instability resulting in chromosomal abnormalities. There are 2 dis. RTS & BS. Rothmund-Thomson syndrome (RTS): also known as poikiloderma congenitale, is a rare autosomal recessive disorder ccc by poikiloderma, sparse hair, sparse eyebrows/ lashes, small stature, skeletal abnormalities, cataracts, and an increased risk for cancer, especially osteosarcoma. Gene mutations is RECQL4 gene in 66%, with risk of osteosarcoma. C/F: Erythema, swelling, & blistering of the face that develops in infancy, generally at 3 to 6 months of age, with sparing of the trunk & flexural areas, then evolves into reticulated hyper- & hypopigmented patches, telangiectases, & areas of punctate atrophy. The eruption extends to extensor surface of the extremities, trunk, abdomen, & buttocks. Keratotic lesions in 1/3 of cases on the elbows, knees, hands, & feet. Palmoplantar keratoderma. Sparse hair, eyelashes, &/or eyebrows. Nail abnormalities, and gastrointestinal disturbances. Juvenile cataract, prevalence of<10%. Many individuals tend to be small for gestational age at birth, & have small stature throughout life. The majority of individuals (75%) have radiographic finding of the bone (dysplasias, absent or malformed bones, or delayed bone formation) & dental abnormalities (rudimentary or hypoplastic teeth & increase incidence of caries). Osteosarcoma is the most common malignancy in RTS, (prevalence 30% & median age of onset at 11 years of age). Othere, BCC, SCC & melanoma, prevalence 5%. Rothmund-Thomson syndrome. A, Widespread poikiloderma, sparse hair, some keratotic papules on the trunk & extremities. B, Plantar hyperkeratosis. C, Sparse hair & scarring alopecia on the crown area. D, Absence of radii & thumbs on both hands. Bloom syndrome (BS): also called congenital telangiectatic erythema, is a rare autosomal recessive disorder that is associated with a predisposition to cancer. 80% of affected children are male. Higher prevalence within the Ashkenazi Jewish population Mutations in the gene Bloom helicase (BLM helicase or BLM ) lack of BLM protein may lead to tumor formation C/F: ccc of severe pre & postnatal growth retardation, sun-induced chronic erythema, type II diabetes in 17.7%, & frequent infections. The most striking C/F is proportionate dwarfism with highly ccc sparseness of subcutaneous fat tissue. BS patients are usually small for gestational age. Lack of interest in feeding. Cutanuous features in the first few years of life inform of Erythematous patches & telangiectasia arise on sun-exposed areas, Loss of the lower eyelashes & blister & fissure of the lower lip. Multiple cafe-au-lait spots with neighboring hypopigmentation Gastroesophageal reflux--------repeated otitis media & pneumonia BS pts are prone to CA., mean age 24 years, & death before 30 years Lymphomas & leukemia occur 150 to 300 times than normal, CA of GIT, (colorectal CA), respiratory tract, skin, breast, & liver; hematologic malignancy, acute leukemia & lymphoma; connective tissue sarcoma; retinoblastoma; & brain tumor. Chronic bronchitis & bronchiectasis are also common. Most pts have normal intelligence. Women fertile, but menopause occurs early, whereas men are infertile. Dx: confirmed by molecular genetic analysis of BLM. The cutaneous findings in BS have a tendency to improve with age. Rx: Avoidance of sun exposure & protection by clothing & sunscreens can prevent some of the cutaneous eruptions associated with photosensitivity. Appropriate antibiotics for infections & control of gastroesophageal reflux. Patients should be followed closely for early signs of neoplasm. Hereditary photodermatoses caused by abnormal biochemical substances Smith-Lemli-Opitz syndrome (SLOS): • Autosomal recessively inherited syndrome caused by an abnormality in cholesterol metabolism resulting from deficiency of the enzyme 7dehydrocholestrol (7-DHC) reductase. • Growth and mental retardation & hypospadias are common. • Photosensitivity in the UVA light range 73% of patients. • Dx is made based on C/F & detection of elevated serum concentration of 7-DHC. Although serum concentration of cholesterol is usually low, it may be in the normal range in about 10% of patients. • Sequence analysis of DHCR7 detects 96% of known mutations. • Objective improvement in clinical symptoms including photosensitivity shown after supplementation with cholesterol. • Photoprotection, including sun avoidance, is recommended. • Early intervention & physical/occupational/speech therapies for identified disability should be encouraged Hartnup disease (HD): Rare autosomal recessive metabolic disorder caused by impaired gastrointestinal & renal transport of neutral amino acids, including tryptophan. Clinical presentations are attributed to defective transport of tryptophan & a consequent decrease in nicotinic synthesis; its clinical symptoms are similar to niacin deficiency (pellagra). Patients present with pellagra-like skin eruptions, cerebellar ataxia, and gross aminoaciduria. Mutations in SLC6A19 encoding the neutral A.A. transporter B0AT1. The onset of disease in children is 3 to 9 years of age. Dx: elevation of neutral amino acids in urine. Plasma amino acid concentrations are usually normal. Rx: avoidance of sunlight exposure & high protein diet intake. In patients with niacin deficiency & symptomatic disease, prolong oral administration of high doses (100-250 mg daily) of nicotinic acid or nicotinamide is recommended. Other hereditary photodermatoses Kindler syndrome (KS): Kindler syndrome is an autosomal recessive genodermatosis associated with mutations in FERMT1 Kindler syndrome is ccc by poikiloderma, skin and mucosal fragility, trauma induced skin blistering, photosensitivity, & an increased risk of cancer. PHOTOAGGRAVATED DERMATOSES • Photoaggravation is well documented in this group of diseases, but the pathophysiology is poorly understood Atopic dermatitis • 3% of patients with AD; the majority are female • 2 clinical reaction patterns; photosensitive AD & AD with coexisting PMLE. Darier disease • DD can be exacerbated by UVB irradiation, heat, friction, & infection. Juvenile dermatomyositis • Photosensitivity clearly is a part of dermatomyositis, but the pathogenesis remains unknown. Lupus erythematosus and neonatal lupus erythematosus There is a clear relationship between UVR & the C/F of LE. UVR may induce or exacerbate the cutaneous lesions & systemic manifestations associated with the diseases of LE. The American College of Rheumatology defines photosensitivity in their criteria for diagnosis of SLE as ‘‘unusual skin reaction from exposure to sunlight by patient’s history or physician’s observation”. This college also define photosensitivity, • 57% - 73% of patients with SLE, • 50% - 90% with SCLE, • 50% with DLE, • & nearly all with tumid LE (LET) It is difficult for patients with LE to link sun exposure with their skin lesions, because of a delayed time interval between UV exposure & the exacerbation of skin lesions. Neonatal lupus erythematosus. A, A 2-month-old infant presenting with scaling annular erythema on the face. B, Characteristic ‘‘owleye’’ appearance in a patient with neonatal lupus erythematosus. Pellagra Pellagra is a systemic disturbance caused by a cellular deficiency of niacin; it is clinically manifested by the 4 D’s: photosensitive dermatitis, diarrhea, dementia, & death. Pellagra is the late stage of severe niacin (vitaminB3) deficiency. 4 theories in photosensitivity have been proposed: (1) cutaneous deficiency in urocanic acid; (2) accumulation of kynurenic acid; (3) deficiency of nicotinamide adenine dinucleotide/nicotinamide adenine dinucleotide phosphate; (4) altered porphyrin metabolism. Exposure to UVA, UVB, & visible light has been reported to induce photosensitivity in pellagra. Thank you