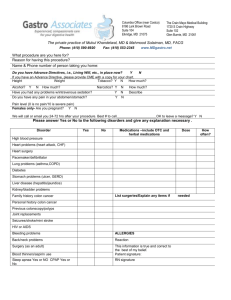
Function of the Ileocecal Valve
advertisement

Gastrointestinal I - #16 Dr. Gwirtz 2/19/03, 11AM Scribe – Matthew Stine Page of 7 Checked By Dr. Gwirtz!! GI Motility: Part 3 – Colon, Diarrhea, Vomiting, Gas and Good Times Note: This lecture began on Slide #60 in the GI Motility Slides. I. Colon A. Anatomical Subdivisions of the Colon 1. Terminal Ileum empties into the Cecum through the ileocecal valve. 2. Ascending Colon, Transverse Colon, Descending Colon, Sigmoid Colon, rectum. B. Function of the Ileocecal Valve 1. Prevents back-flow of fecal material from colon into small intestine. 2. Normally remains mildly constricted. Distension of colon causes contraction of ileocecal valve to delay emptying. 3. Slows emptying of ileal contents into cecum. Prolongs stay of chyme in ileum, and therefore, facilitates absorption. 3. Relaxed by gastroileal reflex (myenteric/PNS reflex), gastrin (increases small intestine motility). 4. Does not control the entry of material from the intestine to the colon. C. Functions of the Colon. 1. 750 - 1000 ml chyme enters colon daily 2. Absorption of water and electrolytes from the chyme. This Occurs primarily in proximal half of colon. 3. Storage of fecal matter until it can by expelled. Occurs in distal half. Approximately 100-150 ml of material defecated daily. D. Movements of the Colon 1. Mixing Movements - Haustrations a. Bulging out like bag-like sacs b. Fecal matter moves slowly analward c. Myogenic; myenteric plexus mediated d. Sluggish (4-6 per min). Each contraction lasts 60 seconds. It takes 15 hours to move across transverse colon. e. Longitudinal smooth muscle is not continuous. You see bulging upon contraction. f. Dig into fecal material to allow maximal absorption of water and electrolytes. g. Regulated by myenteric plexus in proximal colon h. Regulated by PS nerves in distal colon 2. Propulsive “Mass” Movements a. Peristaltic contractions. Gastrointestinal I - #16 Dr. Gwirtz 2/19/03, 11AM Scribe – Matthew Stine Page of 7 b. Usually occur 1-3 times daily, especially 15 min after eating breakfast. c. Initiated by: gastrocolic, duodenocolic reflexes (as soon as stomach fills, reflex stimulation of colon); intense PS stimulation (caused by anger, hostility, fright); overdistension of colon; irritation : enterotoxins (produced by bacteria), parasites, food antigens (food allergies), bile, laxatives d. Transmitted through parasympathetic (pelvic) nerves and myenteric plexus. e. Modified type of peristalsis. f. Persists 10-20 min: if defecation does not occur, new set of mass movements might not recur for another half day or day g. Chemoreceptors & mechanoreceptors in cecum & ascending colon feedback to regulate ileocecal tone 1. controls delivery of chyme into colon. E. Emotions and Colonic Motility 1. Anger and resentment, hostility, “fight or flight” response increase motility - diarrhea. 2. Depression, sadness, long term fear decreases motility – constipation. F. Defecation (Pooing) Reflexes – 2 reflexes in one. Receptors in the rectum sense stretch 1. Mass movement a. forces poo into rectum; rectal distension initiates desire to defecate - reflex reaction is transient. b. Reflex contraction of the rectum and relaxation of the internal (involuntary) and external (voluntary) anal sphincters 2. Intrinsic myenteric defecation reflex a. weak (myenteric) smooth muscle contraction 3. Parasympathetic defecation reflex a. strong 4. Relaxation of external anal sphincter leads to pooage. If contraction maintained, defecation reflex dies out after few minutes. It is a conscious decision. If you choose not to poo, you will not. 5. Defecation reflexes initiate other effects a. deep breath, valsalva maneuver b. increases abdominal pressure to force colonic contents down and help inhibit (relax) external anal sphincter 6. If inhibited, sensation subsides. Reflexes weaken with persistent inhibition. If inhibit too often, constipation results. Frequency of pooing, time of day when it is performed is matter of habit. a. most individuals 5-7 times weekly, after breakfast Gastrointestinal I - #16 Dr. Gwirtz 2/19/03, 11AM Scribe – Matthew Stine Page of 7 b. Some people only poo 2-3 times a week normally, so when assessing whether a patient is constipated or not, you must take an accurate history and take note of normal pooing habits. II. Constipation A. Definition: Slow movement of feces through the large intestine; frequent malfunction of the colon. 1. Often associated with large quantities of hard, dry poo in the descending colon, which accumulates because of the long time available for the absorption of fluid. There is a lot of water absorption. 2. Can result in diverticulosis, hemorroids or other complications. a. Diverticulosis is an inpocketing of the wall of the colon caused by abnormally high intra-abdominal pressures. These pockets can fill with feces and cause irritation, infection or even cancer. B. Symptoms: 1. Depression (decreases motility), restlessness, dull headache, anorexia, nausea, bad breath, coated tongue, abdominal discomfort with heaviness and swelling. C. Causes: 1. Usually due to irregular bowel habits (inhibiting normal defecation reflexes). 2. Overuse of laxatives. Long continuous use of laxatives weakens the defecation reflex. 3. Anal lesions, pain. Pain leads to a decrease in motility in the colon. 4. Diabetes mellitus (autonomic neuropathy). Destruction of parasympathetic NS influence. Diabetes also destroys ganglion cells of myenteric plexus. 5. Hypothyroidism – decreases motility 6. Pregnancy – progesterone decreases motility in the colon. 7. Fear, pain sympathetic stim BF mucus production & motility. Norepinephrine from the SNS causes vasoconstriction, reducing blood flow. D. Hirschsprung's Disease (Megacolon) 1. Most frequent cause is absence of myenteric plexus in sigmoid colon. There are damaged or absent ganglion cells. 2. As a result, neither defecation reflexes nor peristaltic motility can occur through this area, and therefore, the end result is constipation. 3. Constipation is so severe that bowel movements occur only once every week or so, causing accumulation of large quantities of poo in the bowel. One patient on record went over 1 year without his normal time to think and reflect on the day’s activities. Gastrointestinal I - #16 Dr. Gwirtz 2/19/03, 11AM Scribe – Matthew Stine Page of 7 a. This guy had the absolute pleasure of having the rocks of poo in his colon chiseled out by a very lucky surgeon. Good times indeed. 4. Management is difficult; and thankfully, this disorder is not common. a. Now this disease is caught in infancy and treated early before any “hard” problems ensue. E. Treatment of Constipation 1. Dietary (fiber 20-30 gm daily). Fiber increases motility because we lack the necessary enzymes to digest it. Because of that, the fiber pulls water into the colon, loosening the poo and making it easier to pass. 2. Behavioral counseling 3. Laxatives, stool softeners – on a short-term basis only. 4. Digital disimpaction. This does not involve computers, rather it involves fingers; fingers of physicians questioning their choice of specialty. III. Diarrhea = Good Times A. Rapid movement of fecal matter through the large intestine. Can be serious and debilitating due to loss of fluid and electrolytes. 1. A patient can lose up to 12 L of fluid with especially wretched diarrhea. 2. Bacterial (e.g. cholera) infection in the gut can also produce greater secretions, increasing fluid output. B. Causes of Diarrhea 1. Major cause: infection in GI tract (enteritis) a. Enterotoxins, parasites, food antigens, intense PS stimulation, overdistension of colon – increase colon motility. 2. Generalized increased motility 3. Increased rate of small intestinal secretion a. Example: cholera toxin stimulates excessive secretion of electrolytes and fluid from the crypts of Lieberkuhn in distal ileum and colon. i. There is a lot of water in the colon, which is unable to handle very much water. ii. There is also less time for water absorption. 4. Osmotic (malabsorptive) a. fats, cholesterol, lactose, sorbital, laxatives, etc. (any nutrient not absorbed in the small intestine. These nutrients will pull water into the colon. 5. Secretory (deranged electrolyte transport). a. cholera toxin, VIP tumor (causing massive release of fluid into the small intestine), bile salt malabsorption (bowel irritant), neoplasm, bacteria, etc. 6. Abnormal GI motility Gastrointestinal I - #16 Dr. Gwirtz 2/19/03, 11AM Scribe – Matthew Stine Page of 7 a. peristaltic rush, psychogenic (anger, hostility). 7. Exudative (blood, mucus, pus) a. viral, bacterial – can increase mucus secretions. IV. Vomiting A. Means by which upper GI tract rids itself of its contents when excessively irritated, overdistended or overexcited. B. Stimuli: distention, inflammation or irritation of duodenum; abnormal sensory signals outside GI tract (heart (angina), kidneys, eyes, nose, psychic (bad smells), pancreas, uterus, testicular pain, semicircular canals) C. Mechanism: 1. Afferent signals sent via vagus and sympathetic nerves to vomiting center in medulla for processing. 2. Efferent signals mediating vomiting sent to upper GI tract, diaphragm, abdominal muscles. 3. Vomiting center coordinates input to produce a preprogrammed emetic response. a. CTZ (chemoreceptor trigger zone), vestibular system, cerebral cortex, thalamus, hypothalamus, peripheral sites 4. Vomiting can also be caused by nervous signals arising in areas of the brain outside of the vomiting center, such as the chemoreceptor trigger zone (CTZ), which is next to the vomiting center. a. CTZ (receptors) stimulated by: drugs (apomorphine, morphine, digitalis, ipecac), rapid changes in direction of motion (seasickness, car, swing), GI irritation (radiation, chemotherapeutic agents, toxins). D. Chemoreceptor Trigger Zone 1. Lies on the floor of 4th ventricle - outside the blood brain barrier a. Senses blood borne chemicals that induce emesis 2. Sends afferents to vomiting center when stimulated by emetics or motion sickness a. via H1 ( Histamine) & cholinergic receptors in vestibular system. Antihistamines can be a treatment for nausea. 3. Vomiting center then initiates emesis (vomiting) E. Vomiting Act – Nausea – Initial event. 1. Conscious recognition of subconscious excitation in an area of the medulla closely associated with or part of the vomiting center 2. Prodrome of vomiting. Can be caused by irritative impulses coming from the GI tract, impulses originating in lower brain associated with motion sickness, or from cerebral cortex to initiate vomiting F. Vomiting Act - Retching 1. Antiperistalsis (reverse peristalsis, towards oral end) occurs in early stages; may begin as far down as the ileum. The start point for this depends on the location of the irritation. 2. Stimulus - overdistension, especially in duodenum Gastrointestinal I - #16 Dr. Gwirtz 2/19/03, 11AM Scribe – Matthew Stine Page of 7 3. A single antiperistaltic wave travels backward up the intestine 23 cm/sec; pushes contents up to duodenum and stomach in 3-5 min. - this wave begins "retching" process 4. “Retching" process = contraction of diaphragm agains a closed glottis, also known as a dry heave. a. causes strong negative intra-thoracic pressure, which opens the esophagus. b. LES then opens by relaxation G. Vomiting Act 1. During vomiting, strong contractions in duodenum and stomach, and relaxation of LES, move contents into esophagus. 2. Vomiting then involves abdominal muscle contraction to increase intragastric pressure and to expel vomitus out of the mouth. 3. Deep inspiration 4. Open upper esophageal sphincter 5. Close the glottis 6. Close the posterior nares (hope so!, even though this might be endlessly funny to see happen to someone else) 7. Diaphragm and abdominal muscles contract 8. Lower esophageal sphincter relaxes 9. Expulsion of gastric contents upward through the esophagus H. Consequences of prolonged vomiting 1. There are physical, metabolic and psychological consequences for consistent, prolonged vomiting. Just be aware of the physical, and psychological signs listed in the notes. There will not be any questions on the metabolic pathways covered in the flow chart in the slides. That will be covered in renal. Know though, that there are electrolyte imbalances (hypokalemia, hyponatremia, and hypovolemia). 2. Causes severe problems in fluid and electrolyte balance a. loss of H+, K+ causing metabolic alkalosis and hypokalemia. There is also loss of Na+, causing hyponatremia. 3. Anti-emetics include: a. antihistamines (act on H1 receptors in vomiting center and cortex and in vestibular system) b. anticholinergics – act cerebrally on vomiting center and CTZ. c. phenthiazines V. Sources of Gases, Flatulence, Bad Smells (Flatus) A. Swallowed air – usually burped on out of stomach through mouth, more so if you are male. B. Gases released due to bacterial action on food (stachyose, sorbital, lactulose), especially in the colon. Bacteria act on undigested nutrients, which releases gases. Gastrointestinal I - #16 Dr. Gwirtz 2/19/03, 11AM Scribe – Matthew Stine Page of 7 C. Diffusion of gases from blood into GI tract: oxygen, nitrogen, carbon dioxide. Gases can also move from the GI into the blood. D. Emotions – such as depression (inhibit GI motility and allow gas to accumulate). E. Bowel obstruction – torsion (twisting), tumors, hernias allow gas to accumulate. F. Post-operative decrease in GI motility allows gas to accumulate G. Inflammatory disease (ulcer, colitis) VI. Composition of Gases in the GI Tract A. Stomach: 50 cc. 1. contains nitrogen, oxygen, carbon dioxide from swallowed air, foods (carbonated beverages) and most of it is belched out. B. Small intestine: 1. Not much gas because it passes through very rapidly to the colon. 2. Contains contains nitrogen, carbon dioxide, hydrogen, methane no oxygen 3. As gas passes through small intestine, it produces borborygmi (abdominal sounds) a rate of 8-12 per min. a. You can auscultate to hear these sounds, and this is often done to assess normal intestinal motility. C. Large intestine – mostly from bacteria working on undigested food. 1. Contains: nitrogen, carbon dioxide, methane, hydrogen, hydrogen sulphide - no oxygen 2. Explosive! a. Helps guys get the ladies. 3. Expelled periodically a. 14 times or so daily. D. Food Sources 1. Beans, cabbage, broccoli, brussel sprouts, cucumbers, radishes, raisins, onions, cauliflower, corn, vinegar 2. Milk products in lactase deficiency 3. Fermentation of foods by bacteria E. Amount of Gases Expelled by GI Tract – Flatus 1. Amount: 7-10 liters of gas enter large intestine daily 2. Expel 600 ml daily with a normal diet (14 X daily) 3. Remainder of gas is absorbed through intestinal mucosa 4. Normally, we do not recognize that we are even doing it. This is known as silent, but deadly. 5. Many other people in your surrounding vicinity recognize that you are doing it, so STOP!!