Physiological Adaptations to Labor and Delivery
advertisement

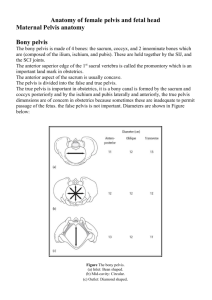
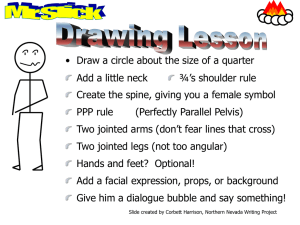
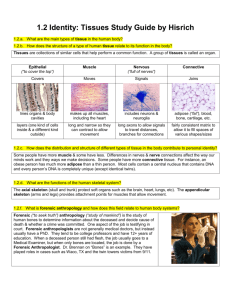
Physiological Adaptations to Labor and Delivery Labor - the process by which the products of conception are expelled from the body. Delivery - refers to the actual birth Essential Factors in Labor Successful labor and delivery results from the effective interplay of several factors: anatomic, physiologic, and physiological. These factors are referred to as the four “P”s: Passenger, Passageway, Powers and the Psychological. The Birth Passage: Pelvis -the purpose of examination of the bony pelvis is to determine if the pelvic cavity is of adequate size to allow for the passage of the full term infant. True pelvis and false pelvis: a. False pelvis supports weight of uterus. Shallow basin above the inlet or brim. b. True pelvis consists of brim or inlet - upper margin pubic bone posteriorly by upper margin of sacrum. Outlet pubic arch to tip of coccyx. Types of pelvis - the most satisfactory for delivery is gynecoid. (anthropoid, android, plattypoid) The portion of the pelvis that has the most impact on a successful labor and delivery is the outlet. If the baby enters the inlet and progresses down the birth canal and cannot get through the outlet, then there are problems. The Passenger / the Fetus 1. Fetal Head - because of its size and rigidity, the fetal head has a major effect on the birth process. Looking from the vertex position. Bones - 2 parietal, 2 temporal, 2 frontal, occiput. These bones are united by sutures, sagittal, lambdoidal, coronal. At intersections are the anterior fontanel (diamond shaped) and the posterior fontanel (triangle shaped) These bones are not firmly united - slight overlapping or molding of head occurs in labor. Slide over one another permits adaption. Head can also rotate, flex, and extend. Measure head to check if can fit through pelvis. Bi-parietal diameter and bitemporal diameter are measured. 2. Fetal Lie - relationship of long axis of fetus to long axis of mother. a. Longitudinal lie - parallel with each other cephalic or breech, optimal b. Transverse lie - across axis, usually have C-section 3. Attitude - relationship of fetal body parts to each other. Posture in utero = ovoid. Head flexed on chest, knees flexed etc. Change in attitude, particularly the head causes the fetus to present larger diameters of the head to the pelvis. 4. Presentation - that portion of the fetus that enters the pelvis first and covers the internal os. The three main types include: a. cephalic – 95% are in the cephalic presentation. Head presentations are in three types using the reference point = occiput 1) vertex 2) face 3) brow 4) military b. breech – 3% are buttocks present first. The reference point = sacrum c. shoulder –2% are transverse 5. Position - relationship of the fetal presenting part to the maternal bony pelvis. The landmark on fetus is the posterior fontanel. a. Step 1 - determine presenting part. Is it vertex = occiput; face - mentum; breech = sacrum b. Step 2 - mothers pelvis is divided into four imaginary quadrants: right or left; anterior or posterior. The Passageway Pelvis -the purpose of examination of the bony pelvis is to determine if the pelvic cavity is of adequate size to allow for the passage of the full term infant. True pelvis and false pelvis: a. False pelvis supports weight of uterus. Shallow basin above the inlet or brim. b. True pelvis consists of brim or inlet - upper margin pubic bone posteriorly by upper margin of sacrum. Outlet pubic arch to tip of coccyx. Types of pelvis - the most satisfactory for delivery is gynecoid. (anthropoid, android, plattypoid) Relationship of Maternal Pelvis and Presenting Part: Engagement -the largest diameter of the presenting part has passed through the pelvic inlet. Once this happens you’ve established that the inlet is adequate. No info about outlet. The process of Engagement is includes floating or ballotable, dipping, and engaged. Station - degree to which the presenting part has descended into the pelvis. Relationship between the presenting part and the ischial spines. 0 station is at level of the ischial spines. 0 station is at level of the ischial spines and is said to be engaged. Above the ischial spines is - (minus) station and below the ischial spines is + (plus) station. Primary Forces of Labor - The Powers Primary Powers: Involuntary Uterine Contractions - muscular contractions effect all the changes during the first stage of labor which lead to complete dilation and effacement of the cervix. Secondary Powers: Voluntary Uterine Contractions - abdominal muscles assist in second stage with pushing. Bearing down urge results in upper intra-abdominal pressure that compresses all sides of uterus and aids in expulsive forces. Psychological Considerations: Women who are relaxed, knowledgeable of birth process can have an easier labor. Childbirth classes focus on this concept - decrease fear, decrease tension, and therefore, decrease pain. Techniques for Assessment of Labor Now that we have gone through the four essential factors of labor we are ready to assess the patient. I. Abdominal Palpation / Leopold’s Maneuver The Leopold’s Maneuver is a systematic external examination of the abdomen to assess fetal position, lie, presentation, fetal movement, number of fetus, and engagement. Preparation - empty bladder, lie on back with pillow to tilt to side, knees flexed to relax abdomen. Procedure -stand on right side face woman and begin. Palpate with fingers and palms of hands, not fingertips. 1. Start at upper fundus, palpate for head or buttocks 2. With palms go down each side and locate back 3. Gently grasp lower portion with thumb and forefinger and feel for the head 4. Turn and face woman=s feet and repeat the procedure Auscultation Assess for the area of greatest intensity of the FHR. Can determine if breech or vertex and right or left. Vaginal Examination Sterile examination per vagina to determine: 1. Presentation 2. Position - find sagittal suture and fontanels, usually the posterior fontanel 3. Condition of Membranes - intact or bulging. If think may be ruptured then check with nitrazine paper -will turn blue. Then perform fern test. 4. Effacement -shortening and thinning of cervix. The cervix is obliterated or taken-up by shortening of the uterine muscles. Pulled into the lower uterine segment. Measured in % ranging from 0%-100%. 5. Dilatation -Enlargement and widening of cervical os. Dilatation of cervix is involuntary and occurs by the drawing upward of the musculofiber components of the cervix. Measure in cm. 0-10 cm. Dilatation of cervix is the result of: contractions; pressure of amniotic fluid sac; and pressure of the presenting part. 6. Station – where is the presenting part – at 0 station is at level of the ischial spines and is said to be engaged, above the ischial spines is - (minus) station, or below the ischial spines is + (plus) station. 7. Engagement –is the fetus ballottable, dipping, or engaged. Ultrasound Passage of high-frequency sound waves through uterine area to determine pelvic measurements, locate placenta, and observe fetal outline. Physiology of Labor Causes of Labor: The cause of onset of labor is unknown. Many theories have been said to explain why. Probably the result of a combination of several factors. 1. Progesterone withdrawal hypothesis - A decrease in level of progesterone. Estrogen levels can rise with the decrease in progesterone. 2. Prostaglandin Hypothesis -high level of prostaglandins trigger contractions 3. Corticotropin-releasing hormone – CRH levels rise at pregnancy term Premonitory Signs and Symptoms of Labor: Premonitory signs or impending signs are the physiological changes that take place the last several weeks of pregnancy or even the last several hours. 1. Lightening - descent of uterus downward and forward B the presenting part descends into the pelvis. Found on office visit when measure fundus it decreases. Woman can breathe easier, but feels pelvic pressure, leg cramps, and need to void. 2. False labor pains increase - Braxton-Hicks may become painful and similar to true labor. Usually felt in abdomen and cervix does not dilate and efface. 3. Show - expulsion of mucus plug -pinkish to blood tinged. Labor usually begins in 24-28 hours after expelled. 4. ROM varies from trickle (may think have urinary incontinence) to gush of amniotic fluid. No such thing as dry labor - amniotic fluid produced until delivery. Check with nitrazine paper. 5. Backache – usually occurs day before going into labor 6. Diarrhea 7. Sudden increase in energy – nesting instinct True Labor vs. False Labor: True Labor False Labor Contractions Regular, increase in intensity with walking; increase in frequency and duration Irregular, intensity unchanged Discomfort Lower back and radiates girdle-like fashion from back to front of abdomen Abdomen or groin relief with walk Cervix Show Progressively D & E. pinkish No change; none, or brownish; if had vaginal exam in last 48 hours Phases and Stages of Labor: Stage I Phase I Phase II Phase III Stage II 0-10 cm Early or latent phase 0-3 cm Mid-phase or active phase 4-7 cm Transition phase 8-10 cm Birth of Baby / pushing stage Stage III Stage IV Birth of Placenta Recover 1-2 hours post-partum Forces of Labor: Contractions - each contraction exhibits a wavelike pattern that begins slow increment, reaches acme (peak), and then diminishes (decrement). As labor progresses, contractions should increase in discomfort, intensity, and duration. Frequency - beginning of the increment of one contraction to the beginning of the increment of the next contraction. Duration -beginning of the increment to the completion of decrement of the same contraction. Assessment of Contraction - 1) subjective symptom by the woman; 2) palpation and timing by nurse with fingers placed lightly on the fundus of the uterus; 3) use of electronic monitoring. Duration of Labor: Length 1. 2. 3. of labor depends on: Regular progression of labor Effacement and regular progressive dilation of cervix Progress in descent of presenting part 4. Preparation and relaxation of the mother The length depends on the greater resistance of the cervix. Primigravida - up to 22 hours. Average = 12. 2 hours Multigravida - 8-16 hours Mechanisms of Second Stage: 1. 2. 3. 4. 5. 6. Descent Flexion Internal Rotation Extension External Rotation Expulsion Placental Separation: 1. Globular rise in the abdomen 2. Sudden gush of blood 3. Lengthening of the umbilical cord