Human Life Cycle
advertisement
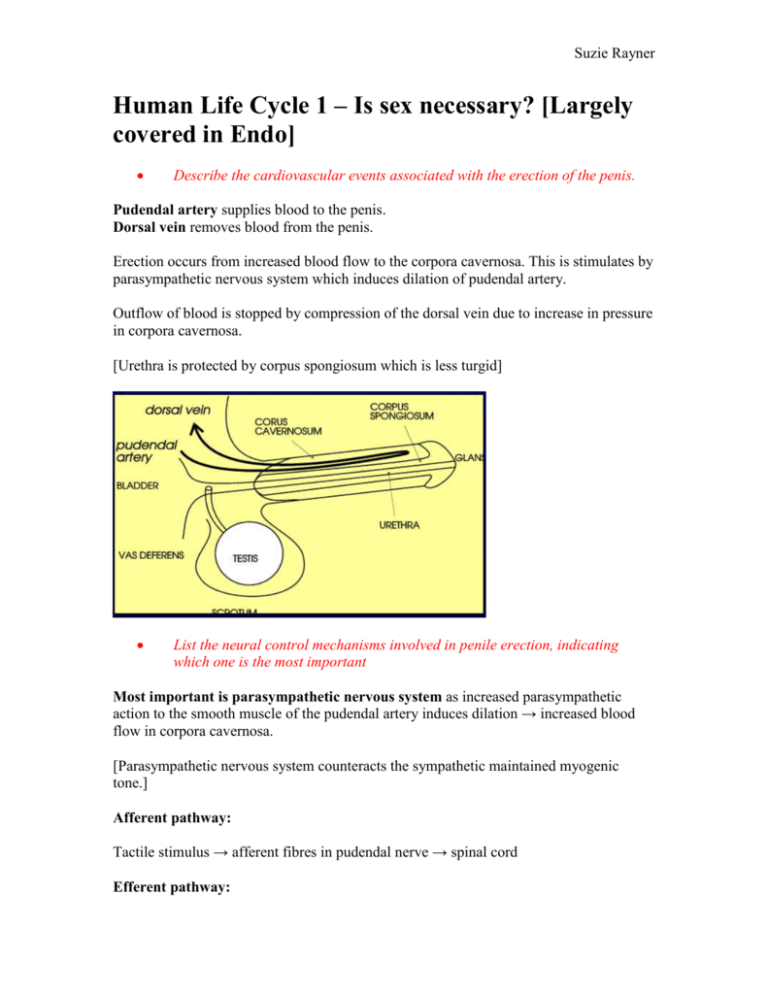
Suzie Rayner Human Life Cycle 1 – Is sex necessary? [Largely covered in Endo] Describe the cardiovascular events associated with the erection of the penis. Pudendal artery supplies blood to the penis. Dorsal vein removes blood from the penis. Erection occurs from increased blood flow to the corpora cavernosa. This is stimulates by parasympathetic nervous system which induces dilation of pudendal artery. Outflow of blood is stopped by compression of the dorsal vein due to increase in pressure in corpora cavernosa. [Urethra is protected by corpus spongiosum which is less turgid] List the neural control mechanisms involved in penile erection, indicating which one is the most important Most important is parasympathetic nervous system as increased parasympathetic action to the smooth muscle of the pudendal artery induces dilation → increased blood flow in corpora cavernosa. [Parasympathetic nervous system counteracts the sympathetic maintained myogenic tone.] Afferent pathway: Tactile stimulus → afferent fibres in pudendal nerve → spinal cord Efferent pathway: Suzie Rayner 3 possible: Nervous System Nerve Erection? Parasympathetic Pelvic Promotes Somatic Pudendal Promotes Sympathetic Hypogastric Depresses Penis: Flaccidity → Tumescence → Erection Mechanism of smooth muscle dilatation [Release of acetylcholine stimulates NO synthase → NO gets converted to cGMP which causes dilatation of arterial smooth muscle.] Clitoris is the erectile tissue in women, increases in size with increased blood flow. Mechanism is likely to be due to release of NO. Define the various stages of the menstrual cycle Understand the changes that occur in the endometrium during the different stages of the menstrual cycle Suzie Rayner Menstrual Phase: 4-5 days Cycle begins on first day of menstruation Shed blood and endothelium Flow of 20-80ml Proliferation Phase [N.B. everything becomes more]: 9 days Growth of follicles occurs, controlled by 17β-oestradiol from follicles 2-3x increase in thickness of endothelium [phase of repair and proliferation – epithelium repairs, glands increase in number] Secretory Phase: 13 days Controlled by progesterone (luteal phase of ovarian cycle) and oestrogen (but less so) Formation, functioning and growth of corpus luteum Glands in epithelium become wider and tortuous [due to progesterone] Thicker endometrium [due to progesterone and oestrogen] Spiral arteries Know how the different stages of the ovarian cycle relate to the stages of the menstrual cycle Describe the various stages and events of the ovarian cycle and the hormones acting at these various stages Follicular phase and luteal phase of the ovarian cycle are linked by chemicals produced during these phases, which changes in endometrium. Follicular phase produces 17β-oestradiol → growth of follicle Luteal phase produces progesterone → widening of glands and thickening of endometrium Know which hormones act at various stages of the menstrual and ovarian cycle Suzie Rayner Explain why the changes occurring in the endometrium are important for implantation Describe how the endometrium is maintained if pregnancy ensues Corpus Luteum is maintained by human chorionic gonadotrophin (hCG), which is produced by the syncytiotrophoblast. Therefore progesterone and oestrogen continue to be produced. Describe the endometrial changes if pregnancy does not occur No fertilization Corpus luteum regresses Menstrual phase occurs Suzie Rayner Understand that the menstrual cycle various in its length from female to female and also within one female from month to month Describe other methods of how the sperm and egg can be artificially brought together In vitro fertilisation Human Life Cycle 2 – In the beginning… Summary of early development: 1st Trimester: Weeks 1-2: Blastocyst stage Weeks 3-8: Embryonic stage Week 9 onwards: Fetal stage 2nd Trimester: Rapid Growth of Fetus 3rd Trimester: Fat production Fertilisation: Occurs in the fallopian tube, at the distal end (ampulla) Sperm penetrates the several oocyte coats Zona pellucida prevents polyspermy and permits implantation at correct site Fertilisation causes oocyte to complete meiosis II – completes number of chromosomes, determines gender Post-fertilisation: Zygote travels down fallopian tubes Divides – first cleavage at around 20 hours → Morula (12-16 cells) → blastocyst Zona pellucida is shed Implantation, hCG production. Suzie Rayner Why do we study development? o Know how structures develop o How normality arises/how abnormality arises o Positioning of adult structures o Understand that several tissues form at same time, requiring same genes What structures are required for development of the human to ensue? Female and male germ cells. [Spermatozoon, Oocyte] Define and understand the following terms: Gametes: mature germ cells [male – spermatozoa, female – oocytes] Fertilisation: the process in which the nucleus of a spermatozoon enters the oocyte and fuses with the female pronucleus to produce a zygote. Pronuclei: nucleus of mature germ cells, haploid Zona pellucida: clear, acellular membrane that surrounds the oocyte protecting against polyspermy (multiple sperms entering) Haploid: 23 chromosomes in the cell, 22 autosomes and 1 sex chromosome. Diploid: 46 chromosomes in the cell, pairs of autosomes and a pair of sex chromosomes. Implantation: process in which the blastocyst imbeds in the endometrium. Suzie Rayner First cleavage division: first cytoplasmic division by meiosis, cell membrane infolds as a deep furrow, dividing cell into 2. Formation of morula: the zygote when it has 12-16 cells (just before it becomes a blastocyst) Formation of blastocyst: hollow ball of blastomeres, formed when fluid is pumped into morula after its compaction. Inner Cell Mass: a.k.a embryoblast. Contains blastomeres which form embryo. Trophoblast: Outside region of blastocyst which invades the endometrium, forms the placenta. Embryo: tissues arising from the zygote which later contribute to fetus/child. Comprehend that development does not always go to plan and that abnormalities can arise at different levels. Give examples of chromosomal abnormalities that may occur Mosaicism, Structural, Numerical Down’s syndrome (trisomy 21) Turner’s syndrome (45, X) Kleinefelter’s syndrome (47, XXY) Patau’s syndrome (Trisomy 13) Edward’s syndrome (Trisomy 18) Name possible sites where an ectopic pregnancy may arise. Most common in the fallopian tubes (95%) Other locations: Ovary Peritoneal cavity Suzie Rayner Name the two layers that the inner cell mass differentiates into to give rise to the bilaminar disk stage of development and how the two layers give rise to the third body or germ layer of the embryo. Inner cell mass differentiates into 2 layers: Epiblast – forms amniotic cavity and fluid Hypoblast – forms yolk sac Day 15: Gastrulation: formation of trilaminar embryo Coordinated process of cell movement. Has organiser at top and bottom end of embryonic ectoderm – Cranial and Caudal Suzie Rayner Primitive streak from caudal end – where cells from epiblast are proliferating and moving into gap between epiblast and hypoblast. This results in formation of 3 layers: Epiblast becomes ectoderm. The mesoderm forms between the two layers Hypoblast becomes endoderm. Primitive streak moves towards cranial end from caudal end Primitive node forms Human Life Cycle 3 – Pattern Formation Name the structures that are derived from the three body or germ layers of the embryo. Ectoderm: develops into skin and nervous system Mesoderm: develops into skeleton, muscle, kidney, heart, blood Endoderm: develops into gut, liver and lungs Day 17: Define how the neuroectoderm gives rise to the neural plate and how this structure folds to form an early neural tube that will give rise to the brain and spinal cord later in development. Suzie Rayner Notochord: forms at primitive node from invaginating epiblast cells extends cranially, forming basis of axial skeleton involved in inducing formation of neural tube and somite formation Neurulation - Day 19-27: Notochord induces ectoderm to become neuroectoderm. Neuroectoderm gives rise to: o Neural plate o Neural groove o Neural folds Ultimately gives rise to neural tube Neural Crest: arises from crest of neural folds migrates from neurectoderm into underlying mesoderm [see following diagram] gives rise to: o melanocytes (melanin production) o Glial and Schwann cells o cranial nerves o odontoblasts (creation of dentin – tooth enamel) o connective tissue and bones of face and skull Suzie Rayner Define the divisions of the intra-embryonic mesoderm and briefly describe which structures each will give rise to. Intra-embryonic mesoderm is divided into: Paraxial mesoderm: becomes somites Intermediate mesoderm: becomes urogenital Lateral plate mesoderm: lines body cavities and surround organs (coelom) – splits into two (visceral next to endoderm, parietal next to ectoderm) Suzie Rayner Somites [3 layers]: Sclerotome – precursor to cartilage and bone Myotome – precursor to muscle Dermatome – precursor to skin 1st – Day 20 Anterior to posterior, 35 by Day 30. Parts of extra-embryonic mesoderm will become: Body stalk – umbilical cord Amnion, yolk sac, chorion Describe which two parts of the embryonic disk always remain as a bilaminar disk and the consequences of this. Buccopharangeal membrane at front of embryo and cloacal membrane at bottom. These mark where the gut starts and finishes. Which part of the neural tube develops most vigorously during early development and what is the consequence of this? Give an example of genetic regulation of embryonic development. Example: Hox genes: Establish A-P axis (anterior-posterior?) Differences in vertebrae CNS divisions Patterns of limbs One signal that controls activation of Hox genes is Retanoic Acid (derivative of Vit. A) Suzie Rayner Define the causes of abnormalities during embryonic patterning. All Chromosomal Genetic examples: Holt-Oram syndrome (heart/hand defects) Achondroplasia (dwarfism) Cleft lip CF Environmental: Dietary Alcohol abuse Drug use Radiation Rubella Spina Bifida (posterior neuropore doesn’t close properly, neural tissue bulges out) Suzie Rayner Summary of embryonic development (first 9 weeks) Time Day 6 Day 8-9 Day 12-13 Week 3 Week 4 Week 5 Week 6 Week 7 Week 8 Event Attachment to endometrial epithelium Implantation and formation of trophoblast shell Bilaminar embryonic disc Trophoblast invasion and contact with maternal blood Formation of trilaminar disc Formation of CNS Formation of somites Blood vessel initiation Heart forms Formation of placental villi Closure of neural tube Face and arm initiated Umbilical cord forms Elaboration of placental villi Face and Limbs continue Face, ears, hands, feet, liver, bladder, gut, pancreas Face, ears, fingers, toes Lungs, liver, Kidneys Placental elaboration continues Villous Localisation Placental endocrinology becomes dominant Size 2mm 3mm 4mm 5-8mm 10-14mm 17-22mm 28-30mm [N.B. up to Week 5, Week approximately equals Length] HLC 4 – Body Cavities Placental mammals evolved from egg-laying reptiles, therefore same cavities but newly evolved roles: Cavity/structure Yolk sac Chorionic cavity Chorion Amniotic cavity Allantois Allantoic mesoderm Role Part in gut development, other than that redundant Obliterated early Gives rise to placenta Embryo floats in it, later tests its urinary and respiratory systems into it Gives rise to part of urinary bladder Gives rise to placental blood vessels Suzie Rayner Chorion and amnion eventually fuse (chorioamnion) and obliterate chorionic cavity. [N.B. Amniocentesis – used to check for embryo abnormalities, culture embryonic cells and test for α-fetoprotein as indicative of neural tube defect] Explain how the intra-embryonic coelom develops Cavities form in preoral and lateral plate mesoderm. These join to form a horseshoe shape called intra-embryonic coelom The intra-embryonic coelom develops into: Pericardial cavity (cranially – heart) Pleural cavity (intermediate – lungs) Peritoneal cavity (caudally – urogenital) Suzie Rayner Explain how the cranial part of the intra-embryonic coelom forms the pericardial cavity Head and tail folding: Tucks developing heart and pericardial sac ventrally Pinches gut tube off yolk sac Narrows body stalk Completion of head folding: Forebrain now cranial to heart Gut tube connected to yolk sac by narrow stalk Heart ventral to gut tube Original cranial part of coelom is now ventral to intermediate parts Describe the process of development of the visceral and parietal pericardium Explain the derivation of the visceral and parietal peritoneum Develop from lateral plate mesoderm – splits in two: Visceral adjacent to endoderm Parietal adjacent to ectoderm Give an account of lateral folding of the embryo Lateral body folding: Embryo’s body is turned into cylinder from sheet. Rolls up gut tube, nips off yolk sac Cuts intraembryonic coelom off from chorionic cavity Amniotic cavity surrounds embryo except at body stalk Be able to give an account of formation of the body cavities and how the lateral plate mesoderm is so important in their development Suzie Rayner Human Life Cycle 5 – The placenta: life support system of the fetus Draw simple sketches to show the differentiation of the chorion through morula and blastocyst stages In blastocyst: Inner cell mass develops into embryo, amnion and yolk sac Trophoblast (epithelial layer of the chorion) forms a fused layer (syncytiotrophoblast), which eventually develops into the placenta Define cytotrophoblast and syncytiotrophoblast Cytotrophoblast: inner layer of the trophoblast, consisting of cells which contribute to the amnion and the syncytiotrophoblast. Syncytiotrophoblast: outer layer of the trophoblast, consists of a syncytium of giant cells and invades endothelium forming placenta [Syncytium: many nuclei in same extent of cytoplasm] Describe the invasion of maternal tissues by the syncytiotrophoblast during and after implantation Suzie Rayner Syncytiotrophoblast burrows through the uterine epithelium to implant the conceptus within the uterus wall [Resembles Cancer] invades uterine epithelium and connective tissue invades and destroys small vessels of uterus lining (causing maternal blood to flow into intervillous space) Widens uterine arteries (increasing flow) Sheds fragments into maternal blood These fragments may metastasise to mothers lungs or may reach systemic circulation This causes pre-eclampsia: Increased blood pressure Protein leaking into urine Caused by metastasis of syncytiotrophoblast causing vascular disturbance or insufficient placental invasion of uterine wall Compare the main sources of nutrition of the embryo or fetus before implantation, during the first trimester and in the latter two trimesters Before implantation: Embryo depends on its own reserves and fluid in the uterine tube No net. growth Expansion of blastocyst depends on the uptake of NaCl and water. Week 2 – Week 8/12: Maternal tissue fluid and breakdown products within intervillous space Week 8/12 onwards: Maternal blood flow through intervillous space Explain the terms “ectopic pregnancy” “placenta praevia” and indicate why these conditions are dangerous Suzie Rayner Ectopic pregnancy: where the conceptus has implanted in the wrong place Placenta praevia: when the placenta is sited so that it will block normal cervical delivery Cause complications in labour, cause ruptures to mothers reproductive system…etc Explain why the term “haemochorial” is applied to the human placenta There is no point where the fetal and maternal blood come into direct contact. Explain the origin of the intervillous spaces and the establishment of maternal blood circulation through them Chorionic villi are initially sprouts of the trophoblasts over the whole surface, but over time they: retreat to basal side forming placental disc branch and acquire cores of connective tissue become vascularised and connected to embryos cardiovascular system Allantoic vessels grow through the body stalk to the placenta, allowing all exchanges with the mother. Syncytiotrophoblast adapts blood flow (see previous learning objective) Feto-maternal blood interface: Fetal blood circulates through villous cores in capillaries Maternal blood flows from dilated arteries directly into intervillous space Suzie Rayner Define “decidualisation” and explain its importance Decidualisation: normal response of endometrium to implantation modifies uterine arteries to ensure adequate blood flow provides protective mechanisms against rejection of feto-placental tissue by mothers immune system Describe the origin of the amnion and outline the origins and importance of amniotic fluid Inner cell mass divides forming epiblast. Within the epiblast layer, many small fluidfilled spaces appear which combine forming the amniotic cavity. Amnion lines the chorion and contains amniotic fluid which the fetus floats it, drinks and excretes into. (acts as a shock absorber) Sketch the tissue layers separating maternal from fetal blood Contrast the mechanisms by which (a) respiratory gases (b) electrolytes, glucose and amino acids and (c) immunoglobulin G cross the materno-fetal barrier Lipid soluble molecules are unrestricted (e.g. blood gases, ethanol, anaestetics, steroids) Small uncharged molecules are unrestricted (e.g. water, urea) Large hydrophilic molecules are limited by membrane transporters (e.g. glucose, amino acids) Proteins are held back unless there is a specialised transport system (e.g. for IgG) [N.B. Respiratory gases – unrestricted, electrolytes etc – limited, IgG – specialised transport] Suzie Rayner Indicate the endocrine roles of the placenta Suggest how the placenta may avoid attack by the maternal immune system Secretes hormones which: maintain pregnancy promote lactation (prepare breasts for it) suppress menstruation Involved in initiation of labour Does not evoke maternal response to foreign tissue Outline how uterine blood loss is minimised when the placenta is delivered Know what proportion of the maternal cardiac output perfuses the uterus at term 1/6 of maternal blood. Human Life Cycle 6 – The significance of the Y chromosome Explain the significance of the Y chromosome with particular reference to the SRY gene. Describe the role of the SRY protein with respect to control over gonadal development. Gonads derived from somatic mesenchymal tissues (forming matrix) and primitive germ cells (forming gametes) Differentiation of gonads begins after Week 6 – formation of testes is actively initiated (i.e. without activation, become female) Within developing seminiferous cords (in males): Primordial germ cells → spermatozoa Mesodermal cells → Sertoli cells of seminiferous tubules Between seminiferous tubules, clusters of interstitial cells condense → Leydig cells SRY (sex determining region) gene is located on the Y chromosome SRY initiates formation of sertoli cells (expressed in male sertoli cells) SRY protein is a transcription factor regulating other gene activity. Suzie Rayner Draw a diagram illustrating the effects of androgens and Mullerian Inhibitory Factor on fetal reproductive system development. Draw a diagram illustrating the development of Testicular Feminization Syndrome (Complete androgen insensitivity syndrome – CAIS) Draw a diagram illustrating the consequences of excess androgens in a fetal female genotype. Excess androgens cause both male and female internal genitalia to develop, and male external genitalia. Suzie Rayner Human Life Cycle 7 – Development of urinary and reproductive organs Outline the development of the kidneys, ureters, urinary bladder and urethra. Intermediate mesoderm gives rise to most of upper urinary and genital systems Intermediate mesoderm gives rise to urogenital ridge, within which the nephrogenic cord develops (kidney making). Nephrogenic cord is source of most of urogenital system (exceptions: primordial germ cells, lower urinary tract, perineum) Development of kidneys: Sweeps cranio-caudially (top to bottom) Region Cervical Thoraco-lumbar Mesonephric duct Sacral mesonephros Ureter grows out from mesonephric duct. Event in kidney development Never differentiates, regresses by Week 4 Mesonephros differentiates, but has mainly gone by Week 8 Persists in males Appears in Week 5, becomes definitive kidney Suzie Rayner Maldevelopment of kidneys: fail to reposition (retain sacropelvic position) joined together – trapped below inferior mesenteric artery (horseshoe kidney) Development of urinary bladder: Allantois gives rise to most of bladder [N.B. slender duct extending to umbilicus normally closes but if it does not it can cause problems] Cloaca becomes partitioned into urogenital sinus and rectal sinus. [N.B. sometimes partitioning is incomplete and congenital fistula (opening) connects urogenital and alimentary tracts] Maldevelopment of ureters: Complete duplication Partial duplication (become one at some point) Ectopic (opening in abnormal place) Position of kidneys and ureters: Shared sections of ureter and mesonephric duct (in males) are absorbed into the back of the bladder. Ureters now open into bladder and the Mesonephric ducts into urethra. Differential growth shifts metanephric kidneys from sacral site of origin to the posterior wall of upper abdomen (up and backwards) Suzie Rayner Outline the mechanism of differentiation of male and female structures in the pelvis and perineum, including gonads, uterine tubes, uterus, vagina, vulva, ducti deferentes, seminal vesicles, prostate, scrotum and penis. Outline gonadal descent and the formation of the inguinal canal. In males – (the relationship of the gonads and the mesonephric duct.) Gonads develop medially to mesonephros kidney Most of mesonephros atrophies but parts between gonads and mesonephric ducts persists These persistent parts will become efferent ducts between testis and ductus deferens Developing testes link with mesonephric duct through some persistent mesonephric tubules In 4th month testes descend into scrotum (through inguinal canal) Ductus deferens develop into seminal vesicles Urethra develops into prostate In Females – (Paramesonephric ducts) Paramesonephric ducts develop in most lateral part of intermediate mesoderm In females they become uterine tubes, uterus and upper vagina [Not important in males] From Week 8 - 4th month, paramesonephric ducts link with each other and the urogenital sinus to assemble definitive female structure Ovaries descend from origin, in upper lumbar region, to the pelvis Primordial germ cells give rise to eggs and sperm arise from yolk sac in week 6 they migrate to genital ridge (via hindgut and mesentery) A few survive to form PGCs and somatic cells of next generation Suzie Rayner Sex determination – covered in HLC 5 Development of external genitalia: Same for both genders from weeks 3-6 Female: Genital swelling → labia majora Cloacal fold → urethral fold → labia minora Urethra opens into vestibule posterior to clitoris Suzie Rayner Male: Expansion of phallus Fusion of urethral folds to enclose the penile urethra (if incomplete – hypospadius) Expansion and fusion of genital swellings to form scrotum Outline the origin of the disorders of urogenital system development below Duplication of a ureter from mesonephric duct Absence of kidneys Pelvic and horseshoe kidneys Pelvic – kidneys do not migrate from their origin Horseshoe – kidneys are joined together and get stuck below the inferior mesenteric artery Polycystic kidneys Wilm’s tumour of the kidney Hypospadias Incomplete fusing of the urethral folds Mismatch between genetic and phenotypic sex (pseudohermaphroditism) Androgen insensitivity (receptors don’t work)