Cardio67-ElectricalActivityOfTheHeartII

Cardio #67
Wed, 01/22/03, 9am
Dr. Downey
Tom Hubmer
Page 1 of 5
Electrical Activity of the Heart II
I. Modulators of Ca++ Conductance Continued
A.
Positive Effects – decrease calcium influx and conductance
B.
Acetylcholine
1.
Released by Parasympathetic System
2.
binds to muscarinic receptors
3.
inhibit adenylyl cyclase
4.
decrease cAMP
5.
decrease activation of L-type Ca++ channels
C. Calcium channel antagonists
1.
used for treatment of Hypertension – (called Ca++ channel blockers)
2.
decrease tone of vascular smooth muscles and thereby reduce the force of the blood pressure
3.
use with caution because can also dangerously decrease cardiac performance
4.
sometimes used to intentionally decrease cardiac performance if myocardium is deprived of Oxygen or ATP
II. Ligand Gated Potassium Channels
A.
ATP Sensitive K+ Channels
1.
If low levels of ATP, K+ channels open and allow efflux a. will also open in the presence of adenosine, an ATP breakdown product
2.
Leads to Hyperpolarization – shortens plateau of action potential
3.
Thought to be protective by having the cell conserve its energy a.
if cells are in ischemia many will hyperpolarize like this
B.
Acetylcholine-activate K+ Channel
1.
opened by Vagal Stimulation
2.
decrease the resting (diastolic) potential
3.
decrease rate of rise of pacemaker potential
4.
decrease duration of Action potential
III. Slow Response Action Potentials
A. Ionic Basis for Slow Response
1.
if phase 4 is not sufficiently negative, h gates on fast Na+ channels remain set.
The fast channels cannot be activated, so rapid Na+ influx cannot occur, Ca++ channels are functional, and at their threshold begin to open. This leads to a slowly developing inward Ca++ current and produces a slow raising phase 0 a.
this can occur in abnormal fast response cells if ischemia prevents them from sufficiently repolarizing and opening h gates normally.
This leads to a slower response
2.
SA and AV nodal cells may lack fast Na+ channels. Thus the nodal cells have slow responses during their phase 0 due to their reliance on Ca++ influx
Cardio #67
Wed, 01/22/03, 9am
Dr. Downey
Tom Hubmer
Page 2 of 5
B. Pacemaker Currents
1.
Pacemaker cells have the ability to spontaneously depolarize but they all do so at a different rate. When one reaches action potential it will depolarize adjacent cells which will conduct outward to the rest of the heart
2.
There are four proposed different pacemaker currents a.
I k
(The repolarizing potassium current) activated by full depolarization. Then, as the voltage decreases, it becomes inactivated and decays (thus sometimes called the waning K+ current). As it decays it takes the breaks off the Ca++ and Na+ channels allowing for depolarization when appropriate again b.
I b
(nonspecific background current of Na+ influx– not shown) then begins to flow and depolarize c.
I f
(inward current evoked by hyperpolarization) – called the funny current as it causes Na+ influx with hyperpolarization . Thought to be a safety device designed to prevent too much hyperpolarization. d.
I
Ca-T ( transient inward calcium current) is activated with sufficient depolarization which will eventually trigger the action potential itself.
3. Pacemaker Firing Rate a.
The figure below shows how Firing rates are altered b.
The top graph illustrates how a reduction in the slope of the I
Ca-T
will cause a delay in the generation of the action potential c.
The bottom graph illustrates how increasing the threshold potential can diminish the firing frequency. similar results with hyperpolarization of resting potential.
Cardio #67
Wed, 01/22/03, 9am
Dr. Downey
Tom Hubmer
Page 3 of 5 d.
likewise, giving catecholamines (ex: Epinephrine) will increase the likelihood of depolarization and thus increase the heart rate by decreasing the length of phase 4. e.
The next figure illustrates how by providing Vagal (Acetylcholine) stimulation K+ channels will be opened causing hyperpolarization and preventing the SA from generating an action potential
4. Overdrive Suppression a.
Automaticity of pacemaker cells diminishes after a period of excitation at a high frequency . so high heart rates will decrease automaticity afterwards b.
Firing of SA node suppresses automaticity of other loci. c.
As rate increases, influx of Na
+
, activity of Na
+
, K
+
-ATPase increases, and by its electogenic property hyperpolarizes the membrane. d.
Example given: After a period of High Heart Rates patient will experience syncope due to a overdrive suppression causing a prolonged diastole while normal rate of depolarization is reestablished
5. Catecholamine Effects e.
giving catecholamines (ex: Epinephrine) will increase the likelihood of depolarization and thus increase the heartrate by decreasing the length of phase 4 in the SA node.
IV. Cardiac Conduction
A Conduction of the Action Potential – see next page for board diagram
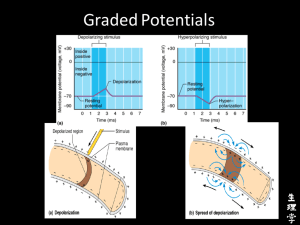
1. Along the Cell Membrane - Local-circuit currents precede the action
potential wave front and bring adjacent membrane to threshold. These
Cardio #67
Wed, 01/22/03, 9am
Dr. Downey
Tom Hubmer
Page 4 of 5
local-circuit currents are due to movement of ions parallel to the
membrane. At threshold, transmural currents depolarize the membrane. a. if an action potential has greater amplitude the local current will extend further forward and be more effective in reaching phase 0.
2. Cell to Cell - Within the intercalated disks, the membranes of two cells
are in close apposition, and form a nexus containing gap junctions.
Gap junction channels provide a low resistance path for local-circuit
currents
- - - - - - - - +++++++++++
+ + + + + + - - - - - - -
+
+
-
-
+ -
+ -
ACTION POTENTIAL
IV. Cardiac Conduction
Local Circuit currents
Cell to Cell currents at gap jxns
A. Velocity of Cardiac Conduction
1.
Atrial and Ventricular Contractile Cells: 0.3 to 0.5 meters per second
2.
AV Node: 0.02 meters per second – a necessary delay to allow the ventricles to fill with blood because the atrial ejection is insufficient alone. Atria and ventricles are completely insulated from each other except at AV node.
3.
Purkinje System: 4 meters per second (Huge fast fibers) – have many gap junctions along adjacent walls to allow rapid conduction
B. Factors that Influence Velocity of Conduction
Slow Response less negative at rest slow rise of phase 0 low degree of depol
Fast Responses more negative at rest hi slope of phase 0 hi degree of depol
Cardio #67
Wed, 01/22/03, 9am
Dr. Downey
Tom Hubmer
Page 5 of 5
1.
Fast or Slow Response Action Potentials
2.
Negativity of Resting Potential
3.
Rate of Rise of Phase 0
4.
The Degree of Depolarization
C.
Parasympathetic Effects
1.
Parasympathetic Stimulation Slows or Blocks AV Conduction – similar to the effects on the SA node graph seen on page 3 of this scribe. When hyperpolarization occurs, stimulation is sometimes blocked.
D.
Excitation of various areas of the heart in fractions of a second after SA stimulation – Know the pathway of conductance as covered in Dr. Leppi’s lectures.
1.
Dr. Downey listed 4 times that we should be familiar with
2.
Left Atrium = 0.1 seconds overall
3.
AV node = 0.07 seconds
4.
Ventricular Septum = 0.16 seconds note the delay in AV conductance
5.
All of Ventricle = 0.22 seconds note the rapid conduction of the purkinjes
V. Afterpotentials and Conductance problems– Dr. Downey said this would not be on the exam nor would the last 2 power points. Know that afterpotentials can occur and that they are pathologic and unrelated to signals from the nodes.
A.
Alterations in cycle length and K+ availability will trigger early afterdeploarizations (EAD’s) in which cells have difficulty in reaching resting potentials and have action potentials triggered too early
B.
Something in the cell membrane having to do with K+ and Ca++ channels cause spontaneous depolarizations too early or late after a normal depolarization
C.
This will cause Arrhythmias
D.
The final 3 powerpoints before the supplemental material dealing with conduction pathways and the overall EKG were only briefly reviewed and
Dr. Downey said that we would be covering this in the weeks to come know that if conduction pathways are blocked you can get pathology or electrical disturbances.

![Applied Heat Transfer [Opens in New Window]](http://s3.studylib.net/store/data/008526779_1-b12564ed87263f3384d65f395321d919-300x300.png)