Document
advertisement
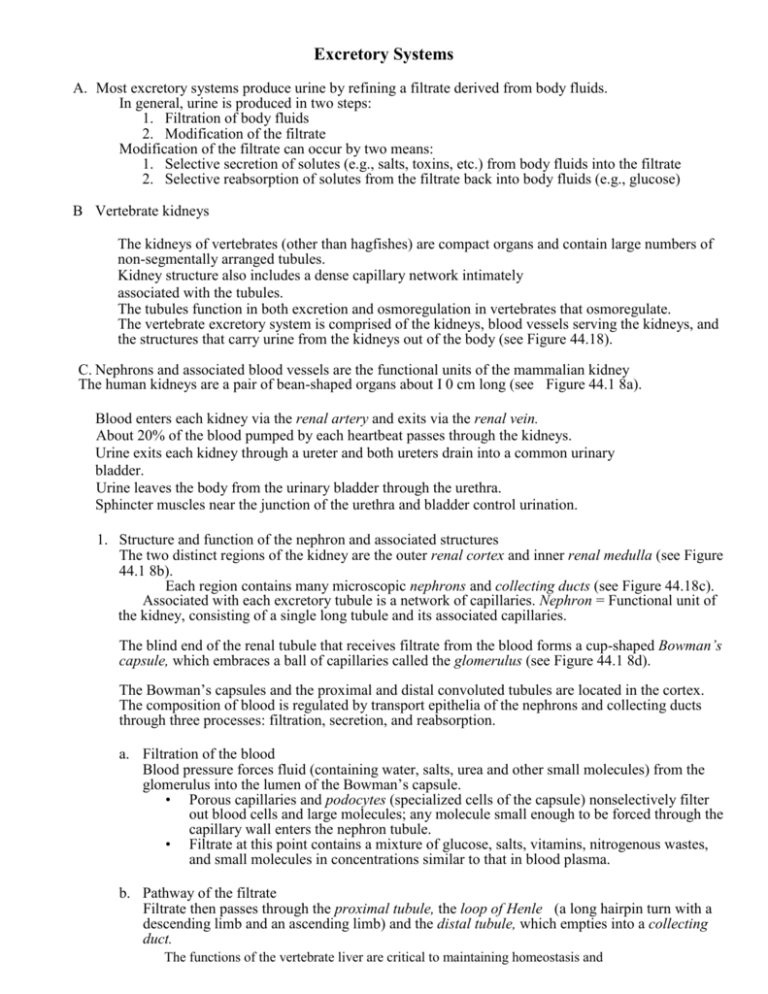
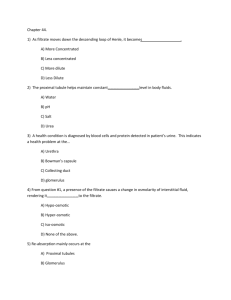
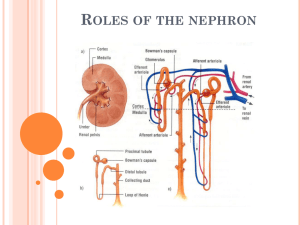
Excretory Systems A. Most excretory systems produce urine by refining a filtrate derived from body fluids. In general, urine is produced in two steps: 1. Filtration of body fluids 2. Modification of the filtrate Modification of the filtrate can occur by two means: 1. Selective secretion of solutes (e.g., salts, toxins, etc.) from body fluids into the filtrate 2. Selective reabsorption of solutes from the filtrate back into body fluids (e.g., glucose) B Vertebrate kidneys The kidneys of vertebrates (other than hagfishes) are compact organs and contain large numbers of non-segmentally arranged tubules. Kidney structure also includes a dense capillary network intimately associated with the tubules. The tubules function in both excretion and osmoregulation in vertebrates that osmoregulate. The vertebrate excretory system is comprised of the kidneys, blood vessels serving the kidneys, and the structures that carry urine from the kidneys out of the body (see Figure 44.18). C. Nephrons and associated blood vessels are the functional units of the mammalian kidney The human kidneys are a pair of bean-shaped organs about I 0 cm long (see Figure 44.1 8a). Blood enters each kidney via the renal artery and exits via the renal vein. About 20% of the blood pumped by each heartbeat passes through the kidneys. Urine exits each kidney through a ureter and both ureters drain into a common urinary bladder. Urine leaves the body from the urinary bladder through the urethra. Sphincter muscles near the junction of the urethra and bladder control urination. 1. Structure and function of the nephron and associated structures The two distinct regions of the kidney are the outer renal cortex and inner renal medulla (see Figure 44.1 8b). Each region contains many microscopic nephrons and collecting ducts (see Figure 44.18c). Associated with each excretory tubule is a network of capillaries. Nephron = Functional unit of the kidney, consisting of a single long tubule and its associated capillaries. The blind end of the renal tubule that receives filtrate from the blood forms a cup-shaped Bowman’s capsule, which embraces a ball of capillaries called the glomerulus (see Figure 44.1 8d). The Bowman’s capsules and the proximal and distal convoluted tubules are located in the cortex. The composition of blood is regulated by transport epithelia of the nephrons and collecting ducts through three processes: filtration, secretion, and reabsorption. a. Filtration of the blood Blood pressure forces fluid (containing water, salts, urea and other small molecules) from the glomerulus into the lumen of the Bowman’s capsule. • Porous capillaries and podocytes (specialized cells of the capsule) nonselectively filter out blood cells and large molecules; any molecule small enough to be forced through the capillary wall enters the nephron tubule. • Filtrate at this point contains a mixture of glucose, salts, vitamins, nitrogenous wastes, and small molecules in concentrations similar to that in blood plasma. b. Pathway of the filtrate Filtrate then passes through the proximal tubule, the loop of Henle (a long hairpin turn with a descending limb and an ascending limb) and the distal tubule, which empties into a collecting duct. The functions of the vertebrate liver are critical to maintaining homeostasis and • • The collecting duct receives filtrate from many nephrons. Filtrate, now called presumptive urine (further modification can occur in the bladder), flows from the collecting ducts into the renal pelvis. The presumptive urine then drains from the chamberlike pelvis into the ureter. Two types of nephrons are found in mammals and birds: cortical nephrons and juxtamedullary nephrons. • Cortical nephrons = Nephrons that have reduced loops of Henle and are confined to the renal cortex; 80% of the nephrons in humans are cortical nephrons • Juxtamedullary nephrons = Nephrons that have long loops that extend into the renal medulla; 20% of the nephrons are juxtamedullary nephrons (see Figure 44.1 8c). The nephron and collecting duct are lined by transport epithelium that processes the filtrate into urine. • About 1100 to 1200 L of blood flow through the human kidneys each day. • The nephrons process 180 L of filtrate per day, and the transport epithelium processes this filtrate to form the approximately 1.5 L urine excreted daily. • The rest of the filtrate is reabsorbed into the blood. c. Blood vessels associated with the nephrons Each nephron is closely associated with blood vessels: • Afferent arteriole is a branch of the renal artery that divides to form the capillaries of the glomemlus. • Efferent arteriole forms from the converging capillaries as they leave the glomerulus. This subdivides to form the peritubular capillaries which intermingle with the proximal and distal tubules. • Vasa recta is the capillary system branching downward from the peritubular capillaries that serves the loop of Henle. Materials are exchanged between capillaries and nephrons through interstitial fluids. d. Secretion Filtrate is joined by substances transported across the tubule epithelium from the surrounding interstitial fluid as it moves through the nephron tubule. • Adds plasma solutes to the filtrate. The proximal and distal tubules are the most common sites of secretion. Secretion is a very selective process involving both passive and active transport. • For example, controlled secretion of H+ ions helps maintain constant body fluid pH. e. Reabsorption Reabsorption is the selective transport of filtrate substances across the excretory tubule epithelium from the filtrate back to the interstitial fluid. • Reclaims small molecules essential to the body • Occurs in the proximal tubule, distal tubule, loop of Henle, and collecting duct • Nearly all sugar, vitamins, organic nutrients are reabsorbed. In mammals and birds, water is also reabsorbed. The composition of the filtrate is modified by selective secretion and reabsorption. • The concentration of beneficial substances in the filtrate is reduced as they are returned to the body. • The concentration of wastes and nonuseful substances is increased and excreted from the body. The kidneys are central to the process of homeostasis as they clear metabolic The functions of the vertebrate liver are critical to maintaining homeostasis and wastes from the blood and respond to body fluid imbalances. From blood to filtrate Reclamation of small molecules and water from the filtrate as it flows through the nephron and collecting duct converts the filtrate into urine (see Figure 44.19). 1. The proximal tubule alters the volume and composition of filtrate by reabsorption and secretion. • In this area, ammonia, drugs, and poisons processed in the liver are secreted to join the filtrate. • Helps maintain a constant body fluid pH by controlled secretion of H+ and reabsorption of bicarbonate. • Nutrients such as glucose and amino acids are reabsorbed (by active transport) from the filtrate and returned to the interstitial fluid from which they enter the blood. The reabsorption of NaCI and water is also an important function of the proximal tubule. • Salt diffuses into the transport epithelium cells; the membranes facing the interstitial fluid then actively pump Na out of the cells, which is balanced by passive transport of Cl-. Water follows passively by osmosis. • Cells facing the interstitial fluid (outside the tubule) have a small surface area to minimize leakage of salt and water back into the filtrate. 2. In the descending limb of the loop of Henle, the transport epithelium is freely permeable to water but not to salt and other small solutes. • Filtrate moving down the tubule from the cortex to the medulla continues to lose water by osmosis since the interstitial fluid in this region increases in osmolarity. • The NaCl concentration of the filtrate increases due to the water loss. 3. In the ascending limb of the loop of Henle, the transport epithelium is very permeable to salt, but not to water. • As the filtrate ascends through the thin segment near the loop tip, NaCl diffuses out and contributes to the high osmolarity of interstitial fluids of the medulla. • In the thick segment leading to the distal convoluted tubule, NaCl is actively transported out into the interstitial fluid. • The filtrate becomes more dilute due to the removal of salts without loss of water. 4. The distal tubule is an important site of selective secretion and absorption. • It regulates K+ and NaCl concentrations of body fluids by regulating K+ secretion into the filtrate and NaCl reabsorption from the filtrate. • This region also contributes to pH regulation by controlled secretion of H+ and reabsorption of bicarbonate. 5. The collecting duct carries filtrate back through the medulla into the renal pelvis. • The transport epithelium here is permeable to water but not to salt. The filtrate loses water by osmosis to the hyperosmotic fluid outside the duct which results in a concentration of urea in the filtrate. This contributes to the high osmolarity of the interstitial fluid of the renal medulla, which enables the kidney to conserve water by excreting a hyperosmotic urine. The mammalian kidney’s ability to conserve water is a key terrestrial adaptation Cooperative action between the loop of Henle and the collecting duct maintains the osmolarity gradient in the tissues of the kidney. • The two solutes responsible for the gradient are NaCl (deposited by the loop of Henle) and urea which leaks across the epithelium of the collecting ducts. • The urine formed is up to four times as concentrated as the blood (about 1200 mosm/L). Conservation of water by two solute gradients The juxtamedullary nephron, with its urine-concentrating features, is a key adaptation to terrestrial life that enables mammals to excrete nitrogenous waste without squandering water. The functions of the vertebrate liver are critical to maintaining homeostasis and Filtrate passing from the Bowman’s capsule to the proximal tubule has about the same osmolarity as blood (300 mosm/L) (see Figure 44.20) A large amount of water and salt is reabsorbed as filtrate passes through the proximal tubule, which is located in the renal cortex. ~ The osmolarity remains about the same during the decrease in volume. Water moves out of the filtrate by osmosis as it flows from the cortex into the medulla through the descending loop of Henle. ~ The osmolarity steadily increases due to loss of water until it peaks at the apex. As filtrate moves up the ascending loop of Henle back to the cortex, salt leaves the filtrate first by passive transport and then by active transport. Osmolarity decreases to about 100 mosm/L at this point. Osmolarity changes very little as filtrate flows through the distal tubule as it is hypoosmotic to the interstitial fluids of the cortex. After entering the collecting duct, the filtrate passes back through the medulla. The filtrate loses water which increases osmolarity. Some urea also leaks out of the lower portion of the collecting duct. The passage of the filtrate back through the hyperosmotic medulla causes a gradual increase in osmolarity to about 1200 mosm/L; the remaining molecules are excreted in a minimal amount of water as urine which passes to the renal pelvis to the ureter. The loss of salt from the filtrate passing through the ascending limb of the loop of Henle to the interstitial fluid of the medulla contributes to the high osmolarity of the medulla. This, in turn, helps conserve water. The vasa recta (capillary network of the renal medulla) maintains the crucial osmolarity gradient in the kidney. • As the descending vessel conveys blood toward the inner medulla, water is lost from the blood and NaCl diffuses into the blood. • These fluxes are reversed as blood flows back toward the cortex in the ascending vessel. • This countercurrent system allows the vasa recta to supply the tissues with necessary substances without interfering with the osmolarity gradient. Urine, at its most concentrated, is isoosmotic to the interstitial fluid of the inner medulla, but is hyperosmotic to body fluids elsewhere. Nervous and hormonal feedback circuits regulate kidney functions The kidney is a versatile osmoregulatory organ subject to a combination of nervous and hormonal controls. • It excretes hyper- or hypoosmotic urine as necessary. Three mechanisms regulate the kidneys ability to change the osmolarity, salt concentration, volume, and blood pressure: 1) antidiuretic hormone 2) juxtaglomerular apparatus, and 3) atrial natriuretic factor. 1. Antidiuretic hormone (ADH) enhances fluid retention by increasing the water permeability of epithelium of the distal tubules and the collecting duct (see Figure 44.21a) • ADH is produced in the hypothalamus and stored and released from the posterior pituitary gland. • ADH release is triggered when osmoreceptor cells in the hypothalamus detect increased blood osmolarity due to an excessive loss of water from the body. • Increased water reabsorption reduces blood osmolarity and reduces stimulation of the osmoreceptor cells. Results in less ADH being secreted The functions of the vertebrate liver are critical to maintaining homeostasis and • • Ingestion of water returns blood osmolarity to normal When a large volume of water has been ingested, little ADH is released and the kidneys produce a dilute urine since little water is absorbed. Alcohol can inhibit ADH release, causing dehydration. 2. The juxtaglomerular apparatus (JGA) is a specialized tissue near the afferent arterioles, which carries blood to the glomeruli (see Figure 44.21b). • It responds to a decrease in blood pressure or blood volume, as well as to a decrease in blood sodium ion concentration by releasing the enzyme renin into the blood. • Renin leads to the conversion of inactive angiotensinogen to active angiotensin II, which functions as a hormone. • Angiotensin II directly increases blood pressure by causing arteriole constriction. • Angiotensin II acts indirectly by: Signaling adrenal glands to release aldosterone, which stimulates Na+ reabsorption by the distal tubules (water follows by osmosis) Stimulating thirst centers in brain to induce drinking behavior Increasing blood pressure and blood volume. • The increased blood pressure and blood volume suppresses further release of renin. • The renin-angiotensin-aldosterone system (RAAS) is part of a complex feedback circuit that functions in homeostasis. ADH and the RAAS cooperate in homeostasis. • ADH is released in response to increased blood osmolarity, but this does not compensate for excessive loss of salts and body fluids if blood osmolarity does not change. • RAAS responds to a decrease in blood volume caused by fluid loss. ADH alone would lower blood Na+ concentration by increasing water reabsorption, but the RAAS maintains balance by stimulating Na+ reabsorption. The hormone atrial natriuretic factor (ANF) opposes the RAAS. Released by the heart’s atrial walls in response to increased blood volume and pressure Inhibits release of renin from the JGA, inhibits NaCl absorption by the collecting ducts, and reduces aldosterone release from the adrenal glands; this decreases blood volume and lowers blood pressure The functions of the vertebrate liver are critical to maintaining homeostasis and