Just The Two Of Us - PBL-J-2015
Just The Two Of Us
Physiology and Biochemistry Of The Menstrual Cycle
1. Define the term amenorrhoea and identify causes
Amenorrhea: Absence / abnormal stoppage of menstruation. Causes - primary or secondary:
Primary: The absence of menstruation in females who have never menstruated.
Usually caused by developmental abnormalities of ovaries or reproductive tract. Or scar tissue in those structures in response to physical injury or infection before menarche.
Secondary: More common. Cessation of menstruation in females who have previously menstruated. Time since last menstruation should be three times longer than a normal cycle.
Pregnancy.
Can result from malfunctions at the level of the ovary, uterus, pituitary, or hypothalamus. o Ovaries: Chemotherapy, radiation therapy, surgery or infections can cause scar tissue, result in ovarian failure and a reduction in the number of viable follicles. o Uterus: Infection, surgery chemotherapy or radiation therapy. o Pituitary: The presence of a prolactin secreting tumour, which results in hyperprolactinemia and consequent suppression of GnRH. o Hypothalamus: Suppression of GnRH
Physical stress, usually from excessive exercise can suppress GnRH release.
Extreme weight loss, including anorexia nervosa.
Extreme weight gain ↑ in adipose tissue leads to an increase conversion of adrenal androgens to oestrogen, thus disrupting the normal feedback cycle to the hypothalamus.
Psychological stress.
Following the cessation of the pill. May be caused by a hypothalamic disturbance in response to the steroid contents of the pill.
2. Describe the cellular events that make up the menstrual cycle.
Two phases: The follicular phase before ovulation, and the luteal phase after ovulation.
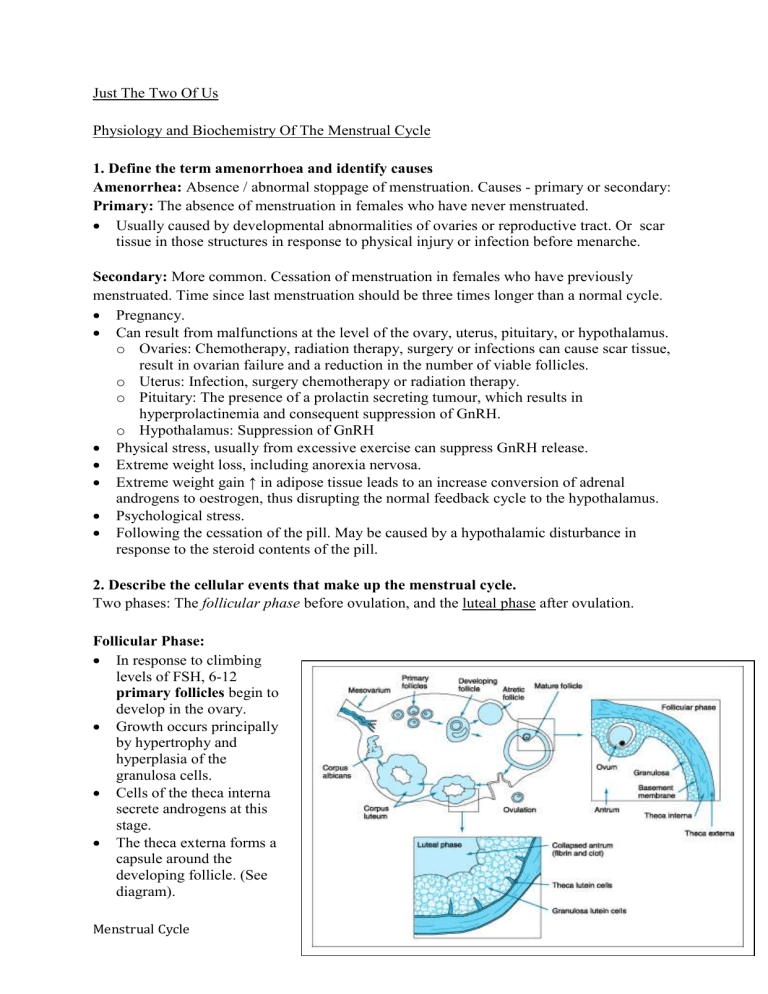
Follicular Phase:
In response to climbing levels of FSH, 6-12 primary follicles begin to develop in the ovary.
Growth occurs principally by hypertrophy and hyperplasia of the granulosa cells.
Cells of the theca interna secrete androgens at this stage.
The theca externa forms a capsule around the developing follicle. (See diagram).
Menstrual Cycle Page 1
Also stimulated by FSH, granulosa cells produce oestrogens from the thecal androgens.
They secrete a follicular fluid which contains oestrogens and this leads to formation of the antrum (fluid filled space in the middle of the follicle).
At this stage, the follicle is known as the vesicular follicle (or Graafian Follicle).
The oocyte is now ready for ovulation.
In the late follicular phase, explosive growth occurs due to a number of synergistic feedback mechanisms: o Oestrogen in the follicle induces increased production of FSH receptors, making the granulosa cells more responsive to the stimulating effects of FSH and causing them to produce more oestrogen! o Oestrogen and FSH act synergistically to induce production of LH receptors. LH and
FHS cause a rapid final growth in the few days before ovulation. o Maintained high levels of oestrogen produced by the vesicular follicle induce positive feedback on LH production. This is the LH surge which in turn induces ovulation.
The dominant follicle induces atresia of the other follicles, possibly by negative feedback of oestrogen on GnRH which cuts off their FSH support.
Luteal Phase:
Once the follicle ruptures (day 14), the remaining granulosa cells and theca interna are stimulated by LH change into lutein cells and proliferate into the corpus luteum .
The corpus luteum is a highly secretory body which produces progesterone , oestrogen and inhibin .
Even though oestrogen levels are very high following ovulation, progesterone secreted by the corpus luteum ensures that its stimulatory effect on LH production is inhibited, preventing further surges of LH.
Inhibin also has an inhibitory effect on GnRH, decreasing production of FSH.
The combined effects of these hormones cause FSH and LH levels to return to baseline.
Once this occurs, the corpus luteum no longer has hormonal support and on around day
26 of the cycle it involutes and becomes the scar like tissue of the corpus albicans .
In pregnancy, an LH analogue called chorionic gonadotropin maintains the corpus luteum until the trophoblast assumes the role of progesterone secretion.
Around day 28, progesterone levels drop off and FSH and LH are once more uninhibited.
Menstrual Cycle Page 2
As they begin to rise, a new batch of primary follicles are stimulated - cycle begins again.
3. Correlate the sequence of hormonal changes with the cellular events of the menstrual cycle
The activity of the female reproductive tract is under hormonal regulation that involves endocrine stimulation of the gonads (ovaries) and feedback to the pituitary. (The hypothalamic-pituitary-gonad axis.)
The cycle averages 28 days per cycle but varies from 20 to 45 days. In each menstrual cycle only one ovum is normally released.
The uterine endometrium is prepared for implantation at the required time each month.
Circulating hormones must coordinate the ovarian and uterine cycles to ensure proper reproductive function.
GnRH released from the hypothalamus regulates the female reproductive cycle. o The release of GnRH in females is in a pulsatile fashion. o Difference in pulse intensity is interpreted by the cells of the pituitary, which respond differently according to the strength of the signal. o For example, differing pulse intensity may cause preferential release of either FSH or
LH .
The ovarian cycle may be divided into two phases while the uterine cycle has three phases. o The 2 stages of the ovarian cycle
1) Follicular phase
2) Luteal phase. o The 3 stages of the uterine cycle
1) Menses phase
2) Proliferative phase
3) Secretory phase.
Ovarian Cycle
Follicular Phase
Follicular development begins under FSH stimulation.
During the first few days after the beginning of menstruation the concentrations of FSH and LH increase slightly.
The FSH stimulates some primordial follicles (present at birth and are composed of an ovum, suspended in prophase of meiosis, surrounded by a single layer of granulosa cells ) to begin to develop into primary follicles.
The elevated FSH levels cause accelerated growth of 6 to 12 primary follicles each month.
The initial effect is rapid proliferation of the granulosa cells and the production of thecal cells in the ovarian interstitium outside the granulosa cells .
As the follicles begin to enlarge thecal cells start producing androstenedione (a steroid hormone that is a precursor of most sex hormones).
Granulosa cells surrounding the ovum absorb the androstenedione and convert it to oestrogen .
There are several layers of granulosa cells surrounding the ovum in a primary follicle.
Menstrual Cycle Page 3
The many granulosa cells secrete an oestrogen rich follicular fluid that accumulates to form the antrum that appears between the masses of granulosa cells .
Once the antrum is formed the granulosa and thecal cells proliferate more rapidly, the rate of secretion accelerates and each developing follicle quickly becomes an antral follicle .
The early growth of the primary follicle, up to the antral stage, is stimulated solely by
FSH as LH secretion is inhibited by low levels of circulating oestrogen secreted by the developing follicles and the pulse frequency of GnRH favours release of FSH .
After the antral follicle stage accelerated growth leads to much larger follicles called vesicular follicles due to oestrogen from the granulosa cells increasing numbers of FSH receptors making the granulosa cells more sensitive to FSH .
However FSH levels begin decline due to feedback inhibition by inhibin .
The combined FSH and oestrogen act to promote LH receptors on the granulosa cells also allowing LH stimulation of the granulosa cells in addition to FSH .
Finally, the combined effects of LH and oestrogen act to proliferate the thecal cells and increase their secretion of steroid hormones and proteolytic enzymes to digest the follicular wall.
During this time the ovum also increases greatly in diameter.
As the follicle grows the ovum itself remains embedded in a mass of granulosa cells located at one pole of the follicle.
After one week or more of growth, but before ovulation, one follicle begins to outgrow the others.
The follicles that recede are called atretic follicles .
Ovulation generally occurs 14 days after the start of menstruation.
As oestrogen levels rise the hypothalamus is stimulated to increase the pulse frequency of
GnRH , which in turn favours the release of LH from the anterior pituitary.
In addition at about day 10 oestrogen levels reach a threshold and switch from inhibitory to stimulatory to LH secretion.
At about day 14 oestrogen levels have peaked resulting in a massive release of LH from the pituitary, while FSH levels also rise.
This massive surge of LH triggers the completion of meiosis I by the primary oocyte , rupture of the follicle wall and ovulation.
Luteal Phase
The spike in LH levels triggers the formation of the corpus luteum as well as converting the granulosa and theca cells to secrete progesterone .
The rise in progesterone and fall in oestrogen cause the pulse frequency of GnRH to drop markedly favouring LH secretion, which maintains the structure and function of the corpus luteum .
The progesterone secreted by the corpus luteum promotes enhancement of the endometrial blood supply and secretion of endometrial glands.
Progesterone levels remain high for about 7 days and unless pregnancy occurs the corpus luteum begins to degenerate.
Roughly 12 days after ovulation the corpus luteum becomes non-functional and oestrogen and progesterone levels decline markedly.
The blood supply to the functional zone of the endometrium is restricted and the endometrial tissue degenerates.
Menstrual Cycle Page 4
The fall in oestrogen and progesterone also allow an increase in pulse frequency of release of GnRH and the cycle begins again.
Uterine Cycle
The endometrium can be divided into two zones.
1) The functional zone , which is the surface layer and contains most of the endometrial glands and contributes most of the thickness of the endometrium.
2) The basilar zone is the outer layer connecting the endometrium to the myometrium.
The structure of the basilar zone remains relatively constant while the functional zone undergoes cyclical changes under the influence of hormones.
There are three phases.
1) The menstrual phase: Corresponds to the follicular phase of the ovarian cycle.
2) The proliferative phase: Corresponds to the follicular phase of the ovarian cycle.
3) The secretory phase: Corresponds to the luteal phase of the ovarian cycle.
Menstrual Phase
The uterine cycle begins with the onset of menses .
It is caused by constriction of the spiral arteries, which reduces blood flow to the endometrium.
As a result of nutrient and oxygen deprivation the glands and other functional tissue of the functional zone deteriorate and eventually arterial walls weaken and rupture and blood and degenerating tissues break away and enter the uterine lumen to be passed out the vagina.
Repair begins immediately.
The basilar zone is unaffected, as the straight arteries supplying it remain unconstricted.
Proliferative Phase
The basilar zone survives the menses intact including its uterine glands.
In the days post menses the epithelial glands multiply and spread across the endometrium resulting in the complete restoration of the functional zone.
This restoration occurs at the same time as the enlargement of primary and secondary follicles.
So the proliferative phase is stimulated and sustained by oestrogens secreted by the developing ovarian follicles.
At the time of ovulation the functional zone is several millimetres thick with prominent mucous glands that release secretions rich in glycogen for use by the blastocyst as fuel.
Secretory Phase
During the secretory phase the uterine glands enlarge and accelerate their rate of secretion.
Arteries also elongate and spiral through the tissues of the functional zone.
This activity is stimulated and maintained under the influence of predominantly progesterone but also oestrogen form the corpus luteum .
Secretory activity peaks about 12 days after ovulation.
Menstrual Cycle Page 5
Over the next two days the glandular activity declines and the uterine cycle comes to a close as the corpus luteum degenerates and secretion of progesterone stops.
The cycle starts again as the menses begin again.
4. Identify the hormones released by the ovary, pituitary and hypothalamus respectively and describe their roles in the menstrual cycle and in maintenance of pregnancy
There are three different hierarchies of hormones involved in the female reproductive system.
1.
Hypothalamic Releasing Hormone: GnRH (Gonadotrophin Releasing Hormone)
2.
Anterior Pituitary Hormones
Follicle Stimulating Hormone (FSH)
Luteinising Hormone (LH)
3.
Ovarian Hormones
Oestrogen
Progesterone
The Hypothalamus and GnRH
Secretion of most of the anterior pituitary hormones is controlled by releasing hormones that are formed in the hypothalamus and transported to the anterior pituitary gland by the hypothalamic-hypophysial portal system .
Through this system, essentially all of the blood that enters the anterior pituitary has previously transversed the lower hypothalamus, carrying with it any hypothalamic hormones.
The anterior pituitary is a highly vascularised gland with many capillary sinuses along the glandular cells.
Specialised neurons in the hypothalamus synthesise and secrete hormones.
Menstrual Cycle Page 6
They terminate in the median eminence and secrete their hormones into the tissue fluids.
These hormones are then immediately absorbed into the hypothalamic-hypophysial portal capillaries and carried directly to the sinuses of the anterior pituitary.
The hypothalamus secretion of GnRH is done by the arcurate nuclei of the mediobasal hypothalamus and the preoptic areas of the hypothalamus.
GnRH isn’t secreted continuously, but in pulses lasting several minutes every one to three hours.
GnRH acts on the anterior pituitary to stimulate secretion of FSH and LH.
When GnRH is infused constantly, the effects on release of FSH and LH are lost, therefore, the pulsative release is essential.
Anterior Pituitary Hormones, Oestrogen and Progesterone
FSH and LH act on the ovarian follicle and influence its development. However, they are not independent of the ovarian hormones!
Oestrogen, FSH & LH (Follicular Phase)
FSH is essential for maturation of the Graafian follicle before ovulation.
As the follicle matures and produces increasing amounts of oestrogen, FSH is inhibited and this can be seen by a decline in FSH towards the end of the follicular phase.
When the high levels of oestrogen in the follicular phase reach a peak, this acts positively on the anterior pituitary (and hypothalamus), resulting in a peak of LH (& FSH to a lesser extent), thus stimulating ovulation.
Oestrogen exerts positive feedback on the hypothalamus and anterior pituitary during the follicular phase in order for ovulation to occur.
However, in the luteal phase, oestrogen is inhibitory on the FSH-secreting cells of the anterior pituitary and hypothalamus.
Inhibin
Anther hormone produced by the gonads and inhibits FSH secretion by action on the anterior pituitary.
FSH
Progesterone, LH &
(Luteal Phase)
High plasma concentration of progesterone inhibits hypothalamic output of
GnRH and inhibits the anterior pituitary, resulting in ↓ FSH and
↓LH secretion.
Menstrual Cycle Page 7
Pregnancy
Orientation: ovulation has occurred, fertilization successful and we are now investigating proceedings in the luteal phase of the ovarian cycle and beyond…..
Progesterone
The corpus luteum is the main source of progesterone during the luteal phase.
LH is responsible for regulating the normal function of the corpus luteum. (If there was no fertilization, the corpus luteum undergoes luteolysis , perhaps due to dwindling levels of LH secretion towards the end of the luteal phase).
Progesterone is essential for pregnancy.
If progesterone is not maintained, menstruation occurs and the conceptus (embryo) is lost.
In order for the corpus luteum to “know” that there is an embryo around, human
Chorionic Gonadotrophin (hCG) is secreted by the trophoblast cells of the blastocyst within 9 days following fertilization (just enough time before the corpus luteum would degenerate!).
hCG is a glycoprotein, is similar to LH, and thus is able to stimulate the continued development of the corpus luteum.
The corpus luteum is the only source of progesterone during early pregnancy. The placenta begins to secrete progesterone after the 6 th
Progesterone is essential for pregnancy because:
week of pregnancy.
1.
Induces growth of endometrium and secretion of nutrients for developing embryo
2.
Inhibits contractions of uterus to prevent premature expulsion of the foetus
3.
Progesterone & oxytocin stimulate the breast in preparation for milk production and release
4.
Is a foetal tranquilliser – high doses of progesterones act as anaesthetics by inhibiting membrane excitability
Oestrogens
Oestrogen levels in maternal plasma rise progressively throughout the pregnancy. In the first month, oestrogen is secreted by the corpus luteum in response to hCG.
However, after the first month, the placenta takes over oestrogen secretion.
The human placenta does not contain all the enzymes required for oestrogen synthesis and relies on interaction between the adrenal gland of the foetus and placenta for the process to occur.
The foetal adrenal cortex contains enzymes that are capable of forming androgens from cholesterol (DHEA-sulfate).
The DHEA-sulpfate produced by the foetus is transported to the placenta and are converted into oestriol by the placental enzymes.
Oestradiol = oestrogen of menstrual cycle
Oestriol = oestrogen of pregnancy from the placenta
Oestrone = oestrogen of menopause
5. Describe how the menstrual cycle is regulated with particular reference to the role of the follicles.
The follicles enlarge and the antrum forms in response to FSH.
The early stages of pre antral growth do not require gonadotrophic stimulation.
The connective tissue around the ovarian stroma surrounding the follicles differentiates into two thecal layers , interna and externa.
Menstrual Cycle Page 8
When one of the follicles becomes dominant a layer of follicle cells lining the antral cavity under the basement forms, this is the granulosa layer . When this is developed the follicle is called a mature graafian follicle.
Both FSH and oestrogen stimulate proliferation of the granulosa cells .
LH and FSH are required for synthesis and secretion of oestrogen by the follicle .
The thecal cells produce androgens but are unable to convert them into oestrogens.
The granulosa cells are unable to produce androgens but are capable of converting the androgens into oestrogen.
LH acts on thecal cells to stimulate androgen production while FSH acts on granulosa cells to promote the conversion into oestrogens.
Some of the oestrogen produced enters the circulation and acts on the uterus to instigate the proliferative phase and inhibits the hypothalamus and anterior pituitary in negative feedback to reduce FSH release.
This is seen as declining levels in FSH and increasing LH in the follicular phase.
The LH surge of ovulation is triggered by a positive feedback effect of oestrogen
(produced by the combined efforts of thecal and granulosa cells). As it acts directly on the hypothalamus as well as the anterior pituitary, there is also a surge in FSH at ovulation.
However, there is no known role for this FSH surge.
6. Briefly describe the effects of stress and neural influences on the menstrual cycle
The hypothalamus can override or reinforce ovarian signals and therefore, can respond to conditions such as stress by inhibiting GnRH release and therefore hinder the cycle.
The hypothalamus receives neural input from almost all tissues in the body, therefore is highly sensitive to changes.
Known examples of where hypothalamic control is altered: o Calorie deprived women with loss of adipose tissue and have a lean body mass o Excessive exercise o Physical translocation o Chronic inflammatory disease
These inhibitory influences may be mediated by hypothalamic endorphins, corticotropin releasing hormone or even leptin.
It has been observed that women who live close to one another can adopt a common timing of their menstrual cycles. This is possibly due to pheromones emitted by one individual that affects a nearby individual.
Menstrual Cycle Page 9
Menstrual Cycle Page 10