MCQs Final Test
advertisement
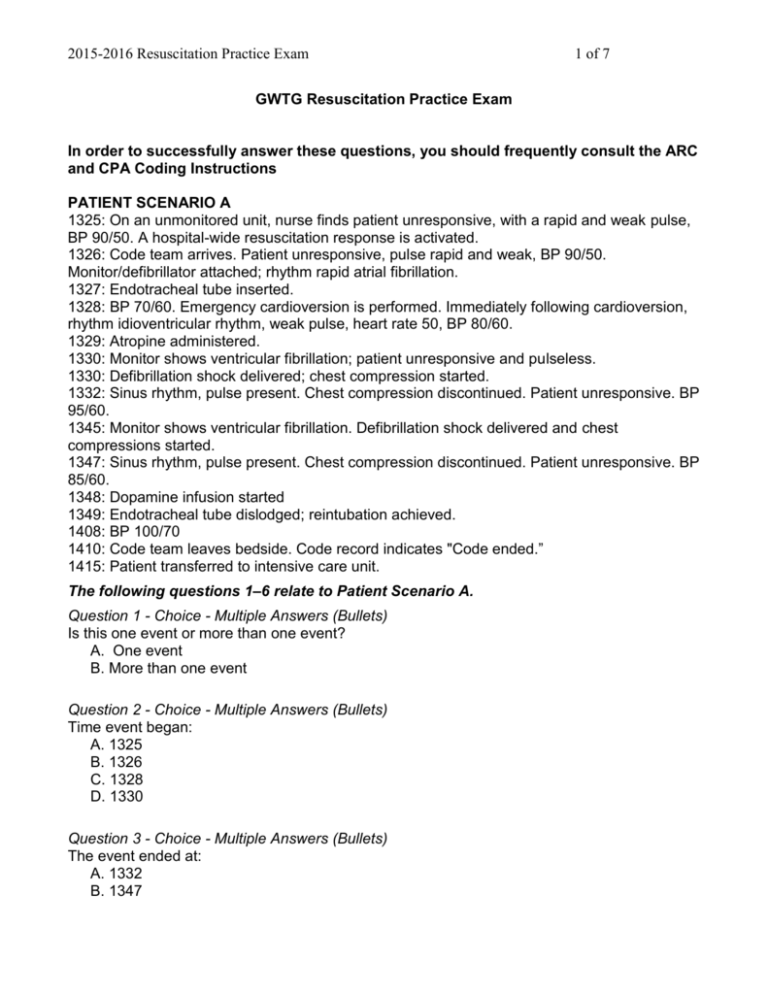
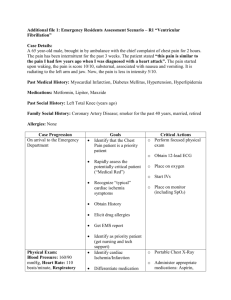
2015-2016 Resuscitation Practice Exam 1 of 7 GWTG Resuscitation Practice Exam In order to successfully answer these questions, you should frequently consult the ARC and CPA Coding Instructions PATIENT SCENARIO A 1325: On an unmonitored unit, nurse finds patient unresponsive, with a rapid and weak pulse, BP 90/50. A hospital-wide resuscitation response is activated. 1326: Code team arrives. Patient unresponsive, pulse rapid and weak, BP 90/50. Monitor/defibrillator attached; rhythm rapid atrial fibrillation. 1327: Endotracheal tube inserted. 1328: BP 70/60. Emergency cardioversion is performed. Immediately following cardioversion, rhythm idioventricular rhythm, weak pulse, heart rate 50, BP 80/60. 1329: Atropine administered. 1330: Monitor shows ventricular fibrillation; patient unresponsive and pulseless. 1330: Defibrillation shock delivered; chest compression started. 1332: Sinus rhythm, pulse present. Chest compression discontinued. Patient unresponsive. BP 95/60. 1345: Monitor shows ventricular fibrillation. Defibrillation shock delivered and chest compressions started. 1347: Sinus rhythm, pulse present. Chest compression discontinued. Patient unresponsive. BP 85/60. 1348: Dopamine infusion started 1349: Endotracheal tube dislodged; reintubation achieved. 1408: BP 100/70 1410: Code team leaves bedside. Code record indicates "Code ended.” 1415: Patient transferred to intensive care unit. The following questions 1–6 relate to Patient Scenario A. Question 1 - Choice - Multiple Answers (Bullets) Is this one event or more than one event? A. One event B. More than one event Question 2 - Choice - Multiple Answers (Bullets) Time event began: A. 1325 B. 1326 C. 1328 D. 1330 Question 3 - Choice - Multiple Answers (Bullets) The event ended at: A. 1332 B. 1347 2015-2016 Resuscitation Practice Exam 2 of 7 C. 1408 D. 1410 Question 4 - Choice - Multiple Answers (Bullets) Condition that best describes the event: A. Patient was PULSELESS when need for chest compressions and/or need for defibrillation of initial rhythm VF/Pulseless VT was first identified B. Patient had a pulse (poor perfusion) requiring chest compressions PRIOR to becoming pulseless C. Patient had a pulse (poor perfusion) requiring chest compressions but never became pulseless. Question 5 - Choice - Multiple Answers (Bullets) The following medications/interventions should be included for this patient during the CPA event: A. Atropine and dopamine, and invasive airway insertion and reinsertion B. Invasive airway reinsertion C. Dopamine D. None of the above Question 6 - Choice - Multiple Answers (Bullets) Was an invasive airway inserted/reinserted during the event? A. Yes, both initial insertion and reinsertion of invasive airway achieved B. Yes, initial insertion and of invasive airway achieved C. Yes, reinsertion of invasive airway achieved D. No, already in place PATIENT SCENARIO B 0529: Staff identify patient on telemetry with rhythm sinus, rate 40. Patient is lethargic, breathing, with a weak, slow pulse; blood pressure 70/40. A hospital-wide resuscitation response is activated. 0530: Atropine IV administered. 0531: Transcutaneous pacing attempted; fails to capture 0532: Blood pressure 50 palpable, heart rate 35. Bag-mask ventilation and chest compressions started. 0534: Patient pulseless. Rhythm idioventricular, rate 30. 1 mg IV epinephrine given 0538: Another 1 mg dose of epinephrine IV is administered. 0541: Pulse present, BP 80/60, rhythm sinus tachycardia. Chest compressions stopped. 0544: Dopamine infusion is initiated. 0602: BP has stabilized. The following questions 7–12 relate to Patient Scenario B. Question 7 - Choice - Multiple Answers (Bullets) 2015-2016 Resuscitation Practice Exam 3 of 7 Time the need for chest compressions (or defibrillation when initial rhythm was VF or Pulseless VT) was FIRST recognized: A. 0529 B. 0531 C. 0532 D. 0533 Question 8 - Choice - Multiple Answers (Bullets) Condition that best describes the event: A. Patient was PULSELESS when need for chest compressions and/or need for defibrillation of initial rhythm VF/Pulseless VT was first identified B. Patient had a pulse (poor perfusion) requiring chest compressions PRIOR to becoming pulseless C. Patient had a pulse (poor perfusion) requiring chest compressions but never became pulseless Question 9 - Choice - Multiple Answers (Bullets) The initial rhythm is: A. Sinus B. Bradycardia C. Idioventricular rhythm D. Ventricular tachycardia Question 10 - Choice – Multi0ple Answers (Bullets) The initial pulseless rhythm is A. Asystole B. Idioventricular rhythm C. Pulseless electrical activity (PEA) D. Ventricular tachycardia Question 11 - Choice - Multiple Answers (Bullets) The following medications/interventions should be included for this patient during the CPA event: A. 2 doses of epinephrine, atropine and dopamine B. 2 doses of epinephrine C. 2 doses of epinephrine and transcutaneous pacing D. 2 doses of epinephrine, atropine, dopamine and transcutaneous pacing Question 12- Choice - Multiple Answers (Bullets) Time sustained return of circulation (ROC) began that lasted > 20 minutes A. 0533 B. 0538 C. 0541 D. 0602 2015-2016 Resuscitation Practice Exam 4 of 7 PATIENT SCENARIO C 1030: Patient complains of chest pain at same-day surgical area and is taken to the Emergency Department 1032: She is admitted to Emergency Department. 1145: She is admitted to the hospital coronary care unit. 1600: She has a cardiopulmonary arrest (CPA) while in the coronary care unit. The following question 13 relates to Patient Scenario C. Question 13 - Choice - Multiple Answers (Bullets) The system entry time for this patient is: A. 1030 B. 1032 C. 1145 D. 1600 PATIENT SCENARIO D 1930: Patient in ICU, intubated on T-piece. Monitor shows ventricular fibrillation. 1931: Nurse finds patient unresponsive, not breathing and pulseless. Chest compressions and bag-valve ventilation started. 1931: ICU staff activated (called for help) 1932: Defibrillation shock delivered; chest compressions continued 1934: Pulseless, rhythm asystole, chest compressions continued 1935: IV epinephrine bolus 1935: Patient cyanotic, high airway pressure alarm on ventilator 1938: Endotracheal tube removed and new endotracheal tube reinserted 1938: Pulseless, rhythm asystole, chest compressions continued; IV epinephrine bolus 1940: Rhythm sinus tachycardia. Pulse present. Chest compressions stopped. 1944: Lidocaine bolus administered and infusion started. 1950: Dopamine started for BP 80/60. 1955: Blood pressure 90/60 2001: Blood pressure 110/70. Patient stabilized The following questions 14–17 relate to Patient Scenario D. Question 14 - Choice - Multiple Answers (Bullets) Time need for chest compression (or defibrillation of VF/pulseless VT) first recognized: A. 1930 B. 1931 C. 1934 D. 1940 Question 15 - Choice - Multiple Answers (Bullets) Was a hospital-wide resuscitation response activated? A. Yes 2015-2016 Resuscitation Practice Exam 5 of 7 B. No Question 16 - Choice - Multiple Answers (Bullets) The initial pulseless rhythm is: A. Asystole B. Pulseless electrical activity (PEA) C. Pulseless ventricular tachycardia D. Ventricular fibrillation Question 17 - Choice - Multiple Answers (Bullets) Was any invasive airway inserted/re-inserted during event? A. Yes, initial insertion of invasive airway achieved B. Yes, reinsertion of invasive airway achieved C. No, already in place D. No, not inserted (includes unsuccessfully attempted). Question 18 - Choice - Multiple Answers (Bullets) A patient has an ARC event in the field ten minutes prior to Emergency Department (ED) arrival. Pre-hospital EMS providers are providing assisted ventilation using a bag-valve device as the patient comes through the ED doors. Two minutes after arriving in the ED, the patient develops pulseless electrical activity requiring chest compressions. Resuscitation is stopped after 30 minutes and the patient is pronounced dead. You should: A. Not include the event at all B. Include the event as ARC C. Include the event as an ARC event that ends in a CPA event D. Include the event as CPA only. Question 19 - Choice - Multiple Answers (Bullets) When a patient survives a CPA event, the time of the end of the event is determined by: A. Twenty minutes after the beginning of the patient’s first Return of Circulation (ROC). B. The time of the beginning of a period of sustained return of circulation (ROC) lasting greater than 20 minutes. C. The time written on the code record for “Resuscitation ended at….” D. The time the patient is transferred to a critical care unit from a general floor. Question 20 - Choice - Multiple Answers (Bullets) A patient collapsed outside the hospital on the sidewalk. Initial response for CPA was by a bystander and facility first-responders. Ongoing resuscitation was transferred to EMS personnel who transported the patient to the hospital ED. Upon arrival in the ED, staff continued CPR, intubated the trachea, and provided intubation and drugs. This CPA event is: A. Included because ED staff provided ACLS care of intubation, defibrillation and drugs B. Included because the event began outside the hospital on the sidewalk. C. Excluded because response was by facility first-responders with ongoing resuscitation 2015-2016 Resuscitation Practice Exam 6 of 7 transferred to EMS personnel. D. Excluded because the event occurred outside the hospital. Question 21 - Choice - Multiple Answers (Bullets) In pulseless CPA events, the beginning of Return of Circulation (ROC) is determined by: A. Record of Normal Sinus Rhythm (NSR) on the code sheet. B. Return of pulse (e.g. palpated, Doppler, auscultated, arterial blood pressure waveform or documented blood pressure C. Record of paced rhythm with electrical capture on the code sheet. D. All of the above. The following questions 22-23 relate to this scenario: An unmonitored patient experiences sudden cardiac arrest. The first line on the code sheet shows a time of 4:15 AM with a rhythm of "Unknown” and CPR started. At 4:16 AM a monitor/defibrillator is applied. The Code Sheet indicates sinus, rate 40 with no pulse at 4:17 AM. Question 22 - Choice - Multiple Answers (Bullets) The first documented pulseless rhythm for this patient would be: A. Sinus rhythm B. Bradycardia C. Pulseless Electrical Activity (PEA) D. Unknown Question 23 - Choice - Multiple Answers (Bullets) Time need for chest compression (or defibrillation of VF/pulseless VT) first recognized: A. 0415 B. 0417 C. 1615 D. 1617 PATIENT SCENARIO E 1439: Visitor collapses in hospital lobby 1440: Hospital code team responds, finds patient unresponsive, not breathing and pulseless, and starts chest compressions. 1441: AED attached 1442: Shock advised and delivered. Chest compressions continued. 1444: Rhythm sinus tachycardia and pulse present. Compressions stopped. 1451: Patient admitted to ED. The following questions 24-25 relate to Patient Scenario E. Question 24 - Choice - Multiple Answers (Bullets) This event: 2015-2016 Resuscitation Practice Exam A. Meets inclusion criteria B. Does not meet inclusion criteria Question 25 - Choice - Multiple Answers (Bullets) The system entry time for this patient would be A. Not applicable; event does not meet inclusion criteria B. 1439 C. 1440 D. 1451 7 of 7