approved
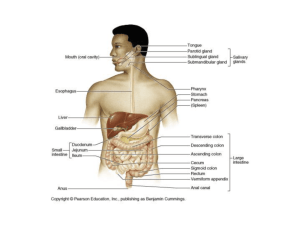
advertisement
Ministry of Health of Ukraine BUKOVINIAN STATE MEDICAL UNIVERSITY “APPROVED” on methodical meeting of the Department of Anatomy, Topographical anatomy and Operative Surgery “………”…………………….2008 р. (Protocol №……….) The chief of department professor ……………………….……Yu.T.Achtemiichuk “………”…………………….2008 р. METHODICAL GUIDELINES for the 2nd-year foreign students of English-spoken groups of the Medical Faculty (speciality “General medicine”) for independent work during the preparation to practical studies THE THEME OF STUDIES “Topographical anatomy of the peritoneum and their derivatives. The revision of the peritoneal cavity” MODULE I Topographical Anatomy and Operative Surgery of the Head, Neck, Thorax and Abdomen Semantic module 3 “Topographical Anatomy and Operative Surgery of the Abdomen” Chernivtsi – 2008 1. Actuality of theme: The topographical anatomy and operative surgery of the abdomen are very importance, because without the knowledge about peculiarities and variants of structure, form, location and mutual location of abdominal anatomical structures, their age-specific it is impossible to diagnose in a proper time and correctly and to prescribe a necessary treatment to the patient. Surgeons usually pay much attention to the topographo-anatomic basis of surgical operations on the abdomen. 2. Duration of studies: 2 working hours. 3. Objectives (concrete purposes): To know the definition of regions of the abdomen. To know classification of surgical operations on the abdomen. To know the topographical anatomy and operative surgery of the organs of the abdomenal cavity. 4. Basic knowledges, abilities, skills, that necessary for the study themes (interdisciplinary integration): The names of previous disciplines 1. Normal anatomy 2. Physiology 3. Biophysics The got skills To describe the structure and function of the different organs of the human body, to determine projectors and landmarks of the anatomical structures. To understand the basic physical principles of using medical equipment and instruments. 5. Advices to the student. 5.1. Table of contents of the theme: The peritoneum is a thin, transparent serous membrane that consists of two layers. The peritoneum lining the abdominal wall is called parietal peritoneum, whereas the peritoneum investing the viscera is called visceral peritoneum. Both types of peritoneum consist of a single layer of squamous epithelium called mesothelium. The parietal and visceral layers of peritoneum are separated from each other by a capillary film of peritoneal fluid. This serous fluid lubricates the peritoneal surfaces, enabling the viscera to move on each other without friction. Some organs such as the kidneys protrude only slightly; they are called retroperitoneal organs. Other organs, such as the ascending colon, protrude further into the peritoneal sac and are covered on each side with peritoneum. Organs such as the stomach and jejunum protrude completely into the peritoneal sac and are completely covered with visceral peritoneum. The peritoneum forms the serosa of the walls of these organs. They are also attached to the posterior abdominal wall by two apposed layers of peritoneum, called a mesentery. The peritoneal cavity is divided into two peritoneal sacs, the greater and lesser sacs of peritoneum. A surgical incision through the anterior abdominal wall enters the greater peritoneal sac. The lesser sac, known as the omental bursa, lies posterior to the stomach, lesser omentum, and liver). The peritoneal cavity is closed in males, but in females there is communication with the exterior through the uterine tubes, uterus, and vagina. Mesentery. This is a double layer of peritoneum that encloses an organ and connects it to the abdominal wall. Mesenteries have a core of loose connective tissue containing a variable number of fat cells and lymph nodes, together with vessels and nerves passing to and from the viscus. Omentum. This is a double-layered sheet or fold of peritoneum. The lesser omentum and the greater omentum attach the stomach to the body wall or to other abdominal organs. The Greater Omentum. This fat-laden fold of peritoneum hangs down from the greater curvature of the stomach and connects the stomach with the diaphragm, spleen, and transverse colon. The Lesser Omentum. This fold of peritoneum connects the lesser curvature of the stomach and the proximal part of the duodenum to the liver. Individually these connections are referred to as the hepatogastric ligament and the hepatoduodenal ligament. Peritoneal Ligament. A peritoneal ligament is a double layer of peritoneum that connects an organ (e.g., the liver) with another organ or with the abdominal wall. Ligaments may contain blood vessels or remnants of vessels (e.g., the falciform ligament contains the ligamentum teres, a remnant of the fetal umbilical vein). For descriptive purposes, the greater omentum is divided into three parts: (1) The apronlike part, called the gastrocolic ligament, is attached to the transverse colon: (2) the left part, called the gastrosplenic ligament (gastrolienal ligament), is attached to the spleen (G. splen) and connects the spleen to the greater curvature of the stomach; and (3) the superior part, called the gastrophrenic ligament, is attached to the diaphragm (G. phren). Peritoneal Folds. A peritoneal fold (L. plica) is a reflection of peritoneum with more or less sharp borders. Often it is formed by peritoneum that covers blood vessels, ducts. and obliterated fetal vessels (e.g., the medial and lateral umbilical folds). Peritoneal Recesses. In certain places the peritoneum folds to form blind pouches (cul-desacs) or tubular cavities that are closed at one end with an opening into the peritoneal cavity. The duodenojejunal area often has two or three peritoneal recesses. In the ileocecal area there is a retrocecal recess where the peritoneal cavity extends superiorly, posterior to the cecum. Frequently the vermiform appendix lies in this recess. Subdivisions of the Peritoneal Cavity The transverse colon and transverse mesocolon, forms a shelf that subdivides the peritoneal cavity into supracolic and infracolic compartments. The Supracolic Compartment. This compartment is divided into smaller parts or spaces by the falciform ligament. The right and left anterior subphrenic recesses are located between the inferior surface of the diaphragm and the superior surfaces of the right and left lobes of the liver. The hepatorenal recess is located between the inferior surface of the right lobe of the liver and the right kidney. The Infracolic Compartment. This compartment is divided into right and left infracolic spaces by the mesentery of the small intestine. Owing to the obliquity of the mesentery, the right infracolic space is superior and to the right and the left infracolic space is inferior and to the left. Related to the ascending and descending colon are longitudinal depressions or channels, called paracolic gutters or grooves. There are medial and lateral paracolic gutters on the right (associated with the ascending colon) and the left (associated with the descending colon). The right lateral paracolic gutter is of particular surgical significance because it is continuous superiorly with the hepatorenal recess, and beyond this with the omental bursa and its superior recess. Inferiorly this gutter is continuous with the rectovesical pouch in the male and the rectouterine pouch in the female. On each side of the vertebral column is a.paravertebral gutter or groove containing a kidney, a ureter, and a part of the colon. The paracolic gutters or grooves slope posterosuperiorly so that when fluid accumulates in the peritoneal cavity, it follows these gutters to the superior part of the abdomen when a person is in the supine position. The greater omentum prevents the visceral peritoneum covering the intestine from adhering to the parietal peritoneum lining the anterior abdominal wall. It has considerable mobility and can migrate to any area of the abdomen and wrap itself around an inflamed organ such as the appendix. Because it "walls off" and protects an infected organ from other viscera, it has been called the "policeman of the abdomen''. The division of the peritoneal cavity into peritoneal recesses is of clinical importance in connection with the spread of pathological fluids (e.g., pus). The subdivisions determine the extent and direction of the spread of fluids (e.g., blood), which may be present in the peritoneal cavity when an organ is diseased or injured. Normally these recesses are in communication with each other, but they may become separated from each other by adhesions between the peritoneum and viscera. The Omental Bursa The omental bursa (lesser sac of peritoneum) is the large compartment or recess of the peritoneal cavity that is located between the stomach and the posterior abdominal wall. The omental bursa is also located posterior to the lesser omentum and the stomach. As the anterior and posterior walls of the bursa slide smoothly on each other, the omental bursa gives considerable movement to the stomach, permitting it to slide freely on the bursa during contraction and distention. The omental bursa is an extension of the main peritoneal cavity into the invaginated right side of the dorsal mesentery of the stomach (gastric mesentery). The inferior extension of the omental bursa, called the inferior recess, is between the duplicated layers of the gastrocolic ligament of the greater omentum. In adults the inferior recess of the omental bursa is a potential space; it is usually shut off from the main part of the bursa owing to adhesion of the layers of the gastrocolic ligament. The omental bursa also has a superior recess, which is limited superiorly by the diaphragm and the posterior layers of the coronary ligament. The omental bursa is in communication with the main peritoneal cavity (greater sac of peritoneum) through the omental foramen (epiploic foramen or foramen of Winslow), located posterior to the free edge of the lesser omentum. The omental (epiploic) foramen is usually large enough to admit two digits. The Latin term omentum, meaning "fat skin," is widely used, whereas the Greek term epiploon for the omentum is unfamiliar to most people. Consequently the adjective "epiploic" has been replaced by "omental" in the current list of terms in Nomina Anatomica (Warwick, 1989). Therefore omental foramen is used instead of epiploic foramen. Similarly the gastroepiploic vessels are now known as the gastroomental vessels. It will take time to gain acceptance of these new terms because the old ones are firmly entrenched in the minds of both basic science and clinical teachers. Boundaries of the Omental Foramen. The boundaries of the omental foramen are the following: anteriorly, the portal vein, hepatic artery, and bile duct (all in the free edge of the lesser omentum); posteriorly, the inferior vena cava and right crus of the diaphragm; superiorly, the caudate lobe of the liver; and inferiorly, the superior part of the duodenum, portal vein, hepatic artery, and bile duct. 5.2. Theoretical questions to studies: 1. The structure of the peritoneal cavity. 2. The leafs of the peritoneal cavity. 3. The Subdivisions of the Peritoneal Cavity 4. The Boundaries of the Omental Foramen. 5. The derivates of the peritoneum. 6. The mesenteries. 7. The Supracolic Compartment. 8. The Infracolic Compartment. 9. The Peritoneal Ligaments. 10.The spreading of exudate into the peritoneal cavity. 5.3. Materials for self-control: 1. Diffuse pain referred to the epigastric region and radiating circumferentially around the chest is the result of afferent fibers that travel via which of the following nerves? A B C D E 2. Greater splanchnic Intercostal Phrenic Vagus None of the above In the patient described, the subsequent localization of the pain in the right hypochondriac region is the result of inflammatory stimulation of fibers that are extensions of which of the following nerves? A B C D E Greater splanchnic Intercostal Phrenic Vagus None of the above 3. The patient receives a general anesthetic in preparation for a cholecystectomy. A right subcostal incision is made, which begins near the xiphoid process, runs along and immediately beneath the costal margin to the anterior axillary line, and transects the rectus abdominis muscle and rectus sheath. At the level of the transpyloric plane, the anterior wall of the sheath of the rectus abdominis muscle receives contributions from the A aponeuroses of the internal and external oblique muscles B aponeuroses of the transversus abdominis and internal oblique muscles C aponeuroses of the transversus abdominis and internal and external oblique muscles D transversalis fascia E transversalis fascia and aponeu-rosis of the transversus abdominis muscle 4. At this level of incision, liga-tion of the superior epigastric artery probably will result in little, if any, necrosis of the rectus abdominis muscle because the superior epigastric artery anastomoses with the A B C D E 5. deep circumflex iliac artery inferior epigastric artery intercostal arteries internal thoracic artery musculophrenic artery Exploration of the peritoneal cavity disclosed a distended gallbladder. It is located A B C D E between the left and caudate lobes of the liver between the right and quadrate lobes of the liver in the falciform ligament in the lesser omentum in the right anterior leaf of the coronary ligament 6. Numerous stones could be palpated. A finger was inserted into the omental foramen (of Winslow), and the common bile duct was palpated for stones. Structures that bound the omental foramen include all the following EXCEPT the A B C D E 7. caudate lobe of the liver common bile duct hepatic vein inferior vena cava superior part of the duodenum Before closure of the incision, it is felt that a drain should be left in place in the abdominal cavity so that any leakage of bile from the sutured stump or from inadvertent injury to the duct system can be detected. This drain would most advantageously be located in the A B C D E omental bursa pelvic cavity pouch of Morison right paracolic gutter right subphrenic recess Literature 1. Snell R.S. Clinical Anatomy for medical students. – Lippincott Williams & Wilkins, 2000. – 898 p. 2. Skandalakis J.E., Skandalakis P.N., Skandalakis L.J. Surgical Anatomy and Technique. – Springer, 1995. – 674 p. 3. Netter F.H. Atlas of human anatomy. – Ciba-Geigy Co., 1994. – 514 p. 4. Ellis H. Clinical Anatomy Arevision and applied anatomy for clinical students. – Blackwell publishing, 2006. – 439 p.