Basic Health Assessment: The Physical Exam
advertisement

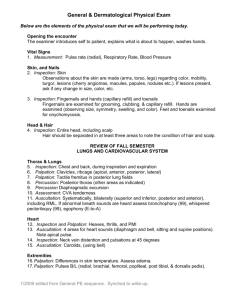
Basic Health Assessment: The Physical Exam ALLWISE Publications Pat Camillo PhD,RNC,ARNP-BC May 1, 2003 Important Points Before You Begin! • Purpose of the PE is to uncover variations from normal – SO, you must know the range of normal! • The history is a continuous process and will continue throughout the PE • Surprises should be avoided – always explain what you are doing • Professional demeanor is critical- maintain eye contact, avoid inappropriate jokes, watch non verbal behavior • Be prepared! The General Survey • Begins the moment the person enters the office! • Observe for the following: – Appearance (frail, posture, stature, weight, gait, facial expression) – Behavior (agitated, restless, argumentative, oppositional) – Odors (alcohol, acidosis, poor hygiene) – Speech (fast, slow, hoarse) – Signs of distress (pain, breathing, limping) – Determine if an in depth mental status exam is needed prior to continuing. Vital Signs • • • • Pulse Respiratory rate Temperature Blood pressure Key Techniques • • • • Inspection Palpation Percussion Auscultation Inspection • Must learn to inspect and observe, not just see! • Be aware of symmetry and asymmetry. • Need adequate lighting • Need adequate exposure • Helpful instruments: penlight, otoscope, opthalmoscope, nasal speculum, vaginal speculum. Palpation • Touch is a diagnostic tool! • Characteristics to note: hard, soft, hot, cold, rough, smooth • Fingertips are the most sensitive to touch • The palm is most sensitive to vibrations • Then ulnar and dorsal surface of the hand is most sensitive to temperature How to Palpate • Always start with light palpation! • Deep palpation follows (esp. in abdominal exam) • Technique for deep palpation: Place the fingers of one hand over the area to be palpated – then place the fingers of the other hand right in front of the first set of fingers and push deeply with both hands. Percussion • The process of striking a portion of the body to evaluate the condition of underlying structures. • Blunt percussion can produce pain when an underlying structure is inflamed (as in a kidney infection) • Commonly, percussion uses the fingers to create vibrations on the body surface How to Percuss • Place the middle finger of the left hand firmly over the area to be percussed. This is called the pleximeter finger. • The percussion blow is struck by the tip of the middle finger of the right hand. • If you are left handed you need to switch the above instructions . • You want to use the tip of the finger – not the pad – otherwise you won’t get a good, clear sound. SO……….nails must be short! • Hint: The action is in your wrist – not your arm! Sounds Produced with Percussion • The action must be brisk and short in order to produce a sharp, clear sound. • The kind of sounds produced depend on the nature of the tissue under the pleximeter. • PRACTICE…..PRACTICE….PRACTICE Normal Percussion Sounds • Resonance – low pitched – normal in the lung. To hear this - try percussing the right anterior thorax above the level of the breast. • Dullness – Higher pitched sound heard over solid tissue……..try the heart or liver. • Tympany – VERY low pitched – often in the abdomen, in areas where air dominates. Other Percussion Sounds • Flatness – ABSOLUTE dullness…….what you hear when you percuss the thigh. • Hyperresonance – Even lower than resonance – what you would hear if you percussed an air-filled lung as in a pneumothorax. NOTE: Percussion only goes so far – structures smaller than 4 or 5 cm or more than 4 or 5 cm deep – are out of reach! Auscultation • The stethoscope should be fairly thick, about 12-15 inches long and should have both a bell and diaphragm. • It should fit YOU properly – ear canals come in all sizes • The most important part of auscultation is what goes on between your ears! Uses and Sounds • The diaphragm – transmits higher pitched sounds better than lower frequency sounds. • The diaphragm should be pressed firmly against the chest wall. • The bell transmits low pitched sounds – should be placed lightly on the skin – just to make contact. • Both bell and diaphragm are used for heart sounds. • The diaphragm is sufficient for lung sounds since most of what you hear in the chest is a higher pitch. Equipment • • • • • • • • Penlight Reflex hammer Tuning fork Tape measure Transparent ruler Blood pressure set Otoscope/opthalmoscope set Something to carry it all in Skin, Hair and Nails • Two essential techniques: –Inspection –Palpation Inspection • • • • Good lighting is essential! Skin color and tint (uniform, pigmented Lesions (location, extent, characteristics) Don’t forget fingernails, toenails, arm pits, back of the neck. • Inspect hair for color, amount, texture Palpation • • • • • • Skin temperature Moisture Texture Pay attention to symmetry Note skin turger (normal loss in elders) Edema Normal Findings • • • • • • • Uniform skin color Intact, without inflammation Smooth, soft and dry Reactive hyperemia Free of lesions Without edema No obvious extremes Transcultural Considerations • The darker the skin – the greater the melanin and the less risk for skin cancer. • Interesting note: Eskimos sweat less on their trunks and extremities and more on their face as compared to say people who are not eskimos. Why? It’s an environmental adaptation that allows temperature regulation without causing perspiration and dampness in their clothes, which would decrease their ability to insulate themselves from the cold weather! Remember • Sexual skin areas are typically darker, especially among dark skinned and asian races…….this includes the nipples, areola, scrotum and labia. • Observe for signs of possible abuse: a concern would be multiple bruises at different stages of healing. Hints: Possible Concerns • • • • • • • • Cold – arterial insufficiency Warm – hyperthyroidism Increased moisture – anxiety, hyperthyroidism Dry skin – hypothyroid Poor turger – dehydration, scleroderma Hair loss or excess – endocrine problems Clubbing nails – emphysema, heart disease Pits, lines in nails – possible nutritional problems Primary Skin Lesions • • • • • • • • • • • Macules Papules Patch Plaque Nodule Wheal Tumor Vesicle Pustule Bulla Cyst Secondary Skin Lesions • • • • • • • • • Crust Scale Fissure Erosion Ulcer Excoriation Scar Lichenification Keloid Reminder • The focus in Basic Health Assessment is on NORMALS……….don’t get too distracted or spend too much time with abnormal findings…….that’s what we’ll do in Practicum I and Clinical Decision Making! Head and Neck Exam • Primarily use Inspection and Palpation in a routine exam – although some people will routinely auscultate for bruits along the carotid arteries. • Always expect a little asymmetry in faces • The skull, however, should be symmetric and smooth • The trachea should be midline – not deviated to the left or right. • Ask person to take a drink of water and inspect for any deviations from normal with swallowing. • Thyroid tissue will move up with swallowing. Palpating the Thyroid Gland • A normal thyroid gland is neither visible or palpable! • How to find it: It lies in the anterior lower neck on both sides of the trachea, with the isthmus overlying the trachea. The 2 lateral lobes are butterfly shaped and joined by the isthmus at the lower part. Most of the lobes are covered by the sternocleidomastoid muscles. Technique for Palpating the Thyroid • Can be done from the front of the person or from behind them – your preference. • Try this simple procedure: Press gently on one side of the gland, displacing the larynx and trachea laterally. The opposite side is then palpated lightly. Ask the person to swallow. This motion will move the gland past your finger tips and help you to identify nodules – if any! Lymph Nodes – Know Your Anatomy! • Preauricular – in front of the ear • Postauricular – superficial to the mastoid process • Occipital – at the base of the skull • Submental – midline, behind the tip of the mandible • Submaxillary – Halfway between the angle and the tip of the mandible. • Tonsilar – at the angle of the mandible • Superficial cervical – overlying the sternomastoid muscle • Posterior cervical – in the posterior triangle along the edge of the trapezius muscle • Supraclavicular – just above and behind the clavicle Nose, Sinuses, Mouth, Throat • Primarily inspection and palpation • Again – know your anatomy: – Temporal sinuses – Maxillary sinuses – Temporomandibular joint – Buccal mucosa Normal Findings • Nose: midline, intact, no discharge, no redness, no tenderness • Sinuses: no tenderness or inflammation • Lips: pink, moist, symmetrical, no lesions • Oral Mucosa: pink, smooth, no lesions or odors NOTE: In dark skinned persons, it’s normal to have some patchy pigmentation or bluish coloration to the mucosa. More Normals • Gingivae: pink, withour bleeding or lesions • Teeth: intact and present! • Tongue: smooth, midline, pink, without lesions – don’t forget to look under the tongue (common for cancers to hide there!) • Throat: pink, moist, no exudate or lesions, note presence of tonsils, movement of uvula and gag reflex Lymph Nodes • • • • • • • Note: Location Size Shape Mobility Consistency Tenderness Normal Lymph Glands • • • • • Moveable Discrete Soft Non tender Less than 1 cm Ear and Auditory Exam • Again, primarily inspection and palpation • Note deformities, trauma, lesions, tenderness. • Always inspect before you touch! • After the history, you should have some indication of whether or not this person can hear Some Easy Tests • Whisper Test: whisper something standing about a foot or two away and ask the person to repeat it – while they are facing away from you. • Weber Test: This test is also not usually done in a general exam, but here is how it works: Place a vibrating tuning fork in the midline of the skull and ask the person to tell you if she hears the sound equally in both ears. If she doesn’t note the ear in which the sound is louder. A Word About Hearing Tests • These exams are crude, screening tests that really don’t tell the examiner more than this: if there is a problem with either the whisper or the weber test, refer this person for a complete hearing evaluation and don’t waste their time or yours by playing with this tuning fork . Using an Otoscope General guidelines: 1. Tilt the persons head away from you. 2. Hold the otoscope between the thumb and fingers of one hand. 3. Hold the auricle between the thumb and finger of the other hand – use other fingers to steady the head. 4. Pull the pinna up and back in order to straighten the canal and get a good view. Normal Findings • External Ear and canal: no inflamation, lesions or drainage. Some grey-brown cerumen may be present. • Tympanic membrane: Intact, pearly grey, no bulging, bleeding, retraction, or lesions • Malleus: dense whitish streak originating from the superior hemisphere of the tympanic membrane Eye Exam • Again, inspection and palpation dominates the exam for this system. • Remember – you are not expected to be an expert in this area! • The role of the primary care provider is to identify deviations from normal and REFER!! Visual Acuity • Use of the Snellen Chart: if the person can read most or all of the letters in line 8 at 20 feet, vision is considered normal. • There are now cards that can also be used to test near vision as well and can come in handy to help people identify whether or not they should be suing reading glasses. Visual Fields The confrontation method: Place yourself in front of the person, about 2 feet away, and about the same height. Ask the person to cover one eye with something opaque and have the other eye look directly at you. Hold a pencil midline between you and the other person, and slowly move it in from the periphery in several directions (up, down, laterally). Ask her to tell you when she sees the pencil – it should be the same time as you see it. If not, she may have some peripheral vision loss. Using the Opthalmoscope Important Points: 1. Usually you do not have the advantage of being able to medically dilate the persons pupils……..so once again, this is a very crude exam! 2. Darken the room – that will help. It will also help if the person has big brown eyes – much more difficult in persons with light eyes. More Guidlines • If you have a dog who doesn’t mind, they are usually good specimens - easy to see! • DO not wear your eyeglasses when using this instrument. There is a built in diopter setting that can compensate for you. • There are lots of interesting settings on this instrument – most of which you will never use. Mostly you will use the large round aperture with the white light for routine exams. • Ask the person to stare at a distant object – this will help to dilate the pupil and keep the retina still. Even More! • ALWAYS match sides with the person: Use your right eye to look into their right eye and hold the opthalmoscope in your right hand. Place your free hand on the persons forehead. This helps to stabilize you in space – since it can get a little disorientating and you don’t want to bump heads . In Search of the Optic Disc! • Once you are in position, and still about a foot away, use your instrument to first find the red reflex. You should be able to see this before you get too close to the person. • Then gradually move in, following that red reflex and until you start to see vessals. • Once you see vessels, follow one of them – it will lead you to the optic disc! Normals • Arteries are a brighter red than veins. • Arteries have a thin strip of light down the middle – the arterial light reflex. • The ratio of artery to vein width (A:V ratio) is 2:3 • Sometimes an artery and a vein will cross but they should not be nicked and should not be more than 2 disc diameters (DD) away. • It’s normal to see pulsations in veins as you get near to the disc. More Normals! • The optic disc is a creamy colored round or oval structure with distinct margins. Once you see it – you will know! • The macula is off temporal to the disc. This can cause some discomfort for the person if you stay there too long – it’s very sensitive, so you want to do it last, take a look and move on. Tends to be a little darker than the rest of the fundus. Examining the Thorax and Lungs Here is where you will use all of the techniques for the physical exam: Inspection Palpation Percussion Auscultation Normal Breath Sounds • Vesicular Sounds: soft, low pitched, heard over most of the chest • Bronchial Sounds: loud, high pitched, heard only over the trachea and major bronchi. • Broncho-vesicular Sounds: a combination of the above, can be heard over portions of the chest where a bronchus is near lung parenchyma (the upper anterior chest). Testing for Tactile Fremitus