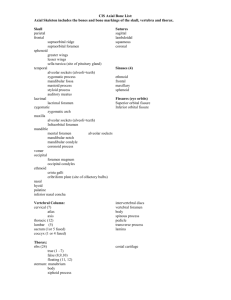
orthopedic review - HenFord
advertisement
ORTHOPEDIC REVIEW Learn it, live it, love it! Dolor, Tumor, Calor, RuborSTICKOR Cerebral Palsy Definition: non-progressive neurologic disorder in infants <3 yo Number 1 risk factor: Pre-maturity Types: A ARMS Ataxic (5%), Athetoid (10%), Rigid (10%), Mixed (15%), Spastic (60%) Athetoid is almost unheard of now due to the decreased frequency of Erythroblastosis Fetalis (ABO incompatibility) Blecks Criteria (2=poor, 1=fair, 0=good chance will walk) (The chance the CP patient will ambulate 15m w/wo forearm walker on level surface before 3yo) F oot Placement (absence of is bad) “steppage”-brush dorsum of foot or anterior aspect of tibia on table and the normal child will flex the hip and knee, dorsiflex ankle, and place the foot on the table spontaneously. E xtensor Thrust - apply pressure to sole of foot with hip in flexed position and the child will extend entire leg. (In a normal child, this reflex will disappear at 2 months, persistence is abnormal.) M oro Reflex (persistence of is bad) startle reflex or quick extension of neck –The child will abduct and extend all 4 extremities, extend the spine, extend and fan the digits except for flexion of the distal phalanges of the index finger and thumb. This reflex normally disappears at 4 –6 months. S ymmetric Tonic Neck Reflex Place the child in the quadriped position: When you flex the neck the LE ext/UE flex, and when you extend the neck the LE flex/UE ext. This reflex normally appears by 6 months. N eck Righting Reflex - Place child supine-rotate head to one side and the normal patient will log roll shoulders/pelvis as one to the same side. A ssymmetric Tonic Neck Reflex (persistence of bad) fencers posture. Place patient supine and rotate head to one side for 5 seconds then rotate to other side. The “face side” arm and leg will extend and the “occiput side” arm and leg will extend. This reflex normally disappears at 4-6 months. P arachute Reflex (absence of bad) Suspend patient and suddenly move head toward the floor. The normal patient will extend his arms and wrists so as to break the force of the fall. Spine/Scoliosis Thoracolumbar (45%) C-shaped/paralytic curves Lumbar (25%) Thoracic (16%) Double primary (14%) Standing Postures: 1. Knees extended, Hips flexed, Excessive lumbar lordosis 2. Knees extended, Hips flexed, Forward lean of trunk 3. Knees flexed, Hips flexed (Jumpers position) 2 foot problems: equinus, planovalgus Compensation for equinus: 1. Genu recurvatum 2. Midfoot break 3. Hindfoot valgus 1 SCFE Epidemiology: 2:100,000, Age 10-15 yo, M:F 2-5:1, 2 years younger in females, 25-40% bilateral, L>R Ant/lat displacement of the femoral neck on the head-head stays located in acetabulum Present as pain in knee with limited IR/ER--mom brings kid in because of limp Body types: Tall, thin athletic male (rare) Hypogonadal, obese, delayed sexual maturity Etiology theories: 1. S ynovial hypervascularity (increased height of growth plate) slip through zone of Hypertrophy 2. E piphyseal cartilage weakening (dyschondroplasia) 3. T hinning & weakening of the periosteum-lose support for head 4. 5. 6. M etabolic (Radiation, Renal osteodystrophy, Scurvy) E ndocrine (Hypothyroidism, GH, Sex hormone) T rauma 7. P hysical theory (Shear stress with oblique physis, deep acetabulum) 8. E piphysiolysis (through zone of proliferation) 9. T raumatic separation (through zone of calcification) Anatomy: Perichondral ring is last structure to fail Loder Classification: 1. Acute: <3 weeks, trauma, disabling pain, unstable Stable(can walk on it) one pin 2. Acute on Chronic: >3 weeks, limp Unstable(can’t walk on it) two pins 3. Chronic: most common ~47+% AVN rate (Loder et al) Stages: Preslip-x-ray-widening of physis, +/- Blush sign Minimal slip (<1 cm) Moderate slip (1 cm-2/3 head) Severe slip (>2/3 head) Lovell/Winter Classification: I (0-33%), II (33-50%), III (>50%) X-ray: Shentons line, Kleins line, Blush sign-osseous density in chronic slips in the metaphysis just below epiphysis (healing bone) aka Steele's sign, pistol-grip deformity, Jones bone--reactive bone on medial side Need to know: Chronicity-acute vs. chronic Open/closed growth plates Severity Systemic diseases Treatment: 1. cast 2. percutaneous pins (Stable--can walk on it--one pin, Unstable--can’t walk on it--two pins) 3. bone-peg epiphysiodesis 4. osteotomies (Southwick, Sutherland, Sugioka)--valgus and rotation 5. sex hormone manipulation--not recommended 6. open epiphysiodesis with bone graft 7. Dunn procedure--shortens femoral neck Objectives: Prevent further slip, and if acute, gently reduce slip but don't tell anyone Cause early closure of physis Prevent AVN/chondrolysis/DJD Increase function of child Complications: AVN – from unstable slips (47+% chance of AVN-Loder et al) Chondrolysis (worst complication) from leaving pins proud through femoral head Mosely approach/withdraw test-ROM under fluoro to check if pins are in joint space "Safe zone" 8mm from subchondral bone DJD, LLD 2 Perthes Disease Epidemiology: 1:1200, M:F 4:1, 15% bilateral (AVN in different stages), Peak age 5-6yo, familial 10-15% If bilateral think: 1. Meyers Dysplasia – AVN in same stage in both hips 2. Multiple Epiphyseal Dysplasia 3. Spondyloepiphyseal Dysplasia – spine involved--platyspondyly If black think HgbSS Etiology: Protein C & S or AT-III deficiencies, high lipoprotein a, hemophilia A/B, secondary to trauma, other vascular diseases, exposure to cigarette smoking Most commonly presents as PAINLESS limp Classifications: Goff-Aegeter-Ferguson---WAFR I: Widened joint space--apparent (delayed growth of ossific nucleus, hypertrophied cartilage) II: AVN (subchondral fx, crescent sign) III: Fragmentation-subchondral comp fx with cystic irreg in head, metaphyseal cyst formation IV: Resolution (Normal, Coxa magna/plana/vara/breva, gr. troch overgrowth esp if <5yo Catteral (Prognosis: I, II good/ III, IV poor) I: Anterolateral head involvement II: Central collapse (medial, lateral columns intact) III: Central sequestrum (medial column intact, head within head) IV: Whole head involvement (III and IV physis at risk due to minimal support) Salter-Thompson (True Perthes only with subchondral fracture-starts ant/lat, prognostic classification in predicting eventual involvement of the femoral head - apply only after crescent sign) A: less than half of the head (intact lateral margin) B: more than half the head (absence of lateral margin) Herring (Lateral pillar classification)-central/medial pillars are irrelevant A: Minimal involvement lateral pillar B: >50% Lateral pillar height remains => if <6yo=observe, >6yo=operate C: <50% Lateral pillar height remains =>operate Conway (bone scan stages-“biologic”) I: total lack of uptake II: lateral column uptake III: gradual fill of ant/lat epiphysis IV: base fill in epiphysis adjacent to physis Sequence of events: (Salter) VCRR TOPS 1. Vascular compromise (see etiologies above) \ 2. Cessation of growth of bony epiphysis _____ \ potential Perthes 3. Revascularization (from periphery) / 4. Resumption of ossification which is fragile / 5. Trauma leads to pathologic fracture (onset of True Perthes) 6. Onset of resorption 7. Plastic bone replacement 8. Subluxation....Residual deformity Head at Risk 1. Gages Sign (lateral V-shaped lucency on the ossific center) 2. Lateral calcification (represents fracture through epiphysis extending into physis) 3. Subluxation (worst) 4. Metaphyseal cysts 5. Horizontal physis Good prognosis: Less than half the head involved and less than a half dozen years of age 3 Evaluation Center-Edge angle Center of femoral head ....Vertical line through this point.....Line from center of head to lateral edge of acetabulum Normal is 20-40 Pathologic <20, if <15 need to augment Salter with a shelf Method of Mose: Radius= Good (w/in 2mm), Fair (2-4mm), Poor (>4mm) Treatment Goals – essentially ROM and containment 1. Decrease initial irritability 2. Maintain ROM 3. Prevent subluxation 4. Obtain spherical head Surgical Treatment: Soft tissue releases – adductor longus, ileopsoas lengthening, medial capsulotomy Salter: Age <6, Total head involvement, Congruity, Good ROM, Poor compliance w/ orthosis Lengthens leg VDRO: Procedure of choice w/ bilateral or dislocated hips Complications: Short leg limp Residual deformity – applied at skeletal maturity (Stulberg classification) 1. Round head, round acetabulum (congruent) 2. Sperical head with coxa magna/breva/vara, round/dysplastic acetabulum (congruent) 3. Mushroom head, dysplastic acetabulum (congruent) 4. Square head, square acetabulum (congruent) 5. Square head, round acetabulum (non-congruent) 4 Developmental Dysplasia of the Hip (DDH) Incidence: 1/1,000---AVN, the most devastating complication Risks: First born, Female, Frank breech, Fair complexion, Family history, Facial twist (torticollis) Diagnosis: Barlow/Ortolani initially, Galeazzi/Limitation of abduction (best after 2 mos of age) Also on physical exam: Nelaton's line: Line b/w ASIS & ischium on the lateral....greater troch should be lower Klisic's line: Line from greater troch to ASIS....should extend cephalad to umbilicus Asymetric thigh, gluteal folds X-Ray: Shenton's line Lateral displacement –Reimer Migration Index (Asymmetry b/w medial femoral metaphysis and midline) Quadrant: Horizontal = Hilg., Vertical =Perkins (Normal: Medial prox femoral metaphysis in medial/lower quadrant) Pathologic: Acetabular index >30, CE angle <20 Van Rosens View: Adduct......Push......Abduct.......Internal rotation Hourglass Deficiency: (Arthrogram) caused by Iliopsoas Gage's Position: -1 = Above Hilgenreiners line 0 = Below Hilg. line, Above nl position +1 = At normal level +2 = Below normal level Graf Classification (ultrasound) Classification & Treatment (per AHC): I: (<6 weeks) Pavlik harness - 3 mo treatment/ 1 mo of age II: (6wk - 1 year) Ortolani +: Pavlic Ortolani -: TAAT (Traction, Adductor tenotomy, Arthrography, Trumpet cast) III: (1-3 years): TAAT, +/- VDRO, Pelvic osteotomy IV: (>3 years): Open reduction, femoral shortening, +/- pelvic osteotomy In newborn with ultrasound +, but physical exam -, observation and repeat physical exam Blocks to closed reduction (LT CLIP) Hypertrophied Ligamentum teres Transverse acetabular ligament Medial Capsule Inverted Labrum Iliopsoas Pulvinar Signs of AVN (Salter): AVN increases with age and d/l 1. No ossific nucleus by 1 year following tx 25% at 1yo 2. Failure of growth of ossific nucleus following tx 50% 3yo 3. Broadened femoral neck 67% with no tx. 4. Sclerosis, Fragmentation 5. Residual deformity (Coxa magna/plana/vara) AVN resulting in a mushroom head will produce the xray finding of "the sagging rope sign" 5 Clubfoot: Talipes Equinovarus Incidence: 1/1,000, M(65%) > F, 30-40% bilateral Etiology: PAAAG 1. Packing phenomenon 2. Arrested fetal development 3. Abnormal tendon insertions 4. Abnormal talus rotation 5. Germ plasm defect Associations: PB PB MAD LSO 1. PFFD 2. Bifurcated femur 3. Pierre-Robin Syndrome – Micrognathia with glossoptosis (X-linked recessive) 4. Bilateral uni-digit foot 5. Myelodysplasia 6. AMC (Arthrogryposis) 7. Diastrophic dwarfism 8. Larsen’s Syndrome – Multiple congenital dislocations including ant. Dislocation of the tibia on the femur, frontal bossing, flat facies, hypertelorism, depressed nasal bridge. 9. Amniotic Band Syndrome (Streeters Dysplasia) 10. Other Packing Phenomena (DDH, Torticollis) Physical Findings: X-Ray findings 1. Shorter leg 1. Forefoot adduction 2. Smaller calf 2. Parallelism of talo/calc on lat max 3. Tibia internally rotated (? Internal tibial torsion) dorsiflexion 4. Talus internal/medial rotation 3. Decr. Kite’s angle on AP of foot 5. Lateral dimple over ant/lat talus 4. Plantar/medial subluxation of 6. Small/wider foot navicular (ossifies @ 5yrs) 7. Cavus-midfoot 5. Stacking of metatarsals on lateral 8. Adduction-forefoot (forefoot supination) 9. Varus-hindfoot 10. Equinus-hindfoot Poor Prognosis: 1. Teratogenic (Myelomeningocele, AMC, Diastrophic dwarfism) (Crawfordism—MAD) 2. Short, fat, rigid foot 3. Physical findings: Keel-shaped heel, Midfoot crease, Atavistic great toe 4. Delay in treatment 5. Failure to respond to initial surgery Turco’s Ball and Socket Ankle: Ball = talus Socket = calcaneus, cuboid, navicular, y-bifurcate ligament Pathologic anatomy 1. Medial deviation of head and neck of talus 2. Navicular medially/plantarly subluxed 3. Calcaneus in varus (to articulate with abnormal talus position) 4. Medial subluxation of forefoot (navicular medial and plantar) 5. Calcaneus -cuboid articulation is medial to tib-fib interosseus space (medial spin) Medial spin: Abnormal talus position causes calcaneus to spin medially (decreased Kites angle AP) Must release lateral ligaments (CFL, PTFL) to correct spin Kites Angle: Talo-calcaneal angle on AP (Normal 20-40, <30 infers varus) 6 Treatment: Manipulation (70 forefoot abduction, 20 heel valgus, 10 dorsiflexion) Casting (1-1-2-2-1: 1 week, 1 week, 2 weeks, 2 weeks, 1 month) Order of correction: CAVE Cavus, Adductus, Varus, Equinus Maximum lateral dorsiflexion film If parallelism b/w calcaneus and talus then percutaneous HCL Straight or reverse last shoes Posterior medial release (most dangerous comp. =>osteotomizing talar neck looking for talo/nav joint) Tendon lengthening: Heel cord, Post tib, FHL, FDL Posterior capsulotomy at subtalar, tibiotalar joint Ligament release: Talofibular, Calcaneofibular, Talocalcaneal, Y-bifurcate (calc-cuboid, calc-nav), Spring (med plantar calc-nav) Reduction and pinning Talonavicular joint Further treatment for partially corrected, over corrected, or recurrent clubfoot Soft tissue: Anterior tibialis tendon transfer __\ corrects “pigeon toe” deform, allows foot to Posterior tibialis tendon transfer / dorsiflex into neutral position Heyman-Herndon-Strong tarsometatarsal capsulorrhaphy Bony: Metatarsal osteotomies (for residual forefoot adduction) Evans calcaneal osteotomy (calcaneal-cuboid osteotomy / fusion) Dwyer calcaneal osteotomy (medial opening wedge osteotomy) Triple arthrodesis Talectomy => especially in AMC 7 Lower Extremity Abnormalities Congenitally Short Femur & Fibular Hemimelia Associated findings 1. PFFD 2. Hypoplastic lateral condyle 3. Hypoplastic tibial spines (absent cruciates) 4. Fibular hemimelia 5. Ball and socket ankle 6. Tarsal coalition 7. Absent lateral rays PFFD Aitken Classification A: Head present, Coxa vara, +/- Pseudarthrosis-head not articulating with acetabulum B: Head present, Pseudarthrosis at neck (Most common) C: No head, spike pointing toward acetabulum D: No head or acetabulum Coxa Vara Autosomal Dominant Defn: Shaft-Neck angle <125 degrees, metaphyseal triangle Associated with Congenitally Short Femur Hilgenreiner-Epiphyseal Angle-angle subtended through physis from Hilg line Normal is 20. Observe from 20-60. >60 => valgus osteotomy-overcorrect to allow for growth Tibial Bowing Anterolateral -- >55% have Neurofibromatosis Malignant - High risk of pseudarthrosis Anteromedial Bowing--Think O.I. Posteromedial bowing (Kyphoscoliosis tibia)-- Benign Association: Calcaneovalgus deformity Residual defect is LLD Streeter's Dysplasia Congenital constriction band syndrome Tx: Staged Z-plasties Dysplasia Epiphysialis Hemimelica (Trevor's Disease) Prevalence: 1: 1 million M:F 3:1 Intra-articular osteochondroma which stops growing at maturity. Sx. – dec. ROM, pain Multiple lesions 70% of the time Medial side > lateral joint side Most common in talus Treatment is aggressive surgery 8 Knee Disorders Congenital Knee Dislocation Classification (Finder) 1. Physiologic: 20 degrees hyperextension, Resolves by age 8 2. Simple: Physiologic that carries into adulthood 3. Subluxation: <90 degrees hyperextension, resisted flexion beyond neutral 4. Dislocation, tibia ant/prox to femur 5. Complex variants associated with AMC, MM Physiologic Genu Varum Normal under age 2 Association: Internal tibial torsion Nail-Patella Syndrome-Onchoosteodysplasia Autosomal Dominant Absence of patellae with abnormal nail beds Elbow flexion contractures Short stature Iliac wings => Fong’s Horns Blount's Disease Epidemiology: Blacks, Obese, Short, Early walkers X-Ray: Fragmentation of medial tibial metaphysis Failure of development of proximal tibial epiphysis Drennan: Metaphyseal-diaphyseal angle (>11 or 14 degrees) Classification (Langenskiold - applies only to infantile) 1. Irregularity <3yo Ignorant 2. Beaking 2-4yo Butt-heads 3. Depression of physis 4-6yo Don’t 4. Step-off 5-10yo Study 5. Two epiphyses Their 6. Bony bar Books 9 Common Foot Problems Calcaneovalgus Common (1/1000) Findings: Forefoot dorsiflexed (against tibia), Everted, Abducted Tx: Stretching exercises (Casting if rigid) Flatfeet Types: 1. Flexible: Ligamentous laxity, No treatment 2. Rigid: Insole supports if symptomatic (R/O CVT, Tarsal coalition) Congenital Vertical Talus (Rocker Bottom foot, Serpentine foot, Persian slipper foot) 0.5:1000, associated with AMC, MM Findings: Fixed equinus of hindfoot, Fixed dorsiflexion of forefoot (Post tib/Per longus=dorsiflexors) Sine qua non=navicular is dorsally dislocated and sits on anterior head/neck of talus *X-Ray: No reduction of talonavicular joint on maximum plantarflexion view, Meary’s Angle >0 ** can’t see nav until approx 5yo, so talus doesn’t line up with meta-tarsals ** if talus does line up with the meta-tarsals it is called an OBLIQUE VERTICAL TALUS Type A: Calc-cuboid located Type B: Calc-cuboid d/l Coleman/Stelling Tx: Stage 1- Stretching, Casting Stage 2- Release/lengthen anterior dorsiflexors, Triple capsulotomy, ORIF talo/nav and talo/calc with pins Stage 3- HCL, Posterior capsulotomy, Kidner procedure (Post tib transfer under navicular) Older kids, may have to excise navicular Zed Foot/Skew Foot Navicular is lateral to talus, forefoot adduction, hindfoot valgus Peroneal Spastic Flatfoot Sx: Flatfoot, Pain over lateral calf Etiology: Tarsal coalition, Trauma, JRA, Neoplasms Tarsal Coalition Age: 8-12 yo Sx: Multiple ankle sprains, Decr subtalar ROM Types: 1. Calcaneonavicular (Most common) pain in sinus tarsi with decr in subtalar ROM X-Ray: Sloman's view, Anteater nose Webster/Steward Tx: BKC first => Excision w/ peroneus brevis interposition 2. Talocalcaneal X-Ray: CT is best, if middle facet not horizontal => coalition Dorsal beaking of talar neck, narrow subtalar jt, broad lateral talar process Tx: BKC (walking), if still painful: Excise if <50% joint, o/w fuse (triple is last resort) Hallux Valgus F>M, increase IMA (>100), first MTPA (>200) Tx: 1. Release adductor hallucis 2. Medial capsulotomy, Attach adductor tendon to 1st metatarsal 3. Resect exostosis, Proximal opening wedge osteotomy of 1st metatarsal (medially) 4. Medial MTP capsulorrhaphy Most common complication: recurrence 10 Intoeing Metatarsus Adductus (Neonate to 18 months) Etiology: Packing phenomenon Differences from clubfoot 1. Can correct forefoot and hindfoot 2. Hindfoot often in valgus (not varus) 3. Talocalcaneal divergence on AP X-Ray 4. Talocalcaneal convergence on Lateral X-Ray Types: I. Corrects spontaneously (Tx: Observation) II. Passively corrects (Tx: Stretching) III. Rigid (Tx: Casting, surgery) Internal Tibial Torsion (18-36 months) Normal: Transmalleolar axis = 20 degrees of external rotation Femoral Anteversion (3-8 years) Newborn ~ 40 degrees, Adult ~ 15-20 degrees Etiology: 1. Hereditary 2. Packing phenomenon 3. Pull of iliopsoas 4. Sleeping position 5. TV squat position, “W” position Types: A - Compensation: Tibia externally rotated, Valgus feet B - No compensation Tx: Osteotomy indications: >8 yo, <10 degrees external rotation (Stehali) Osteochondroses and Pseudoosteochondroses Koehler's Disease (AVN of navicular) Sever's Disease (Calcaneal apophysitis) Iselin’s Disease ( Prox. 5th metatarsal apophysitis) Diaz’s Disease (Talus AVN) Pump Bump (Bursitis at tendoachilles attachment) Freiburg's Infraction (AVN of 2nd MT head) Van Neck's Disease (normal appearance in ischiopubic fusion) 11 Upper Extremity Disorders Klippel Feil Syndrome Failure of segmentation of upper cervical spine Triad (seen <50%): Low hairline, Decreased ROM, Short neck X-Rays: look for omovertebral bone connecting spinous process to scapula Associated findings: 1. Scoliosis-congenital (60%) 4. Hearing (30%) 2. Sprengel's (40%) 5. Synkinesia (18%) mirror-like movements 3. Renal (35%) 6. Heart (14%) Torticollis Associations: DDH (20%) Tx: Release before 5-6 yo (Ocular righting reflex) Acquired must r/o; AA rotatory subluxation Posterior fossa tumors Spinal canal tumors Retropharyngeal abscess Sprengel's Deformity Failure of scapular descent (normal C4 to T7) Sx: Cosmesis, Decreased ROM Associations: Scoliosis (Klippel-Feil), Torticollis, Hairlip, Renal disorders Tx: most common complication is brachial plexopathy => clavicle ostectomy/morcelization to avoid Woodward: Muscular release at spinous processes Green: Muscular release at scapula.....Brought down.....Secured Clavicle Pseudarthrosis Location: Right side (Think dextrocardia if on left side) Congenital Fusion of Elbow (Boomerang Elbow) Association: Idiopathic scoliosis Congenital Radioulnar Synostosis No limits in function Radial Clubhand Autosomal dominant (~1/100,000) Classification (Bayne) -- (SHIT) I. Short radius---Short II. Hypoplastic radius---Hypoplastic III. Partial absence---Isn't all there IV. Total absence (most common)---Totally not there Absence of radial artery and nerve, absent distal biceps tendon Associations: TAR (Thrombocytopenia, Absent Radius) Holt-Oram (cardiac septal defects) Fanconi syndrome (aplastic anemia) VATER (Vertebral, Anal atresia, Tracheo-Esophogeal, Radial) VACTERLS (Vertebral, Anal, Cardiac, Tracheo-Esoph., Renal, Limb def, Single umbilical artery) Treatment: Bora- soft tissue release with realignment over ulna Delorme centralization procedure- metallic rod to stabilize hand over ulna Madelung's Deformity Prominence of distal ulna, abnormal ulnar aspect of distal radial physis Types: 1. Congenital: Triangulation of proximal carpals F>M, Usually bilateral 2. Traumatic: due to distal radius fx--volar/ulnar physis growth cessation, no triangulation 12 Scoliosis Non-Structural Etiology: LLD, hip flexion contractures, neuromuscular imbalance, postural Flexible on bending films, correct with supine films Structural WAR: Wedging, Angulation, Rotation Treat WARP: Wedging, Angulation, Rotation, Progression 1. Idiopathic Epidemiology: 8-11% of children 10-13 yo 0.3% require treatment, 0.03% require surgery Family Hx (Risk): Mom (10x), Mom + older sister (20x), Older sister (<50x), Both parents (80x) Complications: cosmesis, pain, neurologic, cardiopulmonary (if apex above diaphragm) Cardiopulmonary: >100-110 -Correction: No change in tidal volumes; V-Q ratio, oxygenation improved -Thoracic lordosis: Early decompensation, Mitral valve prolapse Types: Infantile (0-3 yrs), Juvenile (3-10 yrs), Adolescent (10-maturity) Infantile: Great Britain, Left thoracic curves, RVAD < 20 good prognosis Vertebral maturity: Fusing of vertebral apophysis (best indicator) Curve patterns: 1. Right thoracic (most common) [Worst cosmesis] 2. Thoracolumbar (second most common) 3. Lumbar curve 4. Double primary (R thoracic, L lumbar) [Best cosmesis] Milwaukee brace -Indications: Curve <33 degrees, Progressive, Skeletal immaturity -Contraindications: Curves >40-45, Thoracic lordosis, Psych probs, Poor cosmesis Surgery >45 degrees, Progressive Spinal Cord Monitoring Risk of progression: 1. SSEP 1. Lonstein table 2. MEP Curve 5-19 20-29 3. EMG Risser 0,1 22% 68% 4. Stagnara wake-up test 2,3,4 1.6% 23% 2. Weinstein table 10-12 yo 13-15 yo >16 yo <19 degrees 25% 10% 0% 20-29 deg 60% 40% 10% 30-59 deg 90% 70% 30% 60 deg 100% 90% 70% Kings Classification: 5 distinct idiopathic thoracic curve patterns I. L>T: T more flexible II. T>L: L more flexible, L must cross midline III. T-L curve: L doesnt cross midline, apex usually at T 7/8, fuse L 1/2 IV. Long T curve: L4 points into curve, L5 balanced over sacrum V. Double thoracic curve (not double major!) T1 tilts into concavity, elevation of left shoulder Surgery tips: Fuse primary curve only Fuse neutral (not rotated) to neutral vertebrae (Moe) Lowest vertebrae fused must also be stable (centered over lumbosacral junction) Avoid L4 and L5 when possible 13 2. Congenital Etiology: Failure of Segmentation (bar) vs Formation (hemivertebrae) Most progressive: 1. Unilateral unsegmented bar (Most malignant) 2. Multiple unilateral hemivertebrae 3. Unsegmented bar with convex hemivertebrae 4. Hemivertebrae w/ kyphosis Anomalous takeoff: congenital element at LS junction with compensatory curve above 3. Neuromuscular Treatment: Fuse to sacrum (Bracing not effective) Indications: 1. Cosmesis 2. Pain prevention 3. Improve pulmonary function 4. Improve function 5. Improve nursing -Curve >50 degrees in standers, >30 degrees in sitters 4. Mesenchymal Morquio’s, Marfan’s, AMC, Dwarfs, OI, Scheuermann’s Myelodysplasia -Fuse to sacrum (high incidence of infection, pseudarthrosis) => may stop walking -Hydromyelia: Suspect if sudden worsening curve 5. Neurofibromatosis -Short segments, Sharply angulated Types: 1. Dysplastic (Pseudarthrosis common after fusion-17%) -Wedging, Rotation of apical vertebrae, Scalloping of vert bodies, Spindling of transverse processes, Enlarged foramina, Pencil ribs 2. Idiopathic 3. Kyphosis: >50 degrees.....Fuse anterior and posterior -Pseudarthrosis common 6. Trauma 7. Miscellaneous post radiation Kyphosis: normal is 20-40, measure from T3-T12 on lateral Scheurman's Kyphosis Def: >3 successive vertebrae with >5 degrees wedging (Sorenson's rule) Fixed deformity at puberty Treatment: -Four 6's (Curves < 60) 1. 6 weeks - Risser 2. 6 months - Milwaukee Brace 3. 6 weeks - Wean (8 hours out per day) 4. 6 months - Nighttime brace -Surgery 1. Kyphosis >70 deg 2. Wedging >10 deg 3. Pain 4. Neurologic findings 5. Progressive deformity 14 Juvenile Roundback Flexible, treatment is postural exercises Congenital Kyphosis Types: I. Failure of formation II. Failure of segmentation III. Mixed Treatment: Early PSF (<3 yo if rapidly progressive) Halo-femoral traction contraindicated => high risk of paralysis Spondylolysis/Spondolisthesis Population: gymnasts, football players, weight-lifters, divers, eskimo’s (Never in non-ambulators) Sx: Low back/buttock/thigh pain, Tight hams, Waddling gait, Neuro findings Etiology: Hammer (Inf. facet of L4), Anvil (Sup. sacral facet) creates fx/defect in pars interarticularis (usually L5) Classification (Wiltse-Newman-Macnab 1976) Classification of degree of slip (Meyerding): I. Dysplastic (Congenital, 94% Spina bifida occulta) Grade I: 0-25% II. Isthmic (elongated pars) Grade II: 25-50% III. Traumatic Grade III: 50-75% IV. Degenerative Grade IV: 75-100% V. Pathologic Grade V: >100% => spondyloptosis Anatomy (Scotty Dog): x-ray = Napolean’s hat sign Face: Transverse process Body: lamina Eye: Pedicle Front leg: Inferior facet Ear: Superior facet Hind leg: Transverse process Neck: Pars interarticularis Tail: Spinous process Nerve root involvement: Isthmic type – L5, Dysplastic type – S1 Diastematomyelia Epidemiology: F:M 4:1, lesion of spinal column which protrudes from posterior midline dividing cord (usually L1L3) Suspicion: 1. Congenital scoliosis 2. Neuromuscular Def (Neuro. bladder, Gait abnorm., Uni. Clubfoot / Cavus / Flatfoot) 3. Cutaneous abnormality – hairy patch 4. X-Ray: Widened inter-pedicular distance Midline spike Narrow disk space Myelomeningocele Level: Lowest root level of active muscle Increased incidence of latex allergy and UTI Ambulatory status (Hoffer): Community Household Non-functional (In gym/PT only) Non-walker Factors affecting ambulation 1. Extent of paralysis 5. Hydrocephalus 2. Spinal deformity 6. Intelligence 3. Hip instability 7. Home environment 4. Obesity Foot: Hip: Valgus deformity often truly ankle valgus (get AP of ankle if fib physis above mortise = ankle valgus) Must have strong quads (lesion L3 or lower) before surgically address hip dislocation Surgery: External oblique transfer to greater trochanter => improves sitting balance, trunk stability Mustard: Iliopsoas transfer through anterior ilium notch to greater troch 15 (Increased abductor power) Sharrard: Iliopsoas transfer through post-medial ilium to greater troch (Increased abductor & extensor power) Lower extremity management < 2 yo: Stretching No surgery until able to sit independently >2 yo: Put in standing braces when able to sit independently Spine: 80% have scoliosis consider ant/post fuse to sacrum Galveston: rods between inner/outer tables Warner: through S1 foramen Dunn/McCarthy: place bars over sacrum anteriorly Sacral Agenesis Mother always has insulin dependent diabetes mellitus Types: Renshaw classification (Type 2 most common) 1. Partial or total unilateral absence of sacral elements 2. Complete loss of lower sacral/coccygeal elements, stable articulation between ilia 3. L5/S1 non-union, no sacrum, ilia articulate with the sides of the lowest vertebra present 4. No L5/S1 junction, no sacrum, caudal end plate of the lowest vertebra fused to ilia or an iliac amphiarthrosis Muscular Dystrophy Duchennes Features: 1. 2. 3. 4. 5. 6. Age 2-7, stop walking avg. 8-10yo Sex-linked recessive Clumsy gait (Gowers sign - use hands to stand up from floor) Pseudohypertrophy of calves – 80% of patients Weak proximal muscle masses (Shoulder and Pelvic girdle muscles affected first) Hip flexion, Iliotibial band/Tensor fascia, knee flexion, foot plantar flexion contractures [Hip and knee extension lag test: >90 deg contracture then release] 7. Lumbar lordosis (Protuberant abdomen) 8. Posterior tib. tendon tends to retain power over long period of time Histology: (Do not biopsy at previous EMG site) 1. Muscle fibers vary in size 2. Central nuclei 3. Signet ring (infiltration of fat), Chicken-wire fence [End stage disease] Functional Assessment Scale (10 parts, based on walking, stair climbing...) Scoliosis 16 Types: 1. J-type: Most common, Windswept hips 2. Z-type: Pelvis OK, Translation at L-S junction Treatment: Surgery if curve >30 deg in sitter (May cease walking) Becker's 5. Tend to live longer Sx: Chest protuberance, Scapular winging, Calf hypertrophy Spinal Muscular Atrophy (Auto Recessive) Anterior horn cell degeneration Classification: I. Infantile (<12 mos), Oppenheimers Dz, Floppy Baby, no sit or walk, die ~4 yo II. Intermediate (3-18 mos), Werding-Hoffmans, sit OK, no walk, live >4 yo III. Juvenile (>2 yo), “Kugleburg-Weidlander”, can sit w/ support, may walk, live to adult Fascioscapulohumeral Dystrophy (Landouze-Dejerine MD) Autosomal Dominant Findings: 1. Upper extremity weakness 2. Scapular winging 3. Increased trapezius mass 4. Popeye forearms 5. Can't blow up balloon, puff cheeks, purse lips, or whistle deltoids usually spared Dwarfism Achondroplastic Dwarfism Characteristics: 1. Short stature 2. Paddle-shaped ribs 3. Alphabet block vertebrae 4. Narrowed inter-pedicular space 5. Lumbar kyphosis 6. Horizontal sacrum 7. Genu varum 8. Coxa valga 9. Trident hands 10. Frontal bossing 11. Saddle shaped nose 12. Short mid-face Pseudo-achondroplasia Characteristics: 1. Short limb 5. Odontoid hyperplasia 2. Normal head 6. Epiphysis and Metaphysis affected 3. Flame vertebra (platyspondyly) 7. Joint hyperlaxity 4. Normal interpedicular distance 17 Ellis van Crevald Characteristics: 1. Short stature 2. Poor dentition 3. 6 digit hands 4. Immunodeficiencies Diastrophic Dwarfism Characteristics 1. Short limbs 2. Scoliosis 3. Hitchiker thumb – short 1st metacarpal 4. Cauliflower ears 5. Equinovarus 6. Flexion contractures 7. Usually distal femoral epiphysis not ossified at birth Metabolic Disorders Osteopetrosis (Marble-bone Disease, Marie-Alber-Schoenberg Dz) Osteoclast disorder, don’t respond to PTH tx. X-ray: Erlenmeyer flask, Rugger jersey spine Associations: Anemia, Immunodeficiency => BMT to cure Rickets Types: 1. Vitamin D Deficient (Dietary rickets) -Rare -Age 6 mos - 3 yrs -Low Vit D > Decr Ca, PO4 absorption > Incr PTH (Low-nl Ca, Low PO4) -Associations: Prematurity, Hyperalimentation, Anti-convulsants (Compete with Vit D uptake) -Sx: Weakness, Lethargy, Bowlegs, Protuberant abdomen, Cranio tabes (large forehead), Rachitic rosary (large osteochondral rib articulation) -Tx: Vit D, Calcium 2. Vitamin D Resistant (Renal tubular insufficiency, Familial hypophosphatemic rickets) -X-linked dominant (F:M.....2:1) 18 -Impaired renal reabsorption of PO4 (GFR normal) > Low PO4, Nl Ca, incr alkphos -Impaired response to Vitamin D -Sx: Bowing, Frontal bossing, Incr lumbar lordosis, Poor teeth, Short -Tx: Phospate, Vitamin D3 (High dose, Stop before surgery) 3. Renal Insufficiency (Chronic renal failure) -tx = high dose Vit D, dialysis => kid txp X-Ray: Widened physis Metaphyseal flaring (Trumpeting) Physeal cupping, Serrated metaphyseal edge Loosers lines (Fracture on compression side of bone) Milkmans fracture (Pseudofracture) Osteogenesis Imperfecta Defect in collagen synthesis – Type 1 collagen-(alpha 2) Classification (Sillence): I. AD, Blue sclera, hearing loss, most common, most mild (Familial) IA. Dentinogenesis absent IB. Dentinogenesis present II. AR or AD, Blue sclera (perinatal fatality) III. AR, Normal sclera, fractures at birth, progressive and deforming (Auto Recessive) IV. AD, Normal sclera, bowing of long bones, improves at puberty, normal hearing (Sporadic) IVA: nl teeth IVB: Dentinogenesis imperfecta Surgery: Sofield-Miller (Shish-kebob) Correct scoliosis if curve > 45, use PMMA to augment and segmental fusion techniques Increased risk for malignant hyperthermia Ehlers-Danlos Syndrome Defect in collagen metabolism Sx: Skin hyperextensibility (Cigarette paper skin), Joint hypermobility, Bruisability, Soft tissue calcification, Bone fragility, Bursa formation, Osteopenia Many types Mucopolysaccharidosis Features: 1. Proportionate short stature 2. Anterior beaking of vertebrae (platyspondyly) 3. Bullet-shaped metacarpals 4. Wide pelvis Types: 1. Hunter 2. Hurler 3. Morquio 4. San-Filippo 5. Scheie 6. Maroteaux-Lamy 7. Sly Hypothyroidism Congenital (Cretinism) F>M Dwarfism, Mental retardation, Osteopatia cretinoidia (~Perthes) Acquired SCFE Scurvy Age 6-12 mos Sx: Decr appetite, Slow wt gain, Bleeding gums, Subperiosteal hemorrhage X-Ray: Wimbergers ring (density around cartilaginous ossific nucleus) [Subperiosteal hemorrhage Differential: Scurvy, Menkes Kinky Hair Syndrome, Abuse, Neglect] 19 Wormian bones C leidocranial dysostosis – retarded ossification of membranous as well as cartilaginous precursors of bone. Congenital absence of clavicles combined with softness of the calvarium. H ypothyroidism O steogenesis Imperfecta M einkes Kinky Hair Syndrome P yknodysostosis – form of osteopetrosis showing short stature, separated cranial sutures, delayed closure of fontanelles and hypoplasia of the terminal phalanges. Helmet Heads O.I. Frontometaphyseal Dysplasia Dentoagenesis Neurofibromatosis: Tumors of neural crest/mesodermal origin Types: 1. NF-1 (von Recklinghausen, Peripheral NF) => chromosome 17- (long arm) 2. NF-2 (Central NF, Acoustic neuroma) => chromosome 22 Diagnosis for NF1: (2 out of 7) 1. Cafe-au-lait spots: Five >5mm (child), Six > 1.5cm (adult) 2. Neurofibroma (2) or Plexiform (1) 3. Freckles (axillary, groin)-Crowe Sign 4. Osseous lesions- sphenoid dysplasia or thinning of cortex of a long bone (+/- pseudarthrosis) 5. Optic glioma 6. Lisch nodules 7. Primary relative with NF Findings: 1. Spinal deformity (Scoliosis, Kyphosis, or both) 23.6% of patients (Most common bone abnormality) Short segmented, Sharply angulated 2. Tibial pseudarthrosis (congenital tibial dysplasia): Antero-lateral bow-5.7% Types I: Dense cortex, Canal OK [Observe] IIA: Failure of tubulation [Brace] IIB: Cystic lesion or pre-fracture [Bone graft] IIC: Frank Fracture- “sucked candy” appearance of bone[Bone graft +/- Amputate] Other Classifications of congenital pseudarthrosis of the tibia: Incidence 1/190,000 M>F Boyd Anderson 20 I. Fx present at birth II. Hourglass constriction Dysplastic III. Bone cysts Cystic IV. Sclerotic segment Sclerotic V. Dysplastic fibula Fibular VI. Intra-osseous NF Clubfoot or congenital band type 3. Hemihypertrophy - 1.4%(Subperiosteal bone proliferation) 4. Bone erosions: Secondary to pressure from neurofibroma (Dumbell lesion in vertebrae) 5. Neoplasias (Leukemia, Wilms tumor, Rhabdomyosarcoma (UG tract)) 6. Pectus deformity – 4.3% 7. Plexiform neurofibroma 25% 8. LLD – 7.1% Diagnosis for NF2: (need 1) 1. Bilateral CN VIII neuromas 2. 1 relative with NF2 Gait Determinants of Gait: 1. Pelvic rotation 2. Pelvic tilt 3. Knee flexion after heel strike in stance 4. Foot and ankle motion 5. Knee motion 6. Lateral Displacement of Pelvis Limb Lengthening Indication: 8-12 yo, Discrepancy > 4cm Wagner: open corticotomy, distract, plate, bring back later and bone graft Ilizarov: perc corticotomy (don’t violate medullary canal), ring fixator, wait 5-7 days, distract 1mm/day De Bastiani; same as Ilizarov, except use unilateral ex-fix (OrthoFix) Tumor Epidemiology: Benign - 3 most common -> UBC, Osteochondroma, NOF Malignant - 3 most common -> Osteosarcoma > Ewings > Rhabdomyosarcoma Work-up: H&P, X-Ray, Bone scan, CT, MRI, Angiogram, Lung CT Enneking Staging 5 yr Survival IA Low grade Intra-comp No mets 97% IB Low grade Extra-comp No mets 89% IIA High grade Intra-comp No mets 73% IIB High grade Extra-comp No mets 45% III Mets 8% Osteochondroma: Most common tumor--failure of differentiation/tubulation at prox metaphysis Multiple hereditary exostosis (Ehrenfried’s Dz) Autosomal dominant Short stature X-ray: trabeculae flow into lesion, lesions point away from physis Tx: Excise if - Limit ROM, Pain, Neurovascular compromise Malignant degeneration: 5-15% Enchondroma Unilateral, Monomelic Olliers Dz (Multiple enchondroma)--Maffucis Syndrome (Ollier's+Hemangioma->risk of malignancy) Unicameral Bone Cyst--usually in proximal humerus (fallen leaf sign) 21 Type: Active (w/in 1 cm of physis), Latent (>1cm from physis) Tx: Aspiration, Steroid injection (Scaglietti), possible Nancy nail Aneurysmal Bone Cyst Multiple loculations with septa X-Ray: Cyst is wider than metaphysis Histo: vascular lakes, with giant cell laden epithelized septa Osteoid Osteoma--common in prox fem metaphysis (calcar), and posterior elements of the spine Pea in a pod” sclerotic nidus <1cm Symptoms: night pain relieved by ASA, exacerbated by EtOH Histiocytosis (EG) EG of spine - Vertebrae plana (platyspondyly) aka Calves vertebrae Hans-Schuller-Christian Dz: Histiocytosis, Skin & Bone...., Pituitary (DI, Exophthalmos) Letterer-Siwe Dz: HSC Dz w/ MR, Cystic manifestations Fibrous Dysplasia Failure of complete remodeling of immature bone, Shepherd’s Crook in prox femur Cafe-au-lait spots: Coast of Maine [Neurofibromatosis: Coast of California] Albrights Syndrome: 1. Fibrous dysplasia (“Shepherds crook” deformity if in hip) + 2. Endocrinopathies (precocious puberty) + 3. Cafe-au-lait spots Ewings Age 10-30 yo Sx: Pain, Mass, Tenderness, Systemic sx (fever) Location: Diaphyseal, Femur #1, in pts >20yo, flat bones more common X-Ray: Onion skinning due to periosteum trying to wall off soft tissue expansion Histo: + PAS, monotonous sheets of round cells Osteosarcoma Sx: Swelling, Tenderness, Decr ROM, Warmth, Pathologic fx Differential Dx: Infection, Ewings, Metabolic disease, Traumatic, Congenital lesion Chemo: MAP: methotrexate, adriamycin, platinum) OR COMPAdra: cytoxin, O(vincristine), methotrexate, prednisone, adriamycin COMMON IN THE SPINE--ant elements: EG, Hemangioma post elements:Osteoid Osteoma, Osteoblastoma, ABC Growth Plate Zones: Resting - Lipid/glycogen/proteoglycan production, Low oxygen tension - Lysosomal storage diseases Proliferative -Align longitudinally, Chondrocytes multiply, Linear growth -Achondroplasia Hypertrophic -Cells increase 5x, Matrix preparation, Calcification -Rickets, Enchondromas, Mucopolysaccharidosis, Fractures Maturation Degeneration Provisional Calcification Most common fractures: SH I Distal fibula SH II Distal radius SH III Distal tibia SH IV Distal femur Growth: Lower Extremity: Proximal femur 10 Distal femur 40 Proximal tibia 30 Distal tibia 20 Individual Bones: Prox. Humerus 22 80% Prox. Femur 30% Dist. Humerus Prox. Radius Dist. Radius Prox. Ulna Dist. Ulna 20 25 75 20 75 Ossification sequences: Ankle: Middle (at Poland’s hump), Medial, Lateral Elbow: Appearance: Come Rub My Tool Of Love Capitellum 6 months Radial head 2 yrs Medial epicondyle 4 Trochlea 6 Olecranon 8 Lateral epicondyle 10 Dist. Femur Prox. Tibia Dist. Tibia Prox. Fibula Dist. Fibula 70 57 43 60 40 Closure: TLC OR ME Trochlea Lateral epicondyle Capitellum 13 yrs Olecranon Radial head 15 yrs Medial Epicondyle 17 yrs Epiphyseal Centers present at birth: Full Term Children Have These Centers 1. Distal femur 2. Proximal tibia 3. Calcaneous 4. Proximal humerus 5. Talus 6. Cuboid Hemoglobinopathies (Sickle Cell Disease) Sx: Small size (due to persistent anemia, or decr O2 at growth plate) Osseous manifestations: 1. Marrow hyperplasia 2. Infarction 3. Growth disturbances 4. Osteomyelitis 5. Pathologic fracture X-Ray: Vertebrae - Most common involved bone, Cup-like biconcavity in central endplate -Step-deformity Skull - Thick cortex, Widened diploe, Porcupine quill, Hair-on-end Joints - Bone crisis, Bone infarcts Hip: AVN, Osteochondritis, Coxa vara Differential Dx: Perthes (SS = Older [age > 10yo], Black) Chung/Ralston classification Group 1: Total head involvement ~ Perthes Group 2: Localized involvement ~ OCD Group 3: Late changes Hand-Foot Syndrome Age < 2yo Sx: Painful soft tissue swelling of hands/feet X-Ray: Periosteal new bone, Lytic lesions Osteomyelitis Sx: ~ Bone crisis 23 Organism: Salmonella Juvenile Rheumatoid Arthritis (Stills Disease) Sx: Fever, Rash, Anemia, Splenomegaly, Multiple joint involvement Age: < 6yo, 10-15 yo Dx: Synovitis of joint (Knee, ankle, elbow, wrist) > 6 weeks Types: Monoarticular, Pauciarticular (2-4 joints), Polyarticular (>4 joints) Septic Arthritis Epidemiology: Age 1-3yo Organisms: Staph A., Streptococcus, Pneumococcus, H. flu (#1 <6 mo) Diagnosis: Joint fluid (Incr WBC [>35,000], Inc protein, Dec glucose[40 < blood Glc]) Diff Dx (Septic hip): 1. Osteomyelitis 4. Iliopsoas abscess 7. Perthes 2. Toxic synovitis 5. JRA 3. Diskitis 6. Rheumatic fever Sequelae (Septic hip): 1. Dislocation of hip 4. Coxa magna 2. Osteomyelitis of fem neck 5. Coxa vara 3. AVN 6. Leg length discrepancy Poor Prognosis: 1. Delay in diagnosis (>5 days) 2. Hip joint 3. Associated osteomyelitis 4. Younger age (diagnosis difficult in infants) Osteomyelitis Seasonal (Spring, Fall) Etiology: 1. Hematogenous 2. Direct extension 3. External 24 Organisms: Staph A., H. Flu (infants), Salmonella (Sickle cell) Location: Femur > Tibia > Humerus Metaphysis (Sludging of blood flow in sinusoidal vessels) Differential Diagnosis: 1. Septic arthritis 5. Blood dyscrasias 2. Cellulitis 6. Tumor 3. Syphilis 7. Hypervitaminosis A 4. Sickle cell crisis 8. Caffes Dz (Infantile cortical hyperostosis) X-Ray: 7-10 days: Soft tissue swelling > 10 days: Lucency or Opacity Sequestrum (localized area of dead bone) & Involucrum (periosteal new bone formation) Complications: 1. Bone overgrowth 2. Growth Arrest 3. Pathologic Fracture 4. Amyloidosis 5. Epidermoid Carcinoma Treatment: 3 weeks IV ABX, then PO ABX until ESR returns to normal; Immobilization -Sickle cell pts: Serial aspirations (No I&D due to risk of Staph wound infxn) Diskitis Sx: Refusal to walk (<3 yo), Abdominal pain (3-9 yo), Back pain (>9 yo) X-Ray: Crosses disk space THIS FILE SAVED IN MICROSOFT WORD UNDER PEDIATRIC ORTHOPAEDIC REVIEW Please continue to add and update this document. Last revised 7/02 25