Cranial and Peripheral Nerve Disorders and Brain Tumors MLP
advertisement

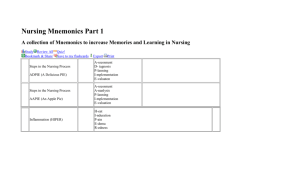
AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors Instructor Serial/Semester Location Start/Finish Time Date LESSON OBJECTIVE Performance: To gain an understanding of cranial nerve and peripheral nerve disorders and brain tumors. Conditions: The student will be presented a powerpoint presentation by the instructor and will have all necessary references made available to him/her. Standard: 1. Given the five elements of the nursing care process and a patient with a cranial nerve/peripheral nerve disorder or brain tumor by correctly responding to written, oral, and experiential assessment measures TEACHING POINTS 1. Identify the etiology/pathophysiology, clinical manifestations, assessment, diagnosis, and medical and nursing management of the patient with Trigeminal Neuralgia 2. Identify the etiology/pathophysiology, clinical manifestations, assessment, diagnosis, and medical and nursing management of the patient with Bell's palsy 3. Identify the etiology/pathophysiology, assessment, diagnostic findings, medical /surgical and nursing management of a patient with a brain tumor. 4. 5. 6. 7. 8 9. 10. INSTRUCTIONAL STRATEGY Interactive Lecture Method: Instructor Media: Classroom Environment: OTHER LESSON SPECIFICATIONS Knowledge Lesson Type of Lesson: 1/50 Ratio: Resources: . End of Lesson Test: None Minutes Instructional Time: 111 Reference(s): ISBN 0-323-01728-2 Adult Health Nursing, 4th Edition 01 Jan 2003 ISBN 0-7817-3553-X Introductory Medical-Surgical Nursing, 8th Edition 01 Jan 2002 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors LESSON PLAN APPROVAL Signature of Standards Officer 1 Date AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors INTRODUCTION Allocated Time: Review: 5 Minutes You have had previous anatomy and physiology lectures in your combat medic training, this lecture will build upon prior instruction. Objective: To discuss/describe topics related to the nursing process. Importance: Nurses work in various health care settings so it is important to gain an understanding of this subject as it will apply to your clinical practice. Fit: The patient who suffers from cranial/ peripheral nerve disorders usually experiences severe pain, and physical and emotional stress. The practical nurse must provide this patient with physical and emotional support, pain relief, reassurance, and health instructions. During this period we will focus on nursing of the patient with cranial/ peripheral nerve disorders and brain tumors. Approach: You will be presented the subject in lecture format and will be tested using a written exam at a later date. Control Statement: If you have any questions during the lesson please feel free to ask. BODY 1. Teaching Point: Identify the etiology/pathophysiology, clinical manifestations, assessment, diagnosis, and medical and nursing management of the patient with Trigeminal Neuralgia Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Please follow along with your hand outs and take notes. Skill Lesson Powerpoint presentation with associated handouts. Learning Support: a. Trigeminal Neuralgia. (1) Etiology/Pathophysiology. (a) Trigeminal neuralgia is one specific kind of peripheral nerve problem. (b) Caused by degeneration of or pressure on the nerve. (c) Etiology is unknown. (d) Tic douloureux is another name. (e) Usually affects persons in middle or late adulthood. (f) More common in women. 2 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors (2) Clinical Manifestations, Assessment, Diagnosis. (a) Characterized by excruciating, burning pain that radiates along one or more of the three divisions of the fifth cranial nerve. (See figure 14-20 in Christensen, page 642) This pain can last a few seconds or minutes and occur with great frequency. 1) Some patients may have constant discomfort. (b) The second and third divisions are most commonly affected. (c ) Pain typically extends only to the midline of the face and head because this is the extent of the tissue supplied by the offending nerve. (d ) There are areas along the course of the nerve known as trigger points. (e ) The slightest stimulation of these trigger points may initiate pain. (f ) Patients try desperately to avoid triggering these points. (3) Medical Management. (a) Drugs of choice for the treatment of trigeminal neuralgia pain: 1) Tegretol (Carbamazepine). 2) Dilantin (Phenytoin). 3) Depakene (Valproate). 4) Neurontin (Gabapentin). (b) Absolute alcohol may be injected into the peripheral branches of the trigeminal nerve. This provides relief for weeks to months. (c) Permanent relief of pain is obtained only by surgery that involves inserting a fine needle through the cheek and injecting an alcohol solution or surgically resecting the sensory root of the trigeminal nerve. 1) This is not always successful. (d) Within 24 hours after a fifth nerve resection, many patients develop herpes simplex of the lips (cold sores). These take about 1 week to heal. (4) Nursing Interventions. (a) Often patients have not eaten properly for some time because eating causes pain. They may be undernourished and dehydrated. Offer puree and warm foods. (b) They may not have washed, shaved, or combed the hair for sometime. (c) Oral hygiene often has been neglected. 3 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors (d) Comfort Measures for Patients with Trigeminal Neuralgia are: (1) Keep room free of drafts. (2) Avoid walking briskly to bedside of patient. (3) Place bed out of traffic area to prevent jarring of bed. (4) Avoid touching the patient’s face. (5) Do not urge patients to wash or shave the affected area or to comb the hair. (6) Avoid hot or cold liquids, which trigger pain. (7) Puree food and ensure that it is lukewarm. If necessary, suggest that food be taken through a straw. (8) Medication Teaching. (a) Tegretol-Toxic side effects include rash, drowsiness, ataxia. (b) Dilantin-Toxic side effects include ataxia, vomiting, nystagmus, drowsiness, rash, fever, gum hypertrophy, lymphadenopathy. (c) Depakene-Toxic side effects include nausea, vomiting, indigestion, sedation, emotional disturbance, weakness, altered blood coagulation. (d) Neurontin-Toxic side effects include somnolence, dizziness, ataxia, nystagmus, fatigue, G.I. upset. Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. Permanent relief of Trigeminal Neuralgia pain is obtained only by? Surgery Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 2. Teaching Point: Identify the etiology/pathophysiology, clinical manifestations, assessment, diagnosis, and medical and nursing management of the patient with Bell's palsy Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Please follow along with your hand outs and take notes. Skill Lesson Powerpoint presentation with associated handouts. Learning Support: a. Bell’s Palsy (Peripheral Facial Paralysis). 4 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors (1) Etiology/Pathophysiology. (a) Caused by an inflammatory process involving the facial nerve (VII), anywhere from the nucleus in the brain to the periphery. (b) Etiology is unknown but evidence that reactivated herpes simplex virus (HSV) may be involved in the majority of cases. (c) The reactivation of the HSV causes inflammation, edema, ischemia, and eventual demyelination of the VII (facial nerve). This causes pain and disturbances in motor and sensory function. (d) Any of the three branches of the facial nerve may be affected. (e) Disorder can be unilateral or bilateral. (2) Clinical manifestations, Assessment, Diagnosis. (a) Usually an abrupt onset of numbness or a feeling of stiffness or drawing sensation of the face. (b) Unilateral weakness of the facial muscles is most common resulting in inability to wrinkle the forehead, close the eyelid, pucker the lips, or retract the mouth on that side. (c) The face appears asymmetric, with drooping of the mouth and cheek. (d) Other symptoms that may occur include the following: 1) Loss of taste. 2) Reduction of saliva on affected side. 3) Pain behind the ear. 4) Ringing in ear or other hearing loss. (3) Medical Management. (a) There is no specific therapy for Bell’s palsy. (b) Electrical stimulation or warm moist heat along the course of the nerve may help. (c) Corticosteroids, especially prednisone, are started immediately. The best results are obtained if coricosteroids are initiated before paralysis is complete. Coricosteriods-Prednisone; Helps minimize paralysis if started immediately. Need to monitor blood glucose levels before, during, and after therapy as carbohydrate metabolism is affected. (d) Because the herpes simplex virus is implicated in approximately 70% of cases, treatment with the following alone or in conjunction with prednisone is common. 1) Zovirax (Acyclovir). 5 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors 2) Valtrex (Valacyclovir). 3) Famvir (Famciclovir). (e) Approximately 85% of patients recover fully in weeks or months but may take as long as one year. Taste is usually the first sign of improvement. (f) Recovery of taste within the first week signals a good chance for full recovery of motor function. (g) If paralysis remains incomplete within the first 5 to 7 days, the prognosis is also improved. (h) The remaining 15% of patients continue to be bothered by asymmetrical movement of facial muscles. (4) Nursing Interventions. (a) Protection of the eye when the eyelid does not close is important with use of a patch over the eye and tear drops to moisten the cornea. (b) Massage of the affected areas is recommended. (c) Exercises may be prescribed for 5 minutes TID. This includes wrinkling the brow and forehead, closing the eyes, and puffing out the cheeks. Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. Bell’s Palsy (Peripheral Facial Paralysis) is caused by? Etiology is unknown but evidence that reactivated herpes simplex virus (HSV) may be involved in the majority of cases. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 3. Teaching Point: Identify the etiology/pathophysiology, assessment, diagnostic findings, medical /surgical and nursing management of a patient with a brain tumor. Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Please follow along with your hand outs and take notes. Skill Lesson Powerpoint presentation with associated handouts. Learning Support: a. Intracranial Tumors. (1) Etiology/Pathophysiology. (a) Intracranial tumors include both benign and metastatic lesions. 6 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors (b) All areas of the brain can be affected. (c) Primary tumors, or neoplasms, arise from the cells of brain tissue and the primary and pineal glands. (d) These tumors include: 1) Gliomas. 2) Meningiomas. 3) Pituitary Tumors. 4) Neuromas. (e) Metastatic tumors also occur frequently. (f) Brain tumors are named for the tissues from which they arise. (2) Assessment. (a) Subjective data with a complete and thorough neurological exam. 1) Include the patient’s understanding of the diagnosis. 2) Note changes in personality or judgement . 3) Note presence of abnormal sensation or visual problems. 4) Complaints of unusual odors may be present with tumors of the temporal lobe. 5) Note history of headaches. 6) Note any hearing loss. 7) Note inability to carry out daily activities. (b) Objective data includes: 1) Motor strengths. 2) Gait. 3) Level of alertness. 4) Consciousness. 5) Orientation. 6) Pupils assessed for response and equality. 7 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors 7) Note any presence of seizures. 8) Speech abnormalities. 9) Note cranial nerve abnormalities. 10) Note any signs and symptoms of increased intracranial pressure. (3) Diagnostic Test. (a) No one procedure is entirely diagnostic of brain tumors. (b) CT scan is often the basis for the diagnosis. (c ) Other tests that may be performed include: (see Christensen p. 609-612) 1) Brain scan. 2) MRI. 3) PET scans. 4) EEG. 5) Arteriography. (4) Medical and Surgical Management. 1) Surgical removal when feasible. 2) Radiation. 3) Chemotherapy. (b) Choice of therapy is determined by: 1) Tumor site. 2) Tumor type. (c) A combination of medical and surgical management is often used. (d) Craniotomy is a surgical opening through the skull. This removal of the bone is carefully preserved and replaced at the end of surgery if there is no indication of infection or increased intracranial pressure. (e) Craniectomy is the surgical removal of part of the skull without replacing it. (f) Advances have been made in the use of intracranial endoscopy. 8 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors (g) Medications used to control increased intracranial pressure: 1) Osmotic diuretics/hyperosmolar drugs. They draw water from the edematous brain tissue. Examples: Manitol. 2) Corticosteriods- Usually given as dexamethasone. Monitor blood glucose levels as carbohydrate metabolism and glucose utilization can be affected. 3) Anticonvulsants are given to prevent seizures. a) Dilantin is the most commonly used. 4) Cerebyx is a short term IV or IM. Toxic side effects include cardiac collapse and central venous system depression. 5) Opioids and other drugs that cause respiratory depression are used sparingly post-operatively for pain control (they are used in the ICU for increased ICP). b. Nursing Management of a Patient with a Brain Tumor. (1) Preoperative preparation of both the patient and the family is important. (2) Fears are related to a possible permanent change in appearance, dependency, and possible death. (3) A baseline knowledge of neurological assessment is critical to master. (4) All treatments and procedures must be explained to patient, (e.g. shaving of hair). (a) Usually hair is shaved in the operating room. It is then given to the patient, who may choose to have it made into a wig. (5) Prepare the family ahead of time for the possible appearance of the patient. c. Nursing Diagnosis and Interventions: (1) Communication, impaired verbal, related to ischemic injury. (a) Speak slowly and distinctly. (b) Ask questions that can be answered by yes or no (or by signals). (c) Try to anticipate patient needs. (d) Provide call signal within reach of unaffected hand. (e) Begin speech therapy as soon as possible. (2) Nutrition, imbalanced: less than body requirements, related to impaired ability to swallow. (a) Provide IV fluids and tube feedings as prescribed during initial period. 9 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors (b) Assess ability to swallow before initiating feedings. (c) Position patient with head elevated and turned to unaffected side when feeding patient. (d) Provide foods initially that are easier to swallow (soft or pureed foods except for mashed potatoes). (e) Use training cup or feeding syringe for fluids as necessary. (f) Inspect mouth for food trapped in cheek pockets. (g) Be patient when feeding patient and provide directions for swallowing as needed. (h) Encourage patient to feed self as soon as possible; provide self-help devices as necessary. (3) Sensory perception, disturbed: visual, auditory, kinesthetic, tactile, related to compression/displacement of brain tissue. (a) Maintain method of communication. (b) Provide for social interaction. (c) Maintain a safe environment. (d) Provide orientation and appropriate level of stimuli. (4) Thought processes, disturbed, related to altered circulation or destruction of brain tissue. (a) Protect patient from self-injury. (b) Provide soft safety reminder devices as indicated. (c) Assist patient in self-care activities. (d) Speak in kind tone using short, simple sentences. (e) Give one direction at a time. (f) Relate date, time of day, and recent activities. (g) Maintain a therapeutic environment. (h) Keep equipment and personal possessions in same place. (i) Encourage socialization. 10 AFAMS Master Lesson Plan (MLP) Nursing Program Cranial Nerve and Peripheral Nerve Disorders and Brain Tumors Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. What are the diagnostic tests used to diagnose a brain tumor? CT scan, brain scan, MRI, PET scan, EEG, Arteriography. No one procedure is entirely used to make the diagnosis. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. END OF LESSON TEST Allocated Time: Instructions: Test Questions or Performance Expected: Test Key: 0 Minutes You will be tested on this subject at a later date. You will be expected to review and study the material taught in this session in order to pass the associated written test. If you have difficulty with the material please see me so we can review together. None. CONCLUSION Allocated Time: Summary: 5 Minutes Review and re-emphasize the difficult Teaching Points below. 1. 2. 3. Identify the etiology/pathophysiology, clinical manifestations, assessment, diagnosis, and medical and nursing management of the patient with Trigeminal Neuralgia Identify the etiology/pathophysiology, clinical manifestations, assessment, diagnosis, and medical and nursing management of the patient with Bell's palsy Identify the etiology/pathophysiology, assessment, diagnostic findings, medical /surgical and nursing management of a patient with a brain tumor. 4. 5. 6. 7. 8 9. 10. Closing Statement: Nurses work in various health care settings so it is important to gain an understanding of this subject as it will apply to your clinical practice. Re-motivating Statement: The patient who suffers from cranial/ peripheral nerve disorders usually experiences severe pain, and physical and emotional stress. The practical nurse must provide this patient with physical and emotional support, pain relief, reassurance, and health instructions. During this period we will focus on nursing of the patient with cranial/ peripheral nerve disorders and brain tumors. 11