مفاهيم في التمريض3- أ. هناء أبو سنينة مع أستاذ عبد الباسط الحليقاوي
advertisement
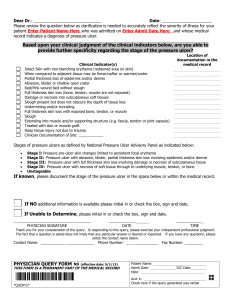
Kingdom of Saudi Arabia Ministry of Higher Education Al-Jouf University Collage of Applied Medical Sciences Department of Nursing Subject: concept of nursing (123 nur) Outline: 1- Define Immobility: 2- effect of Immobility: 3- Pressure ulcer 4- Stage of Pressure ulcer 5- Causes Pressure ulcer 6- Pathophysiology Pressure ulcer 7- Signs and symptoms Pressure ulcer 8- Complications of Pressure ulcer 9- Diagnosis 10- Treatment of Pressure ulcer Define Immobility: Refers to a reduction in the amount and control of movement a person has. Normally people move when they experience discomfort due to pressure on an area of the body. Healthy people rarely exceed their tolerance to pressure. However. Paralysis, extreme weakness, pain, or any cause of decreased activity can hinder person's ability to change positions independently and relative the pressure, even if the person can perceive the pressure. Effect of Immobility: a. Cardiovascular System. (1) Venous stasis caused by prolonged inactivity that restricts or slows venous circulation. Muscular activity, especially in the legs, helps move blood toward the central circulatory system. (2) Increased cardiac workload due to increased viscosity from dehydration and decreased venous return. The heart works more when the body is resting, probably because there is less resistance offered by the blood vessels and because there is a change in the distribution of blood in the immobile person. The result is that the heart rate, cardiac output, and stroke volume increase. (3)Thrombus and embolus formation caused by slow flowing blood, which may begin clotting within hours, and an increased rate in the coagulation of blood. During periods of immobility, calcium leaves bones and enters the blood, where it has an influence on blood coagulation. (4)Orthostatic hypotension probably due to a decrease in the neurovascular reflexes, which normally causes vasoconstriction, and to a loss of muscle tone. The result is that blood pools and does not squeeze from veins in the lower part of the body to the central circulatory system. The immobile person is more susceptible to developing orthostatic hypotension. The person tends to feel weak and faint when the condition occurs. b. Respiratory System. (1) Hypostatic pneumonia. The depth and rate of respirations and the movement of secretions in the respiratory tract is decreased when a person is immobile. The pooling secretions and congestion predispose to respiratory tract infections. Signs and symptoms include: Increased temperature. Thick copious secretions. Cough. Increased pulse. Sharp chest pain. Dyspnea. (2) Atelectasis: When areas of lung tissue are not used over a period of time, incomplete expansion or collapse of lung tissue may occur. (3) Impaired coughing: Impairment of coughing mechanism may be due to the patient's position in bed decreasing chest cage expansion. c. Musculoskeletal System. (1) Muscle atrophy. Disuse leads to decreased muscle size, tone, and strength. (2) Contracture. Decreased joint movement leads to permanent shortening of muscle tissue, resistant to stretching. The strong flexor muscles pull tight, causing a contraction of the extremity or a permanent position of flexion. (3) Ankylosis. Consolidation and immobility of a joint in a particular position due to contracture. (4) Osteoporosis. Lack of stress on the bone causes an increase in calcium absorption, weakening the bone. d. Nervous System. (1)Altered sensation caused by prolonged pressure and continual stimulation of nerves. Usually pain is felt at first and then sensation is altered, and the patient no longer senses the pain. (2)Peripheral nerve palsy. e. Gastrointestinal System. (1) Disturbance in appetite caused by the slowing of gastrointestinal tract, secondary immobility, and decreased activity resulting in anorexia. (2) Altered digestion and utilization of nutrients resulting in constipation. (3) Altered protein metabolism. f. Integumentary System. Risk of skin breakdown, which leads to necrosis and ulceration of tissues, especially on bony areas. g. Urinary System. (1) Renal calculi (kidney stones) caused by stagnation of urine in the renal pelvis and the high levels of urinary calcium. (2) Urinary tract infections caused by urinary stasis that favors the growth of bacteria. (3) Decreased bladder muscle tone resulting in urinary retention. h. Metabolism. (1) Increased risk of electrolyte imbalance. An absence of weight on the skeleton and immobility causes protein to be broken down faster than it is made, resulting in a negative nitrogen balance. (2) Decreased metabolic rate. (3) Altered exchange of nutrients and gases. i. Psychosocial Functioning. (1) Decrease in self-concept and increase in sense of powerlessness due to inability to move purposefully and dependence on someone for assistance with simple self-care activities. (2) Body image distortions (depends on diagnosis). (3) Decrease in sensory stimulation due to lack of activity, and altered sleep-wake pattern. (4) Increased risk of depression, which may cause the patient to become apathetic, possibly because of decreased sensory stimulation; or the patient may exhibit altered thought processes. (5) Decreased social interaction. Pressure ulcer Pressure ulcers, commonly called pressure sores or bedsores, are localized areas of cellular necrosis that occur most often in the skin and subcutaneous tissue over bony prominences. These ulcers may be superficial, caused by local skin irritation with subsequent surface maceration, or deep, originating in underlying tissue. Deep lesions often go undetected until they penetrate the skin, but by then, they've usually caused subcutaneous damage. Most pressure ulcers develop over five body locations: sacral area, greater trochanter, ischial tuberosity, heel, and lateral malleolus. AGE ALERT Age also has a role in the incidence of pressure ulcers. Muscle is lost with aging, and skin elasticity decreases. Both these factors increase the risk for developing pressure ulcers. STAGES OF PRESSURE ULCER: A stage 1: pressure ulcer is an observable pressure-related alteration of intact skin. The indicators, compared with the adjacent or opposite area on the body, may include changes in one or more of the following factors: skin temperature (warmth or coolness), tissue consistency (firm or boggy feel), or sensation (pain or itching). The ulcer appears as a defined area of persistent redness in lightly pigmented skin; in darker skin, the ulcer may appear with persistent red, blue, or purple hues A stage 2 pressure ulcer is characterized by partial-thickness skin loss involving the epidermis or dermis. The ulcer is superficial and appears as an abrasion, blister, or shallow crater. A stage 3: pressure ulcer is characterized by full-thickness skin loss involving damage or necrosis of subcutaneous tissue, which may extend down to, but not through, the underlying fascia. The ulcer appears as a deep crater with or without undermining of adjacent tissue A stage 4: Full-thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or support structures (for example, tendon or joint capsule) characterize a stage 4 pressure ulcer. Causes: Possible causes of pressure ulcers include: immobility and decreased level of activity friction causing damage to the epidermal and upper dermal skin layers constant moisture on the skin causing tissue maceration impaired hygiene status, such as with fecal incontinence, leading to skin breakdown malnutrition (associated with pressure ulcer development) medical conditions such as diabetes and orthopedic injuries (predispose to pressure ulcer development) psychological factors, such as depression and chronic emotional stresses (may have a role in pressure ulcer development). Pathophysiology: A pressure ulcer is caused by an injury to the skin and its underlying tissues. The pressure exerted on the area causes ischemia and hypoxemia to the affected tissues because of decreased blood flow to the site. As the capillaries collapse, thrombosis occurs, which subsequently leads to tissue edema and progression to tissue necrosis. Ischemia also adds to an accumulation of waste products at the site, which in turn leads to the production of toxins. The toxins further break down the tissue and eventually lead to the death of the cells. Signs and symptoms: Signs and symptoms of pressure ulcers may include: blanching erythema, varying from pink to bright red depending on the patient's skin color; in dark-skinned people, purple discoloration or a darkening of normal skin color (first clinical sign); when the examiner presses a finger on the reddened area, the “pressed on” area whitens and color returns within 1 to 3 seconds if capillary refill is good pain at the site and surrounding area localized edema due to the inflammatory response increased body temperature due to initial inflammatory response (in more severe cases, cool skin due to more severe damage or necrosis) nonblanching erythema (more severe cases) ranging from dark red to purple or cyanotic; indicates deeper dermal involvement blisters, crusts, or scaling as the skin deteriorates and the ulcer progresses usually dusky-red appearance, doesn't bleed easily, warm to the touch, and possibly mottled (deep ulcer originating at the bony prominence below the skin surface). Complications: Possible complications of pressure ulcers include: progression of the pressure ulcer to a more severe state (greatest risk) secondary infections such as sepsis loss of limb from bone involvement. Diagnosis Diagnosis is based on: physical examination showing presence of the ulcer wound culture with exudate or evidence of infection elevated white blood cell count with infection possibly elevated erythrocyte sedimentation rate total serum protein and serum albumin levels showing severe hypoproteinemia. Treatment Treatment for pressure ulcers includes: Repositioning by the caregiver every 2 hours or more often if indicated, with support of pillows for immobile patients; a pillow and encouragement to change position for those able to move Foam, gel, or air mattress to aid in healing by reducing pressure on the ulcer site and reducing the risk for more ulcers Foam, gel, or air mattress on chairs and wheelchairs as indicated Nutritional assessment and dietary consult as indicated; nutritional supplements, such as vitamin C and zinc, for the malnourished patient; monitoring serum albumin and protein markers and body weight Adequate fluid intake (I.V. if indicated) and increased fluids for a dehydrated patient Good skin care and hygiene practices (for example, meticulous hygiene and skin care for the incontinent patient to prevent breakdown of the affected tissue and skin) Stage II, cover ulcer with transparent film, polyurethane foam, or hydrocolloid dressing Stage II or IV, loosely fill wound with saline- or gel-moistened gauze, manage exudates with absorbent dressing (moist gauze or foam) and cover with secondary dressing Clean, bulky dressing for certain types of ulcers, such as decubiti Surgical debridement for deeper wounds stage III or IV as indicated.