Neurological examination
advertisement

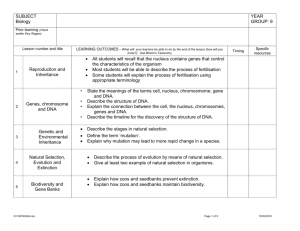
The University of Newcastle Faculty of Medicine and Health Sciences Bachelor of Medicine Year 2 Professional Skills Neurology YEAR TWO Prepared by: Dr I Kerridge Dr M Parsons Dr D Williams THE NEUROLOGICAL EXAMINATION CONTENTS Page NEUROLOGY: PROFESSIONAL SKILLS ............................................................................. 3 MENTAL STATUS EXAMINATION ...................................................................................... 4 HIGHER CENTRES .................................................................................................................. 5 SPEECH..................................................................................................................................... 6 GAIT .......................................................................................................................................... 8 CRANIAL NERVES ................................................................................................................. 9 UPPER LIMBS ........................................................................................................................ 14 LOWER LIMBS ...................................................................................................................... 17 CEREBELLAR ........................................................................................................................ 20 D:\106757935.DOC\March 9, 2016\RSPOUSE 2 NEUROLOGY: PROFESSIONAL SKILLS The neurological examination may be divided into a number of parts. These are: 1. MMSE ] 2. Higher Centres ] 3. Speech ] 4. Cranial Nerves 5. Gait 6. Cerebellar 7. Upper limb 8. Lower limb Crossover There is a huge amount of information that can be elicited in a neurological examination, but a fairly complete examination can be done in 10-15 minutes if the examiner is well-practised. The general approach to neurological short case examinations is for the candidate to: 1. Listen to the examiner. 2. Be sensitive to the patient. This includes talk to the patients and making any commands clearly. In many cases the exact wording of commands needs a lot of practise. 3. Inspect : skin, scars posture drips/catheters face involuntary movements D:\106757935.DOC\March 9, 2016\RSPOUSE 3 voice. 4. Palpation 5. Tone 6. Power 7. Reflexes 8. Co-ordination 9. Sensation The aim of the neurological examination is to recognize various patterns of signs that allow you to decide: 1. What are the findings on examination? e.g. - Hemiparesis 2. Where is the lesion(s)? e.g. - Cortex 3. What is the underlying cause? e.g. - CVA D:\106757935.DOC\March 9, 2016\RSPOUSE 4 MENTAL STATUS EXAMINATION Folsteins’ Mini-Mental State Examination (MMSE) The mini-mental state examination is a test of cognitive dysfunction. It is important that a low score on a mini-mental state exam should not automatically lead the examiner to state that the patient has dementia because there are a number of reasons why a person might have cognitive dysfunction, including delirium and dementia and depression. The major dificulty with using the MMSE is that the normal range of scores varies with age and educational level. For example, the median score for a 50 year old with some higher education is 30 (and the 25th percentile is 28), whereas the median score for n 85 year old with less than 4 years education is 20 ( and the 25th percentile is 15). Tables of normal values for the MMSE are available (see for example Crum RM, Anthony JC, Bassett SS et al. “Population-based norms for the Mini-mental State examination by age and educational level.” JAMA 269: 2386-91, 1993., however most clinicians appear to simply remember a cut off score of about 23 in which those above are thought of as normal and those below are thought of as impaired. If this approach is used, it must be supplemented by the examiner -carefully looking at the responses to each question and asking if the response is consistent with the age and educational level of the patient. For example, a professor of English literature who cannot spell the word “world” backwards, has clearly got a degree of cognitive decline, whereas an illiterate labourer wit the same answer may be perfectly normal. There are a number of other problems with the MMSE that the user should be aware of. Some questions are known to be a little unclear, (for example the marking of question 4 is unclear), and no time limit. Furthermore, other ethnic groups are known to score badly on some items compared to English speakers (including season, county, spelling, serial subtraction, and “no ifs ands or buts”) Some of the questions need to be modified slightly for D:\106757935.DOC\March 9, 2016\RSPOUSE 5 other countries (ie “county” has no meaning in Australia.) With these limitations in mind, the MMSE is a useful screening test for cognitive dysfunction. Specific Test Function and Area Tested Points 1. What is the year/season/day/date/month? Orientation (frontal) 5 2. What is the state/county/town/ Orientation (frontal) 5 3. Repeat three items Registration (frontal) 3 4. Serial subtraction of sevens or spell Concentration (frontal) 5 Naming (dominant 2 Score hospital/floor? “World” backwards 5. Name wristwatch and pen Temporoparietal) 6. Say “no ifs, ands, or buts” Expressive speech (dominant 1 frontal) 7. Take this paper in your right hand, fold it in half and put it on the table. Three-stage command 3 (frontal) D:\106757935.DOC\March 9, 2016\RSPOUSE 6 8. Read “close your eyes” and do it Reading (dominant 1 temporoparietal) 9. Remember the three items from Part 3 above 10. Write a sentence Short-term memory 3 (dominant hippocampal) Writing (dominant 1 temporoparietal) 11. Copy intersecting pentagons “Construction” (non- 1 dominant parietal) TOTAL D:\106757935.DOC\March 9, 2016\RSPOUSE 7 There are a number of alternative tests to the Folstein’s MMSE including the “Blessed Six Item Orientation-Memory-Concentration Test”. Total score: < 8 - normal or minimal impairment; 9 to 19 - moderate impairment; > 20 - indicates severe impairment. Reference: Katzman et al American Journal of Psychiatry 140 (1983) 6. Item Number of Score given errors for each error Score possible 1. What YEAR is it now? 1 x4 2. What MONTH is it now? 1 x3 MEMORY PHRASE: Repeat this phrase after me: “John Brown, 42 Market St, BRISBANE.” 3. About what TIME is it? (Within 1 hour) 1 x3 4. Count backwards 20 to 1 2 x2 5. Say the months in reverse order 2 x3 D:\106757935.DOC\March 9, 2016\RSPOUSE 8 6. Repeat the memory phrase 5 x2 TOTAL /30 D:\106757935.DOC\March 9, 2016\RSPOUSE 9 HIGHER CENTRES EXAMINATION 1. ASK PATIENT IF LEFT OR RIGHT-HANDED: The text books have very conflicting data about handedness and dominance. One often quoted figure is : 94% Right-handed persons - Dominant Left hemisphere 60% Left-handed persons - Left dominant 30% Left-handed persons - Mixed dominant 10% Left-handed persons - Right dominant however there are many other figures suggested. In general, the important fact is that almost all right handed people have left hemisphere dominance, but that some left-handed people have right or mixed dominance. 2. ORIENTATION (MMSE) 3. SPEECH 4. PARIETAL LOBE FUNCTION DOMINANT : "Gerstmann’s" ‘ Acalculia/Agraphia/Left-Right disorientation/Finger Agnosia D:\106757935.DOC\March 9, 2016\RSPOUSE 10 NON-DOMINANT : Spatial neglect (clockface)/Apraxia (PJ's, house) NON-LOCALIZING : Inattention (sensual and visual)/Homonomous hemionopia. Cortical sensory loss i.e. Proprioception, 2-point discrimination, Inattention (visual and sensory), Touch-localisation, Graphaesthesia (numbers), Astereognosis (objects). 5. OCCIPITAL - Homonomous Hemianopia - "Cortical" blindness (bilateral) - Topographical amnesia - Unable to : recognize faces (prosopagnosia) : read (alexia) : recognize objects (visual agnosia) 6. TEMPORAL - STM loss (4 words: honesty, brown, tulip, eyedropper) - LTM loss (AWhen did WWII start? ... finish?) - Confabulation (Have we met before?) - Dysphasia (receptive) and Nominal dysphasia (angular gyms of temporal lobe) - Upper Quadrant Hemianopia D:\106757935.DOC\March 9, 2016\RSPOUSE 11 7. FRONTAL - Anosmia - Proverb interpretation - Gait ataxia (wide-based, shuffling) - Primitive reflexes: grasp, pout, snout, suck, palmar-mental - Incontinence - Expressive dysphasia (Dominant: Broca's area) - Personality change : abulic (decreased initiation and spontaneity) : impaired concentration/attention : cannot pursue goals : personality change : disinhibition SPEECH Dysphasia : Disturbance in understanding or production of language. : Dominant hemisphere lesion. : Speech disorder is either fluent or non-fluent: Fluent - Sentences are of normal length and words flow easily but words are used incorrectly and D:\106757935.DOC\March 9, 2016\RSPOUSE 12 speech is difficult to understand. Patient uses paraphrasias, e g : literal paraphrasia, verbal paraphrasia and/or neologisms. Non-fluent - Speech slurred and lacks “fillers” (and, the, so, to) therefore sounds like a telegram. : Most common dysphasias: expressive, receptive, conductive and nominal. Dysarthria : Difficulty with articulation. : Cerebellar disease, bulbar palsy, pseudobulbar palsy, extrapyramidal disease. (Differentiation is difficult in terms of the quality of speech alone. Diagnosis can usually be made by the associated neurological abnormalities!). Dysphonia : Altered quality of voice. : Laryngeal disease, recurrent laryngeal nerve palsy, hysteria, myopathy. To Test: 1. Introduce yourself and shake hands. D:\106757935.DOC\March 9, 2016\RSPOUSE 13 2. 3. Free speech Comprehension : How long have you been in hospital? : What sort of work do you do? : Do you understand what I am saying? : Close your eyes (1-step command). : With your right finger touch your nose and then your ear (2-step command). : I would like you to pick up this piece of paper, fold it in half and then place it back on the bed/table (3-step command). 4. Repetition/Dysarthria assessment : Please repeat after me......”No ifs, ands or buts.” ...”West Register Street.” ...”British Constitution.” : Repeat PUH (lip weakness), TUH (tongue) KUH (palate). 5. Naming objects : Shirt, sleeve, cuff, button. Watch, band, face, hand, tell time. 6. Reading : “Read what it says on this card and do what it says”. D:\106757935.DOC\March 9, 2016\RSPOUSE 14 7. Writing : “Please write a sentence”. D:\106757935.DOC\March 9, 2016\RSPOUSE 15 TYPES OF DYSPHASIA NON-FLUENT FLUENT EXPRESSIVE RECEPTIVE CONDUCTIVE NOMINAL Understands but cannot Speech fluent but Repeats statements and Cannot name objects answer. disorganized. Unable to names objects poorly but but all other aspects of understand written or can follow commands. speech normal. spoken words/commands. BROCA’S AREA WERNICKE’S AREA TEMPORAL LOBE Dominant Posterior Dominant Third Frontal Dominant Temporal First Arcuate Fasciculus Temporoparietal area: Gyrus Gyrus Linking W and B area. Angular gyrus NAMING Poor Poor Poor Poor REPETITION May be possible with effort. Poor Poor Normal COMPREHENSION Normal Poor Normal Normal READING May have dyslexia Neologisms paraphrasias Poor Normal Abnormal content Impaired Normal Gerstmann’s Hemianopia Paraphrasia Use long sentences to SITE WRITING OTHER Hemiparesis overcome word-finding D:\106757935.DOC\March 9, 2016\RSPOUSE 16 difficulty (circumlocution) GAIT Complex. For locomotion need :Basal ganglia :Locomotor Region (mesencephalon) :Cerebellum :Spinal cord :Sensory input from joints/muscular afferents 1. Ask ... "May I walk Mr/Mrs ....." 2. Ask someone else to assist. YOU WATCH 3. Observe: posture arm swing stride base involuntary movements D:\106757935.DOC\March 9, 2016\RSPOUSE 17 4. Tandem Gait (walk heel-to-toe) 5. Rhombergs (Need 2 of 3: eyes, vestib, JPS) 6. Screening: Arms held in front with eyes closed + touch nose + lift arms up straight and then down to the horizontal. 7. Stand on toes (weak gastrocnemius) 8. Stand on heels (foot-drop) 9. Squat (proximal myopathy) +/10. If suspect cerebellar: 1. Walk around chair (fall to side of lesion) 2. March on spot (unterbergers: turn to side of lesion) COMMON GAIT DISORDERS 1. High stepping : Unilateral foot drop 2. High and slapping : 1. Bilateral foot drop (Peripheral neuropathy, HMSN) 2. Sensory ataxia (MS, Tabes dorsalis, Spinocerebellar Degeneration, sensory neuropathy) D:\106757935.DOC\March 9, 2016\RSPOUSE 18 3. Waddling (shoulders swap/tilt trunk/flex knee + hip) ‘ Weak hip abductors (proximal myopathy, OA) 4. Hemiparetic: Arm flexed, foot extended, circumduction. 5. "Scissor" (Spastic Paraparetic): both legs circumduct. (Cerebral Palsy, M.S.) 6. Parkinsonian: (freeze, no arm swing, festination, propulsion, retropropulsion) 7. Broad-based shuffle and small steps: (marche à petit pas) [Normal Pressure Hydrocephalus (Dementia, incontinence), Multi-infarct Dementia (Hyper-reflexic, brisk jaw jerk).] 8. Ataxic/ wide-based. ‘ 1. Unilateral cerebellar (falls to side of lesion) 2. Midline (staggers in all directions) CRANIAL NERVES CN 1: OLFACTORY sensory usually not tested may wish to test in the presence of personality disturbance, hemiparesis or visual loss D:\106757935.DOC\March 9, 2016\RSPOUSE 19 Test each nostril separately (use easily recognized substance e.g. peppermint oil, oil of cloves). CN 2: OPTIC 1. Observe : : 2. Acuity : Level of eyelid Position of eye - Ptosis (CN 3 lesion, myasthenia,Horner’s) - Lid retraction - Exopthalmos (Graves, tumour) - Enopthalmos (Horner’s) (Using two acuity cards - patient may use glasses) - "What is the smallest line you can read?" (Snellen card) - If less than 6/60: Counting fingers :Hand waving :Perception of light and dark 3. Gross visual fields/visual inattention: Finger confrontation. 4. Visual fields (red pin) Test with red pin: White objects more easily seen than red. Central vision ‘ Colour : cones Peripheral vision ‘ B+W : rods D:\106757935.DOC\March 9, 2016\RSPOUSE 20 Therefore earlier peripheral loss with red pin. Fig.1. The visual pathways as seen from above the brain. Letters A-F refer to visual field defects following lesions in the corresponding brain areas. Circles indicate what the left and right eyes see (the left and right visual fields). Black areas represent visual field defects. D:\106757935.DOC\March 9, 2016\RSPOUSE 21 A. Constricted field left eye (e.g. end-stage glaucoma). When constricted fields are bilateral, it sometimes signifies hysteria. B. Central scotoma (e.g. optic neuritis in multiple sclerosis). C. Total blindness of the left eye. D. Bitemporal hemianopia (e.g. pituitary gland tumor). E. Right homonymous hemianopia (e.g. stroke). F. Right superior quadrantopia. D:\106757935.DOC\March 9, 2016\RSPOUSE 22 5. Blind spot (red pin) 6. Pupils Afferent - optic nerve Efferent - PNS component of CN 3 20% difference in size - Normal (Anisocoria) Small pupil - SNS lesion Large pupil - PNS lesion : Light Reflex - direct - consensual : Accommodation : Swinging light test: Normal : Pupil always constricts Abnormal : Pupil dilates to light ‘ Afferent pupillary defect ‘ Marcus Gunn pupil ‘ Anterior to chiasm (optic neuritic or compression of the optic nerve) D:\106757935.DOC\March 9, 2016\RSPOUSE 23 Fig. 2. The pathways for the pupillary light reflex and accommodation. LGB, lateral geniculate body. The depicted lesions presumably also interrupt light reflex fibers crossing from the opposite side of the brian stem. The pathway shown innervating the eye is highly schematic; the light reflex pathway involves only pupillary constriction, whereas the accommodation pathway affects both pupillary constriction and ciliary body accommodation. D:\106757935.DOC\March 9, 2016\RSPOUSE 24 7. Fundoscopy using Opthalmoscope : Red reflex : Retina: Locate vessel: follow to disc then periphery : Venous pulse : (at cup) : Retinal background : Dilate pupil with tropic amide (DO NOT USE IN GLAUCOMA) CN 3: OCULOMOTOR CN 4: TROCHLEAR CN 6: ABDUCENS Motor to eye Autonomic Eye movements have complex control including: 1. Saccadic/command (frontal) 2. Pursuit (occipital/parietal) 3. Vestibular/positional (cerebellar/vestibular nuclei) Test 1. 2. Observe: position of head (head tilted away from the side of a CN 4 lesion). : eyelid (ptosis suggest CN 3 lesion or a Horners) : eye position (one eye looking up or down suggests skew deviation). Screen: Instruct patient to “look up, look down, look to the left, look to the D:\106757935.DOC\March 9, 2016\RSPOUSE 25 right.” 3. Pursuit movements : following a pin 4. Saccadic movements : finger to fist 5. Accommodation/convergence : "Look in to the distance ... now at my finger" 6. Consider Cover Test Note: * Diplopia (double vision) is usually maximal in the direction of gaze of the affected muscle. This indicates the abnormal cranial nerve. * In diplopia the false image is usually the outer image. This indicates the abnormal eye, e.g. CN 6 : Diplopia on lateral gaze. CN4 : Diplopia maximal looking down and in. Images at an angle. Unable to look down and out. * Comment on Nystagmus - Nystagmus defined in direction of fast movement. - When testing take inward looking eye to edge of caruncle - any further will cause physiological nystagmoid jerks. - Peripheral (vestibular) disease causes symmetrical nystagmus with the D:\106757935.DOC\March 9, 2016\RSPOUSE 26 fast phase away from the side of the lesion. The fast phase remains in the same direction despite the direction of gaze. The amplitude of nystagmus is sometimes increased by looking in the direction of the fast phase. - Central (brainstem) disease cause asymmetrical nystagmus. It is rotatory or vertical (always implies brainstem dysfunction in the absence of drugs) and may demonstrate fast phase changes with change in gaze direction. - Cerebellar disease classically cause nystagmus with the fast phase towards the side of the lesion, however, there is often distortion of the brainstem and nystagmus may be much more complex. Vermis lesions can cause up-beating nystagmus. * Internuclear opthalmoplegia: eye movements frequently normal when each eye tested individually but abnormal when pursuit movements are tested together. e.g. Left INO : Left eye fails to adduct Right eye develops nystagmus D:\106757935.DOC\March 9, 2016\RSPOUSE 27 D:\106757935.DOC\March 9, 2016\RSPOUSE 28 Fig.3. The pathway for lateral conjugate gaze. PPRF - pontine paramedian reticular formation. D:\106757935.DOC\March 9, 2016\RSPOUSE 29 CN 5: TRIGEMINAL Sensorimotor Motor to temporalis and masseter sensory to face. Large sensory nucleus extending from Pons to upper cervical cord: light touch in Pons, pain/temparature in Medulla/cervical. (Therefore pontine lesions may demonstrate loss of light touch with preservation of pain and temperature. Test: 1. 2. Corneal reflex (CN5 to feel CN7 to blink) Sensation: (Test pin-prick/soft-touch in each of the three anatomical divisions - opthalmic, maxillary and mandibular). 3. Motor: i “Clench your jaw.” Palpate temporalis/masseter bulk. ii Strength of jaw opening. “Hold your jaw open.” (Look for deviation to the side of weakness.) iii Jaw-jerk. D:\106757935.DOC\March 9, 2016\RSPOUSE 30 Fig.4. Trigeminal nerve sensory dermatomes. D:\106757935.DOC\March 9, 2016\RSPOUSE 31 CN 7 : FACIAL Sensory, motor, autonomic Motor : Facial musculature Ear Tensor tympani and stapedius : Taste : ( via chordae tympani) to the anterior 2/3 of the tongue. Test: 1. "Smile" CN 8 : 2. "Show me your teeth" 3. "Screw up your eyes" 4. "Look up to the ceiling" 5. "Whistle" 6. "Blow out your cheeks" AUDITORY Auditory/vestibular function. Test: 1. Hearing : Whispering numbers (at arms length whilst occluding the opposite ear). 2. Webers : 512 Hz tuning fork held on the centre of the head. "Where is it louder?" 3. Rinne's : 512 Hz tuning fork held on the mastoid then in front D:\106757935.DOC\March 9, 2016\RSPOUSE 32 of the ear to test bone and air conduction. Normally air conduction better than bone conduction. 4. Vestibular : Gait Nystagmus not usually part of CN exam Caloric testing WEBERS RINNE’S IN DEAF EAR Conductive Deafness Heard in deaf ear BC>AC Sensorineural Deafness Heard in normal ear AC>BC CN 9 : GLOSSOPHARYNGEAL Sensory : Posterior 1/3 of tongue, soft palate, pharynx. Motor : Stylopharyngeus Test : Gag reflex (bilaterally) D:\106757935.DOC\March 9, 2016\RSPOUSE 33 CN 10 : VAGUS Sensory : External ear Motor : Palate, pharynx, larynx (via recurrent laryngeal) Test : 1. Cough, voice quality 2. "Say Ahh" - Observe soft-palate movement. If normal uvula stays in midline - If weak uvula deviates (pulled over) to the normal side. 3. CN 11: SPINAL ACCESSORY Motor : Test Gag (Sensory - CN 9, Motor - CN 10) : Supplies - ipsilateral trapezium - ipsilateral sternomastoid 1. Shoulder elevation (trapezius) 2. Lateral head rotation (opposite sternomastoid) D:\106757935.DOC\March 9, 2016\RSPOUSE 34 3. Pushing forehead forward against resistance (bilateral sternomastoid, weakness, myopathy). CN 12 : HYPOGLOSSAL Motor to tongue Test : 1. Observe in mouth for wasting, fasiculations. 2. Stick out the tongue: Tongue points toward (pushed) to the weak side. 3. Test tongue strength. UPPER LIMBS 1) OBSERVE THE ENTIRE PATIENT 2) SHAKE HANDS (Grip strength, co-ordination, myotonia) 3) ASK PATIENT TO SIT ON THE EDGE OF THE BED 4) INSPECT: wasting (distal/proximal) deformity D:\106757935.DOC\March 9, 2016\RSPOUSE 35 fasciculation tremor 5) HOLD OUT ARMS/EYES CLOSED Drift - UMN weakness (down) - cerebellar (up: hypotonia) - post column loss (impaired JPS) 6) PIANO PLAYING (SCREENING) 7) PALPATE : muscle bulk tenderness thickened nerves 8) TONE : - median : wrist ulnar : elbow Clonus (> 3 beats) Rigidity Spasticity Cog-wheeling 9) POWER (GRADE 0 - 5) SHOULDER: Elevation - C3,4 + CN11 Abduction - C5 Deltoid (Axillary n.) + Supraspinatus Adduction - C7 Pectoralis Major (Pectoral nerves) Latissimus Dorsi D:\106757935.DOC\March 9, 2016\RSPOUSE 36 ELBOW: WRIST: Flexion - C6 Biceps (Musculocutaneous n.) Extension - C7 Triceps (Radial n) Thumb up - C6 Brachioradialis (Radial n.) Flexion - C7 Flexor carpi ulnaris (Median) Extension - C7 Extensor carpi radialis (Radial) wrist drop. FINGERS: Extension - C8 Extensor digitorum (Radial - post interosseous n.) Flexion - C8 Flexor digitorum superficialis and profundus Abduction - T1 1st Dorsal interossei, Abductor digiti minimi (Ulnar) Thumb 10) 11) REFLEXES : - T2 Abductor pollicus brevis (Median) Biceps C5 Triceps C7 Brachioradialis C6 Finger C8 CO-ORDINATION :Finger-nose :Dysdiadokokinesis D:\106757935.DOC\March 9, 2016\RSPOUSE 37 12) SENSORY With sensory examination consider cortical, intracapsular, cord, dermatomal, peripheral nerve distribution. there is significant overlap between dermatomes and between peripheral nerves therefore the area of sensory loss in dermatome or nerve lesions may be less than illustrated/expected. 1. Pain/temperature (enters cord and crosses 1-2 segments above): Pin Chest wall first Dermatomal. Dull or sharp Start proximally (unless cord compression or peripheral neuropathy suspected) Move from abnormal to normal 2. Vibration (128 Hz) (Dorsal column) 3. Proprioception (Spinocerebellar tract: Ipsilateral) D:\106757935.DOC\March 9, 2016\RSPOUSE 38 4. Light touch (Posterior column and Anterior spinothalamic tract) C4 chest to shoulders T2 Axilla C5 arm to below elbow C6 thumb/wrist T1 elbow C8 little finger D:\106757935.DOC\March 9, 2016\RSPOUSE 39 Median nerve] NOTE: Small muscles of hand supplied by: + T1 nerve root. Ulnar nerve ] Therefore look at Abductor digiti minimi, First dorsal interossei, Abductor pollicus brevis. 1. APB weak : Median nerve 2. ADM and 1st DI weak : Ulnar 3. All three weak : Many causes; cord, root, plexus lesion. Peripheral neuropathy. Motor neuron disease etc. D:\106757935.DOC\March 9, 2016\RSPOUSE 40 LOWER LIMBS 1) GAIT : Can I walk Mr/Mrs ...? If yes ... see Gait exam: Rhombergs Normal Heel-toe Stand on toes Stand on heels Squat 2) LIE DOWN 3) OBSERVE - Expose legs (use towel) - ?IDUC - Wasting: esp - 1. Generalized - 2. Tibialus Anterior/EDB/Quadriceps - 3. Pes cavus (High arch, clawed toes, thick foot) HMSN, Friedreichs, Spina bifida. 4) - Fasciculations - Tremor - Deformities PALPATE - Tenderness D:\106757935.DOC\March 9, 2016\RSPOUSE 41 5) TONE - Bulk - Tap/flick for fasiculations - Thickened nerves - Leg roll - Knee (lift up with hand in popliteal fossa) - Clonus : ankle (sustained rhythmical contractions ‘ UMN) +/- patella clomnus. 6) POWER [1. LMN: Weak, wasted, flaccid, hyporeflexic, fasciculation. [2. UMN: Spastic, clonus, hyper-reflexic, Babinski, UMN pattern weakness - Arm: Abd + Ext] Leg: HIP: Add+Flex] Flexion - L2 Ilipsoas (Femoral n) Extension - L5 S1-2 Gluteus Maximus (Inf glueal n) Abduction - L4-5 S1 Gluteus medium/minimus + Tensor fascia lata (Sup gluteal n) Adduction - L2-3 (Obturator n) D:\106757935.DOC\March 9, 2016\RSPOUSE 42 KNEE: ANKLE: Flexion - L5 S1 Hamstrings (Sciatic n) Extension - L3 Quadriceps (Femoral n) Plantarflex - S1 Soleus/Gastrocnemius (tibial n) Dorsiflex - L4-5 Tibialus Anterior (Common peroneal n) Eversion - L5 S1 Peroneus Longus (Common peroneal n) UMN Inversion - L4 Tibialus Posterior (Tibial n) Root/Plexus L5 S1 Ext digitarum longus (Deep peroneal n) - L4 Quadriceps Ankle - S1 Gastrocnemius Plantar - S1 Plantar or babinski Anal - S3-4-5 Ant Abdo - Upper - T6-8 Lower - T10-12 Dorsiflex toe - 7) 8) REFLEXES: Knee CO-ORDINATION: Heel-shin Finger-toe Foot-tap 9) SENSORY: Pin prick ] Vibration sense ] If a sensory level is present: Go to the abdomen Proprioception ] Check saddle sensation Soft touch ] Check anal reflex D:\106757935.DOC\March 9, 2016\RSPOUSE 43 10) BACK: Deformity Scars Neurofibroma D:\106757935.DOC\March 9, 2016\RSPOUSE 44 L3 knee L4 to heel (medial) L5 lateral leg and large toe S1 sole + small toe S2 up middle of leg at posteriorly D:\106757935.DOC\March 9, 2016\RSPOUSE 45 CEREBELLAR FUNCTION: Basically a servocontrol mechanism 1. Maintain posture/balance 2. Fine voluntary movements 3. Co-ordinate smooth tracking movements of eyes 4. Control trajectory, velocity and acceleration of movements. STRUCTURE: Complex Inputs: Ascending 1. spinocerebellar 2. vestib apparatus Descending 1. pyramidal 2. extrapyramidal Outputs: 1. Motor cortex 2. Basal ganglia 3. Red nucleus 4. Reticular formation 5. Vestib appartus D:\106757935.DOC\March 9, 2016\RSPOUSE 46 EXAMINATION TECHNIQUE 1. LISTEN: "This patient has a problem with co-ordination." (DDx : Cerebellar, posterior column, extrapyramidal lesions) 2. EYES : Nystagmus (when look to side of lesion Central Labyrinthe 3. :Rapid to side of lesion.) :Rapid away from lesion.) SPEECH: Impaired rate, rhythm and amplitude i.e.Jerky, explosive and loud with irregular separation of syllables: West Register Street Irish Constabulatory British Constitution 4. UPPER LIMBS : Drift : Rebound : Tremor (agonist hypotonia) : Hypotonia (loss facilitatory influence on spinal motor neurons) 5. FINGER NOSE : Intention tremor : Past-pointing D:\106757935.DOC\March 9, 2016\RSPOUSE 47 6. RAPID MOVEMENTS 7. DYSDIADOKOKINESIS 8. LEGS : tone : heel-shin : foot-tap 9. SIT ON BED : truncal ataxia : reflexes (pendular) 10. GAIT PATTERNS Midline: Dysarthria gait and truncal ataxia Hemispheric: Limb ataxia, tremor, nystagmus, hypotonia I. UNILATERAL - Ischaemia (Lateral Medullary Sydnrome), MS, Tumour, abscess, trauma, PNS II. BILATERAL - Drugs (ETOH, Phenytoin), MS, SOL, PNS, Friedreichs Ataxia, Hypothyroid, Arnold Chiar malformation. D:\106757935.DOC\March 9, 2016\RSPOUSE 48 III. MIDLINE IV. ROSTRAL/VERMIS (Spares arms) - PNS, Midline tumours - Alcohol D:\106757935.DOC\March 9, 2016\RSPOUSE 49