Potential adverse effects to hypothermia may also be consequences
advertisement
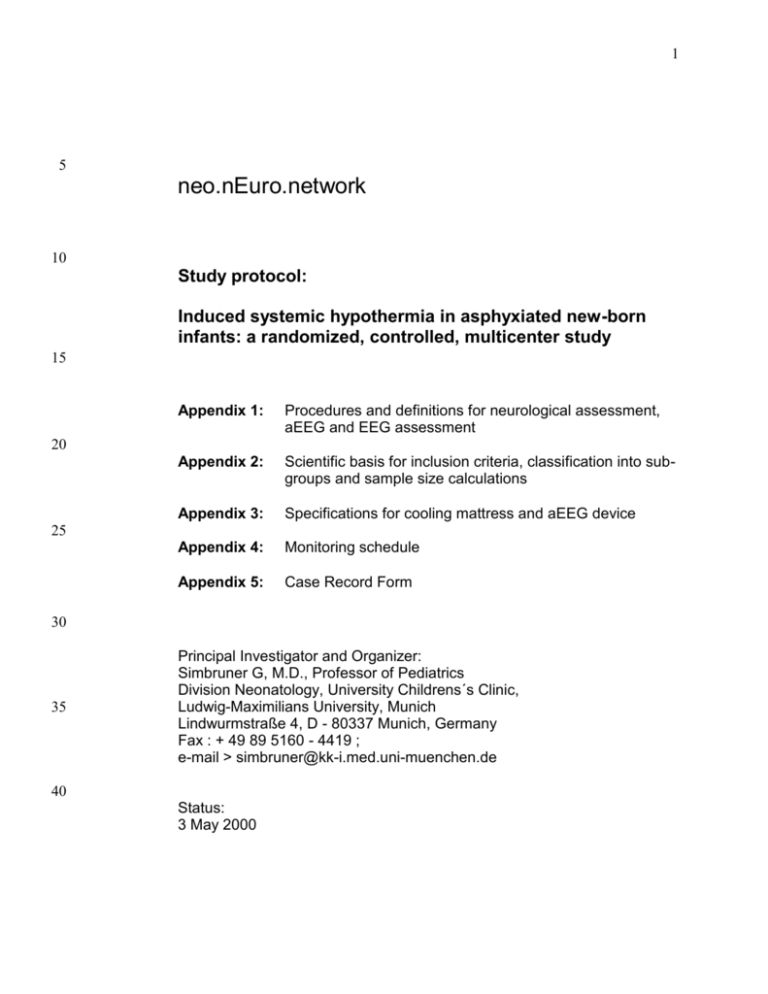
1 5 neo.nEuro.network 10 Study protocol: Induced systemic hypothermia in asphyxiated new-born infants: a randomized, controlled, multicenter study 15 Appendix 1: Procedures and definitions for neurological assessment, aEEG and EEG assessment Appendix 2: Scientific basis for inclusion criteria, classification into subgroups and sample size calculations Appendix 3: Specifications for cooling mattress and aEEG device Appendix 4: Monitoring schedule Appendix 5: Case Record Form 20 25 30 35 Principal Investigator and Organizer: Simbruner G, M.D., Professor of Pediatrics Division Neonatology, University Childrens´s Clinic, Ludwig-Maximilians University, Munich Lindwurmstraße 4, D - 80337 Munich, Germany Fax : + 49 89 5160 - 4419 ; e-mail > simbruner@kk-i.med.uni-muenchen.de 40 Status: 3 May 2000 2 45 Study protocol : Induced systemic hypothermia in asphyxiated new-born infants: a randomized, controlled, multicenter study. ________________________________________________________________ 50 55 Study Group Participants in Germany and other European Countries within the framework of the ”neo-nEuro-network” (abbreviated n.n.n), an non-juridal association of neonatologists interested in neurological and neuro-intensive care investigations. 60 Prinicipal Investigator: Simbruner G, Division Neonatology, Ludwig-Maximilians University, Munich Fax : + 49 89 5160 - 4419 ; e-mail > simbruner@kk-i.med.uni-muenchen.de 65 70 75 80 Scientific Committee of the nnn Hypothermia Study: Blennow M, Huddige Hospital , Huddige, Sweden, Gaus W, Univ Ulm, Ulm, Germany Greisen G, Univ Copenhagen, Copenhagen, Denmark Obladen M, Charite, Humboldt Univ, Berlin, Germany Pohlandt F, Univ Ulm, Ulm, Germany Simbruner G, LMU, Munich,Germany Thoresen M, Univ Bristol, Bristol , UK Zupan V, Univ Paris, Paris, France Biometry: W. Gaus, Department of Biometry and Medical Documentation University of Ulm, Germany Fax: +49 731 50-26902; e-mail: wilhelm.gaus@medizin.uni-ulm.de Regional co-ordinators (Status 12 April, 2000): Copenhagen, Denmark: Gorm Greisen Munchen, Germany: Georg Simbruner Paris, France: Veronique Zupan 85 90 Acknowledgement : We thank the principal investigator Peter D Gluckman, Auckland, New Zealand of the Olympic Medical Brain Cooling Trial and Olympic Medical for providing a copy of that protocol. Inclusion and exclusion criteria and the primary endpoint is identical in the two protocols. The brain cooling trial uses a cooling cap and a target body temperature of 34.5C whereas we will use systemic cooling to 33.5C and all patients receive morphine for pain and sedation. We think that the results from the two trials can add up to 3 95 document a potential benefit of hypothermia as well as suggest a difference between the two approaches. I thank Professors Azzopardi D and Edwards DA for also providing insight into their study protocol. Synopsis 100 105 110 115 This randomized, controlled multicenter study aims to determine whether inducing systemic hypothermia in birth-asphyxiated new-born infants born at term increases the chance of survival without severe neurodevelopmental handicap. Secondary objectives are to determine whether the treatment benefit is greater in milder rather than more severe asphyxia, and whether systemic hypothermia is associated with significant sideeffects. New-born infants with a gestational age of > 36 weeks , asphyxiated at birth, who show evidence of encephalopathy and who have abnormal EEG within 6 hrs of postnatal age, will be randomized to hypothermia or to normothermia. Hypothermia (target rectal temperature 33.5°C) will be induced by a cooling matters, perfused with water. Hypothermia will be maintained for 72 hours. Infants in both groups will receive morphine at a sedative and analgesic dosage. Neurological assessment will be done at 7 days, 6 and 18 months. Further, at 18 months the Griffith General Quotient will be assessed. The primary outcome is (1) death, or (2) inability to sit unsupported, or (3) Griffith GQ < 85, or (43) bilateral cortical blindness at 18 months or a combination thereof. The statistical analysis will examine whether the hypothermia and control group differ in their proportion of infants surviving without disability . 120 Background Ethical considerations. 125 130 135 Severe birth asphyxia results in brain damage and death or lifelong handicap. The scientific community so far failed to provide an effective protective or therapeutic intervention. Controlled mild hypothermia is the best candidate for a post-asphyxia intervention. Hypothermia has been proven effective in several animal species. Extensive clinical experience with short term, deep hypothermia exists from heart surgery practice. Some clinical experience exists with long-term moderate hypothermia. Although hypothermia may have side effects, even if serious, they are likely to be acute, whereas the benefits are likely to be long term. It is therefore reasonable to proceed to a randomized controlled trial. A trial of selective head cooling is under way in New Zealand, USA, Canada and the UK. The present protocol is sufficiently similar and sufficiently different to the Olympic Medical Head Cooling Trial to be likely to add significantly to the evidence provided by that study. The major ethical concern is the limited possibility to obtain truly informed, free consent by the parents. There is no solution to this problem. It will be the duty of the investiga- 4 140 tors to remain sensitive to parental wishes, to obtain the best possible consent, and to offer a high level of information to the parents throughout the study. Epidemiolgy. 145 The incidence of asphyxiated full-term infants still ranges between 2 and 4 infants per 1000 deliveries in high income countries (1, 2) and may be significantly higher in low income countries. Birth asphyxia results in longterm neurological sequelae in up to 20% of infants, if moderate and in up to 100% of infants, if severe. Birth asphyxia causes high costs for posthospital care and severe suffering of families (3, 4). 150 Systemic and selective hypothermia. 155 160 165 From animal experiments a vast body of knowledge demonstrates that a low intraischemic brain temperature or lowering brain temperature by 2-4 °C post ischemia may protect the asphyxiated brain from neuronal damage and cell death and improve long term neurological outcome (5-7, 47). In factually all animal experiments, hypothermia of the brain was induced and associated with hypothermia of the rest of the body. Selective brain cooling while maintaining normal rectal temperature was demonstrated to be possible in new-born piglets (8), but evidence of long lasting effects or superiority to systemic hypothermia is still lacking. In analogy, all human hypothermia studies in adults were based on systemic body cooling. Mellegard P. demonstrated that effective selective cooling of the brain was not possible in adult neurosurgical patients (9). Simply heat balance calculations or complex mathematical model indicate, that selective brain cooling is only possible if one accepts extreme temperature gradients across both, body and brain (10). EFFECTS 170 175 Hypothermic interventions have five domains which appear to determine the balance between protective and adverse effects: (1) temperature range of and profile within brain tissue, (2) time relation of occurrence of insult to inducing hypothermia, (3) duration of cooling, (4) degree of severity of the neuronal injury, and (5) developmental and biological age of the individuum subjected to hypothermia. Temperature range. 180 185 Though a controversial issue, most animal studies suggest, that the optimal brain temperature for neuroprotection ranges between 32 and 34 °C. In some studies mild hypothermia (34°C) was found to mitigate neuronal damage to a larger extent than moderate (32 - 28°C) or deep hypothermia (28 - 17°C) (11,12). In other studies, mild hypothermia was as effective in reducing biochemical and histological markers of neuronal injury and in reducing abnormal behaviour (12 - 15). Time relation between insult and hypothermia. 5 190 195 Hypoxic-ischemic injury resulting in encephalopathy evolves in two phases , the primary and secundary energy failure. The primary event triggers a series of biochemical and immunological responses which are responsible for the pathophysiology of the second phase and for the final manifestation of cerebral damage. These biochemical and immunologic responses include release of cytotoxic neurotransmitters (13), oxygen radicals (16), inflammatory mediators and signals inducing apoptosis (17). It appears natural that an immediate or earlier intervention might be more successful than delayed ones. In animal experiments, hypothermia induced at 1 to 5.5 hours were more effective compared to later inductions (14,18 -20). The neuroprotective effects diminishes and disappears if cooling is delayed beyond 6 hours (14, 20) Duration of hypothermia. 200 205 210 215 Duration of cooling clearly relates to short and long term outcome of asphyxia (7, 14, 20), longer periods being more effective than shorter periods of hypothermia. The duration of hypothermia ranges up to 72 hours in asphyxiated animals, kept at 35°C (20). In human trauma patients a hypothermia of about 33°C was applied for 24 hours (21). Asphyxiated human new-borns have been kept at a rectal temperature of 35.5 °C for 72 hours (22) and at a nasopharyngal temperature of 34.5° for an average of 78 hours (23) Severity of the injury and developmental stage of the injured. Scarce data in animal and human studies indicate that the neuroprotective impact of hypothermia is stronger in mild than severe neuronal injury (18, 21, 24). Few and controversial studies are available which investigated the effectiveness of hypothermia on neuroprotection in dependence of developmental age (25, 26). However, in rats of various developmental stages, brains of immature rats were found to be less resistant to hypoxia (26). The neonatal brain undergoes drastic neuronal remodelling through apoptosis before and after birth. Different remodelling and healing capacity in developing individuals might be responsible for the fact, that similar therapeutic procedures like ECMO generally produce better outcome result in new-born infants than in pediatric or adult patients (see ECMO registry). ADVERSE EFFECTS 220 225 230 Hypothermia on one hand can be the manifestation of an underlying disease and on the other hand the result of an accidental or actively induced heat loss. Hypothermia causes a wide spectrum of effects on all organ systems. We suggest to classify these effects into (i) physiological changes, which are reversible. Amongst them, low heart and breathing rate immediately reverse to normal, when normothermia is reinstituted , (ii) pathologic alterations, which are reversible, probably represent some health risks, but have not shown to result in irreversible damage, either without or with treatment . Amongst them hypoglycemia, altered coagulation states or low platelets, and (iii) alterations which result in irreversible damage despite attempts of or due to lack of effective treatments, amongst them occurrence of intracranial tissue bleeding or untreatable cardiac arrest due to arrhythmias (although arrhythmias are not reported to occur at mild hypothermia). Difficulties in assessing the hypothermic effects arise from possible combinations of causes, their manifestations and their consequences. 6 235 240 245 250 255 260 265 270 Accidental hypothermia and hypothermia, caused by disease or therapy, is known to affect factually all organ systems (27, 28). Some of these effects are reversed at normothermia without causing disease or impairment. Other effects like arrhythmias, coagulation disorders or infections may have long term sequelae (29 - 34). Accidentally cooled prematures with a rectal temperature < 34 °C at admission suffered from coagulation disorders, a high incidence of hemorrhage and mortality, whilst another group of newly born prematures with an average rectal temperature of 31 ± 2.7 °C at admission exhibited only transient thromobcytopenia and renal failure (31,32). In controlled clinical trials on adult trauma or cardiac arrest patients , induced mild to moderate hypothermia for up to 24 hours resulted in some beneficial effects (21,35, 36) without any significant, irreversible side-effects. In a study by Metz et al. on ten traumatized adults, subjected to moderate hypothermia for 24 hours, adverse effects such as temporary decrease of cardiac index, thrombocytes and creatinine clearance, and an elevated serum lipase activity were reported (37). Whole body cooling had been applied to asphyxiated mature human new-borns after delivery by Westin (38) in the sixties. Several trials treating asphyxiated term infants with hypothermia followed without reporting details on immediate effects or complications (39). Head cooling in 12 asphyxiated new-borns to two temperature levels (six at 36.536.0°C and six at 35.5 - 35.9°C) was reported not to result in any adverse effects which could be specifically attributed to hypothermia (22). Incidences of adverse side effects in asphyxiated new-borns cooled to 34.5° nasopharyngeal temperature for 3 1/2 days were not different from those asphyxiated but kept at normal body temperature (23). A randomized, controlled study on the effect of mild hypothermia (two arms: control vs. head cooling method) is in process by Gluckman & Wyatt in cooperation with Olympic Medical , Seattle, USA with the following known characteristics: 1) Hypothermia induced by external head cooling (cooling cap Olympic Medical) 2) Hypothermia maintained for three days 3) Inclusion of moderate and severe cases of asphyxia (aEEG < 5 uVolt) with an estimated chance of death or disability of 80% 4) Regulatory endpoint Trectal 34. 5± 0.5 °C 5) Study endpoint : combined rate of mortality and neurodevelopmental impairment at 18 month of age. 7 275 280 This study will differ from the one of Gluckman & Wyatt in the following respects: 1) Systemic cooling without any efforts to achieve a temperature difference between head and rest-of-the body by cooling the head and to add radiative heat to the rest-of-the body. 2) Regulatory end-point is T rectal 33-34°C, a mean of 33.5 °C 3) Routine analgesia and sedation in both groups with morphine. 4) Prospectively planned assessment of treatment effect in mild to moderate vs. severe asphyxia. 5) Option of cooling before transport 6) Trectum measured at 2-3 cm from anus, thus allowing measurements with ubiquitous available rectal thermometers. Study objectives 285 290 The objectives of this randomized, controlled, multicenter study are 1) to determine whether inducing systemic hypothermia in birth asphyxiated new-born infants at term decreases the proportion of infants who die or survive with severe neurodevelopmental handicap when compared to new-born infants whose body temperature is maintained within the normal range, 2) to determine whether the protective effect of hypothermia is related to the severity of asphyxia and 3) to evaluate the safety of hypothermia. Hypotheses 295 300 Primary: Hypothermia at 33-34°C, induced by a cooled mattress for three days in severely asphyxiated new-born infants, reduces the risk of death or severe neurodevelopmental handicap at 18 - 21 months. Secondary (a): Hypothermia reduces neurodevelopmental retardation (measured by Griffith GQ) at 18 - 21 months to a significant larger extent in the group with moderately abnormal EEG compared to the group with severely abnormal EEG. Secondary (b): Systemic hypothermia in the range 33-34°C for 72 hours is safe. 305 Study design 1. Randomized, controlled, multicenter neurodevelopmental outcome. 2. The protocol and data acquisition is designed to provide a common minimal dataset to test the primary and two secondary hypotheses by participation of regional study groups. The common statistical analysis will be carried out by Prof. W. Gaus, Department of Biometry and Medical Documentation, University of Ulm, Germany. 3. Statistical analysis will be based on intention-to-treat. 310 315 trial with blinded assessment of 8 4. Safety and interim analyses at 1/4, 1/2 and 3/4 of patient recruitment in a fixed sample design. A safety monitoring committee will be headed by Prof. F Pohlandt, Dept of Paediatrics, University of Ulm, Germany. Severe adverse events, likely to be related to hypothermia must be reported to the Department of Biometry and Medical Documentation, University of Ulm, Germany, by fax on the same day. 5. Regional co-ordinators are responsible for data quality. As a minimum, all entries in patient record forms must be dated and signed, and all participating centers must be visited by a regional monitor once per year when a sample of case record forms must be checked against patient charts. This quality control must be documented. 6. Inclusion of new patients must be reported to the regional co-ordinator by fax on the same day. 7. Individual centres are encouraged to add on studies provided this does not interfere with the objectives of this protocol. 8. Centres involved in testing of new, unproven and unpublished neuroprotective strategies for asphyxiated infants cannot participate in the study. 9. Publication will be in the name of ‘neo-nEuro-network’ with a detailed acknowledgement of all contributions. 320 325 330 335 10. Publication of add-on studies can be done as relevant with the mention of the participation in the neo-nEuro-network. Statistics which can be used to test the hypotheses of this protocol must be avoided. 340 PATIENT SELECTION 6.1 Inclusion Criteria The infant will be assessed sequentially by criteria A, B and C listed below: A. Evidence of severe birth asphyxia in infants >36 weeks gestation admitted to the NICU: ONE of the following 345 350 355 Apgar score of < 5 at 10 minutes after birth Continued need for resuscitation, including endotracheal or mask ventilation, at 10 minutes after birth Acidosis defined as either umbilical cord pH or any arterial pH within 60 minutes of birth <7.00 Base Deficit 16 mmol/L in umbilical cord blood sample or any blood sample within 60 minutes of birth (arterial or venous blood) B. Evidence of encephalopathy (assessed by certified study personnel): Moderate to severe encephalopathy consisting of altered state of consciousness: lethargy, stupor or coma, and at least one or more hypotonia, abnormal reflexes including oculomotor or pupillary abnormalities, an absent or weak suck or clinical seizures. C. Evidence of moderate-to-severe neurophysiological dysfunction: At least 30 minutes duration of amplitude integrated EEG or standard EEG recording that shows abnor- 9 mal background EEG activity or seizures (see definitions : Appendix 1). The aEEG or EEG may be performed from one hour of age. aEEG or EEG should be read by certified study personnel. Classification of the aEEG is according to al Naqeeb et al. (42). The classification of the EEG is according to Lamblin et al (45). The aEEG or EEG 30 min following IV anticonvulsant therapy, e.g. phenobarbitone should not be used for classification. 360 Exclusion Criteria 365 Infants expected to be >5.5 hours of age at the time of randomization. Prophylactic administration of high dose anticonvulsants (e.g. >20mg/kg phenobarbitone). After trial entry phenobarbitone or other anticonvulsant therapy may be given as clinically indicated to treat seizures (see co-treatment below). Major congenital abnormalities, such as diaphragmatic hernia requiring ventilation, or congenital abnormalities suggestive of chromosomal anomaly or other syndromes that include brain dysgenesis. Imperforate anus (since this would prevent rectal temperature recordings). Evidence of head trauma or skull fracture causing major intracranial hemorrhage. Infants <1,800 g birth weight. Head circumference <(mean2SD) for gestation if birth weight and length are >(mean2SD). Infants ”in extremis” (those infants for whom no other additional intensive management will be offered in the judgement of the attending neonatologist). Record in detail reason for exclusion. Overt bleeding 370 375 380 If all inclusion and no exclusion criteria are met, the infants are eligible for randomization. 385 STUDY PROCEDURES Recording and Classification of aEEG or standard EEG (Appendix 1) 390 395 The aEEG will be recorded with a Lectromed Cerebral Function Monitor and the use of needle electrodes inserted at an exact distance of 5 cm apart from each other at the parietal regions. The recording speed is 1mm/min. The classification of the aEEG is based on the publication of Niran al Naqeeb et al. (ref 42 : Pediatrics 1999; 103; 12631271) which yields two subgroups: Moderately abnormal aEEG designates mildly to moderately asphyxiated new-borns and suppressed aEEG severely asphyxiated newborns. This classification is used for subgroup analysis. 10 400 The standard EEG is recorded according to the International 10-20 Classification. The classification of the EEG is based on the publication of Lamblin MD et al. (ref 45: Neurophysiol Clin 1999; 29: 123 - 219) Consent 405 Randomisation is done after informed consent from at least one parent. Consent may be written or verbal and documented by a wittness. Entry criteria and other parts of the minimal data set is entered in the Case Record Form. 410 Temperature control 415 420 All infants are nursed in an open care unit (cot, radiant heater unit, bed etc). If relevant, randomisation may be done in a local hospital and treatment started and continued during transfer to a study center, provided temperature control and documentation is adequate. Body temperature is measured rectally, at least 2 cm from the anus, preferentially with a permanent probe . Control Group 425 Infants randomized to the control group are treated according to present standards of postnatal care with the aim of achieving a normal body temperature i.e. T rectum of 37°C (range: 36.5 to 37.5°C) . All handling and treatments otherwise should be identical to the one of the hypothermia group. Hypothermia Group 430 435 Infants randomised to the hypothermia group will be nursed naked on a cooling mattress (cooling device and matrass see: Appendix 3) which is perfused by circulating water at a variable temperature and covered by normal linen. The infant will have a diaper around the lower half of the abdomen. The rectal temperature is targeted at 33.5 °C (range of 33 to 34 °C). The duration of hypothermia is 72 hours. Induction of hypothermia 440 Target temperature should be achieved within 60 min. The water temperature should initially be set to 10°C. The body temperature should be checked every 10 min. If the temperature drop is insufficient the cooling mattress should be wrapped around the infant or cool packs be applied. Maintaining hypothermia 445 11 Normally a mattress temperature of 32-33°C will maintain the temperature within range. The temperature must be recorded every hour. Be prepared to reduce matters temperature in case of seizures, to increase it at initiation of mechanical ventilation etc. 450 455 Rewarming Rewarming is started by stopping the cooling of the mattress. Check the temperature every hour. The infant should reach a normal rectal temperature in 6 -12 hours after stopping cooling. If the infant does not warm up spontaneously, heat may be added from a radiant heater. Check the temperature more frequently. If the temperature rises more than 0.5°C per hour, the cooling mattress should be used to control the rise. After rewarming 460 Temperature is managed according to routine care. Beware of rebound hypothermia. Co-treatments 465 1. All infants in the hypothermia and control group will receive morphine at 0.1 mg/kg every 4 hours during the first three days as brain edema might and as cold does induce discomfort, restlessness, anxiety and irritation (References: in Physiological and Behavioral Temperature Regulation. Chapter 57. Eds. Hardy JD, Gagge AP, Stolwijk JAJ, 1970 Charles C Thomas Publisher) and pain (Reference: Maria Fitzgerald, London, at 11 Anual ESIC Congress, Stockholm, 1998). Hypothermia increases stress hormones (48). 2. In ventilated infants PCO2 should be maintained between 40 and 60 mmHg. In spontaneous breathing infants hyperventilation will not be treated, but hypoventilation with PCO2 > 60 mmHg will be treated. 3. All other treatments will be given according to clinical routines 470 475 Discontinuing hypothermia before 72 hours 1. Parents withdraw consent. 480 2. The attending neonatologist decides, if possible after consultation with the regional co-ordinator (Record reason for withdrawal). Potential reasons might include for example bleeding, thrombosis, pulmonary hypertension or arrhythmia which is difficult to control, or continued inability to maintain rectal temperature in the desired range. 485 3. Need for ECMO. If hypothermia is discontinued prior to 72 hours, rewarming will be done according to clinical routine. The follow-up procedures will be done unless the parents withdraw their permission for this. 490 Improvement on continuous aEEG or standard EEG recording, after trial entry, is not an indication for discontinuing treatment. 12 Follow-up 495 7 ± 1 days postnatal : Neurological assessment by the Thompson score (ref. 41) and brain ultrasound. 6 months: Bodyweight, length, and head circumference and gross neurological assessment (blinded assessment by certified study personnel). 500 12 months: Parental questionnaire. 505 18 month: Neurological examination and determination of Griffith General Quotient (GQ) (blinded assessment by certified study personnel). Persistent neurological signs consistent with a central motor deficit are classified according to five level classification of Palisano et al (40). Primary Outcome Measure 510 Survival at 18–21 months of postnatal age free of severe neurodevelopmental handicap. Severe neurodevelopmental handicap is defined as one or more of 515 Neurological deficit with a functional score of 3-5 as defined by Palisano et al. (40), i.e. sitting only with low back support or worse. Griffith General Quotient of less than 85 (i.e. < 2 SD) Severe bilateral cortical visual deficit (no reaction to a threat to the eye, which has a clear anterior chamber and normal fundi) 520 Secondary outcome measures 1. Thompson Score (ref. 41) at day 7 2. Head Circumference at 6 months 525 13 Outcome measure for Subgroup Analysis 530 Subgroup analysis of infants with (1) moderately abnormal and (2) suppressed aEEG in order to determine which of these subgroups is more responsive to hypothermia treatment. Griffith General Quotient will be used as outcome measure . 535 ADVERSE EFFECTS Definitions 540 Potential adverse effects to hypothermia may also be consequences of asphyxia, and thus statistical testing is essential to determine whether cooling may be a contributing factor. Severe adverse events that in particular may be due to hypothermia will be immediately reported to the Data Safety Monitoring Committee (DSMC) . They are: Cardiac arrhythmia Severe hypotension despite full inotrope support and volume correction Major venous thrombosis not related to an infusion line 545 Severe bleeding, e.g. from the lungs or in the brain Other complications that may occur during the first 7 days of life may include: Death Electrocardiographic evidence of cardiac arrhythmias or myocardial ischemia or hypotension <40mm Hg Coagulopathy (clinical bleeding with abnormal clotting studies, consistent with disseminated intravascular coagulation or hepatic coagulopathy) Abnormal renal function (urine output <0.5 ml /kg/hour for >24 hours after birth, maximum serum creatinine (>0.09 mM). Hyponatremia (<130 mM), hypokalemia (<3.5 mM). Bone marrow depression (platelet count <100,000 per mm 3) Elevated liver enzyme levels (AST >200 IU, ALT >100 IU) Metabolic acidosis (BE <-5) following after entry into study Need for mechanical ventilation Need for nitric oxide Need for ECMO Systemic infection (blood, CSF or urine cultures) 550 555 560 14 565 Hemoconcentration (increase of hematocrit by 20% or more) not associated with transfusions Hypoglycemia (<2.6 mmol/L) Hypocalcemia (<2 mmol/L) adjusted for albumin levels, or <1.0 mmol/L on ionised calcium measurement. Adverse events related directly to cooling device: Difficulties in temperature control 570 STATISTICAL ANALYSIS 575 580 Randomization Randomization will be stratified for hospitals as well as for the severity of asphyxia (moderate/severe). Before the start of the trial, randomization plans will be established in the Department of Biometry and Medical Documentation of the University of Ulm, Germany, for all hospital. The resulting group assignment for each consecutive patient will be concealed in sealed envelopes. The envelopes are identified by Title of study : Induced systemic hypothermia... Name of the hospital 585 moderate / severe asphyxia A patient number. Each participating hospital will receive two piles of envelops, one pile for moderate asphyxia and one pile for severe asphyxia. 590 Envelopes have to be used by increasing patient number, i.e. the envelope with the lowest patient number first. 595 600 The envelopes will contain a self adhesive label with title of study, name of the hospital, the degree of asphyxia (moderate or severe), the patient number and finally the treatment (hypothermia or control). This label has to be placed on the case report form on admission of a patient to the study. Then, a filled out form with the label has to be transmitted by fax to the regional co-ordinator within 24 hours. 15 Statistical Evaluation 605 610 615 The primary null-hypothesis is: ”The proportion of surviving infants without severe neurodevelopmental handicap at the age of 18-21 months is not reduced by hypothermia”. The test is one-sided since it is not relevant to confirm statistically whether hypothermia increases the proportions of death or handicap. The statistical evaluation will be performed on all admitted patients (full sample analysis, intent to treat analysis). The result will be summarized by a 2 x 2 contingency table (outcome by group); Fisher’s exact test (level of significance: 5%) will be used to compare the treatment groups. This test is confirmative. The statistical evaluation of the data will include all necessary descriptive measures. The Griffith General Quotient will be compared using a Wilcoxon test for two parallel groups. All further secondary outcome measures will be evaluated using the appropriate statistical procedures. These tests are one-sided, too, with a level of significance of 5%. The levels of significance will not be adjusted for multiple testing. Hence, these tests are only intended for exploration. At regular intervals, interim analyses will be carried out (see below), their maximum number is 3. 620 Sample size (see APPENDIX 2) 625 630 The sample size of 2 x 75 patients has been determined under the following assumptions: 60% of the patients suffer from moderate asphyxia, 40% from severe asphyxia. Further, 75% of the patients with moderate asphyxia and 95$ of the patients with severe asphyxia will be dead or handicapped after 18-21 months in the control group. If 40% of these cases can be prevented by hypothermia under moderate asphyxia and 10% under severe asphyxia, the overall proportion of dead or handicapped will be 83% in the control group and 61% in the hypothermia group. These assumptions lead to a sample size of 61 patients per group when testing a one-sided hypothesis at a level of 5% with a power of 80% under the given treatment effects. It is realistic to assume that 20% of infants will be lost to follow up. Thus 75 patients will have to be recruited in each group. 635 Data Monitoring and Interim Analysis DATA COLLECTION & MONITORING 640 645 650 Data collection and monitoring of study centres is done by the regional co-ordinators. Data will be passed on to the Department of Biometry and Medical Documentation, University of Ulm, for analysis. Safety and interim analyses will be done when 1/4, 1/2 and 3/4 of the patients are recruited. Severe adverse effects will be reported on the same day to Ulm. Safety data and Interim analysis will be reviewed by the Safety and Data Monitoring Committee (Pohlandt F, Ulm and Versmold H, Berlin and N.N). Regional co-ordinators will meet every 6 months to maintain consistency of procedures when documentation of site visits and sample chart reviews by regional co-ordinators will be reviewed by the principal investigator. 16 INTERIM ANALYSIS 655 660 665 The estimated mortality in the control group is 20% to 30% (assuming a mortality in moderate asphyxia of about 5% and in severe asphyxia of 60%, further a case mix of 60% moderate and 40% severe asphyxia).The majority of deaths after severe birth asphyxia are a consequence of brain damage, and occur within the first week of life. This means that the study hypothesis, assuming a reduction in adverse outcome (death and handicap) of about 30%, includes an expectation of reducing death rate from 20 to 15%; this is a difference of 5% death before 7 days. The interim analyses will be aimed at detecting strong evidence against this. Furthermore, the adverse effects of cooling are recorded within 7 days of life. Safety analysis will compare adverse effects in the hypothermia and control groups. Interim analysis will be done when 40, 75 and 115 of the patients in each group have been recruited and 7 day data is available. 670 675 If the interim analyses show that it is highly unlikely (p < 0.0025 in the first analysis, p < 0.005 in the following two interim analyses) that the mortality will be reduced by an absolute difference 5% or if safety analysis shows that it is highly likely (p-values as above) that hypothermia is associated with increased number of severe adverse effects, premature stopping of the trial will be considered by the Data Safety Monitoring Committee. If the trial is stopped prematurely the patients already included in the study will be followed up as scheduled by this study protocol. 680 Final Analysis 685 690 695 Final analysis will be based on intent-to-treat and carried out after follow-up is closed for all patients on study. The analysis will include Source data listing An elementary descriptive analysis of all variables observed Assessment of data quality achieved Description of study patients Assessment of drop-outs and comparability of groups Evaluation of efficacy including scheduled subgroups analysis Evaluation on adverse events, tolerability and risks of hypothermia Explorative analysis if further interesting results are supposed Biometrical assessment on validity of study results 17 700 In case there will be a serious proportion of drop-outs the most important parts of the analysis have to be done for all admitted patients (full sample analysis) as well as for those patients valid for efficacy. Financial Support 705 G. Simbruner will file an application at the German Federation for Research (Deutsche Forschungsgemeinschaft) to finance insurance, 1/2 post for a statistician, 1 post for data monitoring doctor, and up to 10 Lectromed Ceerebral Function Monitors to increase the number of participants in Germany. Other regional co-ordinators will have to obtain their own funds to fulfil their roles. 710 715 LITERATURE 1 Finer NN, Robertson CM, Richards RT, Pinnell LE, Peters KL. Hypoxic-ischemic encephalopahty in term neonates: Perinatal factors and outcome. J Pediatr 1981; 98: 112-117 2 Thornberg E. Birth asphyxia: incidence, clinical course and outcome in a Swedish population. Acta Paediatr 1995; 84:927-932 3 Robertson CM, Finer NN,Grace MG. School performance of survivors of neonatal encephalopathy associated with birth asphyxia at term. J Pediatr 1989; 114: 75360 4 Shankaran S, Woldt E, Koepke T, Bedard MP, Nadyal R. Acute neonatal morbidity and long-term central nervous system sequelae of perinatal asphyxia in term infants. Early Hum Dev 1991; 25: 136-148 5 Busto R, Dietrich WD, Globus MYT, Valdes I, Scheinberg P, Ginsberg MD Small differences in intra-ischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cerebr Blood Flow Metab 1987; 7: 729 - 38 6 Dietrich WD. The Importance of Brain Temperature in Cerebral Injury. J Neurotrauma 1992; 9: Suppl 2: S-475- 485 7 Thoreson M, Wyatt J. Keeping a cool head, post-hypoxic hypothermia - an old idea revisited. Acta Paediatr 1997; 86: 1029-33 8 Gelman B, Schleien CL, Lohe A, Kuluz JW. Selective brain cooling in infant piglets after cardiac arrest and resuscitation. Crit Care Med 1996; 24: 1009-1017 9 Mellegard P. Changes in human intracerebral temperature in response to different methods of brain cooling. Neurosurgery 1992; 31: 671-677 720 725 730 735 740 745 18 10 Simbruner G.Thermodynamic models for diagnosic purposes in the new-born and fetus; Facultas Verlag, Wien; 1983, ISBN 3-85076-133-9 11 Weinrauch V, Safar P,Tisherman S, Kuboyama K, Radovsky A. Beneficial effects of mild hypothermia and detrimental effect of deep hypothermia after cardiac arrest in dogs. Stroke 1992; 23: 1454-1462 12 Chopp M, Knight R, Tidwell CD, Helpern JA, Brown E Welch KMA. The metabolic effects of mild hypothermia on global cerebral ischemia and recirculation in the cat: comparison to normothermia and hyperthermia. J Cereb Blood Flow Metabol 1989; 9: 141148 13 Busto R, Globus MYT, Dietrich D, Martinez E, Valdes I,Ginsberg MD. Effect of mild hypothermia on ischemia-induced release of neurotransmitters and free fatty acids in rat brain. Stroke 1989; 20: 904-910 14 Coimbra C, Wieloch T. Moderate hypothermia mitigates neuronal damage in the rat brain when initiated several hours following transient cerebral ischemia. Acta Neuropathol 1994; 87: 325-331 15 Clifton GL, Jiang JY, Lyeth BG, Jenkins LW, Hamm RJ, Hayes RL. Marked protection by moderate hypothermia after experimental traumatic brain injury. J Cereb Blood Flow Metab 1991; 1:114-121 16 Armstead WM, Mirro R, Busija DW, Leffler CW. Post-ischemic generation of superoxide anion by newborn pig brain. Am J Physiol 1988; 255: H401-403 17 Edwards AD, Yue X, Cox P, Hope PL, Azzopardi D, Squier MV, Mehmet H. Apoptosis in the brains of infants suffering intrauterine cerebral injury. Pediatr Res 1997; 42(5) 684-689 18 Colbourne F, Corbett D. Delayed and prolonged post-ischemic hypothermia in neuroprotective in the gerbil. Brain Research 1994; 654: 265-272 19 Gunn AJ, Gunn TR, Gunning MI, Williams CE, Gluckman PD. Neuroprotection with prolonged head cooling started before post-ischemic seizures in fetal sheep.Pediatrics 1998; 102 (5): 1098-1106 750 755 760 765 770 775 780 19 785 20 Sirimane ES, Blumberg RM, Bossano E, Gunning M, Edwards AD, Gluckman PD,Williams CE. The effect of prolonged modification of cerebral temperature on outcome after hypoxic-ischemic brain injury in the infant rat. Pediatr Res 1996; 9: 591-597 790 21 Marion-DW; Penrod-LE; Kelsey-SF; Obrist-WD; Kochanek-PM; Palmer-AM; Wisniewski-SR; DeKosky-ST. Treatment of traumatic brain injury with moderate hypothermia. N Engl J Med 1997; 336: 540-546 22 Gunn AJ, Gluckman PD, Gunn TR. Selective head cooling in newborn infants following perinatal asphyxia; a safety study. Pediatrics 1998; 102 : 885 - 892 23 Simbruner G, Haberl C, Harrison V, Linley L. Induced brain hypothermia in asphyxiated human newborn infants: a retrospective chart analysis of physiological and adverse effects . Int Care Med 1999; 25:1111-1117 24 Chopp M, Chen H, Dereski MO, Garcia JH. Mild hypothermic intervention after graded ischemic stress in rats. Stroke 1991; 22: 37-43 25 Berger R, Jensen A, Hossmann KA, Paschen W. Effect of mild hypothermia during and after transient in vitro ischemia on metabolic disturbances in hippocampal slices at different stages of development. Dev Brain Res 1998; 105: 67-77 26 Yager JY, Shuaib A, Thornhill J.The effect of age on susceptibility to brain damage in a model of global hemispheric hypoxia-ischmia. Dev Brain Res 1996; 93: 143-154 27 Cornell HM. Accidental hypothermia. J Pediatr 1992; 120: 671-79. 28 28 Ilievich UM, Spiss CK. Hypothermic therapy for the injured brain. Current Opinions in Anesthesiology 1994; 7:394-400 29 Okada M. The cardiac rhythm in accidental hypothermia. J Electrocardiol 1984; 17: 123-128 30 Mann TP, Elliot RIK. Neonatal cold injury due to accidental exposure to cold. Lancet 1957; 1, 229 31 Chadd Ma, Gray OP. Hypothermia and coagulation defects in the newborn. Arch Dis Child 1972: 41: 819-821 32 Kaplan M, Eidelman AI. Improved prognosis in severely hypothermic newborn infants treated by rapid rewarming. J Pediatr 1984; 105: 470-74 33 Staab BD, Sorensen VJ, Fath JJ, Raman SBK, Horst HM, Obeid FN. Coagulation defects resulting from ambient temperature-induced hypothermia. J Trauma 1994; 36: 634-8 795 800 805 810 815 820 825 830 20 34 El-Radhi AS, Jawad MH, Ibrahim M, Jamil II. Infection in neonatal hypothermia. Arch Dis Child 1983; 58 (2): 143-145 35 Shiozaki T, Sugimoto H, Tenada M, Yoshida H, Iwai A, Yoshioka T, Sugimoto T. Effect of mild hypothermia on uncontrollable intracranial hypertension after severe head injury. J Neurosurger 1993; 79: 363-368 36 Bernard SA, Jones BM,Horne MK. Clincal trial of induced hypothermia in comatose survivers of out-of-hospital cardiac arrest. Ann Emerg Med 1997; 30: 146-53 37 Metz C, Holzschuh M, Bein T, Woertgen C, Frey A, Frey I, Taeger K, Brawanski A. Moderate hypothermia in patients with severe head injury: cerebral and extracerebral effects. J Neurosurgery 1996; 85: 533-541 38 Westin B, Nyberg R, Miller JA, Wedenberg E. Hypothermia and transfusion with oxygenated blood in the treatment of asphyxia neonatorum. Acta paediatr Scand 1962; 51; Suppl 139: 1-80 39 Miller JA, Miller FS, Westin B. Hypothermia in the treatment of asphyxia neonatorum. Biol Neonate 1964; 6: 148-163 40 Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurology 1997; 39: 214-223 41 Thompson CM, Puterman AS, Linley LL, Hann FM, van der Elst CW, Molteno CD, Malan AF. The value of a scoring system for hypoxic ischaemic encephalopathy in predicting neurodevelopmental outcome. Acta Paediatr 1997; 86: 75761 42 al Naqeeb N, Edwards AD, Cowan FM, Azzopardi D. Assessment of Neonatal Encephalopathy by Amplitude-intergrated Electroencephalography. Pediatrics 1999; 103; 1263-1271 835 840 845 850 855 860 865 43 870 Hellström-Westas L, Rosén I, Svenningsen NW (1995) Predictive value of early continuous amplitude integrated EEG recordings on outcome after severe birth asphyxia in full term infants. Arch Dis Child 72: F34-F38 44 875 Toet MC, Eken P, Groenendaal F, de Vries LS Comparison of amplitude integrated EEG in birth asphyxiated term neonates between 3 and 6 hours after birth (Abstr 1902, Neurology; Ped Res 1998; 43, Part 2 of 2) 21 45 Lamblin MD, Andre M, Challamel MJ, Curzi-Dascalova L, dÁllest AM, De Giovanni E , Moussalli-Salefranque F, Navelet Y, Plouin P, Radvanyi-Bouvet MF, Samson-Dollfus D, Vecchierini-Blineau MF. Electroencephalographie du nouveau-ne premature at a term. Aspects maturativs et glossaire. Neurophysiol Clin 1999; 29: 123 - 219 46 Thoresen M and Wyatt J. Review article . Acta Paediatr 1997; 86: 1029-33 Keeping a cool head, post-hypoxic hypothrmia-an old idea revistied (References 29- 34) 47 Thoresen M, Cooling the newborn aftrer asphyxia - physiological and experimental background and its clinical use. Semin Neonatol 2000; 5:61-73 48 Thoresen M, Satas S, Loberg EM, Lindgren C, Acolet D, Steen PA, Haug E, Whitelaw A. Pediatr Res 1999; 45: 46 A 880 885 890 895 22 APPENDIX 1 900 Procedures and definitions for neurological assessment, aEEG and EEG assessment Assessment of Neurological Signs 905 Neurological signs are observed and scored according to Thompson et al (41).The score consists of a clinical assessment of nine signs. Each sign is scored from 0 to 3 and the score for each day is totalled. The higher the score the more severely affected the infant. The maximum possible score on any day is 22. The score is equally applicable to ventilated infants . It cannot be applied to paralyzed infants. 910 Score Sign 915 920 Tone LOC Fits Posture Moro Grasp Suck Respir Fontanell 0 normal normal none normal normal normal normal normal normal 1 hyper hyperalert, stare < 3 per day fisting, cylcing partial poor poor hyperventilation full, not tense 2 3 hypo flaccid lethargic comatouse > 2 per day strong distal flexion decerebrate absent absent absent ± bites brief apnea IPPV (apnea) tense 925 Recording of aEEG and Standard EEG 930 The aEEG will be recorded with a Lectromed Cerebral Function Monitor and the use of needle electrodes inserted at an exact distance of 5 cm apart from each other at the temples. Different distances result in different voltage (Personal communication: Hellström-Westas L, Blennow M). The recording speed is 1mm/min. At least one half hour recording is required, latest between 5.0 and 5.5 hours of age. A 30 min decrease of lower voltage margine below 5uV must not be associated with sleep cylces, manipulations or drug administration. 935 The Standard EEG is recorded according to the International 10-20 classification. Classification of aEEG for Inclusion Criteria 940 The classification of the aEEG is based on the publication of Niran al Naqeeb et al. (ref 42 : Pediatrics 1999; 103; 1263-1271). It yields three subgroups: normal aEEG, moderately abnormal aEEG and suppressed aEEG. Moderately abnormal aEEG designates mildly to moderately asphyxiated new-born and suppressed aEEE severely asphyxiated new-borns. This classification is used for subgroup analysis. Patients with the 23 945 unlikely aEEG combination of upper margin < 10 uV and lower margin >5uV will remain unclassified and excluded from the study. Classification of standard EEG for Inclusion criteria 950 The classification of the standard EEG is based on the publication of Lamblin MD et al. (ref 45: Neurophysiol Clin 1999; 29: 123 - 219) 955 Definition of normal EEG: Continuous , no intervals > 3 sec and no amplitudes < 10 uV Definition of abnormal EEG: Continous low voltage < 25 uV or discontinuous (burst supression) see exact definition 4.1 , 4.2 and 4.4 , 4.5 in article of Lamblin et al. 960 Sampling rate: Every 5 min a time sample of 20 sec long tracing 965 24 APPENDIX 2 970 Scientific basis for inclusion criteria, classification into subgroups and sample size calculations. 975 980 This study includes all asphyxiated new-borns whose aEEG or standard EEG is not normal at any time within the first six hours of age. Infants with a normal aEEG or Standard EEG, not included into the study, may later turn out to have an neurodevelopmental impairment. The false negative rate (normal EEG, but abnormal outcome) might range from 4% to 15% (42 - 44). The study population will contain mild to moderate encephalopathy and severe encephalopathy. These two subgroups will be classified before the intervention and within the first 6 hours of age according to their aEEG or standard EEG (see APPENDIX 1) . Event rate 985 990 The event rate is defined as death or neurodevelopmental impairment of survivors. Depending on the severity, asphyxia causes a certain rate of neurodevelopmental impairments. The table shows the event rates of ”death and neurodevelopmental impairment ”in dependence of the initial severity classified according to aEEG into the two subgroups. Estimated from data from Hellström-Westas et al, Toet et al and AlNaqeeb et al. (42 - 44). Correlation of ampliutde-integrated EEG to neurological outcome 995 Severity Author Normal al Naqueeb 9 Hellström 26 Toet 26 1005 Moderate abnormal aEEG al Naqeeb Hellström Toet 1010 Suppressed aEEG al Naqeeb Hellström Toet 1000 Nr Event rate (%) Disabilty and Death Event rate (%) No Disability 0 1 4 (0%) (4%) (15%) 9 25 22 (100%) (96%) (85%) 17 14 13 13 11 10 (75%) (77%) (77%) 4 3 3 (25%) (23%) (23%) 12 5 5 12 5 5 (100%) (100%) (100%) 0 0 0 (0 %) (0%) (0%) 25 Summarized Results of aEEG Studies 1015 No disability Normal aEEG Abnormal aEEG Disability and death 5 56 61 56 10 66 1020 Nr. 61 66 239 Sensitivity 56/61 = 92 % ; Specificity 56/66 = 85% 1025 Correlation of standard EEG to neurological outcome (analyzed according to criteria of Lamblin MD et al., to be published d ´Allest AM et al.) No disability 1030 Normal EEG Mod abn EEG 128 Disability and Death Nr. (96%) 5 (4%) 133 (55.6 %) 17 (54%) 14 (46%) 31 (13.0 %) 2 (3%) 73 (97%) 75 (31.4 %) 1035 Severe abn EEG 147 30 239 1040 Summarized Results of Standard EEG No disability Disability and death Nr. 128 19 5 87 133 106 147 92 239 1045 Normal EEG Abnormal EEG 1050 1055 Sensitivity 87/92 = 95 % ; Specificity 128/147 = 87 % These data on aEEG and standard EEG on neurodevelopmental outcome demonstrate: (i) that aEEG and standard EEG have a similarly high predicitve power (92% vs 95% sensitivity and 85% vs 87% specificity). Consequently both methods are valid for the inclusion of asphyxiated infants. (ii) that the ratio of moderate to severe aEEG findings is 66 % and 33% respectively in the compiled aEEG studies (ref 42-44) and the ratio of moderate to severe in the standard EEG Data (see above) is 30% vs 70%. 26 1060 Consequently an overall ratio of 60% moderate and 40% severe asphyxia was assumed for sample size calculation and iii) because of the lack of congruence of subgroups defined by aEEG and standard EEG, subgroup analysis will be done only on patients with aEEG inclusion criteria. 1065 Treatment effect 1070 1075 1080 1085 In six new-born animal studies the neuroprotection (expressed as reduction in % cell damage or abnormal neurobehavior) of mild to moderate hypothermia starting within 30 min after the ischemic-hypoxic insult varied between 25 to 80% (the neuroprotective effect was > 50%, when those studies where hypothermia was induced only for <3 hrs, were excluded (46)). No data for the treatment effect of asphyxiated human new-borns are available. The study population will contain infants with mild to moderate encephalopathy. In animal experiments hypothermia has been shown to be more effective in mild to moderate asphyxia than in severe to fatal asphyxia (Chopp M et al. Mild hypothermic intervention after graded ischemic stress in rats. Stroke 1991; 22: 37-43). Gluckman et al in the Olympic Medical Protocol assumed a 30 % reduction of neurodevelopmental impairment and death (an event rate of 70% in the control and 49% in the intervention group) in a group of mixed (moderately and severely) asphyxiated newborns. We thus assumed a 40% reduction (less than the 50% in animal experiments, but more than the 30% for the mixed group) for the mildly to moderately and 10% (less than the mixed group) for the severely asphyxiated group. 27 APPENDIX 3 Specifications for cooling mattress and aEEG device 1090 Cerebral Function Monitor (CFM) The CFM to be used for the study is the one from Lectromed or proven equivalent. 1095 1100 1105 Specification: LECTROMED Cerebral Function Monitor Lectromed MT2-5330 CFM System Representative in Germany: FBI Fred Berninger Importe OHG Bergstraße 12, D-82024 Taufkirchen, Germany Tel.: + 49 89 61 453 453 or +49 161 2832755 Fax.: + 49 89 61 453 453 e-mail > BERNIMPORT@AOL.com Cooling Device 1110 The cooling device to be used for the study is the one of TEC.COM GMBH. It consists of an apparatus which provides a perfusion flow of a temperature regulated fluid and a mattress. A simpler version Tecovit 200 for NICU use and transport, with battery 12 V powering, is available. 1115 Specification: Cooling device Tecotherm TS med 200 (about 3200 Euro) , size 420 x 190 x 350 mm, ca 10 kg; Temperatue range : 5 - 42°C ; hand controlled OR 1120 1125 1130 Tecovit 200 (about 1750 Euro) plus CSZ Cooling matrass, rectangular, cleanable surface, ca.80 x 60 cm (about 90 Euro) TEC.COM GMBH Prof Dr K Berndt Product Manager Böllberger Weg 170 D - 06128 Halle/Saale, Germany Tel.: + 49 (0) 345 – 120 52 04 Fax.: + 49 (0) 345 – 120 52 11 e-mail >berndt-halle@t-online.de< OR >SCHOEPKE:teccom@t-online.de 28 APPENDIX 4 Monitoring Schedule 1135 1140 1145 1150 Time Data Sets adm before 3 12 24 48 72 CerFunction aEEG x----- continous------x x x x cont x Rect Temp ( Thermom ) Cooling Fluid Temp x Environm Temp x x -----------------hourly----------------------x -----------------hourly----------------------- x x x x x x x x x Blood Pressure Heart rate Breathing rate SpO2 PtcCO2 Respir Variables Urine output (3hrs) Blood Samples blood gases glucose x x x x x x x x x x x x x x x x x Clinical Examination Neurol Examination x x x x x -----------------hourly----------------------x -----------------hourly----------------------x -----------------hourly----------------------x -----------------hourly----------------------x -----------------hourly----------------------x x x x x x x x x x x x x 80 hrs x x x x x x x x x x x x x x x x x x x x x x x 1155 Ultasound Imaging x Organ Failure Blood samples electrolytes hemoglobin coagulation infection screen kidney function x x x x x x x x x x x x x x x x x x x x x x x x amylse endocrine lactate x x x 1160 1165 1170 1175 Liquor lumbal Blood S-100, NSE Time x x x x - between - x x - between - x adm before 3 12 24 48 72 80 hrs 29 Appendix 5 1180 Case Report Forms