Gastrin
advertisement

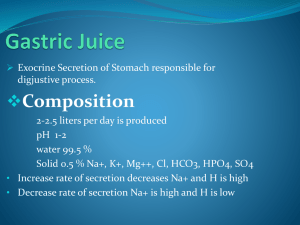
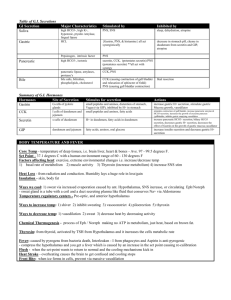
GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 1 of 10 Physiology: Gastrointestinal Secretions II Gastrin 1. Functions of Gastrin a. Stimulates HCL secretion from the parietal cells. b. Increases gastric and intestinal motility. c. Increases pancreatic secretions (mostly enzymes). d. Necessary for the proper growth of GI mucosa. It is a trophic factor that stimulates the growth of the GI mucosa to replace dead or damaged cells. 2. Mechanisms That Regulate HCL Secretion a. Vagal stimulation b. Enterogastrones: hormone signals that are inhibitory or excitatory c. pH: For example, somatostatin is released when the pH<3. d. Food products (secretagogues) i. Protein digestion products ii. Alcohol iii. Calcium iv. Coffee (caffeinated and decaffeinated). This is because coffee contains amino acids, which in return stimulate gastrin secretion. 3. Substances Stimulating Gastrin Secretion a. Bombesin- Gastrin Releasing Peptide (GRP) i. Most likely the NT responsible for stimulating G cells to secrete gastrin. ii. Vagus nerve also increases the release of GRP during the cephalic phase. 4. Substances Inhibiting Gastrin Secretion a. Somatostatin i. Inhibits gastrin secretion, especially when the pH < 3. ii. Released from D Cells in antrum and colon. iii. Vagus nerve inhibits the release of somatostatin during the cephalic phase. b. GIP (Gastric Inhibitory Polypeptide) i. Released by K cells in duodenum in response to fatty acid/glucose chyme. It also inhibits G cell release of gastrin. Pepsinogen 1. Released by chief cells in an inactive form. 2. Secreted in an inactive form, pepsinogen (proenzyme). 3. Activated by acid and previously formed pepsin in the lumen of the stomach. 4. Proteolytic enzyme that begins the process of protein digestion; optimal activity at pH 1.8-3.5. 5. It is responsible for digesting about 20% of the proteins that we eat, and it’s also one of the few proteins that is capable of digesting collagen in meat. It maintains its activity in the lumen of the stomach for a short period of time. 6. If you were to destroy the chief cells (i.e. no pepsin), will there be consequences to protein digestion? NO. You still have adequate proteases from the pancreas. However, this would have a strong role in peptic ulcer disease. Peptic ulcer disease is associated GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 2 of 10 with PEPSIN. The acid is involved in breaking down the mucosal barrier. When the mucosal barrier is broken down, it allows pepsin to digest the stomach cells causing first the erosion and then the ulcer. 7. Regulation of Pepsinogen Secretion a. Cephalic Stage: vagal stimulation; cholinergic nerves within the enteric nervous system directly stimulate chief cells to release pepsinogen. b. Gastric Phase: low pH activates local reflexes, which then activate chief cells to release pepsinogen; gastrin also stimulates the chief cells to release pepsinogen. c. Intestinal Phase: secretin enhances pepsinogen release; CCK will inhibit it. 8. Cellular Mechanisms of Pepsinogen Secretion a. This diagram shows the different receptors on a chief cell, that when stimulated will lead to pepsinogen secretion. b. You don’t need to know these intracellular signal transduction mechanisms. Just know that there are multiple receptors on this cell. Intrinsic Factor 1. Glycoprotein secreted by parietal cells along with acid (HCL). 2. Essential for the absorption of Vitamin B12 in the terminal ileum. This is the ONLY place where the absorption of Vitamin B12 occurs. a. If you have a patient with Crohn’s Disease (an inflammatory bowl disease) you may have to remove their terminal ileum, and thus these patients would need to receive monthly Vitamin B12 shots. If you are just a Crohn’s patient and have not had your terminal ileum removed, then whether or not you take these shots would depend on how much of your tissue has been destroyed. 3. If the parietal cells are destroyed (such as in chronic gastritis), you will develop: a. Achlorhydria (no acid) b. Macrocytic/pernicious anemia due to the failure of maturation of RBC’s. This is because you don’t have the intrinsic factor for Viatmin B12 absorption. i. This takes years to develop and is also usually associated with IronDeficiency Anemia. Iron-Deficiency Anemia 1. You will see the effects of this within months (as compared with pernicious anemia which takes years to develop). 2. Iron in the FERROUS form (Fe2+) is absorbed easily in the intestine. 3. Iron in the FERRIC form (Fe3+) is much harder to absorb. 4. Three things help to convert iron from the Ferric to Ferrous form: a. Vitamin C b. Acid c. Gastroferrin: released by parietal cells. When the parietal cells are destroyed, not only are you not secreting intrinsic factor, but you are also not excreting gastroferrin, which exacerbates the problem. 5. If you do not resolve this problem, then this can lead to pernicious anemia in a year or two. GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 3 of 10 Case Study: Peptic Ulcer 1. A 59 year-old man complains of really bad stomach pain. He works on an assembly line and his boss has been on him for a while. He has had indigestion for a long time. The pain is really severe and burning, radiates to chest and back. Alka-Seltzer relieves his symptoms. 2. What are the causes? Treatments? We will be discussing this in detail through the next part of the lecture. What other diseases could he have? We will see this case next week in the workshop as well. Gastric Mucosal Barrier 1. Protects the stomach from damage by intraluminal HCL, autodigestin by pepsin. 2. Four Components Contribute to the Mucosal Barrier: a. Thick viscous alkaline mucus layer (gel), 1-2 mm thick. b. Very tight junctions between cells. It doesn’t absorb much except for aspirin and alcohol. c. Blood flow to deliver water and nutrients. d. Fast turnover rate of gastric mucosa by stem cells. 3. Results in low level of absorption in the stomach. 4. Integrity maintained by mucosal blood flow, proper nutrient supply to synthesize high quality bicarbonate ion and mucus. 5. The quality of the mucosal barrier is influenced by genetic, environmental, physiological factors. Protection Offered by Mucosal Surface of the Stomach 1. Here is a gastric gland with different cells. You can see the blood vessels which supply the bicarb, sodium, water, and other nutrients that the mucus cells use to make the bicarbonate ion and the mucus. 2. In the bloodstream the pH is about 7.4, while in the mucus gel layer the pH is about 7. In the lumen of the stomach, the pH is very low around 1.5. 3. If any acid in the lumen back diffuses in the mucosal layer, it is quickly buffered by the bicarbonate in the mucus. 4. If you have a situation where you are not making the mucus, or not making enough bicarbonate, then you can have acid back diffusing through the mucus layer. Therefore you can also have pepsin getting through the mucus layer. 5. The mucosal layer leads to a low level of absorption in the stomach, and its integrity is maintained by an adequate blood flow and nutrient supply in order to synthesize a high quality bicarbonate ion. 6. Peptic Ulcer Disease is most likely caused because you have some situation which is disrupting the integrity of the mucosal barrier. Factors Influencing Mucous Secretion 1. Stimulating Factors: All Stimulate Mucus & Bicarb Secretions a. Prostaglandin E2 b. Acetylcholine c. HCL d. Glucagon e. VIP 2. Inhibiting Factors: a. NSAIDs (non-steroidal anti-inflammatory drugs): Act by inhibiting prostaglandin synthesis. People with arthritis who take these medications are particularly prone to ulcers. b. Aspirin c. Alcohol d. Bile Salts: Any reflux from small intestine to the stomach is very toxic. e. Reduced Blood Supply: A patient that has low blood pressure, low blood volume, or who is under a lot of stress so that they have vasoconstriction of their blood vessels are at an increased risk for ulcers. This was demonstrated during the air raids in Britain during WWII. Factors Affecting Gastric Mucosal Barrier 1. Aggressive Factors: (that attack the mucosal layer: things that DECREASE mucus and bicarb secretions). a. Helicobactor pylori b. HCL, pepsin: hypersecretion of HCL can overpower the mucosal barrier. The pepsin can then come in and autodigest the stomach. c. Gastrin d. Bile e. Ischemia (poor blood flow) f. Alcohol g. Nicotine h. NSAIDs, aspirin i. Stress j. Heredity k. Age: causes you to secrete a lesser quality mucus. 2. Defensive Factors: (that prevent damage to the mucosal layer) a. NO (dilator) b. Mucus, bicarbonate ion secretion c. Prostaglandins: help to form mucus and stimulate biocarbonate secretions. d. Blood Flow e. Cell restitution Gastritis 1. Inflammation of gastric mucosa caused by: a. Bacterial infection (Helibacter pylori) i. Related to about 90-95% of all chronic gastritis and peptic ulcer disease cases. b. Ingested irritant substances (aspirin, alcohol) i. Damages the gastric mucosal barrier (viscid mucus glands and/or tight epithelial junctions.) GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 5 of 10 2. Diseases Caused by Infection of Gastric Mucosa by Helibacter pylori: Helibacter pylori Colonization of Gastric Mucus Layer: Secretes urease, which converts urea to ammonia + carbon dioxide. The ammonia liquefies and digests the mucosal barrier. Immune Response Chronic Superficial Gastritis Peptic Ulcer Disease: where the pepsin back diffuses and eats away the wall of the stomach. Chronic Atrophic Gastritis: destroys gastric glands, parietal and chief cells. Predisposes You To: Gastric Cancer 3. Superficial or Acute Gastritis a. Not very harmful b. Self-Limiting c. Penetrates through the mucosa. d. Treat by removing offending agent (alcohol, aspirin, bacteria, caffeine, spices, antibiotic, digitalis, cortisone, NSAIDs). 4. Chronic Atrophic Gastritis a. Role of Helibacter pylori b. Penetrates deeply into gastric mucosa c. Causes progressive gastric atrophy d. Hypo or achlorhydria, pernicious anemia, Fe-deficiency anemia; destroys parietal and chief cells. Gastric Atrophy 1. Absence of gastric secretions; when acid is not secreted pepsin is also not secreted. 2. May predispose patient to ulcers and carcinoma. 3. Treatment: removal of cause; H2-blockers, antacids, sucralfate (drug lines stomach and acts as a protective agent), prostaglandins, Vitamin B12, Iron. 4. Decrease in number of gastric glands a. Achlorhydria (no HCL secretion) b. Hypochlorhydria (diminished HCL secretion) c. Pernicious Anemia: no intrinsic factor secreted when parietal cells are destroyed (this can also occur if the ileum is removed, such as in a severe case of Crohn’s Disease). GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 6 of 10 ULCERS Peptic Ulcer 1. Excoriated area of the mucosa caused by digestive action of gastric secretions (pepsin acting on the mucosa). 2. Location: Occur in the first few cm of duodenum (most common site), antrum of stomach, lower esophagus. a. The duodenum does not have as good of a mucosal barrier as the stomach does. 3. An ulcer penetrates into the submucosa, while a penetrating ulcer can penetrate deeper and cause damage to blood vessels and bleeding. 4. Causes: a. Disruption of Mucosal Barrier i. Helibacter pylori (at least 75-95% of all ulcers not caused by drugs, chemicals). ii. Smoking (nicotine), alcohol, NSAIDs, stress, reflux, bile salts, proteases, free radicals, ischemia, heredity, age, etc. iii. Decreased blood flow b. Excess gastric acid and pepsin secretion i. Zollinger-Ellison Disease: rare gastrinoma, gastrin producing tumor ii. Psychic stress- increased parasympathetic stimulation can lead to the hypersecretion of acid. 5. Mechanisms of Ulcers: Damaged Mucosal Barrier a. Acid stimulates mast cells to release histamine and other inflammatory chemicals. b. Tissue injury, capillary damage decreases blood flow. 6. Sequence of Events: a. Any one of these conditions that causes altered permeability of the mucosal barrier can lead to acid back diffusion and tissue injury. If the tissue injury goes deep enough to effect the blood vessels and mast cells, you can have bleeding, increased capillary permeability (in response to histamine and the acid), which then leads to more acid and pepsin being secreted because histamine stimulates the parietal and chief cells. You will then have edema, loss of fluid and blood into the gastric lumen, and loss of plasma proteins. H.Pylori, Acid, Pepsin, Aspirin, Alcohol, Bile Salts, Ischemia, Etc. ↓ Altered Permeability of mucosal layer ↓ H+ back diffusion ↓ Tissue Injury ↓ If deep enough, damage to blood vessels, histamine release ↓ More acid, pepsin secretion ↓ Increased capillary permeability to proteins ↓ Edema, loss of plasma proteins, bleeding GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 7 of 10 7. Treatments: a. Antibiotics for H. pylori. b. Reduction of stress. c. Antacid drugs. d. H/K proton pump inhibitors. e. H2 receptor blockers. f. Reduce ulcer-inducing factors: smoking, aspirin, alcohol, etc. g. Surgical removal of 3/5 of stomach. h. Vagotomy (an old treatment and is not done much anymore due to better drugs.) i. Dietary Management. j. Within a few weeks the mucosal lining should be healed due to the rapid turnover of gastric cells. Gastric Ulcers 1. Normal HCL secretion, but you still have destruction of the mucosal barrier. 2. Most likely area: antrum 3. Common causes: a. Bile (refluxing into the stomach) b. ethanol c. NSAID’s d. Helibacter pylori e. Ischemia Duodenal Ulcers 1. Increased HCL and pepsin secretion. 2. Excess acetylcholine, histamine, and gastrin. 3. Causes: a. Increased gastric release following meals (effect of Helibacter pylori). i. This leads to an Excess acetylcholine, histamine, and gastrin. b. Tobacco c. Helibacter pylori d. NSAID’s Pancreatic Exocrine Secretions 1. 1-1.5 Liters daily 2. Digestive Enzymes: by the Acinar Cells a. Proteases: i. Secreted in inactive form; kept inactivated in the pancreas and in the pancreatic duct. ii. Requires brushboarder enterokinase for activation iii. Trypsin inhibitor keeps the enzyme in an inactive form and prevents autodigestion of pancreas: trypsin, chymotrypsin, etc. b. Amylases (do not digest cellulose and other fibers) c. Lipases, cholesterol esterase 3. Bicarbonate ions (buffers the gastric acid and provides a proper environment for enzymes), Water: Epithelial cells of ducts GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 8 of 10 4. Some of the Proteins of Human Pancreatic Juice a. Don’t memorize this table. Just realize that there are a number of different enzymes being excreted by the pancreas. 5. Transport Process Involved in Elaboration of Pancreatic Juice. a. You have a spontaneous, primary secretion by the acinar cells which are then modified by the ductal cells. b. The primary secretion will be your enzymes and your different electrolytes (sodium, potassium, bicarb, and chloride.) c. The composition of the electrolytes or ions in the secretion is dependent on how fast you are secreting the pancreatic secretions. d. The ductal system modifies the primary secretion. Here we have active secretion of sodium, potassium, bicarb, and chloride, which is stimulated by secretin. The bicarb is particularly affected by secretin. e. The faster the secretory rate, the more bicarb is being stimulated to be secreted by the ductal cells. f. In the main collecting duct, you have an exchange of bicarb for chloride. At low secretion rates, you will have a lower content of bicarb. g. At low rates of pancreatic secretions anything that is secreted by the acinar cells sits in the pancreatic ducts for a longer period of time. The more time the primary secretion sits in the duct, the more time it has to be modified by the ductal cells. The main modification is the exchange of bicarb for chloride. 6. Effect of Flow Rate on Electrolyte Composition a. At a lower rate of secretion you have uptake of bicarb in exchange for chloride, so the chloride content will be higher. b. When you stimulate the pancreas and the rate of pancreas secretions increase, the primary secretion gets moved through the duct faster and there is less time for modification. You will have less chloride ion and the ductal cells will be stimulated to secrete bicarb. This is why the pH increases when the rate of secretions increase. c. We saw the same thing with salivary secretions. The longer those secretions sit in the salivary duct more modifications can be made. 7. Regulation of Pancreatic Secretion a. Neural and Hormonal Regulations b. Sphincter of Oddi: This controls the entry of secretions into the duodenum. If it is constricted, neither pancreatic secretions of bile can be secreted into the duodenum. CCK relaxes this sphincter during the digestive/intestinal phase. c. Neural i. Ach from the vagus, enteric nerves. This will stimulate the acinar cells to secrete; it has a major effect on enzyme secretions. It also stimulates bicarb secretions to a lesser extent, but neural stimulation primarily influences enzyme secretions. ii. Enzymes are primarily excreted. d. Hormonal Secretions i. Cholecystokinin (CCK) 1. Secreted by cells in the duodenum and upper jejunum in response to fats, proteases and peptones in the chyme. 2. Primarily stimulates the acinar cells to secrete enzymes. GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 9 of 10 3. Effects potentiated by vagal stimulation and secretin. ii. Secretin 1. Secreted by S-cells in the duodenum and upper jejunum in response to acid in the chyme. 2. Stimulates bicarb secretions by the pancreas: increases bicarbonate ions, water: stimulated by the formation of cAMP. 3. Effects potentiated by vagal stimulation and CCK. e. Factors Regulating Pancreatic Secretion After a Meal: Phase Stimulus Cephalic Sight, smell, taste, chewing and swallowing Release of Acetylcholine and gastrin by Vagal stimulation. Increased secretion with a greater effect on enzyme output. Gastric Protein in Food Gastrin Increased secretion with a greater effect on enzyme output. Gastric Distension Acetylcholine release by Vagal stimulation Increased secretion with a greater effect on enzyme output. Acid in Chyme Secretin Increased water and bicarbonate secretion Long-Chain Fatty Acids CCK and vagovagal reflex Increased secretion with a greater effect on enzyme output. Amino Acids and Peptides CCK and vagovagal reflex Increased secretion with a greater effect on enzyme output. Intestinal Mediators Response 8. Case Study: Pancreatitis a. A 57 year-old male presents to the ER after a car accident. He had the accident because of indigestion which got worse while driving home. Drank alcohol at a meeting. In distress, pale. Has had the indigestion for a long time. Pain is sharp, piercing, nausea is present. Fatty Diarrhea (due to inadequate enzymes). b. Dx: pancreatitis: destruction of the pancreas; enzymes in the pancreas could have become active, or you could have a toxic substance destroying it such as alcohol. c. Causes: alcoholism, gallstones, unknown. d. Consequences: defective ductal secretion of bicarbonate, protein plugs form, block ducts causing pain. Leads to the destruction of pancreatic tissue, inflammation; progressive pancreatitis leads to permanent destruction of pancreas; exocrine and endocrine secretions impaired, leads to diabetes mellitus, malnutrition e. Leads to numerous digestion and absorptive disorders. The first nutrients to be effected are the lipids. You must have pancreatic lipases for the digestion of lipids. If you don’t have these, the lipid will move down to the colon and the result will be malnutrition and fatty diarrhea. GI, Lecture #36 Friday, Feb. 28, 10:00am Dr. Gwirtz Deana Lanham for Heather Volkman Page 10 of 10 f. This is extremely painful; many take morphine for pain relief. g. Treatment: pain relief, nutritional support, alcohol abstention (we don’t know the mechanism for this), oral pancreatic enzyme extract. In the hospital you can put a nasogastric tube in the patient to suck out gastric contents so that nothing can go into the duodenum, which leads to a diminished signal to the pancreas to secrete. You want to keep your secretions to a minimum so that you can treat the inflammation.