22-L-HAI-SPICE-Part 1-BSI-April 2014
advertisement

NOSOCOMIAL BLOODSTREAM
INFECTIONS AND SEPSIS: SPICE, 2014
David Jay Weber, M.D., M.P.H.
Professor of Medicine, Pediatrics, & Epidemiology
Associate Chief Medical Officer
University Of North Carolina at Chapel Hill
TOPICS
Epidemiology
Pathogenesis
Impact of healthcare-associated infections
Definitions
NHSN surveillance definitions
Incidence and prevalence of CLA-BSI
Mechanisms of CLA-BSI
Microbiology
Risk factors
Diagnosis
Sepsis
Prevention
LECTURE GOALS
Understand the impact of bloodstream infections
Understand the incidence and causative pathogens of
bloodstream infection
Understand the risk factors for healthcare-associated
bloodstream infections
Understand the prevention and control of bloodstream
infections
Understand the pathophysiology and risk factors for
sepsis and septic shock
IMPACT OF BLOODSTREAM INFECTIONS
Approximately 250,000 nosocomial BSIs per year
Accounts for ~14% of healthcare-associated infections
Increases length of stay by 7-21 days
Attributable cost = $3,700 - $39,000 per episode
Major risk = use of an intravascular device
Rate of BSIs varies by:
Hospital size, unit, and service
Population served (elderly/infants, acute/chronic)
Use and type of intravascular access device
Time-trends
Endemic/Epidemic
Weber DJ, Rutala WA. Infect Dis Clin NA 2011;25:77-102
Magill SS, et al. New Engl J Med 2014;370:1198
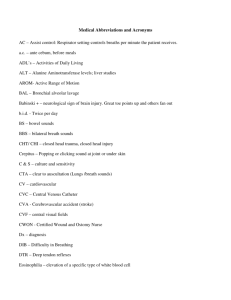
MORTALITY OF NOSOCOMIAL BSI,
SCOPE, 1995-98
CoNS
S. aureus
Enterococcus sp.
Candida sp.
E. coli
BSI Pathogens
Crude mortality
Klebsiella sp.
Enterobacter sp.
Pseudomonas sp.
Edmond M, et al. CID
1999;29:239
Serratia sp.
Viridans streptococci
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
IMPACT OF CLA-BSIs
Prevalence
ICUs: ~80,000 CLA-BSIs/year1
Hospital-wide: ~248,000 CLA-BSI/year1
Cost/year
$7,288 to $29,156 per infection (total ~670 million to $2.7 billion)3
1Mermel
L, et al. CID 2009;49:1 – 2http://www.cdc.gov/ncidod/dhqp/pdf/Scott_CostPaper.pdf
- Eggimann P, Pitter D. CLin Microbiol Infect 2002;8:295
DEFINITIONS
Primary bacteremia: Culture-documented bacteremia occurring in the
absence of recognized infection with the same pathogen at another site
Secondary bacteremia: Culture-documented bacteremia originating from an
identifiable infection at a specific site
Pseudo-bacteremia: Positive blood cultures resulting from contamination
during the collection procedure or during laboratory processing
Septicemia: A systemic disease caused by the presence of microorganisms
or their toxins circulating in the blood
Sepsis: A clinical picture that is consistent with the presence of
microorganisms or their toxic by-products in circulating blood
Septic shock: A syndrome of circulating insufficiency with hypoperfusion of
body tissues resulting from an inadequate cardiac output relative to
metabolic demands
Mermel L, et al. CID 2009;49:1-45
CENTRAL LINE-ASSOCIATED BLOODSTREAM
INFECTION (CLA-BSI) EVENT
HAI
All NHSN site specific infections must first meet the NHSN definition
before a site specific infection (e.g., CLA-BSI) can be reported to NHSN
{An infection is considered an HAI if all elements of a CDC/NHSN sitespecific infection criterion were not present during admission time
period but were all present on or after the 3rd calendar day of admission
to the facility. All elements of the site specific definition mujst occur
within a time frame that does not exceed a gap of 1 calendar day
between any two adjacent elements}
Primary bloodstream infection (BSI)
Primary BSI are laboratory-confirmed bloodstream (LCBI) that are NOT
secondary to an infection at another body site
NHSN DEFINITIONS: CLA-BSI
Central line
The following are NOT considered central lines:
Catheter must terminate in aorta, pulmonary artery, superior or inferior
vena cava, brachiocephalic veins, internal jugular veins, subclavian
veins, external iliac or common iliac veins, femoral veins, umbilical
artery/vein (neonates)
Excludes femoral arterial catheters, intraaortic balloon pump, ECMO
Extracorporeal membrane oxygenation (ECMO)
Femoral arterial catheters
Intra-aortic balloon pump (IABP) devices
Hemodialysis reliable outflow (HeRO) dialysis catheters
Infusion: Introduction of a solution through a blood vessel via a
catheter lumen
NHSN DEFINITIONS: CLA-BSI
Temporary central line: A non-tunneled, non-implanted catheter
Permanent central line:
Tunneled catheters, including certain dialysis catheters
Implanted catheters (including ports)
CENTRAL LINE-ASSOCIATED BLOODSTREAM
INFECTION (CLA-BSI) EVENT
A laboratory-confirmed bloodstream infection (LCBI) where central line (CL)
or umbilical catheter (UC) was in place for >2 calendar days when all
elements of the LCBI were first present, with day of device placement being
Day 1 AND
A CL or UC was in place on the day of the event or the day before.
If a patient is admitted or transferred into a facility with a central line
in place, day of first access is considered Day 1
http://www.cdc.gov/nhsn/acute-care-hospital/clabsi/index.html
LABORATORY CONFIRMED BLOODSTREAM
INFECTION (LCBI)
LCBI 1: Patient has a recognized pathogen cultured from one or
more blood cultures AND organism cultured from blood is not
related to an infection at another site
LCBI 2: Patient has at least one of the following signs or
symptoms: fever (>38oC), chills or hypotension AND positive
laboratory results are not related to an infection at another site AND
common commensal (see list) is cultured from 2 or more blood
cultures drawn on separate occasions. Criterion elements must
occur within a time frame that does not exceed a gap of 1 calendar
day.
LABORATORY CONFIRMED BLOODSTREAM
INFECTION (LCBI)
LCBI 3: Patient <1 year of age has at least one of the following
signs or symptoms: fever (>38oC core), hypothermia (<36oC core),
apnea, or bradycardia AND positive laboratory results are not
related to an infection at another site AND common commensal
(see list) is cultured from 2 or more blood cultures drawn on
separate occasions. Criterion elements must occur within a time
frame that does not exceed a gap of 1 calendar day.
MUCOSAL BARRIER INJURY LABORATORYCONFIRMED BLOODSTREAM INFECITON (MBI-LCBI)
MBI-LCBI 1: Patient of any age meets criterion 1 for LCBI with at least one
blood culture growing one of the intestinal organisms (see list) with no
other organism isolated AND patient meets at least one of the following:
Is an allogeneic hematopoietic stem cell transplant recipient within the
past year with one of the following documented during the same
hospitalization as positive blood culture
Grade III or IV gastrointestinal graft versus host disease (GI GVHD)
>1 liter diarrhea in a 24-hour period (or >20 mL/kg in a 24 hour period for
patients <18 years of age) with onset on or within 7 calendar days before
the date the first positive blood culture was collected
Is neutropenic, defined as at least 2 separate days with values of
absolute neutrophil count (ANC) or total white blood cell count (WBC
<500 cells/mm3 on or within 3 calendar days before the positive blood
culture was collected
MUCOSAL BARRIER INJURY LABORATORYCONFIRMED BLOODSTREAM INFECITON (MBI-LCBI)
MBI-LCBI 2: Patient of any age meets criterion 2 for LCBI when the blood
cultures are growing only viridans group streptococci with no other
organisms isolated AND patient meets at least one of the following:
Is an allogeneic hematopoietic stem cell transplant recipient within the
past year with one of the following documented during the same
hospitalization as positive blood culture
Grade III or IV gastrointestinal graft versus host disease (GI GVHD)
>1 liter diarrhea in a 24-hour period (or >20 mL/kg in a 24 hour period for
patients <18 years of age) with onset on or within 7 calendar days before
the date the first positive blood culture was collected
Is neutropenic, defined as at least 2 separate days with values of
absolute neutrophil count (ANC) or total white blood cell count (WBC
<500 cells/mm3 on or within 3 calendar days before the positive blood
culture was collected
MUCOSAL BARRIER INJURY LABORATORYCONFIRMED BLOODSTREAM INFECITON (MBI-LCBI)
MBI-LCBI 3: Patient <1year of age meets criterion 3 for LCBI when the
blood cultures are growing only viridans group streptococci with no other
organisms isolated AND patient meets at least one of the following:
Is an allogeneic hematopoietic stem cell transplant recipient within the
past year with one of the following documented during the same
hospitalization as positive blood culture
Grade III or IV gastrointestinal graft versus host disease (GI GVHD)
>1 mL/kg diarrhea in a 24-hour period in a 24 hour period with onset on or
within 7 calendar days before the date the first blood culture is collected
Is neutropenic, defined as at least 2 separate days with values of
absolute neutrophil count (ANC) or total white blood cell count (WBC
<500 cells/mm3 on or within 3 calendar days before the positive blood
culture was collected
COMMENSAL ORGANISMS (i.e., skin flora)
Corynebacterium spp. (not C. diphtheriae)
Bacillus spp. (not B. anthracis)
Propionibacterium spp.
Coagulase-negative stahylococci (including S. epidermidis)
Aerococcus spp.
Micrococcus spp.
For full list see: http://www.cdc.gov/nhsn/XLS/master-organismCom-Commensals-Lists.xls
INTESTINAL ORGANISMS
Bacteroides spp.
Candida spp.
Clostridium spp.
Enterococcus spp.
Fusobacterium spp.
Peptostreptococcus spp.
Prevotella spp.
Veillonella spp.
Enterobacteriaceae*
Enterobacteriaceae*
* Partial list
Citrobacter
Enterobacter
Escherichia (e.g., E. coli)
Klebsiella
Providencia
Salmonella
Serratia
Shigella
Yersinia
http://www.cdc.gov/nhsn/TOC_PSCManual.html, 2012
http://www.sciencedirect.com/science/article/pii/S019665531301153X#
BLOODSTREAM INFECTION RATES IN ICUs,
STEP DOWN UNITS (SDUs), and WARDS
# Admissions
# Patientdays
BSI:
# Cases
BSI: Cases
per 100
admissions
BSI: Cases
per 1,000
device days
Medical ICU
2,196
10,643
78
3.55
7.33
Medical SDU
2,505
7,750
30
1.20
3.87
Medical Ward
16,656
72,781
150
0.90
2.06
Surgical ICU
1,063
5,531
52
4.89
9.40
Surgical SDU
3,117
6,587
12
0.38
1.82
Surgical Ward
14,829
73,999
85
0.57
1.15
Weber DJ, et al. ICHE 2007;28:1361-1366
CLA-BSI MRSA RATES, US ICUs, 1997-2007
Burton DC, et al. JAMA 2009;301:727
CHANGES IN INCIDENCE OF CLA-BSI
OVER TIME, UNC HOSPITALS
Weber DJ, et al. ICHE 2010;31:875
DiBiase LM, et al. ICHE 2014;35:200
PATHOGENESIS CLA-BSI
Multifactorial and complex
Most catheter-related infections appear to result form migration of
skin organisms at insertion site into the cutaneous tract with
eventual colonization of the catheter tip
Catheter hub also important contributor to intralumenal colonization
(especially in long-term catheters)
Less important = hematogenous seeding of catheter tip from distant
focus of infection or contaminated infusate
BIOFILM
SOURCE OF CLA-BSI WITH NONCUFFED
SHORT-TERM VENOUS CATHETERS
Safdar N, Maki D. Intensive Care Med 2004;30:62
SOURCE OF CLA-BSI WITH SHORT-TERM
VENOUS CATHETERS FOR TPN
Segura M, et al. Clin Nutrition 1993;12:102
TOP 10 PATHOGENS ASSOCIATED WITH
CLA-BSIs: NHSN, 2009-2010
CoNS
S. aureus
E. faecalis
Other Candida
K. pneumoniae/oxytoca
E. faecium
C. albicans
Enterbacter spp.
Sievert DM, et al. ICHE 2013;34:1-14
E. coli
P. aeruginosa
0%
5%
10%
15%
20%
25%
COMPLICATIONS OF CLA-BSIs
Local infection
Sepsis
Remote site infection
Tunnel infection, pocket infection
Osteomyelitis
Meningitis
Endovascular infection
Endocarditis
Mycotic aneurysms (septic thrombophlebitis)
INDEPENDENT RISK FACTORS
FOR CLA-BSIs
Prolonged hospitalization before catheterization
Prolonged duration of catheterization
Heavy microbial colonization at the insertion site
Heavy microbial colonization of the catheter hub
Internal jugular catheterization
Femoral catheterization
Neutropenia
Prematurity
Reduced nurse-to-patient ratio in the ICU
Total parenteral nutrition
Substandard catheter care e.g., excessive manipulation)
Transfusion of blood products (in children)
Marschall J, et al. ICHE 2009;29(suppl 1):S22
FACTORS ASSOCIATED WITH REDUCED
RISK OF CLA-BSI
Female gender
Antibiotic administration
Minocycline-rifampin impregnated catheters
EVALUATION OF FEVER IN CRITICALLY ILL
ADULT PATIENTS
Definition of temperature
>38.3 oC → trigger for clinical assessment (not necessarily a lab
or radiographic evaluation for infection)
<36.0 oC → in absence of known cause of hypothermia
Most accurate: Pulmonary artery thermistor, urinary bladder
catheter thermistor, esophageal probe, rectal probe
Other acceptable methods: Oral probe, infrared ear thermometry
Less desirable: Temporal artery thermometer, axillary
thermometer, chemical dot
O’Grady NP, et al. Clin Infect Dis 2008;36:1330-1349
EVALUATION OF FEVER IN CRITICALLY ILL
ADULT PATIENTS
Blood cultures
Obtain 3-4 blood cultures within first 24 hours (obtain before
antibiotics if at all possible)
For patients without a CVC, obtain at least 2 blood cultures from
peripheral sites by separate venipunctures
For patients with a CVC, 1 blood culture should be drawn by
venipuncture and at least 1 should be drawn through the CVC
Draw 20-30 mL of blood per blood culture; disinfect the skin with
2% chlorhexidine/70% isopropyl alcohol (ChloraPrep)
BSI INFECTIONS: SYMPTOMS/SIGNS
Constitutional: Fever, rigors, hypotension, shock
Respiratory: Hyperventilation, respiratory failure
Gastrointestinal: Abdominal pain, vomiting, diarrhea
Neurologic: Confusion, seizures
CLUES TO CVC INFECTIONS
CVC: Exit site infection (erythema, tenderness, purulence) or tunnel
infection (erythema, tenderness, purulence, induration)
High grade bacteremia/fungemia (multiple positive cultures)
Abrupt onset, associated with shock
Symptoms/signs of sepsis (i.e., fever/ hypotension) without obvious
source (no identifiable local infection)
Evidence of septic thrombophlebitis of great vein
Continued bacteremia/fungemia despite appropriate therapy
Symptoms/signs of sepsis plus catheter malfunction
Bacteremia with CoNS, Candida, Bacillus, Corynebacterium
CVC INFECTION: EVALUATION
Examine area around catheter exit for redness, tenderness, pus
Examine tunnel tract (implantable catheter) for redness,
tenderness
Blood cultures x 2-3 (always obtain at least one peripheral
culture)
Consider catheter removal with semiquatitative of catheter tip
(not subcutaneous segment). Catheter colonization defined by:
>15 cfu from a 5-cm catheter tip by roll plate method
>102 cfu from a catheter by quantitative (sonication)
broth culture
CELLULITIS OVERLYING CATHETER
SEPSIS: PERIPHERAL EMBOLI TO SKIN
SEPSIS: EMBOLI TO RETINA
GANGRENE
SEPTIC EMBOLI
CVC INFECTION: DIAGNOSIS
A definitive diagnosis of CLA-BSI requires that the same organism
grow from at least 1 percutaneous blood culture and from a culture of
the catheter tip (A-I), OR
Two sets of blood samples (one from the catheter hub and the other
from a peripheral vein) that, when cultured, meet CLA-BSI criteria for
quantitative blood cultures or differential time to positivity (A-II)
For quantitative blood cultures, a colony count of microbes grown from
blood obtained through the catheter hub that is at least 3x greater than
the colony count from blood obtained from a peripheral vein (A-II)
For deferential time to positivity; growth of microbes from a blood
sample drawn from a catheter hub at least 2 hours before microbial
growth is detected in a blood sample obtained from a peripheral vein
(A-II)
LABORATORY METHODS
FOR DIAGNOSIS CLA-BIS
REMOVAL OF CVC: INDICATIONS
Long-term catheters
Severe sepsis
Suppurative thrombophlebitis
Endocarditis
Bloodstream infection that
continues despite >72 hours of
antimicrobial therapy to which
the microbes are susceptible
Infections due to fungi, S.
aureus, P. aeruginosa, or
mycobacteria
Short term catheters
Infections due to Gram negative
bacill, S. aureus, fungi, and
mycobacteria
Mermel L,
et al.
CID
2009;49:1
CVC INFECTION: EMPIRIC THERAPY
Gram-positive cocci (S. aureus, Coag neg staph)
Vancomycin (alternative: daptomycin); avoid linezolid
Gram-negative bacilli (E. coli, Klebsiella, Enterobacter)
4o cephalosporin, carbapenem, -lactam/ -lactamase combination
+/- aminoglycosie
Neutropenic patients
Cover for MDR GNRs including P. aeruginosa
Femoral catheters
In critically ill patients cover for GNRs and Candida
Suspected Candida
TPN, prolonged uss of broad spectrum antibiotics, hematologic
malignancy, stem cell or solid organ transplant, femoral
catheterization, Candida colonization at multiple sites
Choice of drug = echinocandin (selected patients fluconazole)
ANTIBIOTIC LOCK THERAPY
Antibiotic lock therapy is indicated for patients with CLA-BSI involving long-term
catheters without signs of exit site or tunnel infection for whom catheter salvage
is the goal (B-II)
For CLA-BSI, antibiotic lock should not be used alone; instead, it should be used
in conjunction with systemic antimicrobial therapy, with both regimens
administered for 7-14 days (B-II)
Dwell times for antibiotic lock solutions should generally not exceed 48 h before
reinstallation of lock solution; preferably, reinstallation should take place every 24
h for ambulatory patients with femoral catheters (B-II). For dialysis patients, the
lock solution can be renewed every dialysis session (B-II)
Cather removal is recommended for CLA-BSI due to S. aureus, Candida sp.
For patients with multiple positive catheter drawn blood cultures that grow CoNS
or GNRs and concurrent negative peripheral blood cultures, antibiotic lock
therapy can be given without systemic therapy for 10-14 days (B-III)
There is insufficient data to recommend an ethanol lock for treatment (C-III)
The Sepsis Continuum
SIRS
Sepsis
Severe Sepsis
SIRS due to infection
> 2 of the following:
Sepsis + Organ Failure:
• T >38.5oC or <35oC
• Shock / hypotension
• HR >90
• Acute lung Injury
• RR >20 or PaCO2 <32 mmHg
• WBC >12, 000 or <4, 000
or >10% Bands
• Renal
• Hepatic
• Hematologic
• CNS
• Metabolic acidosis
NONINFECTIOUS MIMICS OF SEPSIS
Acute MI
Acute PE
Acute pancreatitis
Fat emboli syndrome
Acute adrenal insufficiency
Acute GI hemorrhage
Overzealous diuresis
Transfusion reactions
Adverse drug reactions
Procedure-related transient
bacteremia
Amniotic fluid embolism
MANAGEMENT OF SEPSIS
Initial resuscitation with fluid replacement
Use dobutamine to maintain blood pressure
Assure adequate ventilation
Obtain appropriate cultures before antibiotics
Perform imaging studies to confirm source of infection, if possible
Begin IV antibiotics within first hour of recognizing sepsis
Use broad spectrum antibiotics
Attempt to identify and control source of infection
Dellinger RP, et al. Crit Care Med 2008;36:296
OUTCOME DEPENDING AN ADEQUECY OF
EMPIRIC THERAPY
60.0%
40.0%
Adequate therapy
Inadequate therapy
30.0%
20.0%
10.0%
Blood
Lung
Abdomen
BC (+)
Mixed
Gram (-)
Gram (+)
Septic shock
0.0%
Overall
Mortality
50.0%
MacArthur R, et al.
CID 2004;38:284
IHI: PREVENTION OF
CENTRAL LINE INFECTIONS
Hand hygiene
Maximal barrier precautions
Chlorhexidine skin antisepsis (now CHG-alcohol)
Optimal catheter site selection, with subclavian vein as the
preferred site for nontunneled catheters
Daily review of line necessity, with prompt removal of
unnecessary lines
PREVENTION OF CLA-BSI:
EDUCATION
Educate HCP regarding indications for intravascular catheter use, proper
procedures for insertion and maintenance of IV catheters (IA)
Periodically assess knowledge of and adherence to guidelines for all HCP
involved in catheter insertion and maintenance (IA)
Designate only trained HCP who demonstrate competency for intersertion
and maintenance of peripheral and central venous catheters (IA)
Ensure appropriate nursing staff levels in ICUs (IB)
O’Grady NP, et al. Clin Infect Dis 2011;52:e1
PREVENTION OF CLA-BSI:
SELECTION OF CVC CATHETERS AND SITES
Weigh the risks and benefits of placing a CVC at a recommended site to
reduce infectious complications against the risk for complications (lA)
Avoid using the femoral vein for central venous access in adult patients (lA)
Use a subclavian site, rather that jugular or femoral site, in adults (lB)
Avoid the subclavian site in hemodialysis & ESRD patients (lA)
Use ultrasound guidance to place CVC (lB)
Use a CVC with the minimum number of ports or lumens essential for the
management of the patient (lB)
Promptly remove any CVC catheter that is no longer essential (lA)
When adherence to aseptic technique cannot be ensured (e.g., ED
placement), replace the catheter as soon as possible (lB)
PREVENTION OF CLA-BSI:
HAND HYGIENE AND ASEPTIC TECHNIQUE
Perform hand hygiene before and after palpating catheter insertion sites as
well as before and after inserting, replacing, accessing, repairing, or
dressing an IV catheter (lB)
Maintain aseptic technique for the insertion and care of IV catheters (lB)
Wear clean vs sterile gloves for the insertion of peripheral IV catheters (lC)
Sterile gloves should be worn for the insertion of arterial, central, or midline
catheters (lA)
Wear either clean or sterile gloves when changing the dressing on IV
catheters (lC)
Use maximal sterile barrier precautions (cap, mask, sterile gown, sterile
gloves, sterile full body drape) for the insertion of CVCs, PICCs, or
guidewire exchange (lB)
PREVENTION OF CLA-BSI:
SKIN PREPARATION
Prepare skin with an antiseptic (70% alcohol, tincture of iodine, an iodophor
or chlorhexidine) before peripheral IV catheter insertion (lB)
Prepare clean skin with a >0.5% chlorhexidine preparation with alcohol
before a CVC or arterial catheter insertion or dressing (lA)
Antiseptics should be allowed to dry according to the manufacturer’s
recommendation prior to placing the catheter (lB)
PREVENTION OF CLA-BSI:
CATHETER SITE DRESSING REGIMENS
Use either sterile gauze or sterile, transparent, semipermeable dressing to
cover the catheter site (lA)
If the patient is diaphoretic or if the site is bleeding or oozing, use a gauze
dressing until this is resolved (ll)
Replace catheter site dressing if the dressing becomes damp, loosened, or
visibly soiled (lB)
Do not use topical antibiotics ointment or creams on insertion sites, except
for dialysis catheter (lB)
Do not submerge the catheter or catheter site in water (lB)
Replace dressings on CVC sites at least every 7 days for transparent
dressings, except in pediatrics (lB)
PREVENTION OF CLA-BSI:
CATHETER SITE DRESSING REGIMENS
Replace transparent dressings used on tunneled or implanted CVC sites no
more than 1x/week until the insertion site has healed (ll)
Ensure that catheter site care is compatible with the catheter material (lB)
Use a chlorhexidine-impregnated sponge dressing for temporary short-term
catheters in patients older than 2 mo of age if CLA-BSI rates are not
decreasing (lB)
Monitor the catheter sites visually when changing the dressing or by
palpation through an intact dressing on a regular basis. If patients have
tenderness at the insertion site, fever with a source, or other manifestations
of local or bloodstream infections, remove the dressing and exam the site
(lB)
PREVENTION OF CLA-BSI:
OTHER
Use a 2% chlorhexidine wash for daily skin cleansing to reduce CLA-BSI (II)
Use a sutureless securement device (ll)
Use a chlorhexidine/silver sulfadiazene or minocycline/rifampin
impregnated CVC in patients whose catheter will remain in place >5d (lA)
Do not administer system antimicrobial prophylaxis (lB0
Use prophylactic antimicrobial lock solution in patients with long-term
catheters who have a history of multiple CLA-BSI despite optimal maximal
adherence to aseptic technique (ll)
Do not routinely use anticoagulant therapy to reduce the risk of catheterassociated infection in general patient populations (ll)
Do not routinely replace CVCs, PICCs, hemodialysis catheters (lB)
CDC EDUCATIONAL MATERIAL
http://www.cdc.gov/HAI/bsi/bsi.html
BATHE ICU PATIENTS >2 MONTHS OF AGE
WITH A CHG PREPARATION DAILY
Intervention = Daily bathing with 2% CHG impregnated washcloth
Design & setting : Cross-over study in MICU
Result: CHG associated with decreased
rate (per 1,000 patient days) of CLA-BSI
(4.1 vs 10.4)
Bleasdale S, et al. Arch Intern Med 2007;167:2073
IMPREGNATED CATHETERS:
META-ANALYSIS, 1985-2006
Meta-analysis, 1985-2006
Site: ICU
34 studies included in the review
Outcome: Catheter colonization (RR, 95% CI), CLA-BSI (RR, 95% CI)
Coated catheter vs uncoated catheter
CH-SS (external)
CH-SS (internal and external)
Minocycline/rifampcin
Silver, platinum, carbon
Silver ion-alloy
Chlorhexidine
CH-SS, chlorhexidine/silver sulfadiazene
Catheter colonization
0.59 (0.50-0.71)
0.44 (0.23-0.85)
0.40 (0.23-0.67)
0.76 (0.57-1.01)
1.09 (0.68-1.74)
1.11 (0.80-1.55)
CLA-BSI
0.66 (0.47-0.93)
0.70 (0.30-1.62)
0.39 (0.17-0.92)
0.54 (0.16-1.85)
0.95 (0.29-3.16)
2.37 (0.63-8.96)
Ramritu P, et al. AJIC 2008;36:104
IMPREGNATED CATHETERS:
META-ANALYSIS , 1985-2006
Ramritu P, et al. Am J Infect Control 2008;36:104-17
IMPREGNATED CATHETERS:
META-ANALYSIS, 1985-2006
CHG/Ag-Sulphadiazene vs Noncoated catheters
Minocycline/Fig vs noncoated catheters
IMPREGNATED CATHETERS:
META-ANALYSIS
Meta-analysis, 1950-2006
34 studies included in the review
Outcome: Catheter colonization (RR, 95% CI), CLA-BSI (RR, 95% CI)
Coated catheter vs uncoated catheter
CH-SS (external)
CH-SS (internal and external)
Minocycline/rifampcin
Silver alloy
Silver iontophoretic
Silver
CH-SS, chlorhexidine/silver sulfadiazene
Catheter colonization
0.51 (0.42-0.61)
0.39 (0.25-0.60)
0.39 (0.27-0.55)
1.21 (0.84-1.77)
0.84 (0.60-1.16)
1.07 (0.71-1.62)
CLA-BSI
0.68 (0.47-0.98)
0.47 (0.20-1.10)
0.29 (0.16-0.52)
0.58 (0.29-1.17)
1.98 (0.40-9.95)
0.93 (0.34-2.50)
Casey A, et al. Lancet ID 2008;8:763
CA-BSI rates since 1999 at UNC HCS
10.00
9.00
CA-BSI per 1000 central line days
8.00
7.00
6.00
ICUs
5.00
Hospital-wide
4.00
3.00
2.00
1.00
0.00
1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012
INFECTION CONTROL INTERVENTIONS
2000: Addition of 2% chlorhexadine/70% isopropyl alcohol (ChoraPrep®)
to the central line dressing kit
2001: Mandatory training for nurses on IV line site care and maintenance.
2003: Full body drape added to central line kit. MD could choose kit
containing a catheter impregnated with antiseptic or antibiotic
2005: 2nd generation impregnated catheter included in all central line kits
(except for Neonatal ICU)
2006: Pilot in MICU of IHI bundle to prevent CLA-BSI.
2007: Implementation of the IHI bundle in all ICUs.
2008: Implementation of Infection Control Liaison Program
2009: Implementation of Biopatch
CONCLUSIONS
Healthcare-associated bloodstream (BSI) cause
significant morbidity and mortality
The most important risk factor for BSI is a central venous
catheter
A near 0 rate of CLA-BSI is possible using existing
technology and appropriate process measures
Current guidelines should be followed for the diagnosis
and management of CLA-BSI