Muscles convert chemical energy into kinetic energy
advertisement

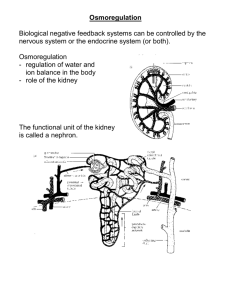
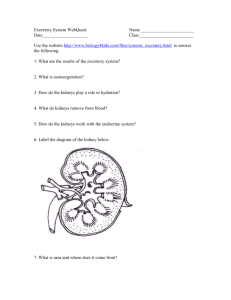
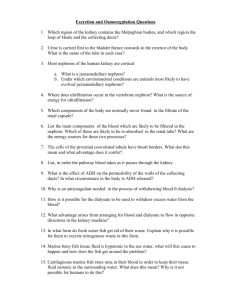
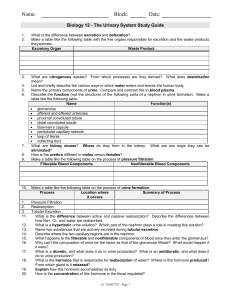
Chapter 12 Excretory System 12.1 The Kidney A. Introduction: The kidneys play a major role in homeostasis. They have three main functions: 1. Remove Wastes o excess protein in the diet is converted into carbohydrates in the liver by a process called deamination o During this process NH3 (ammonia – highly toxic…0.005 mg can kill you) is removed from amino acids o (in the liver) 2 molecules of NH3 combine with CO2 forming urea…….(urea is 1000X less toxic than ammonia) o Uric acid is also formed...but it is from the breakdown of DNA (nucleic acids)… build up of uric acid is called gout 2. Balance Blood pH Kidneys remove H+ ions (acid) and other ions from the blood keeping the pH in normal range (7.4) 3. Maintain Water Balance o we can only survive a few days without water ~ 2L of water is lost per day from perspiration, exhaling, urine 1% loss of H2O = thirst, 5% loss of H2O = pain, collapse, 10% loss of H2O = death…eg. heat exhaustion o hormones such as ADH (antidiuretic hormone) and aldosterone regulate water concentration in the blood o ~ 180 L moves through kidneys in one day…we lose only o 2 L therefore 178 L are reabsorbed! B. Anatomy of the Excretory System Activity: The Urinary System Handout (fill in structures) 1. Renal Blood Vessels 1 o the renal arteries branch from the abdominal aorta and supply the kidneys with oxygenated, unfiltered blood o the renal arteries remove deoxygenated, filtered blood 2. Kidneys o we have two kidneys which filter our blood….together they hold as much as ¼ of our blood at any one time o each kidney has a mass of about 500 g o each kidney has about 1 million nephrons o It is Made up of 3 layers: a.) the cortex: outer layer of connective tissue b.) the medulla: inner layer (beneath the cortex) containing the nephrons c.) the pelvis: hollow chamber joining kidney to ureter 3. Ureters o wastes filtered through the nephrons move from the kidneys into 2 tubes called the ureters 4. Bladder o both ureters lead to the bladder o storage for urine o holds about 200 mL of urine at 400mL stretch receptors signal the brain that it is “time to go….” after 600 mL is collected all voluntary control is lost! 5. Urethra o urine leaves the bladder through the urethra o sphincter muscles relax and urine is voided o the urethra is longer in men than in women therefore women are more susceptible to bladder infections because bacteria on the outside of the body have a shorter distance to travel Your Assignment: Activity; The Nephron Handout: fill in structures Note: the cortex contains the afferent, efferent arterioles and the Bowman’s capsule C. The Nephron nephrons: are the functional units of the kidney (each kidney has about 1 million) Afferent arterioles supply the nephrons with blood and branch into the capillary bed called the glomerulus (high pressure filter) 2 Blood leaves the glomerulus by the efferent arterioles and travels to the peritubular capillaries (they wrap around the kidney tubule) …..to the venule …then to the renal vein The glomerulus is surrounded by the Bowman’capsule (funnel-like part) which tapers to the proximal tubules The proximal tubules connects to the loop of Henle ( in the medulla) The loop of Henle connects to the distal tubule which empties into the collecting ducts …these ducts merge in the renal pelvis Your Assignment: Page 380, 1-3 D. Formation of Urine It depends on: 1. Filtration: the movement of fluid from the blood into the Bowman’s capsule 2. Reabsorption: involves the transfer of essential solutes and water from the nephron back to the blood 3. Secretion: involves the transport of materials from the blood into the nephron 1. Filtration o filtration rate: if the pressure then filtration o blood enters nephron through the afferent arteriole (pressure is 2 kPa) this arteriole branches into a capillary bed called the glomerulus (pressure is 8 kPa) which acts like a high pressure filter o large solutes such as plasma proteins, blood cells and platelets are too large to filter through and move through the glomerulus into the efferent arteriole dissolved solutes (eg. Na+, Ca2+, glucose, urea, uric acid etc) pass through the glomerulus into the Bowman’s capsule the glomerular now can move on to go through reabsorption 2. Reabsorption o occurs from nephron into bloodstream o it occurs till the threshold level is reached…the maximum amount of a substance that can be moved across the nephron o 600 mL of fluid moves through kidney per minute… o about 120 mL of that is filtered into the nephron…and from that only 1 mL of urine is made o both active and passive transport occur o glomerular filtrate (dissolved solutes) travel down the proximal tubule 3 o most reabsorption (85%) occurs in the proximal tubule o contains a rich supply of mitochondria (for energy) and microvilli to greatly increase surface area o as the filtrate moves through the proximal tubule, Loop of Henle and distal tubule, water and certain ions must be reabsorbed back into the bloodstream to maintain proper water and ion balance o Na+ions , glucose and amino acids are actively transported out of the nephron by carrier molecules and into the peritubular capillaries (bloodstream) o in the descending loop, the filtrate is hypertonic therefore water diffuses out of nephron into bloodstream (passive transport) o once the filtrate reaches the ascending loop, the filtrate is hypotonic… more Na+ is actively transported out to keep water from moving the wrong way o Cl and HCO3 ions follow the Na+ ions due to charge attraction (passive transport) o there is a limit to the energy available for active transport so some NaCl and other solutes in excess stay in the urine o once the ions move out an osmotic gradient is set up so water diffuses from tubules and Loop of Henle into bloodstream o filtrate becomes more concentrated as it moves along towards the distal tubule 3. Secretion o movement of wastes from the bloodstream into nephron o left over wastes such as urea, histamine, NH3, K+ ions, H+ ions, HCO3- ions, minerals, drugs such as penicillin etc. move from the blood into the distal tubule of the nephron o usually active transport o urine moves into the collecting ducts which lead to the renal pelvis then on to the ureters and bladder o composition of urine: water (95%) urea uric acid trace amino acids electrolytes: Na+, K+, Cl-, SO42-, PO43 excess vitamins, minerals, etc o pH of urine ranges from 4 to 5 but can get as high as 8.5 4 Remains in Blood Filters into Capsule Reabsorbed RBC Water Water (most of) WBC Amino acids Amino acids (all) Platelets Glucose Glucose (all) Fats Salts Salts (some) Blood Protein Urea, uric acid Urea, uric acid (none) Component Plasma Filtrate Urine Urea 0.03 0.03 2.0 Uric Acid 0.004 0.004 0.05 Glucose 0.10 0.10 0 to trace Amino Acid 0.05 0.05 ----- Salt 0.72 0.72 ~1.5 Protein 8.00 ----- ---- 5 Summary All the glucose and amino acids get reabsorbed Some salts get reabsorbed No urea or uric acid get reabsorbed Proteins Never get filtered Summary: Filtration: o glomerulus and Bowman’s capsule Passive transport Reabsorption o proximal tubule (mainly), loop of Henle active and passive transport Secretion o distal tubule o mainly active transport pH Balance the kidneys help maintain blood pH balance between 7.3 and 7.5 carbon dioxide from the peritubular capillaries is transported to the cells that line the nephron.. where it combines with water H+ and HCO3- ions are produced…. the HCO3- ions diffuse back to the blood (buffering the blood) Your Assignment: Page 386, 1-9 12.2. Kidney Dysfunction Diabetes Mellitus (there are three types: Type 1, Type 2, Gestational ) Caused by inadequate insulin Amount of glucose in blood increases therefore the amount of glucose in the filtrate increases There is a limit to the energy that is available for active transport of glucose back into the bloodstream 6 Excess glucose stays into the nephron and decreases the concentration gradient therefore there is less H20 reabsorbed Urine volume increases and there is glucose in urine Diabetes Insipidus Caused by the destruction of hypothalamus cells or of the nerves that lead to the pituitary gland No ADH is released There is a huge increase in the amount of urine that is produced because of no re-absorption from ADH Bright’s Disease (nephritis) Many causes Blood vessels in the glomerulus become inflamed or are destroyed Glomerulus becomes permeable to plasma proteins and possibly blood cells Body cannot reabsorb these large solutes (no mechanism) Concentration gradient decreases therefore there is less water reabsorbed Urine in put increases (because of excess water) Kidney stones They are caused by the precipitation of mineral solutes from the blood There are two types: acidic and alkaline They can lodge in the renal pelvis or urethra Tissues can be torn…. Very painful! Lithotripsy uses shock waves break the stones up into smaller pieces so that they can be passed If the stones are too big = surgery Dialysis Technology Dialysis the proper functioning of our kidneys is necessary for life people who have malfunctioning kidneys undergo dialysis the person's blood is transferred from their body through a dialysis machine that behaves like a mechanical kidney (peritoneal dialysis and hemodialysis) 7 the dialysis tubing is semipermeable…. large solutes won’t pass through but small solutes (glucose, urea, H+, uric acid, K+, other electrolytes etc) can the solution surrounding the tubing has a lower concentration of the small dissolved solutes the dissolved solutes diffuse from the tubing into the dialysis machine then the “filtered” blood is returned to the body the best option is a kidney transplant There are two types of Dialysis Hemodialysis: A dialysis mimics the action of the nephron. A person has a surgical procedure to create access, a shunt is put in for the needles and tubing which connects the circulatory system to the machine Blood is pumped through a series of tubes that are bathed in solutes. Glucose and a mixture of salts set up a concentration gradient. Because the dialysis fluids have no urea, the solute always moves from the blood into the dialysis fluid By continually flushing this fluid and replacing it urea is removed along with other wastes Peritoneal dialysis Is done through the lining of the abdominal cavity (peritoneal membrane) A catheter (thin tube) is inserted. 2L of Dialysate (a solution) is pumped into the abdominal cavity through the catheter and remains in the abdomen cavity for 4 to 6 hours (The membranes in the cavity filter wastes) The fluid is then drained using the catheter. The process begins again The only function that a dialysis machine can not do is ACTIVE TRANSPORT! 8 Kidney Transplant Involves placing a new kidney and the ureter in the lower abdomen near the groin It takes 2-4 hours Old kidneys are not usually removed Sometimes dialysis will be needed until the new kidney can fully function Water Balance and ADH More water intake = increased urine Less water intake = decreased urine Nervous system and endocrine system balance fluid levels 1. Regulation of ADH The function of ADH (antidiuretic hormone) is to increase H2O reabsorption into the bloodstream nerve cells in the hypothalamus (in the brain) produce ADH 9 it is secreted to the pituitary gland at the base of the brain where it is stored until needed osmoreceptors in the hypothalamus detect changes in osmotic (H2O) pressure in the bloodstream as H2O loss occurs H2O moves from the tissues into the bloodstream which increases the blood’s osmotic pressure the cells of the cells of the hypothalamus shrink causing a nerve message to be sent to the pituitary gland stimulating the release of ADH and triggering the thirst response the kidneys then reabsorb more H2O and produce a more concentrated urine (dark yellow) 2. Effect of ADH on Nephron proximal tubule and descending loop of Henle are permeable to H2O ascending loop of Henle, distal tubule and collecting duct are impermeable to H2O If there is no ADH the 15% H2O that didn’t get reabsorbed in the proximal tubule is lost in the urine ADH causes the distal tubule and collecting duct to become permeable to H2O therefore decreasing the amount of H2O lost in urine Cold weather, caffeine and alcohol all inhibit the release of ADH so that reabsorption of the H2O can’t take place and urine volume is increased Blood Pressure and Aldosterone The kidneys help regulate blood pressure When blood pressure is low: A structure near the glomerulus secretes rennin 1. The adrenal glands release aldosterone 2. The function of aldosterone hormone is to increase blood pressure by increasing the reabsorption of H2O blood volume can regulate blood pressure… as volume decreases blood pressure decreases aldosterone is produced in the adrenal gland which is located above the kidney 10 blood pressure in the kidneys is monitored by the osmoreceptors in the juxtaglomerular apparatus (cells located in the afferent arteriole near the glomerulus) when BP drops the cells in the juxtaglomerular apparatus release rennin which converts angiotensinogen (a plasma protein secreted by the liver) to angiotensin (active form) angiotensin constricts blood vessels and causes aldosterone to be released (both of which increase BP) aldosterone is released and causes an increase in Na+ reabsorption from the ascending loop, distal tubule and collecting duct (nephron) as more NaCl leaves the nephron (ascending loop), the osmotic gradient increases with a higher concentration of H2O in the nephron H2O moves into the bloodstream by osmosis therefore increasing blood volume and BP Your Assignment: Page 396, 1-19 11 12