March, 2005 - Clarkson University
advertisement
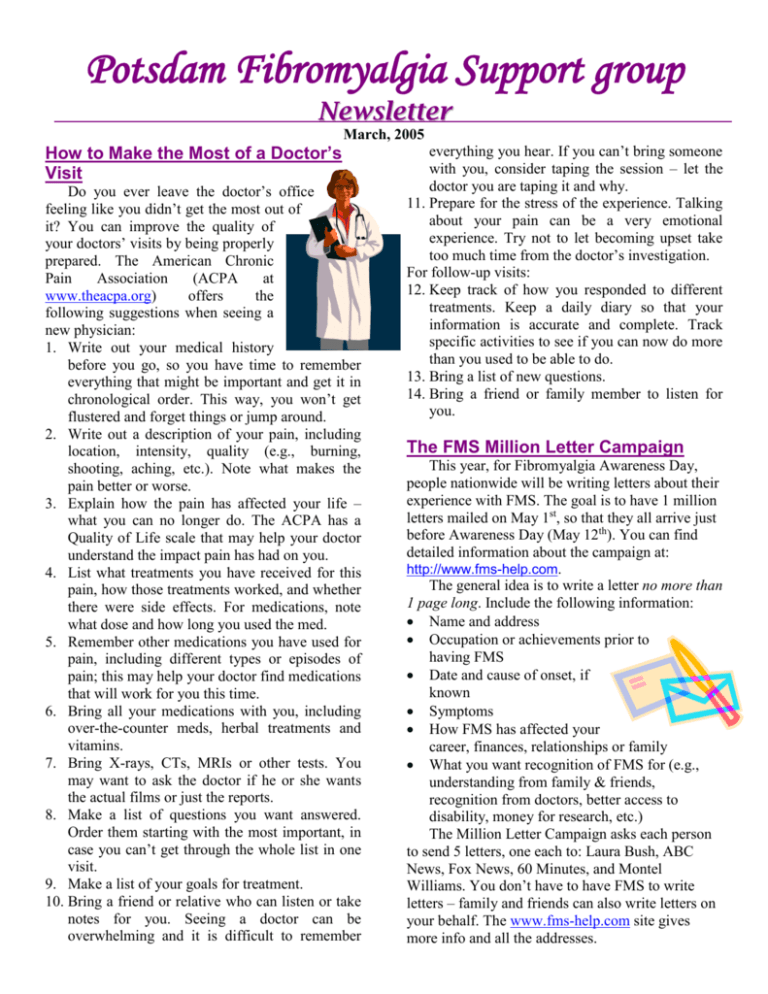
Potsdam Fibromyalgia Support group Newsletter March, 2005 How to Make the Most of a Doctor’s Visit Do you ever leave the doctor’s office feeling like you didn’t get the most out of it? You can improve the quality of your doctors’ visits by being properly prepared. The American Chronic Pain Association (ACPA at www.theacpa.org) offers the following suggestions when seeing a new physician: 1. Write out your medical history before you go, so you have time to remember everything that might be important and get it in chronological order. This way, you won’t get flustered and forget things or jump around. 2. Write out a description of your pain, including location, intensity, quality (e.g., burning, shooting, aching, etc.). Note what makes the pain better or worse. 3. Explain how the pain has affected your life – what you can no longer do. The ACPA has a Quality of Life scale that may help your doctor understand the impact pain has had on you. 4. List what treatments you have received for this pain, how those treatments worked, and whether there were side effects. For medications, note what dose and how long you used the med. 5. Remember other medications you have used for pain, including different types or episodes of pain; this may help your doctor find medications that will work for you this time. 6. Bring all your medications with you, including over-the-counter meds, herbal treatments and vitamins. 7. Bring X-rays, CTs, MRIs or other tests. You may want to ask the doctor if he or she wants the actual films or just the reports. 8. Make a list of questions you want answered. Order them starting with the most important, in case you can’t get through the whole list in one visit. 9. Make a list of your goals for treatment. 10. Bring a friend or relative who can listen or take notes for you. Seeing a doctor can be overwhelming and it is difficult to remember everything you hear. If you can’t bring someone with you, consider taping the session – let the doctor you are taping it and why. 11. Prepare for the stress of the experience. Talking about your pain can be a very emotional experience. Try not to let becoming upset take too much time from the doctor’s investigation. For follow-up visits: 12. Keep track of how you responded to different treatments. Keep a daily diary so that your information is accurate and complete. Track specific activities to see if you can now do more than you used to be able to do. 13. Bring a list of new questions. 14. Bring a friend or family member to listen for you. The FMS Million Letter Campaign This year, for Fibromyalgia Awareness Day, people nationwide will be writing letters about their experience with FMS. The goal is to have 1 million letters mailed on May 1st, so that they all arrive just before Awareness Day (May 12th). You can find detailed information about the campaign at: http://www.fms-help.com. The general idea is to write a letter no more than 1 page long. Include the following information: Name and address Occupation or achievements prior to having FMS Date and cause of onset, if known Symptoms How FMS has affected your career, finances, relationships or family What you want recognition of FMS for (e.g., understanding from family & friends, recognition from doctors, better access to disability, money for research, etc.) The Million Letter Campaign asks each person to send 5 letters, one each to: Laura Bush, ABC News, Fox News, 60 Minutes, and Montel Williams. You don’t have to have FMS to write letters – family and friends can also write letters on your behalf. The www.fms-help.com site gives more info and all the addresses. Fibrofog Fibrofog – trouble concentrating or remembering – can often be one of the most distressing aspects of FMS. It can be inconvenient, embarrassing, or can be an outright threat to your job or safety. Scientists still do not know what causes fibrofog, though trouble sleeping probably contributes. Research shows that people with FMS have trouble accessing knowledge, trouble concentrating on what they hear, slowed problem-solving, and slowed psychomotor function. These difficulties appear to be due to changes in the neuroendocrine system – hormones that regulate response to stress. The Arthritis Foundation and FMAware offer the following suggestions for dealing with ‘the fog’ (www.arthritis.org and search for ‘fibrofog’): 1. Repeat things to yourself to fix it in your mind. 2. Write it down. Be consistent about where you write things: use a calendar or keep a small notebook with you all the time. 3. Do things that require concentration at the time of day when your mind is clearest. 4. Get medical problems treated. Depression, pain and sleep disturbance all affect concentration. 5. Check your meds: some drugs for pain, sleep, hypertension and allergies affect concentration. 6. Learn relaxation techniques; stress impairs memory and concentration; relaxation helps. 7. Use mnemonics and rhymes to remember things such as where you parked the car. 8. Keep your mind active: read books, do crossword or jigsaw puzzles. The more you use your mind the ‘fitter’ it stays. 9. Get moderate exercise – it helps clear the mind, decrease stress and depression; exercise also improves blood flow to the brain. 10. Explain your memory problems to family and friends so that they can be supportive. 11. Breathe: deep breathing and relaxation breathing both improve oxygen to the brain. 12. Keep the environment quiet: keep radios and TVs off (exception: exercise to music helps). 13. Take your time. Rushing makes it more likely you will forget something. 14. Keep a sense of humor. This reduces stress, in general, and the stress of fibrofog in particular. In the FMS News The December-March issue of FMAware includes an article that discusses the possible role of dopamine in FMS. Dopamine is a neurotransmitter (chemical that relays information from one nerve to another) best known for its role in Parkinson’s disease. However, it is also involved in Restless Legs Syndrome (see the January Newsletter for more on RLS). Research shows that people with FMS who do not have night-time leg movement may still have the brain-wave pattern abnormalities seen in RLS. One of the medications used for Parkinson’s, pramipexole, is also sometimes used with RLS. Recent research shows that some people with FMS – who don’t have RLS or Parkinson’s – may also benefit from pramipexole. This medication specifically affects the dopamine receptors, and might offer another approach to managing pain and fatigue in FMS. The role of dopamine in pain is not yet clear. However, it seems to play a role in the body’s ‘fight-or-flight’ response. The ‘fight-or-flight’ response is mediated by the sympathetic nervous system, which affects sleep, heart rate, blood pressure, temperature regulation, bowel and bladder activity, immunity and metabolic rate. More research is needed to learn whether dopamine medications can become part of standard FMS care. March Potsdam Meeting: The Thursday, March 24th Potsdam meeting will be an open discussion about your personal questions or experiences related to FMS. The meeting is at 6:30 at 59 Main St, in Clarkson Hall. April Massena Meeting: The Massena Fibromyalgia Support Group’s April 12th meeting will be an open discussion. The meeting is at 6:30 at Massena Memorial Hospital. For more info, contact facilitator Maxine Dodge, at 769-5778 or maxinesbeach@wmconnect.com. This newsletter is a joint effort of Clarkson University and Canton-Potsdam Hospital. If you would prefer to receive these newsletters electronically, please send your email address to gilberta@clarkson.edu. You can access current and previous Potsdam Fibromyalgia Support Group Newsletters on our web site: www.people.clarkson.edu/~lnrussek/FMSG.