PEDIATRIC_NURSING
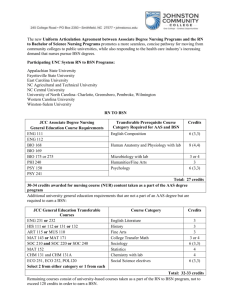
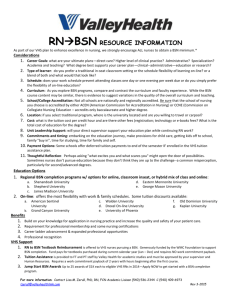
advertisement

The Royal Pentagon Review Specialist Inc. Pediatric Nursing GROWTH AND DEVELOPMENT Growing complex phenomenon of a structure or whole GROWTH Increase in physical size of a structure or whole Quantitative 2 parameters o Weight Most sensitive measurement for growth Weight gain: 2x = 5 – 6 mos. 3x = 1 year 4x = 2 – 2½ years o Height ESTROGEN responsible for increase in height in female TESTOSTERONE responsible for the increase in height in male Stoppage of height coincide with the eruption of the wisdom teeth - 1”/ mo – 1 – 6 mos - 1.5”/ mo – 7 – 12 mos - 50 % - 1st Year HEIGHT COMPARISON 9 y/o male = female 12 y/o Male < Female 13 y/o Male > Female DEVELOPMENT Increase in the skills or capacity to function Qualitatively How to measure development o By simply observing the child doing simple task o By noting parent’s description of the child’s progress o Measure by DENVER DEVELOPMENTAL SCREENING TEST (DDST) MMDST o Metro Manila Developmental Screening Test o Philippine Based exam Main Rated Categories o LANGUAGE ability to communicate o PERSONAL/ SOCIAL ability to interact o FINE MOTOR ADAPTIVE ability to use hand movements o GROSS MOTOR SKILLS ability to use large body movements MATURATION Synonymous with development Readiness/ learning is effortless Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing COGNITIVE DEVELOPMENT Ability to learn and understand from experiences, to acquire and retain knowledge, to respond to a new situation and to solve problems LEARNING change of behavior IQ= [Mental Age/ Chronological Age] x 100 Normal IQ = 90 - 110 GIFTED CHILD > 130 IQ level BASIC DIVISIONS OF LIFE Prenatal o Conception to birth Infancy o Neonatal first 28 days o Formal Infancy 29th – 1 year Early Childhood o Toddler 1 – 3 y/o o Preschool 4 – 6 y/o Middle Childhood o School Age 7 – 12 y/o Late Childhood o Pre – adolescent 11 – 13 y/o o Adolescent – 12 – 13 y/o to 21 PRINCIPLES OF GROWTH AND DEVELOPMENT Growth and development is a continuous process (WOMB TO TOMB PRINCIPLE) begins from conception and ends with death Not all parts of the body grows at the same time or at the same rate (ASSYCHRONOUS GROWTH) Each child is unique Growth and development occurs in a regular direction reflecting definite and predictable patterns or trends o Directional Terms Cephalocaudal/ Head to Tail It occurs along bodies long axis in which control over head, mouth and eye movemens and precedes control over upper body torso and legs Proximo – Distal/ Centro – Distal Progressing from center of the body to the extremities Symmetrical/ Each side of the Body Develop at the same direction at the same time and at the same rate Mass – Specific Differentiation – SIMPLE TO COMPLEX; BROAD TO REFINED o Sequential Trend Involves a predictable sequence of growth and development to which the child normally passes Locomotion Creeps Stands Walks Run Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Language and Social Skills Cry coo Secular Trend Refers to the worldwide tend of maturing earlier and growing larger as compared to succeeding generation o BEHAVIOR most comprehensive indicator of developmental stages o act @ your age PLAY universal language A great deal of skills is learned by practice There is optimum time for initiation of experience or learning Neonatal reflexes must be lost first before development can proceed o persistent primitive infantile reflexes is a possible case of cerebral palsy PATTERNS OF GROWTH AND DEVELOPMENT Renal digestive circulatory musculoskeletal o childhood Brain CNS Neurologic Tissue rapidly grows with in 1 – 2 years o Brain achieves its adult proportion @ 5 years o Rapid growth and development of brain from1 – 2 years o Malnutrition may result to Mild Mental Retardation Lymphatic System (Lymph Nodes) o Grows rapidly during infancy and childhood o Provide protection against infection o TONSIL reach its adult proportion @ 5 years Reproductive o Grows rapidly during puberty RATES OF GROWTH AND DEVELOPMENT Fetal and Infancy o Period of most rapid growth and development o Prone to develop anemia Toddler o Period of slow growth and development Toddler and preschool o Period of alternating rapid and slow growth and development School Aged o Slower growth and development o Least to develop anemia Adolescent o Period of rapid growth o Secondary prone to anemia Two Primary Factors Affecting Growth and Development Heredity o Race o Sex o Intelligence o Nationality Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Environment o Quality of Nutrition o Socio Economic Status o Health o Ordinal Position in the family o Parent – Child Relationship *Universal Principle: F are born < wt. than M by 1 oz.; F are born < lt. than M by 1 in. THEORIES OF DEVELOPMENT Developmental Task A skill or growth responsibility arising at a particular time in the individual’s life. The successful achievement of which will provide a foundation for the accomplishments of the future tasks SIGMUND FREUD’S PSYCHOSEXUAL THEORY 1856 – 1939 An Austrian Neurologist Founder of Psychoanalysis 1st to introduce Personality Development Phase Age Site of Activities Gratificati on Oral 0 – 18 Mouth Biting Phase mos. Crying Sucking (enjoyment and release of tension) Anal 19 mos. – Anus Elimination Phase 3 yrs. Retention/ (stage Defecation of where Feces OC are develop ed) Phallic Phase 4 – 6 yrs. Genital Jomar Anthony D. Maxion, BSN, RN May show exhibitionism Task Provide oral stimulation even if baby is place NPO (use pacifier)CBQ Never discourage thumb sucking Help the child achieve bowel and bladder control even if the child is hospitalized Principle of holding on and letting go Mother wins or child wins Child Wins o Holding on o Child turns to be hardheaded, antisocial, stubborn, unreliable, irresponsible Mother Wins o Letting go o Child turns to be kind, obedient, perfectionist o Meticulous, OCs, reliable, responsible Accept the child fondling his own genetalia as normal area of PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Have or increase knowledge of 2 sexes Latent Phase 7 – 12 yrs. School aged Genital Phase 12 – 18 yrs Genitalia Period of suppression No obvious development, slower growth Child’s energy or Libido is diverted into more concrete type of thinking Achieve sexual maturity and learn to establish satisfactory relationship with the opposite sex Pediatric Nursing exploration Divert attention from masturbation Answer the child’s question directly Human sexuality Help the child achieve (+) experiences so that he’ll be ready to face the conflicts of adolescents Give opportunity to relate to opposite sex ERIK ERICKSON’S STAGES OF PSYCHOSOCIAL THEORY Former student of Freud Stresses the importance of culture and society to the development of one’s personality “environment” 1. Trust vs. Mistrust 0 – 18 months TRUST is the foundation of all psychosocial tasks Theme: Give and Receive Trust is developed via o Satisfying needs of infants on time o Care must be consistent and adequate o Give experiences that will add security Hugs, kisses, touch, eye to eye contact, soft music 2. Autonomy vs. Shame & Doubt 18 mos. to 3 years Theme: independence and self – government Give opportunity for decision making, offer choices Encourage the child to make decision rather than judge Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Parents has a moral obligations to set limits 3. Initiative vs. Guilt 4 – 6 years old Learns how to do BASIC things Give opportunity exploring new places and events Right time for amusement park and zoos Activity recommended: modeling clay and finger painting Enhances creativity and imagination and facilitates fine motor development 4. Industry vs. Inferiority 7 – 12 years old Learns how to do things well Give appropriate short assignments and projects Unfinished project will develop inferiority 5. Identity vs. Role Confusion 12 – 18 or 20 years old Learns who he is or what kind of person he will become by adjusting to new body image and seeking EMANCIPATION/ freedom from parents 6. Intimacy vs. Isolation 18 – 25 or 30 years old Career focus Looking for a lifetime partner 7. Generativity vs. Stagnation 30 – 45 years old 8. Ego Integrity vs. Despair 45 years old and above JEAN PIAGET’S STAGES OF COGNITIVE DEVELOPMENT Reasoning powers Swiss Psychologist Genetic Epistemologist 1. Sensorimotor 0 – 2 years old Also called Practical Intelligence o words and symbols are not yet available o communication through senses 1. Schema 1: Neonatal Reflex o 1 month o Early reflexes 2. Schema 2: Primary Circular Reaction o 1 – 4 months o Activities related to body; repetition of behavior Example: thumbsucking 3. Schema 3: Secondary Circular Behavior o 4 – 8 months o Activities not related to the body o Discover person and object’s permanence Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Memory traces are present and anticipate familiar events 4. Schema 4: Coordination of Secondary Reaction o 8 – 12 months o Exhibit goal directed behavior o sense of permanence and separateness o Play activities: Throw and retrieve 5. Schema 5: Tertiary Circular Reaction o 12 – 18 months o use trial and error to discover characteristic of places and events o “Invention” of new means o capable of space and time perception 6. Schema 6: Invention of New Means thru Mental Coordination o 18 – 24 months o Symbolic representation o Transitional phase to the pre-operational thought period 2. Pre-operational Thought 1. Pre – conceptual Thought o 2 – 4 years old o Concrete, literal, static thinking o CBQ EGOCENTRIC – unable to view anothers viewpoint o CBQ (-) REVERSIBILITY – in every action there is opposite reaction; cause and effect o Concept of time is only now and concept of distance is only as far as they can see o CBQ ANIMISM – consider inanimate object as alive 2. Intuitive Thought o Beginning of causation 3. Concrete Operational o 7 – 12 years old o SYSTEMATIC REASONING as solution to problems o Concept of (+) reversibility o Concept of Conservation – constancy despite of transformation o Activity recommended: Collecting and Classifying 4. Formal Operational o 12 years old and above o Period when cognition achieve its final form o Can solve hypothetical problem with SCIENTIFIC REASONING o Can deal with past, present and future o Capable of ABSTRACT, mature thought and formal reasoning o Activity recommended: talk time; focus on opinions and current events KOHLBERG’S THEORY OF MORAL DEVELOPMENT Recognized the theory of moral development as considered to closely approximate cognitive stages of development Stages of Moral Development o Infancy o Premoral o Amoral Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. o Age Pediatric Nursing Pre-religious Stage 0 – 3 yrs 1 4 – 7 yrs. 2 4 – 10 yrs. 3 10 – 12 yrs. 4 Older than 12 5 6 Descritption PRECONVENTIONAL (Level I) PUNISHMENT/ OBEDIENCE/ ORIENTATION o Heteronomous morality o Child does right because PARENT tells him to and to avoid punishment INDIVIDUALISM o Instrumental purpose and exchange o Carries out action to satisfy own needs rather than society o Will do something for another if that person does something for the child CONVENTIONAL (Level II) ORIENTATION TO INTERPERSONAL RELATIONS OF MUTUALITY o Child follows rules because of need to be a “good person” in own eyes and eyes of others MAINTAINANCE OF SOCIAL ORDER, FIXED RULES AND AUTHORITY o Child finds following rules satisfying o Following rules of authority figures as well as parents in an effort to keep the “system” working POST – CONVENTIONAL (Level III) SOCIAL CONTRACT, UTILITARIAN LAW – MAKING PERSPECTIVE o Follows standards of society for the good of the people UNIVERSAL ETHICAL PRINCIPLE ORIENTATION o Follows internalized standards of conduct o Only few people achieved this level o Only saints and holy DEVELOPMENTAL MILESTONES Major marker of growth and development Determines developmental delays TEETH QUESTIONS 6 mos. Eruption of first temporary teeth 2 LOWER CENTRAL INCISORS 30 mos. Temporary teeth complete 20 decidous teeth POSTERIOR MOLAR --> last to appear Time to go to Dentist Begins to brush teeth 3 years Tooth brushing with minimal supervision 6 years Tooth brushing alone Temporary teeth begins to fail 1st permanent teeth 1st MOLAR Last to appear WISDOM TOOTH Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing BOWEL/ BLADDER CONTROL Bowel Control 18 months / 1 ½ years Day Time Bladder Control 2 years Night Time Bladder Control 3 years MILESTONES Infancy Solitary play o Consider when choosing a play Safety Age appropriateness Hygiene Fear: Stranger Anxiety o Begins: 6 – 7 months o Peaks: 8 months o Diminishes: 9 months Neonate Complete head lag Largely reflex visual fixation for human face Hands fisted with thumbs in Cries without tears because lacrimal glands are not fully developed 1 month Dance reflex disappears Looks at mobile; follows midline Alert to sound, regards face 2 months Holds head up when in prone Social smile, cries with tears, cooing sound Closure of posterior fontanel (2-3 months) Head lag when pulled to sitting position No longer clinches fist tightly Follows object past midline Recognizes parents 3 months Holds head and chest up when in prone Holds hands open at rest Hand regard, follows object past midline Grasp and tonic neck reflexes are fading Reaches for familiar people or object Anticipates feeding 4 months Head control complete Turns front to back; needs space to turn Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Laughs aloud; Babbling sound Babinski Reflex disappears 5 months Turn both ways (roll over) Teething rings, handles rattle well Moro reflex disappears (5 – 6 months) Enjoys looking around environment 6 months Reaches out in the anticipation of being picked- up Sits with support Puts feet in mouth in supine position Eruption of first temporary teeth ( Lower 2 central incisors) Vowel sounds “ah, eh” Uses palmar grasp; handless bottle well Recognizes strangers 7 months Transfer objects from hand to hand (6 – 7 months) Likes objects that are good sized for transferring 8 months Sits without support Peak of stranger anxiety Plantar reflex disappear (6-8 months) 9 months Creeps or crawls; need space for creeping Neat pincer grasp reflex, probes with forefinger Finger feeds, combine 2 syllables “mama & dada” 10 months Pulls self to stand Understand the word no Respond to name Peek – a – boo, pat a cake, since they can clap 11 months Cruising, stand with assistance Walking while holding to his crib’s handle One word other than mama and dada 12 months Stands alone Walk with assistance Drink from cup, cooperates in dressing Says two words other than mama and dada Pots & pans, pull toys and nursery rhymes Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Imitates actions, comes when called Follows one – step command and gesture Uses mature pincer graps, throws objects Toddlerhood Parallel Play – 2 toddlers playing separately Provide 2 similar toys for 2 toddlers Toys o Squeaky frogs to squeeze o Waddling ducks to pull o Trucks to push o Building blocks o Pounding peg Fear: Separation Anxiety o Begins: 9 months o Peaks: 18 months o 3 stages Protest Despair Denial o Prevent: Do not prolong goodbye Say goodbye firmly Say when you’re back Toddler Characteristic Traits Negativistic: says no most of the time Saying no – way of developing independence Limit questions, offer choices Rigid, ritualistic and stereotyped Ritualistic – way to gain mastery Temper Tantrums o Stomping of feet o Holding breath o Screaming o Head banging o NC: Ignore the behavior Scaphoid abdomen – underveloped abdominal muscle Physiologic Anorexia food fad, food jag that last for a short period of time due to the preoccupation to environment 15 Months Plateau stage CBQ WALKS ALONE – lateness in walking is a sign of mild mental retardation Puts small pellets into small bottle Creep upstairs 4 – 6 words Scribbles voluntarily with pencil, holds spoon well, seat self in a chair Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing 18 Months Height of POSSESIVENESS – favorite word MINE Bowel control achieved No longer rotates a spoon Can run and jump in place Walks up and downstairs holding on to a person’s hand or railing, typically places both feet on one step before advancing Names one body part 24 months TERRIBLE TWOS Turns pages one at a time, removes shoes, pants, etc Can open doors by turning door knobs, unscrew lids 50 – 200 words (2 word sentences), knows 5 body parts Walk upstairs alone, still using feet on the same step at same time Daytime Bladder Control CBQ best time to bring the child to dentist: 2 – 3 years or when temporary teeth is complete 30 months Makes simple lines or stroke or crosses with pencil Can jump down from chair Knows full name, holds up finger to show age Copy a circle CBQ Temporary teeth complete (posterior molar: last to erupt) CBQ 20 deciduous teeth CBQ tooth brushing: 2 – 3 years 36 months TRUSTING THREES Tooth brushing with little supervision Unbutton buttons Draws a cross, learns how to share Knows full name and sex Speaks fluently, 200 – 900 words NIGHTIME BLADDER CONTROL achieved Rides tricycle Preschoolers Cooperative play – playhouse Role playing is usual Fears: o Castration/ Body Mutilation o Dark places and witches o Thunder and lightning o Ghost Curious, creative, imaginative and imitative Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Preschooler’s Characteristic Traits Telling tall tales Imaginary friend way of relieving tension and anxiety Sibling rivalry jealousy to a newly delivered baby Regression o Signs: bedwetting o Thumbsucking o Baby talk o Fetal position Masturbation o Sign of boredom o Divert attention o Offering toy 4 years old FURIOUS FOUR Noisy, aggressive and stormy Buttons button Copy square Catches ball, jumps, skips Alternates feet going downstairs CBQ LACES SHOES Vocabulary of 1500, knows the basic color Says song or poem from memory 5 years old FRUSTRATING FIVES Jumps over low obstacles Spreads with a knife Draws 6 part man, copy triangle Imaginary playmates 2100 words Identification with same sex Attachment to opposite sex School – Aged Competitive Play: Tug of war Fears o School Phobia orienting child to his new environment o Displacement from school o Death Significant Person o Teacher o Peer of same sex Stoppage of height coincide with the eruption of wisdom tooth Prone to fracture: Common Green stick Mature vision o 20/200 legal blindness They’ll Cheat can’t afford to lose Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing 6 years old Temporary teeth begins to fall, permanent teeth begins to appear (1st: First Molar) Tooth brushing alone A year of continuous motion, clumsy moving 1st grade teacher becomes authority figure o nail biting sign of strict teacher Beginning interest with God 7 years old Age of assimilation Copies a diamond Enjoys teasing and playing alone Quieting down phase 8 years old Expansive age Smoother movements Normal homosexual Loves to collexct objects Counts backwards 9 years old Coordination improves Tells time correctly Hero worship Stealing and lying are common Takes care of body needs completely Teachers find their group difficult to handle 10 years old Age of special talents Write legibly Ready for competitive games More considerate and cooperative Joins organizations Well mannered with adults and critical with adults 11 – 12 years old Pre adolescent Full of energy and constantly active Secret languages are common Share secrets with friends Sense of humor is present Social and coopoerative School – Aged Characteristic Traits Industrious Modest Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Signs of Sexual Maturity in Female I ncrease in size of breast and genitalia – telarche – 1st sign W idening of hips A ppearance of pubic axilliary and pubic hair - adrenarche M enarche – last sign Signs of Sexual Maturity in Male A ppearance of axilliary and pubic hair D eepening of voice D evelopment of muscle I ncrease in size of penis and scrotum – 1st sign P roduction of viable sperm – last sign Adolescence Fear o Acne o Obesity o Homosexuality o Death o Replacement from friends Peer of opposite sex significant other Experiences conflicts between his needs for sexual satisfaction and societal expectations Core Concern o Change of body image o Acceptance of the opposite sex Nocturnal Emission: Wet dreams o Hallmark of adolescence CBQ distinctive odor due to stimulation of apocrine gland Testes and scrotum increases until age 17 Sperm is viable by age 17 Breast of female and genitalia increases until age 18 Signs of sexual maturity Characteristic traits o Idealistic, rebellious, reformers o Parent child conflict o Very conscious with body image o Peer pressure Problems o Vehicular accident o Smoking o Alcoholism o Drug Addiction o Pre Marital Sex Concept of Death 6 years old death is reversible CBQ 7 – 9 years old personification of death, permanent loss of the corporal life Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing IMMEDIATE CARE OF THE NEWBORN 8 PRIORITIES OF THE NEWBORN IN THE FIRST DAYS OF LIFE 1. Initiation and maintenance of respiration 2. Establishment of extrauterine circulation 3. Control of body temperature 4. Intake of adequate nutrition 5. Establishment of waste elimination 6. Prevention of infection 7. Establishment of an infant – parent relationship 8. Developmental care that balance rest and stimulation for mental developmental INITIATION & MAINTENANCE OF RESPIRATION Alerts! Expulsion is @ 2nd stage of labor Most neonatal deaths w/in the first 24 hours is due to INABILITY TO INITIATE AIRWAY Lung function begins only after birth How? Support head and remove secretion Proper suctioning with a catheter o Place baby’s head to side facilitates drainage o Suction the mouth first before nose newborns are nose breathers o Period of 5 – 10 seconds, should be gentle and quick Prolonged suctioning can cause hypoxia, laryngospasm and bradycardia due to vagal nerve stimulation o Evaluate patency Cover 1 nostril, if newborn struggles, additional suctioning needed If not effective requires effective LARYNGOSCOPY to open airway. After deep suctioning, and ET tube can be inserted and O2 administration by (+) Pressure Bag and mask with 100% O2 @ 40 – 60 bpm Alerts in O2 Administration No Smoking O2 is combustible Must be humidified prevent drying of mucosa Cover the nose and mouth only Scarring Retina results Retinopathy (O2 overdose) Meconium Stain never administer O2 with pressure causes atelactasis ESTABLISHMENT OF EXTRAUTERINE CIRCULATION Alerts! Circulation id initiated by LUNG EXPANSION and PULMONARY VENTILATION Completed by cutting the cord Assess characteristics of cry o Normal strong, vigorous, lusty cry o Hypoglycemia/ Increased ICP high pitched, small cry o Never stimulate crying before all secretion are remove to prevent aspiration Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Feto – Placental Circulation Placenta O2 carried by vein liver Inferior Vena Cava Right atrium 70% goes to Foramen Ovale Remaining 30 tricuspid valve right ventricle pulmonary artery lungs for nutrition vasoconstriction of lung tissue pushes the blood to DUCTOS VENOSUS supply extremities 2 arteries carry unO2 Blood back placenta Ways to facilitate closure of Foramen Ovale Tangential Footslap o Cry expands lung pressure from left to right side of the heart Proper positioning of the Baby o Right side lying position pressure on left side of heart facilitating closure Best Position immediately after Birth CS supine, crib – level position NSD Structure Foramen Ovale Appropriate Time of Obliteration 1 year Complete Closure Ductus Arteriosus 1 month Ductus Venosus Umbilical Arteries Umbilical Vein 2 2 – 3 month W/in 24 hrs completed 1 month W/in 24 hrs completed 1 month 2 – 3 months 2 – 3 months 2 – 3 months 2 –3 months Structure Remaining Failure to Close Fossa Ovalis Atrial Septal Defect Patent Ductus Arteriosus Ligamentum Arteriosum Ligamentum Venosum Lateral Umbilical Artery (Intrerior Iliac Artery) Ligamentum Teres (Round ligament of the liver) Signs of Increased ICP Abnormal large head Bulged & tensed fontanel Projectile Vomiting surest sign of cerebral irritation Cushing Triad of ICP o BP o PR o RR High pitched, shrill cry Dilopia normal in newborns, sign of ICP in older children CONTROL OF BODY TEMPERATURE/ TEMPERATURE REGULATION Alerts! The goal of temperature regulation is to maintain Temperature not less than 97.7 F or 36.7 C Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Factors leading to the development of Hypothermia Preterm are born POIKILOTHERMIC (easily adapt the temperature of environment due to immaturity of thermo regulating center of the body HYPOTHALAMUS) Inadequate subcutaneous tissues Newborn are not yet capable of shivering Newborns are wet Process of Heat Loss Evaporation body to air Conduction body to solid objects (cold compress) Convection body to a cooler surrounding object (fever, aircon) Radiation body to a cold subject not in contact with the body (thermal shift) Effects of Hypothermia (COLD STRESS) RR first sign of hypothermia Hypoglycemia due to utilization of glucose o Normal 45 – 55 mg/ dl o Average/ borderline 40 mg/ dl Metabolic Acidosis due to the catabolism of BROWN FAT (vest-like, best insulators of newborns) leading to the formation of ketone bodies High risk for KERNICTERUS (bilirubin in the brain) Additional fatigue added to already stressful heart Prevention of Cold Stress Dry and wrap the newborn Mechanical measures ( radiant warmer, acrylic sided incubator) Prevent unecesarry exposure cover areas not being examined In case of no electricity o Cover baby with thin foil o Skin to skin contact human blanket/ kangaroo care ESTABLISHING ADEQUATE NUTRITION Breastfeeding Best time NSD – ASAP CS – after 4 hours Physiology of Breastmilk Production Estrogen, Progesterone releases PROLACTIN acts on ACINAR/ ALVEOLI CELLS produces FOREMILK store in LACTIFEROUS TUBULES/ COLLECTING TUBULES Sucking stimulates posterior pituitary gland release oxytocin causes Contraction of smooth muscles of Lactiferous Tubules milk ejection reflex let down reflex Advantages of Breastfeeding Economical Promotes bonding Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Contains LACTOBACILLUS BIFIDUS interfere the attack of pathogenic bacteria in the GIT Helps in early involution of uterus oxytocin causes contraction Always available Incidence of breast cancer Breastfed babies have higher IQ than bottle fed ones Antibody IgA Macrophages Disadvantages of Breastfeeding No iron Possibility of transfer of Hepa B, HIV, CMV (13 – 39% possibility) Father can’t bond with the mother and baby instead, father can sing, suddle, kiss, put baby to sleep Alerts! Freezer good for 6 mos./ don’t reheat Should be stored in a sterile plastic container Pre – Colostrums 6 weeks Colostrums 3 Stages of Breastmilk COLOSTRUM o Present 2 – 4 days o Contents fats CHO Immunoglobulin protein fat soluble vitamin minerals TRANSITIONAL MILK o Present 4 – 14 days o Contents Lactose minerals water soluble vitamins o Lactose Intolerance deficiency in enzyme Lactase responsible for digestion of Lactose sour milk/ smelling of stool MATURE MILK o Present 14 days and above o Contents Linoleic Acid responsible for the development of brain and integrity of skin CHO (Lactose) Protein (lactabulmin) Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing COWS MILK fats – almost similar to mature milk Causes constipation Content o fats o CHO add sugar o CHON casein hard to digest o Minerals (has traumatic effect to kidneys of babies) o PHOSPHORUS ( causes inversely proportional effect of Calcium water to prevent kidney stones Health Teachings 1. Proper Hygiene Hand washing, clean areola with cotton and water or NSS Cleanse the area with CAKE COLOSTRUM 2. Position while Breastfeeding Upright Sitting (best position) 3. Stimulate and Evaluate Feeding Reflexes Rooting Reflexes o Stimulate by touching the side of the cheek or side of flip then the baby will turn to the syimulus o Purpose: to look for food o Disappear by 6th weeks Sucking Reflexes o Stimulate the middle part of the lips and the baby will suck o Disappear by 6 months Swallowing Reflexes o When the food touches the posterior part of the tongue, the baby will automatically swallow o Never disappears Extrusion Reflexes o When food touches anterior part of tounge, it will extrude/ protrude o Purpose: prevent poisoning o Disappears @ 4 moths 4. Criteria for effective sucking Baby’s mouth is hiked well – up @ areola Mother experiences after pain sign of releasing oxytocin thereby contracting uterus The other nipple is also flowing with milk 5. To prevent from crack nipples and initiate proper production of oxytocin Begin initially for 2 – 3 mins/ breast the time 1 min/ breast/ day until it reaches 10 minutes/ breast/ feeding or 20 min/ feeding 6. For proper emptying and continuous milk production per feeding Feed the baby at the last breast that you fed him/ her Problems experience in Breastfeeding ENGORGEMENT o Feeling of fullness and tension in the breast (3rd Day) Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. o o Pediatric Nursing Breastfeeding mother apply warm compress Bottle – Feeding apply cold compress, wear supportive bra SORE NIPPLE/ CRACK NIPPLE o Crack, red, painful nipple o Causes Breastfeeding @ one side only Unhealthy sexual practices o Management Breastfed using the unaffected side Manually express milk @ affected side Antibiotic (continue breastfeeding) MASTITIS o Inflammation of breast o Causative Agent: STAPHYLOCOCCUS AUREUS o Management Avoid wearing lined/ wired bra o 4 weeks – Breast Involution Contraindications for Breastfeeding Maternal Conditions o HIV o Hepa B o CMV o Coumadin/ Warfarin taking moms give heparin instead Newborn Conditions o Erythroblastocis Fetalis o Inborn errors of metabolism Hydrofetalis Phenylketonuria Galactosemia Tay- Sach’s Diseas ESTABLISHMENT OF WASTE ELIMINATION GIT Obstructions Hirshsprung Disease Imperforate Anus Meconium Ileus (common with Cystic Fibrosis) Different Stools MECONIUM/ PHYSIOLOGIC STOOL o Blackish green o Odorless (sterile intestine) o Normally passed within 24 hours o Tar like o Sticky TRANSITIONAL STOOL Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. o o o o Pediatric Nursing Present 4 – 14 days Green Loose Slimy that may appear like diarrhea to the untrained eyes BREASTFED STOOL o Golden yellow o Occur almost nearly after feeding o With sour milk smell o Mushy o Soft BOTTLEFED STOOL o Pale yellow o Hard due to casein o Formed o Typically offensive odor o Seldom passed 2 – 3 days INDICATION OF STOOL CHANGES Light Stool With jaundice Bright Green Under phototherapy Mucus –mixed Milk Allergy Clay Colored Bile Duct Obstruction Black GIT Hemorrhage Blood – Flecked Anal Fissure Curant Jelly Intussuception Fatty, bulky, foul Suspect malabsorption smelling/ Steatorrhea syndrome/ Cystic Fibrosis/ Celiac Disease Ribbon – like Hirshsprung disease ASSESSMENT OF WELL BEING Apgar Scoring Virginia Apgar Special Consideration 1st 1 minute determines general coneral condition of the baby Next 5 Minute determines the capability of the baby to adjust extrauterinely (most important) Next 15 minutes optional depndent on the 5 minutes apgar score Components A ppearance P ulse Rate G rimace A ctivity R espiration Color upon birth is slightly cyanotic After first cry baby will be pink Take apical pulse at the lower left nipple Determines reflex irritability using tangential foot slap and catheter insertion To determine the degree of muscle tone Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Newborns will cry within 30 seconds upon expulsion ASPHYXIA NEONATORUM failure to cry within 30 seconds because mother received Demerol NARCAN antidote of Demerol APGAR SCORING Criteria 0 Heart Rate Absent Respiratory Effort Absent Muscle Tone Flaccid Extremities Reflex Irritability Catheter No Response Tangential FS No Response Color Blue / Pale High score means healthy baby Score 1 < 100 Slow RR/ Weak Some reflexes 2 > 100 Good strong cry Well Flexed Grimace Grimace Acrocyanosis Cough or sneeze Cry Pink Interpretation 0-3 Severely depressed Needs CPR Admission at NICU 4-6 Moderate depression Additional suctioning 7 – 10 Good and healthy CARDIOPULMONARY RESUSCITATION CPCR cardiopulmonary and cerebral resuscitation 5 minutes of 02 deprivation will cause irreversible brain damage Priority: Airway, Breathing, Circulation AIRWAY Clear the airway Shake the baby If no response, call help Immediately do 1 minute CPR before calling for help Flat on bed, put a board if the bed is soft Head tilt – chin lift maneuver No head tilt for suspect of cervical damage Overextension may cause occlusion BREATHING Ventilating the lungs Check breathlessness If breathless give 2 breaths Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing If newborn mouth and nose If child mouth and pinch the nose Force puff only Use one way mask to prevent contact with the secretion CIRCULATION By cardiac compression Check if pulseless Use brachial pulse children No breath + No pulse CPR Infant 1 finger breadth below nipple line, 2 finger 1 year old heal of the palm CPR RATIO Adult 2:15 Infant 1:5 REPIRATORY EVALUATION (SILVERMAN – ANDERSON INDEX) Criteria Chest movement Intercoastal retraction Xiphoid Retraction Nares dilatation Expiratory Grunt 0 Synchronized No retraction No retraction No dilatation None Score 1 Long on inspiration Just visible Just visible Minimal Heard by stet only 2 See-saw Marked Marked Marked Heard by ear Low score means Good condition of the baby Interpretation 0 – 3 normal, no RDS 4 – 6 with moderate RDS 7 – 10 with severe RDS ASSESSMENT OF GESTATIONAL AGE (Ballard and Dubowitz) Score Criteria Less 36 weeks 37 – 38 Weeks Sole creases Anterior transverse Occasional 2/3 only Breast nodule (dm) 2 mm 4 mm (3 – 5 cm) Scalp Hair Fine and fuzzy Fine and fuzzy Ear Lobe Pliable Some Testes and In lower canal, Some intermediate Scrotom covered testes with rugae 39 weeks and up Sole cover with crease 7 mm (>5cm) Course and silky Thick Testes pendulous, scrotum full, extensive rugae PRETERM BABIES babies delivered after 20 weeks and before 37 weeks sign of preterm – less 36 weeks according to Ballatrd and Dubowitz plus frog legs or lax position Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Hypotonic – prone to repiratory infection There is a Scarf Sign elbow passes midline Square window – wrist 90 deg. Angle Heal to ear sign Anterior traverse crease Abundant lanugo Prominent labia minora and clitoris POST TERM BABIES Delivered after 42 weeks Old mans face – classic sign Desquamation – pealing of skin Long and brittle fingernails Wide and alert eyes NEONATES IN THE NURSERY Nursing Responsibilities upon Receiving the Baby 1. Proper identification o Foot print of the baby and the thumb mark of the mother 2. Take anthropometrics measurement o Length 19. 5 – 21 inches Ave: 20 inches 47.5 – 53 cm Ave: 50 cm. o Head Circumference 13 – 14 inches 33 – 35 cm Ave: 34 cm o Chest Circumference 12 – 13 inches 31 – 33 cm Ave: 32 cm o Abdominal Circumference 12 – 13 inches 31 – 33 inches Ave: 32 cm 3. Bathing the baby o Give oil Bath To cleanse the baby and spread the vernix caseosa 2 functions of vernix caseosa insulator bacteriostatic o Full bath is given when cord falls off o Babies of HIV + mothers will be given a full bath immediately after the birth to lessen the transmission of HIV 4. Dressing the Umbilical Cord o Strict asepsis to prevent tetanus neonatorum that is why mothers are given tetanus toxoid while pregnant CHN – 3 Cleans Hand Surface Cord o Betadine (Povidone Iodine) Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Check 3 vessels (AVA) If only 2 vessels is seen suspect that the baby has a kidney malformation 1 inch above the base of the cord when cutting But if IV infusion or blood transfusion is going to be given to the newborn, leave at least 8 inches of the umbilical cord Umbilical cord is the best site for IV and blood transfusion because it has no nerve and no pain OMPHALAGIA bleeding of the cord for more than 30 cc, suspect hemophilia The umbilical cord turns black by the 3rd day and falls of 7 – 10th day UMBILICAL GRANULATION failure of the cord to fall after 2 weeks without foul odor, bring the baby to the hospital and will be given Silver Nitrate or will be cauterized Clean the umbilical cord with saline or 70% alcohol It should be dry PATENT URACHUS itf the cord is always moist, suspect a fistula between the bladder and the umbilicus, do NITRAZINE PAPER TEST (+ for urine if it turns yellow) 5. Crede’s Prophylaxis o Purpose: to prevent opthalmia neonatorum or gonnorheal conjeunctivitis o If mother has an untreated gonorrhea and passed the baby vaginally o ERYTHROMYCIN OPTHALMIC OINTMENT drug of choice, inner to outer canthus o Before 1989 – 2 drops of 2% silver nitrate at lower conujunctival sac o It should be washed immediately after 1 minute to prevent burning 6. Administration of Vitamin K o Purpose: to prevent hemorrhage related o physiologic hypoprothrobinemia o Other name Aquamephyton, Phytomenadone, Konakion 0.5 – 10.5 mg IM @ vastus lateralis or lateral anterior thigh o Preterm give 0.5 mg o Vit. K is synthesized at the intestine o On the 7th day, there is prothrombin 7. Weight Taking o Normal Weight 3000 – 3400 gm 3 – 3.4 kg 6.5 – 7.5 lbs o Arbitrary Lowe Limit 2,500 grams o Low Birth Weight < 2,500 g it is not the same for gestational age o Small for Gestational Age Less than the 10th % rank o Large for Gestational Age > 90% rank Macrosomia – baby delivered 4,000 g or 4 kilos Diabetic mother o Appropriate for Gestational Age Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. o Pediatric Nursing Physiologic Weight Loss 5 – 10% physiologic weight loss 10th days after birth PHYSICAL EXAMINATION AND DEVIATION FROM THE NORMAL Important Consideration If the client is a newborn, cover areas that is not being examined (prevent hypothermia) If the client is an infant, he first vital sign to take is the RR because of fear of stranger will change the normal respiration. Begin from at least intrusive to the most intrusive procedure. If the client is a toddler and preschooler, le them handle the instruments like stethoscope or play syringe. If the client has security blanket (like stuffed toy) give it to them to lessen anxiety If the client is a school age and adolescent, explain the procedure and respect their modesty Components Temperature o Temperature of the newborn is taken rectally o Rectal temperature taking is done only once to rule out imperforated anus o Insert thermometer 1 inch inside the anus o Types of Imperforated Anus No Anal Openning AtreticAgenetice o These two is the most dangerous because there is failure to pass meconium after 24 hours o There is abdominal distention o Foul odor breath o Vomitus of fecal material which might result in aspiration and casue respiratory problems o Management: Surgery with temporary colostomy With anal openning Stenos Membranous Cardiac Rate o Newborn 120 – 160 bpm irregular o Radial pulse of a newborn is normally absent o If radial pulse is prominent suspect that there is a PDA o Femoral pulse is normally palpable, if absent suspect Coarctation of Aorta CONGENITAL HEART DISEASE Common in Boys o Transposition of the great artery (TOGA) o Truncus Arteriosus o Tetralogy of Fallot Common in Girls o Patent Ductus Arteriosus Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. o Pediatric Nursing Atrio Septal Defect Causes o Familial tendency o Exposure to rubella/ German measles – 1st month o Failure of the Heart Structure to progress Two Major Types Acyanotic Heart Defects shunting from left to right Cyanotic Heart Defects from right to left Acyanotic Heart Defects with Increase Pulmonary Blood Flow 1. Vetricular Septal Defect Opening Between 2 ventricles Signs and symptoms o Systolic murmur at lower border of the sternum and no other significant sign o Cardiac catheterization reveals increase oxygen saturation at the right side of the heart o ECG reveals hypertrophy of the right side of the heart o Only 50% of the oxygenated blood will go to the aorta Management o Open heart surgery o Placing the client on a long tern antibiotic therapy to prevent the development of sub-acute bacterial endocarditis o Protect site of catheterization (right femoral vein) o Avoid flexion of joints 2. Atrial Septal Defect Failure of the foramen ovale to close Signs and symptoms o Systolic murmur at the upper border of the sternum with no significant sign o Cardiac catheterization reveals increase oxygen saturation at the right side of the heart o 50% of the blood goes to the right atrium Management o Open heart surgery o Placing the client on a long tern antibiotic therapy to prevent the development of sub-acute bacterial endocarditis 3. Endocardial Cushion Defect AV canal affecting both the tricuspid and the mitral valve Signs and symptoms o Only confirmed by cardiaccatheterization o Valves are closed 4. Patent Ductus Arteriosus Failure of the Ductus Arteriosus to close Signs and symptoms Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Prominent radial pulse o Continuous machinery like murmur o ECG reveals hypertrophy of the left ventricle Management o Indomethacine – prostaglandin inhibitor that facilitate closure of PDA o Ligation of PDA by 2 – 4 years old Acyanotic Heart Defects with Decrease Pulmonary Blood Flow 1. Pulmonary Stenosis Narrowing of valve of pulmonary artery Signs and symptoms o Typical systolic ejection murmur o S2 sound is widely split o ECG reveals right ventricular hypertrophy o Only 50% of the blood goes to the lungs Management o Balloon Stenotomy 2. Aortic Stenosis Narrowing of valve of aorta Signs and symptoms o Typical systolic ejection murmur o Murmur o ECG reveals right ventricular hypertrophy o Only 50% of the blood goes to the body o Angina like symptoms may be present when active Management o Balloon stenotomy 3. Duplication of Aortic Arch Doubling of arch of the aorta causing compression to the trachea and esophagus Signs and symptoms o Dysphagia – due to esophageal compression o Dyspnea – due to tracheal compression o Left ventricular hypertrophy o Only 50% of the blood goes to the body Management o Close heart surgery 4. Coarctation of Aorta Narrowing of ach of aorta Outstanding signs o Absent femoral pulse o BP is higher on the upper extremities and on the lower extremities o Epistaxis o Lesser blood goes to the lower extremities Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Management o Take BP on 4 extremities o Close hear surgery Cyanotic Heart Defects with Increase Pulmonary Blood Flow 1. Transposition of Great Arteries Aorta is arising from the right ventricle while the pulmonary artery is arising from the left Signs and symptoms o Cyanosis after 1st cry o Polycythemia because of increase production of RBC, a compensatory mechanism to the oxygen supply to the body, the blood become viscous o Polycythemia will lead to: Thrombuis Embolus Stroke (CVA) o ECG reveals Cardiomegaly Management o Palliative repair – Rash Kind repair o Complete repair – Mustard repair 2. Total Anomalous Pulmonary Venous Return Situation wherein pulmonary vein instead of entering the left atrium enters the right atrium or superior vena cava Signs and symptoms o Open foramen ovale o Mild – moderate cyanosis o Absent spleen Management o Restructuring of the heart 3. Truncus Arteriosus Situation in which pulmonary artery and aorta is arising in one common trunk or a single vessel with ventricular septal defect Signs and symptoms o Cyanosis after 1st cry o Polycythemia because of increase production of RBC, a compensatory mechanism to the oxygen supply to the body, the blood become viscous o Polycythemia will lead to: Thrombuis Embolus Stroke (CVA) Management o Restructuring the heart Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing 4. Hypoplastic Left Heart Syndrome Non functioning left ventricle Signs and symptoms o Cyanosis after 1st cry o Polycythemia because of increase production of RBC, a compensatory mechanism to the oxygen supply to the body, the blood become viscous o Polycythemia will lead to: Thrombuis Embolus Stroke (CVA) Management o Heart transplant Cyanotic Heart Defects with Decrease Pulmonary Blood Flow 1. Tricuspid Atresia Failure of the tricuspid valve to open Signs and symptoms o Open foramen ovale o Cyanosis o Polycythemia because of increase production of RBC, a compensatory mechanism to the oxygen supply to the body, the blood become viscous o Polycythemia will lead to: Thrombuis Embolus Stroke (CVA) Management o Fontan Proledum 2. Tetralogy of Fallot 4 Anomalies Present (PVOR) o Pulmonary Stenosis o Ventricular Septal Defect o Overriding of Aorta o Right Ventricular Hypertrophy Signs and symptoms o High degree of Cyanosis outstanding Sign o Polycythemia because of increase production of RBC, a compensatory mechanism to the oxygen supply to the body, the blood become viscous o Polycythemia will lead to: Thrombuis Embolus Stroke (CVA) o Severe dyspnea relieved by squatting position because it will prevent venous return and facilitate maximum lung expansion Knee chest position in infants o There is growth retardation Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing TET Spells – blue spells or short episode of hypoxia Syncope – faintaing Mental retardation Clubbing in fingernails because of tissue hypoxia – late and last sign o X – ray reveal a boot shape heart Management o Oxygen therapy o Morphine sulfate – for hypoxic episode o Propanolol (inderal) – decrease heart spasm o Palliative repair – BLT or Blalock Taussig Shunt Procedure o Complete repair – Brock Procedure o o o o ACQUIRED HEART DISEASE Rheumatic Heart Disease Inflammatory disease following an infection caused by Group A Beta Hemoilytic Streptococcus Affected body parts o Musculoskeletal o Cardiac muscle o Integumentary system o CNS Tonsillitis due to love of sweets with no oral hygiene serving a good medium for bacterial growth causing inflammation Group A Beta Hemolytic Streptococcus will release toxin and enters circulation Group A Beta Hemolytic Streptococcus is an anaerobic organism and will stay at the left side of the heart or the mitral valve as an ASCHOFF BODIES ASCHOFF BODIES – round nodules with multi nucleated cell and fibroblast that stays in the miral valve Left sided heart failure because of mitral stenosis due to increase in the size of Aschoff Bodies Diagnostic Exam: JONE’S CRITERIA Major Minor Polyarthritis – multi joint pain Low grade fever Athralgia – joint pain Diagnostic Exams CHOREA/ Sydenhamm’s Chorea/ Antibody St. Vitous Dance – involuntary, C reactive protein purposeless movement of the hand ESR and shoulder accompanied by Anti Streptolysin Titer grimacing Carditis – signs of tachycardia Erythema Marginatum – macular rashes Subcutaneous nodules Presence of 2 major or 1 major and 2 minor plus a history of sore throat will confirm diagnosis Management o Bed rest Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. o o o o o Pediatric Nursing Avoid contact sports Throat swab for C & S Antibiotics – purpose is to prevent recurrence Aspirin Therapy or salicylates – act as an anti-inflammatory agent in RHD Side effect: Reye’s Syndrome encephalopathy accompanied by fatty infiltration of the organs such as the heart and liver RESPIRATION Normal Values = 30 – 60 bpm irregular Either abdominal or diaphragmatic breathing with short period of apnea without cyanosis Normal apnea in newborn is 15 seconds or less Age Newborn 1 year old 2 – 3 years old 5 years old 10 years old 15 and above Vesicular Normal Bronshovesicular Normal Bronchial Normal Ronchi Normal Rales Abnormal Wheezing Abnormal Stridor Resonace Hyper Resonance Rate 40 – 90 20 – 40 20 – 30 20 – 25 18 – 22 12 – 20 Breath Sounds Heard on Auscultation Soft, low pitched, heard over periphery of lungs, aspiration is longer than expiration Soft, medium pitched heard over major bronchi, inspiration equals expiration Loud, high pitched, heard over the trachea, expiration is longer than inspiration Snoring sound made by air moving through mucus in bronchi Crackles (like Celophane) made by air moving through fluid in alveoli Denotes pneumonia, fluid in the lungs or pulmonary edema Whistling on expiration made by air being pushed through narrowed bronchi Denotes children with asthma or foreign body airway obstruction Crowing or roster like sound made by air being pulled through a constricted larynx Indicative of Respiratory Obstruction Loud, low tone, percussion sound over normal lung tissue Louder, lower sound than resonance, percussion sound over hyperinflated lung tissue 1. RESPIRATORY DISTRESS SYNDROME Lack of surfactant within 24 hours of life Aka Hyalin Membrane Disease Common in preterm babies The alveoli cannot expand properly Signs and symptoms o Present within 4 hours of life Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Using the Silverman Anderson Scoring to determine RDS o RR with retraction (1st sign of RDS) o Expiratory Grunting (major sign) o Xiphoid retraction o Flaring nasal flares o Cyanosis o Respiratory acidosis Management o Head elevated o Proper suctioning o O2 administration with humidity o Client placed on CPAP Continuous Positive Airway Pressure PEEP Positive End Expiratory Pressure Purpose id to maintain the alveoli partially open and prevent alveolar collapse o Monitor for acidosis o Surfactant replacement 2. LARYNGOTRACHEO BRONCHITIS (LTB) Most common form of croup Viral infection of the larynx, trachea and bronchi Signs and symptoms o BARKING or CROUPY COUGH outstanding sign o Inspiratory Stridor o Respiratory acidosis o Cyanosis o Death Diagnostic Exams o Throat swab for c & s o ABG o Chest and x-ray to ruyle out epiglotitis Management o Racemic Epinephrine – bronchodilator o Humidified Oxygen 3. BRONCHIOLITIS Inflammation of the bronchioles characterized by production of tenacious mucus FLU – LIKE SYMPTOMS – outstanding sign RR Causative Agent: Respiratory Syncitial Virus Drug: Antiviral – Ribavirin LTB and Bronchiolitis ends with Epiglotitis 4. EPIGLOTITIS Inflammation of the epiglotitis Sudden onset The child always assume the tripod position Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Less than 18 months cannot cough – must be placed on mist tent or “Croup tie” – make sure that the edges are tucked in o Provide washable plastic toys or materials o Avoid toys that crate friction o Avoid toys that are hairy or furry Blood Pressure Newborn – 80 – 46 mmHg After 10 days – 100/ 50 mmHg BP taking begins by 3 years old SKIN If cyanotic after the first cry suspect Transposition of the Great Arteries 1. Acrocyanosis body is pink, extremities are blue 2. Generalized Mottling due to the immaturity of the circulatory system 3. Birthmarks a. Mongolian Spots Slate grya or bluish discoloration/ patches commonly seen across the sacrum or buttock Related to melanocyte which is common in Asian newborn Usually disappear by 1 – 5 years old (preschool) b. Milia Plugged or unopened sebaceous glands usually seen as a white pinpoint patches at the nose, chin and cheeks and will disappear by 2 – 4 weeks c. Lanugu Fine downy hair which is common in preterm d. Desquamation Peeling of the newborn’s skin within 24 hours characterized by extreme dryness that begin in the sole and palm, common in post term babies e. Stork Bites (Talengeiclasis Nevi) Pink patches at the nape, never disappears f. Erythema Toxicum (Flea Bite Rash) First self limiting rash to appear sporadically and unpredictably as to time and place g. Harlequin Sign Dependent part is pink, independent part is blue because of the immaturity of circulation, the RBC settles down h. Cutis Memorata Transitory motlling of the neonates skin when exposed to cold i. Hemangiomas Vascular tumors of the skin Types: o Nevus Flammeus/ Port Wine Stain Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o o j. Macular purple or dark red lesions usually seen on the face or thigh, disappears and be removed surgically Nevus Vasculosus/ Strawberry Hemangioma Dilated capillary in the entire dermal or subdermal area continuing to enlarge but disappear after 10 years old Cavenous Hemangiomas Consist of communicating network of venules in the subcutaneous tissue that never disappear with age Vernix Caseosa White cream cheese – like substance that serves as skin lubricant SKIN COLOR AND THEIR SIGNIFICANCE 1. Blue cyanosis , hypoxia 2. White edema 3. Gray infection 4. Yellow jaundice or carotinemia 5. Pale anemia Burn Trauma Injury to body tissues caused by excessive heat Characteristic 1st Degree Involves only the superficial epidermis characterized by erethema, Partial Thickness dryness and pain Ex: Sunburn – heals by regeneration in 1 – 10 weeks 2nd Degree Involves the entire epidermis, and portion of the dermis, Partial Thickness characterized by erythema, blistered and moist from exudates which is extremely painful Ex: Scalds 3rd Degree Involves skin layers, epidermis and dermis, may involve adipose Full Thickness tissue, fascia, muscle and bone. It appears to be leathery, white or black, not sensitive to pain since nerve ending had been destroyed Ex: Lava Burn Management: First Aid o Put out the flames by rolling the child on a blanket o Immerse the burned part on cold water o Removed burned clothing (sterile material) o Cover burned part with sterile dressing Maintainance of patent airway o Suction PRN o O2 administration with humidity o Endotracheal Intubation o Tracheostomy Prevention of shock and flued and electrolyte imbalances o Colloids to expand blood volume o Isotonic saline to replace electrolyte Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Dextrose in water to provide calories Booster dose of Tetanus Toxoid Relief pain such as IV analgesic (morphine sulfate) Prevention of wound infection o Cleaning and debriding the wound o Open or close method of wound care o Whirl pool therapy Skin grafting o 3rd degree burn o get skin from buttocks or pig skin (xenograft) or from frozen cadaver Diet CHON and calories Atopic Dermatitis Skin disease characterized by papulo-vesicular eruthematous lesions with weeping and crusting Usually caused by food allergen o Milk o Eggs o Citrus Juice o Tomatoes o Wheat Signs and symptoms o Extremely pruritus – outstanding sign o Linear excoriation o Crusty o Lichenification dry and shinny, scaly white skin Management o Avoid allergens o Prosobes/ Isomil – hypoallergenic milk o Prevent infection by proper handwashing, cut the fingernails o Hydrate with a burrows solution o Topical steroid – 1% hydrocortisone cream Impetigo Skin disease caused by Group A Beta Hemolytic Sreptococcuscharacterized by papulovesicular lesions surrounded by localized erythema becoming purulent and ooze forming honey colored crust Before the development, the baby should always been exposed to Pediculosis Capitis (kuto) Management o Proper handwashing o Treated with antibiotic Complication: AGN Acne Self limiting inflammatory disease involving sebaceous gland, common in adolescents Comadones – composed o sebum that is mainly causing white heads Sebum – composed of lipids Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Management o Proper handwashing wild mild soap (sulfur soap) and water, leave for 5 – 10 minutes or use tretenoin or Retin A – anti acne Anemia/ Pallor Caused by o Early cutting of the cord o Bleeding disorders/ blood dyscarias BLEEDING DISORDERS/ BLOOD DYSCARIAS Hemophilia Sex – linked (X) Recessive disorders The mother is the carrier The son is affected The father transmits to daughter Deficiency in clotting factor o Hemophilia A factor 8 classic hemophilia o Hemophilia B Factor 9 Christmas disease o Hemophilia C Factor 11 OMPHALAGIA earliest sign o >300 cc loss of blood during cutting of the cord the maternal clotting factor is present in the new born that is why there is a delayed diagnosis of hemophilia in toddlers sudden bruising HEMARTHROSIS major sign repeated bleeding, bleeding of the synovial membrane Diagnostic exam: PTT Nursing Diagnosis: High Risk for Injury Goal: Prevention of injury Health Teaching o Avoid contact sports o Determine the case before doing any invasive procedure In immunization change the needle into a smaller one o In case of fracture/ injury Immobilize and elevate o Cold compress o Gentle pressure o Blood transfusion of cryoprecipitate Leukemia Group of malignant disease characterized by rapid proliferation of immature RBC Ratio is 500 RBC : 1 WBC The client is immunocompromised Classification of Leukemia o Lympho – affects the lymphatic system o Myelo – affects the bone marrow o Acute/ Blastic – affects the immature cells o Chronic/ cystic – affects the mature cells Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Acute Lymphocytic Leukemia Most common in children Increase immature WBC Signs and Symptoms a. Infection i. Fever ii. Poor wound healing b. Bone weakness and causes fractures c. Signs of bleeding i. Blood in the urine ii. Emesis iii. Petechiae iv. Epistaxis d. Signs of anemia i.Pallor ii. Body malaise iii. constipation e. Invasion of the organs i. Hepatomegaly abdominal pain ii. Spleenomegaly 2. Diagnostic examinations a. Peripheral Blood Smear reveals immature WBC b. CBC reveals anemia and thrombocytopenia; neutropenia c. Lumbar Puncture i. To determine CNS involvement ii. Fetal position without flexion of the neck because it will cause airway obstruction iii. C position or shrimp position d. Bone Marrow Aspiration i. Determines the presence of blast cells ii. Site of bone marrow aspiration iliac Crest post op : prevent hemorrhage iii. Lie on affected site e. Bone Scan determines the degree of bone involvement f. CT Scan determine the degree of organ involvement 3. Management Triad a. Surgery b. Irradiation c. Chemotherapy d. Bone marrow transplant 4. 4 Levels of Chemotherapy a. Induction i. To achieve remission ii. Drugs IV – Vincristine L – Asparagine Oral Prednisone b. Sanctuary i. To treat the leukemic cells that has invaded the testes and CNS ii. Drugs intrathecal methotrexate – via spine Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing cytocine arabinase steroids irradiation c. Maintainance i. To continue remission ii. Drugs oral methotrexate oral 6-mecaptopurine cytarabine d. Reinduction i. Give anti-gout agent To ii. To treat leukemic cells after relapse occurse iii. Treat hyperurecemic neuropathy Alopurinol or zylo[rene 5. Nursing Management a. Assess for common side effects of chemotherapy – nausea and vomiting b. Assess for stomatitis ulceration and abcess of oral mucosa i. Oral care ii. Alcohol free mouthwash iii. Cotton piedgets c. Diet – give food acoording to child’s preference d. Alopecia – temporary side effect of chemotherapy HEMOLYTIC DISORDERS Rh Incompatibility Rh = monkey foreign body Mother (-) – no antigen; no protein factor Fetus (+), Father (+) – has antigen and protein factor 4th baby is severely affected Erythroblastocis Fetalis o hemolysis/ destruction of RBC leading to ↓ O2 carrying capacity leading to IUGR with pathologic jaundice w/in 24 hours ALERT! Baby is small and yellowish Management o RHOGAM Vaccine given to Rh(-) mothers within the first 24 hours or within 72 hours Given once If pregnancy was aborted and the mother udergo D & C, RHOGAM must be given w/in 24 hours, if not given within 24 hours, mother will produce antibody Action: destroys RBC preventing antibody formation Diagnostic Test Coomb’s Test ABO Incompatibility Mother – Type O; Fetus – Type A most common Mother – Type O; Fetus – Type B most severe Hydrops Fetalis Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Common in abo incompatibility o Newborn is edematous, on lethal state, accompanied by pathologic jaundice w/in 24 hours Difference from Rh Incompatibility o First pregnancy is affected o NB is yellow and edematous Management o Initiation of breastfeeding, then temporary suspension of breastfeeding after 4 days ( breastfeeding realeses prenanediole causing kernicterus) o Pregnanediole delays actions of Glucoonyl transferase ( liver enzyme that converts indirect bilirubin into direct bilirubin) Indirect bilirubin Fat soluble Can’t be excreted by kidneys Causes hyperbilirubenemia causing jaundice Direct Bilirubin Water soluble Can be excreted by the kidneys o Use phototherapy o Exchange transfusion for Rh and ABO affectations that tend to casue a continuous decrease in hemoglobin during the first 6 months because the bone marrow fails to produce erythrocytes in reponse to the continuous hemolysis Hyperbilirubenemia More than 12mg of indirect bilirubin among full terms Normal Indirect Bilirubin Level: 0 – 3 mg/dl Kernicterus/ Bilirubin Encephalopathy Irreversible brain damage > 20 mg/dl of indirect bilirubin among full terms > 12 mg/ dl of indirect bilirubin among preterm because of immaturity Physiologic Jaundice Normal Within 48 – 72 hours Mx: Expose to early morning sunlight Pathologic Jaundice Within 24 hours Yellow upon birth Breastfeeding Jaundice Within 6th – 7th day Due to glucoronyl transferase Possible Rh/ ABO incompatibility Assessment of Jaundice blanching of forehead, nose and sternum yellow skin, sclera light stool dark urine Management Phototherapy/ Photooxygenation o Nursing Responsibilities Cover the eyes – prevents retinal damage Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Height of light from baby – 18 – 20 inches Increase Fluid intake Cover genetalia – prevent priapism ( painful continuous erection Change position Avoid lotion and oils Monitor I&O – best way is to weigh the baby Monitor VS Bronze Baby Syndrome Transient bronze discoloration of the skin Minor side effect of phototherapy HEAD ¼ of its legth Structures o sutures o fontanels anterior/ bregma – 3 x 4 – 12 – 18 mos posterior/ lambda - 1 x 1 – 2 – 3 mos Noticeable structures of the Head o Craniotabes Localized softening of the cranial bone common to first bone chiold due to early lightening If present in older children; sign of rickets or Vit. D deficiency o Seborrheic dermatitis/ Cradle Cap Scaling, greasing, appearing salmon – colored patches Usually seen at the scalp, behind ears and umbilicus Usually caused by improper hygiene Management Application of baby oil the night before shampooing the child o Caput Succedaneum Edema of the scalp due to prolonged pressure at birth Present at birth Crosses the suture line Disappears 2 – 3 days Disappears without treatment o Cephalhematoma Collection of blood due to rupture of capillaries of poriosteal capillaries Present after 24 hours Does not cross the suture line Disappears after 4 – 6 weeks Disappears without treatment o Hydrocephalus Excessive accumulation of CSF Types Communicating/ extraventricula hydrocephalus No-communication/ intraventricular hydrocephalus/ obstructive hydrocephalus – caused by tumor Signs and symproms Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Signs of increased ICP o Diplopia – eye deviation @ 6th mos and above o Management Low semi – fowlers (30 degrees) best position Frontal bossing 9 prominent forehead) Sunset eyes Prominent scalp vein Therapeutic management Osmotic Diuretic o Mannitol o Diamox / acetazolamide Seizure precautions Surgery – Shunting o AV Shunt - atrioventricular o VP shunt – ventriculoperitonial – most common Best time to shave the head – just before the surgery – prevent infection Post VP Shunt management Position – sidelying on non-operated side ( applicable to all eyes and head surgeries) Sign of good shunting – sunken fontanel Sign of blocked shunting – bulging fontanel Catheter is changed as the child is growing Child with BP shunt is prone to infection SENSES Sense of Sight Sclera o Normal – light blue o Later Color – dirty white Pupils o Normal – round and adult size o Coloboma – key hole pupils part of the iris is missing o Congenital N Cataract – whiteness/ opacity of the lens Cornea o Normal – round and adult size o Congenital Glaucoma – larger than normal Test for Blindness Age Newborn Can see @ a distance of 10 – 12 inches with visual acuity of 20/200 to 20/ 800 Infant and children Common Test General appearance Check ability to follow object pass midline DOLL’S EYE TEST – done at approximately 10th day GLADELLAR TEST – test for blink reflex, not blinking is a sign of blindness ALLEN’S CARD – test for visual acuity - familiar pictures are flashed 20 ft away from the child Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. 3 years old School age School age – adult Pediatric Nursing ISHIARA PLATE – test for color blindness Cover testing test – for strabismus Snellen’s test RETINOBLASTOMA malignant tumor of the eye signs and symptoms o cat’s eye reflex (whitish glow of pupil) o red, painful eye usually accompanied by glaucoma Management o Surgery innucleation - removal of the eyeball o Irradiation o Therapy SENSE OF SMELL Normal nasal membrane - pinkish Check for sense of smell Check for nasal flaring Sign of Cocaine User Ulceration and abscess of nasal mucosa Absence of hair Epistaxis Nose bleeding Management o Position, upright, sitting, head trilted, slightly forward o Gentle pressure o Cold compress o Epinephrine – last resort SENSE OF HEARING Normal should be aligned with the outer canthus of the eye Low Set Ears is a sign of o Kidney malformation Renal agenesis Absence of kidney o Chromosomal Abnormalities Due to advance maternal age - >35y/o Types o Nondisjunction (uneven divison) Trisomy 21 Down Syndrome Most common type Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Extra chromosome 21 47xx + 21/ 47xy + 21 can be related to advance paternal age signs and symptoms o broad nose o protruding tongue o low- set ears o puppy’s neck o hypotonia prone to URTI o simian crease single traverse line in palm o mental retardation – ranging from educable to institutionalization Trisomy 18 Has 3 numbers of 18 chromosomes Severely cognitively impaire SGA Low set ears, small jaw, CHD, index finger crosses over the other fingers, rounded soles of feet Trisomy 13 Patau’s syndrome Extra chromosome 13 Severely cognitively impaired Signs and symptoms o Microcephaly o Micropthalmia o Cleft-lip and palate o Low-set ears o VSD o Do not survive Turners Gonadal Dysgenesia One functional x chromosome Short in stature Neck appear to be webbed and short COA and kidney problems Only 1 streak (nonfunctional) gonads Secondary sex characteristic does not develop except for pubic hair Lack ovarian function – sterility Cognitively challenged but mostly normal intelligence Klinefelter’s syndrome Males with a XXY chromosome pattern @ puberty child has poorly developed secondary characteristics and small testes that produces ineffective sperm boys tend to develop Gynecomastia o Deletion Abnormalities Cri – du – chat Syndrome Result of a short arm on chromosome 5 Cat’s cry Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Small head, wide set eyes, downward slant to the palbepral fissure of the eyes Severe cognitive impairment Fragile X Syndrome X linked pattern One arm of x chromosome is weakened Most common cause of cognitive impairment in boys Before puberty, boys typically have maladaptive behavior like hyperactivity and autism Large head, long face with high forehead, prominent lower jaw, large protruding ears o Translocation abnormalities Balance translocation Carrier Unbalanced Translocation Syndrome o Others Mosaicism A situation wherein the nondisjunction of chromosome occurs during mitotic cell division after fertilization resulting to different cells contains different numbers of chromosome Isochromosomes A situation wherein the chromosome instead of dividing vertically it divides horizontally resulting to chromosomal mismatch Otitis Media Inflammation of the middle ear Common to children due to wider and shorter Eustachian tube Predisposing factors o Bottle propping o Cleft lip/ palate Signs and symptoms o During otoscopic exam, reveals bulging tympanic membrane o Observe for passage of purulent, foul – smeeling odor discharge Management o Positioning – sidelying on the affected side o Supportive care Medical management o Massive dosage of antibiotics o Mucolytics o Ear drops < 3 y/o – down and back >3 y/o – up and back o Surgery Myringectomy – slight incision of tympanic membrane to prevent hearing loss Side effect – bacterial meningitis MOUTH AND TONGUE Check for symmetry Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Bell’s palsy/ Facial Nerve Paralysis 7th CN injury usually related to forceps delivery risk for URTI Signs and symptoms o Continuous drooling of saliva o Inability to open one eye and close the other Management o Artificial tear o Self limiting o Refer to PT for rehabilitation TEF/ TEA No connection between esophagus and stomach There is a blind pouch Hydramnios – earliest sign intrauterine Signs and symptoms o Coughing o Chocking o Cyanosis o Continuous drooling Management o Emergency surgery Epstein Pearls White glistening cyst Usually seen on palate, gum Related to hypercalcemia Natal Tooth Tooth at the moment of birth Related to hypervitaminosis Management o Manual extraction if rootless Neonatal Tooth Appearance of tooth within 28 days of life Oral Thrush White cheese-like, curd like patches Usually seen in mouth and on toingue Causative agent C. Albicans – fungi Management o Do not remove – can cause wound o Wash with cold, bottled water o Medical – Mycostatin/ Nystatin Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Kawasaki Disease Discovered in Korea Strawberry tongue Common in asian countries Criteria for diagnosis o Fever lasting for more than 5 days o Bilateral conjunctivitis o Changes in lips and oral cavity Dry red fissure lips Strawberry tongue Diffuse erythema of mucos membrane o Changes in the peripheral extremities Erythema on the palms and soles Erythema on the hands and feet Membranous desquamation from fingertips o Polymorphous rash (primarily at trunk) o Acute non purulent sweeling of the cervical lymph nodes to > 1.5 cm in diameter Drug of Choice : ASPIRIN Cleft Lip Failure of the median maxillary nasal process to fuse Common to boys Surgery – cheiloplasty o Done w/in 1 – 3 months o To save sucking reflex Signs and symptoms o Evident at birth o Milk from nostrils spills o Cold is common o Frequent URTI and otitis media Post cheilo – sidelying Nutrition – use rubber tip syringe Cleft Palate Failure of the palate to fuse Common to girls Surgery – Uranoplasty o Done w/in 4 – 6 months o To save speech Signs and symptoms o Evident at birth o Milk from nostrils spills o Cold is common o Frequent URTI and otitis media Post cheilo – prone Nutrition – use paper cup/ plastic cup/ soup spoon Condition to consider for suspension of operation Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing If child has a cold/ nasopharyngitis – may lead to general septicemia General management Maintainance of patent airway Proper nutrition o NPO 4 hours post op o Clear liquid Popsicle except red and brown in color Flavore gelatin No ice cream Observe for bleeding o Frequent swallowing Protect suture lines specially LOGAN BAR o Clean using hydrogen peroxide, bubbles traps microorganism, more bubbles more microorganism trapped o Prevent crying by attending to needs Therapeutic Management Emotional support Proper Nutrition Cleft lip nipple (long tip, made by silicon) Prevent Colic o Burp frequently o One at the middle of the feeding o Another at the end of the feeding o Upright sitting position o Pat at the back – lower to upper o Prone position o Right – sidelying position – facilitates gastric emptying Educate parents Apply elbow restraints so the baby can easily adjust post –op NECK Check for symmetry Congenital Torticollis/ Wry neck Birth injury of sternocleidomastoid due to excessive traction during cephalic delivery A case of incompetence to the one giving birth Management o Passive stretching o Exercise daily o Surgery Complication o Scoliosis Congenital Critinism/ Congenital Hypothyroidism Absence or non – functioning thyroid gland Causes o Due to delayed diagnosis, thyroid is covered by sternocleidomastoid muscle Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Hypothyroidism o Thyroid dysgenesis (absence of thyroid) o Baby receive maternal thyroxine Earliest Signs and Symptoms o Change in sucking o Change in crying o Excessive sleeping (16-20 hours/ day) o Constipation o Edema – moon faced baby o Mental retardation – late sign Diagnostic Test o Radioimmunoassay Test o Protein bounbd iodine Treatment o Synthroid / sodium levothyroxine for life CHEST Witch Milk Transparent Liquid coming out from newborns breast related to hormonal changes ABDOMEN Abdominal Assessment Inspection Ausculation Percussion Palpation Diaphragmatic Hernia Protrusion of stomach contents through a defect in diaphragm due to failure of pleuroperitoneal canal to close Signs and Symptoms o Sunken abdomen o Signs of RDS o Right to left Shunting Treatment – diaphragmatic repair w/in 24 hours Omphalocele Protrusion of stomach content between the the junction of abdominal wall and umbilicus If small – surgery If large – suspend surgery Apply wet dressing GASTROINTESTINAL SYSTEM Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Functions o Assist in maintaining fluid and electrolytes and acid and base balance o Processes and absorbs nutrients to maintain and support growth and development o Excrete wasted products from the digestive process Supplementary Feeding Begin 4 – 6 months As early as 4 months Usually at 6 months Principles o Solid food are often according to the following sequence Cereals rich in iron Fruits Vegetables Meat o Begin with small quantities o Finger food are offered @ 6 months o Soft table food is offered @ 1 year o Diluted citrus/ fruit juices @ 6 months o Offer new food one at a time with an interval of 4 – 7 days or 1 week o Never offer half cooked egg may lead to gastroenteritis/ salmoneliosis Major Concepts of Fluid and Electrolyte Balance Distribution of Body Fluids o Fluids are greater in ECF in infant and children o Newborns are candidate for dehydration o Total Body fluid is 65 – 85% of their body weight in infants and children Acid – Base Imbalance Depending upon the following o Chemical buffers o Renal and respiratory system involvement o Dilution of strong acids and bases in blood Imbalance of Acid o Respiratory Acidosis Carbonic acid excess LTB – RDS Hypoventilation – COPD o Respiratory Alkalosis Carbonic acid deficit Hyperventilation Fever, encephalitis o Metabolic Acidosis Base bicarbonate deficit Diarrhea Severe malnutrition and dehydration celiac o Metabolic Alkalosis Base bicarbonate excess due to uncontrolled vomiting Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing NGT aspiration Gastric lavage Pyloric stenosis Conditions that Produce Fluids and Electrolyte Imbalance Vomiting Forceful expulsion of stomach content Signs and symptoms o Nausea o Abdominal crumping o Flushing of face o Watery eyes Assessment o Frequency o Forces Projectile – increase ICP/ Pyloric stenosis Non – projectile Alerts o Vomiting is an initial symptom of GI Obstruction o Vomitus of upper GI can be blood tinged but bot bile streaked o Vomitus of lower GI is bilous o Projectile vomiting is ewither a sign of increased ICP or GI Obstruction o Abdominal distention is the major symptom of lower GIT obstruction Management o Banana o Rice cereal o Apple sauce o Toast Diarrhea Exaggerated excretion of intestinal contents Acute diarrhea is associated with the following o Gastroenteritis/ salmonelliasis o Antibiotic use – penicillin, tetracycline o Dietary indigestion Chronic non specific diarrhea o Food intolerance o CHO/ CHON malabsorption o Excessive fluid intake Assessment o Frequemcy o Consistency (best criteria) o Appearance of green colored stool Complications o Mild dehydration – 5% weight loss o Moderate dehydration – 10% weight loss o Severe dehydration – 15% weight loss Signs of dehydration o Tachycardia – earliest sign Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Tachypnea o Hypontension o Increase temp o Sunken fontanel o Sunken eyeball o Poor skin turgor o Absence of tears o Scanty urine o Oliguria – severe dehy=dration o Weight loss o Prolonged capillary refill time Management o NPO o IV infusion o KCl – given by doctors Assess child for ability to void before giving KCl – may lead to hyperkalemnia Normal K Value – 3.5 – 5.5 o Order Na Bicarbonate, administer slowly to prevent cardiac overload Gastric Motility Disorders Hirschprung’s Disease/ Congenital Aganglionic Megacolon Absence of ganglion cells needed for peristalsis Assessment o Neonatal Period Abdominal distention Failure to pass meconium within 24 hours o Early childhood Ribbon like stool Constipation Foul smelling stool Diarrhea Vomitus of fecal materials Diagnostic Procedures o Barium enema – reveals narrowed portion of the bowel o Rectal biopsy – reveals absence of ganglion cells o Abdominal x- ray – reveals dilated loops on intestines o Rectal manometry – reveals failure of intestinal sphincter to relax Therapeutic Management o NGT Feeding NGT Measurement Infant – nose-ears – middle of xiphoid process and umbilicus Adult – nose – ears – xiphoid process o Surgery Temporary colostomy Anastomosis and pull through procedure o Diet Increase CHON Increase Calorie Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing ↓ residue diet – pasta foods no raisin/ prunes Gastroesophageal Reflux presence of stomach content on esophagus Assessment o chronic vomiting o failure to thrive syndrome – organic o esophageal bleeding manifested by melena and hematemesis Complications o esophagitis o aspiration pneumonia o esophageal cancer Diagnostic Procedure o barium esophogram o esophageal manometry – reveals lower esophageal pressure o intraesophageal pH content – reveals pH of distal esophagus Medications o anticholinergics bathanechol/ urecholine ↑ esophageal tone and peristaltic activity Methachlopromide (Reglan) ↓ esophageal pressure by relaxing pyloric and duodenal segments ↑ peristalsis without stimulating secretions H2 Blocker/ histamine Receptor Antagonist ↓ gastric acidity and pepsin secretion Maalox/ Cimetidine (Tagamet)/ Ranitidine (Zantac) Neutralizes gastric acid between feedings Surgery: Nissen Fundoplication Diet o Thickened feeding with rice cereal prevents vomiting o Feed slowly o Burp often every 1 oz o Positioning < 9 mos – infant sit/ infant supine > 9 mos – prone with head on mattres slightly elevated on a 30° angle Obstructive Disorders Pyloric Stenosis hypertrophy of the muscle of pylorus causing narrowing and obstruction Assessment o Projectile vomiting o Failure to gain weight o Metabolic alkalosis o Peristaltic wave visible from left to right across epigastrum o Palpation of olived shaped mass Diagnostic Procedure o ABG Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o Serum Electrolyte - ↑ Na and K, ↓ Cl o Ultrasound o X-ray of upper abdomen with barium swallow Management o Pyloromyotomy/ Fredet – Ramstedt Operation Intussusception Telescoping or invagination of one portion of the bowel into the other Peritonitis – danger of intussusception Emergency for URT – epiglotitis Emergency for GIT – peritonitis Signs and symptoms o Acute paroxysmal abdominal pain o Currant jelly stool caused by inflammation and bleeding o Sausage shaped mass Non congenital Caused by fast eating and positioning Management o Hydrostatic reduction with barium enema o Surgery – Anastomosis Inborn Errors of Digestion Phenylketonuria/ PKU Deficiency of the liver in Phenyalanine Hydroxylase Transferase (PHT) PHT is a liver enzyme that coverts protein into amino acid 9 Essential Amino Acids o Tyrosine / phenylalanine o Histidine o Isoleucine o Leucine o Lysine o Methionine/ cysteine o Threonine o Tryptophan o Valine Tyrosine or Phenylalanine – responsible for the melanin production Signs and Symptoms o Fair complexion o Blond hair o Blue eyes o Infantile eczema o Mousy/ musty odor urine o Seizure – due to Phenyl Pyruvic Acid goes to brain o Mental retardation Guthrie Test o Specimen – Blood o Preparation – Increase Fluid Intake Management o Diet Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing ↓ phenylalanine diet indefinitely Chicken, meat, peanuts, milk, legumes, cheese – contraindicated Lofenalac – special formula Celiac Disease/ Malabsorption Syndrome; Gluten Induced Enteropathy Sensitivity or immunologic response to protein Assessment o Early signs Diarrhea, failure to regain weight following diarrheal episode Constipation Vomiting Abdominal pain Steatorhea o Late signs Behavioral changes: irritability and apathy Muscle wasting and loss of subcutaneous fats o Celiac Crisis Development of infection by a child having a celiac disease Acute vomiting and diarrhea Diagnostic Procedure o Stool analysis o Serum antiglandin and antireticulin antibodies o Sweat test Therapeutic management o Vitamin supplements o Mineral supplements o Steroid Poisoning Common accident in toddlers – poisoning Common accident in infants – falls Principles o Determine the substance taken and assess LOC o Unless poisoning was corrosive, caustic (strong alkali, such as lye) or hydrocarbon, vomiting is the most effective way to remove the poison from the body Strong acid poisoning – give weak acid to neutralize strong acid o Syrup of ipecac – oral antiemetic to cause vomiting after drug overdose or poisoning 15 ml – adolescent, school age and preschool 10 ml – infant o Universal Antidote Activated charcoal Milk of magnesia Burned toast Charcoal absorbs toxic substance o Never administer the charcoal before ipecac because giving charcoal first will absorb the effect of ipecac Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing o o Antidote for acetaminophen poisoning : Acetylcysteine (mucomyst) Kerosine/ Gasoline poisoning: Give mineral oil to coat the intestine and prevent poison absorption Tracheostomy set will be at bed side Lead Poisoning Pencil, paint, crayon Lead ↓ Destruction of RBC Functioning ↓ hyupochromic Microcytic Anemia ↓ Destroys Kidney Function ↓ Accumulation of ammonia ↓ Leading to Encephalitis (Late stage) ↓ Severe mental retardation Assessment o Beginning symptoms of lethargy o Impulsiveness and learning difficulty o As lead ↑, severe encephalopathy with seizure and permanent mental retardation Diagnostic procedure o Blood smear o Abdominal x-ray o Lone bone Management o Chelation – binds with the lead and excreted via kidneys o Ca EDTA/ BAL/ Dimercapro Nephrotoxic ANOGENITAL Female Pseudomenstruation o Slight vaginal bleeding related to hormonal changes Rape/ Child Abuse o If the client came with a laceration and bleeding at the perineum o Report rape within 48 hours o Preschool are proneto rape because of their innocence o CBQ Report rape cases to barangay chairman first or bantay bata Male Cryptochirdism o Undecended testes or empty scrotum or ectopic testes Common in preterm babies Testes is palpable at lower quadrant Surgery: Orchioprexy Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Preop – warm the room and hands Epispadias o Urinary meatus is located at the dorsal or above the glans penis Hypospadias o Urinary meatus is located at the ventral or below the glans penis o Hypospadias is usually accompanied by Chordee ( A fibrous band causing penis to curved downward) o Both are manage by surgery Phimosis o Tight foreskin o This will cause infection o Circumcision as management Hydrocele o Fluid filled scrotum o Flashlight/ transillumination test to determine Varicocele o Enlarged vein opf the epididymis RENAL DISORDERS Renal Disorder Nephrotic Syndrome Causes Acute Glomerul onephritis Autoimmun e Group A beta hemolytic streptyococ cus Infection Assessment Findings Anasarca Massive proteinuria Microscopic or no hematuria ↓ serum CHON ↑ serum lipid Normal or ↓ BP Fatigue Primary pheripheral perioprbital edema Moderate Proteinuria Goss hematuria (smokey urine) ↑ serum K Fatigue HPN Treatment Nursing Care Prednisone Skin Care Weigh the client saily with the same clothing ↑ CHON(Normal Diet) ↓ Na ↑K AntiHPN Hydralazine Apresoline Monitor weight Skin Care Monitor BP and neurologic status ↓K ↑ Fe ↓ Na Complication Hypertensive Encephalopat hy BACK Check for flatness and symmetry of the back Spina Bifida Occulta Failure of the posterior lamina or vertebral to fuse Sampling of the lower back Abnormal tufts of hair Spina Bifida Cystica Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing With Sac Types o Meningocele – protrusion of CSF and Meninges o Myelomeningocele – CSF, Meninges and Spinal cord o Ecephacele cranial meningocele - CSF and meninges Myelomeningocele - brain, CSF , meninges Common Complication o Infection o Rupture of Sac Treatment o Surgery to prevent infection: post op – prone position Scoliosis Lateral curvature of the spine, common in school age because of heavy bags Uneven hemline Tell the child to bend forward, one hip higher than athe other and one shoulder is most prominent Types o Structural o Postural Management o Conserbvative Exercise Avoid obesity o Preventive Milwaukee Braces worn 23 hours a day o Corrective: Surgery EXTREMITIES Count the number of digits Digits Syndactyl – webbing of the digits (foot – ginger –like foot) Polydactyl – extra digits Olidactyl – lacks digits Erb – Duchennse Paralysis/ Brachial Plexus Injury Birth injury of breech delivery Signs o Inabiluity to abduct the arm fronm the shoulder, rotate the arm extremely and supinate the forearm o Assymetrical oor absence of moro reflex Management o Abduct the arm from the shoulder with the elbow flexed Congenital Hip Dislocation Congenital hip dysplacia Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing When the head of the femus is outside the scetabulum 2 types o subluxated – most common o dislocated Signs and Symptoms o Shortening of the affected leg o Assymetrical gluteal fold o Limited movement – earliest sign o + ortolanis sign – abnormal clicking of during abduction o when able to walk the child limps (Trendelenburg sign) – late sign Management – facilitate abduction o Triple the diaper o Carry the baby o Frejka Splint o Pavlik Harness o Hip Spica Cast Talipes Club foot 4 types o Equinos – plantar rotation/ horse foot (most common) o Calcenuous – dorsiflexion/ the heel is held lower than the foot/ the anterior portion of the foot is flexed towards the anterior leg o Varus – foot turns in o Valgus – foot turns out Assessment o Make a habit of straightening the legs and flying it to the midline position Management o Corrective shoes : Dennis Brown Shoes o Spica Cast For immobilization Maintain bone alignment Prevent muscle spasm If there is a blood mark on the cast – mark a pen to determine whether there is a hemorrhage Neurobvascular check Circulation Motion Sensation CRUTCHES Wait is on the palm not the axilla Exercise – squeeze ball Different Crutches and Gait Swing Through Advance both crutches Lift both feet/ swing forward/ land feet in front of crutches Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Advance both crutches Lift both feet/ swing forward/ land feet in front of crutches Swing To Advance both crutches Lift both feet/ swing forward/ land feet next to crutches Advance both crutches Lift both feet/ swing forward/ land feet next to crutches Three point gait Advance left foot and both crutches Advance right foot Advance left foot and both crutches Advance right foot Four Point Gait Advance right crutch Advance left foot Advance left crutch Advance right crutch Two Point Gait Advance left foot and right crutch Advance right foot and left crutch Advance left foot and right crutch Advance right foot and left crutch Other Crutch – Maneuvering Technique To Sit Down Grasp the crutches at the hand pieces for control Bend forward slightly while assuming a sitting position Place the affected leg forward to prevent weight bearing and flexion To Stand Up Move forward to the edge of the chair with the strog leg slightly under the seat Place both crutches in the hand on the side of the affected extremity Push down on the hand piece while raising the body to a standing position To Go Downstairs Walk forward as far as possible to the step Advance the crutches to the lower step. The weaker leg is advanced first and then the stronger leg. In this way, the stronger extremity shares the work of raising and lowering the patient’s body weight with the arms To Go Upstairs Advance the stronger leg first up to the next step Then advance the crutches and the weaker extremity ( strong legs goes up first and comes down last.) Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing A memory device for the patient is “UP WITH THE GOOD, DOWN WITH THE BAD” WALKER A walker provides more support than cane andf crutches The patient is taught to ambulate with a walker as follows o Patient must hold the walker on the hand grips for stability o Lift the walker, placing it in front of you while leaning your body slightly forward o Walk into the walker, supporting your body weight on your hands while advancing the weaker leg, permitting partial weight bearing or non weight bearing leg as prescribed o Balance yourself on your feet o Lift the walker and place it in front of you again and continue the pattern of walking. CANE Used to help patient walk with greater balance and support and to relieve the pressure on the weight bearing joints by redistributing the weight. Quad Cane (four – footed cane) is hold on the hand of affected extremity. METHODS OF TRANSFERRING A PATIENT FROM THE BED TO A WHEELCHAIR Weight bearing transfe4r from bed to chair. The patient stands up, pivots his back is opposite the new seat and sits down. (Left) Non weight bearing transfer from chair to bed. (Right) With legs braced. (Left) Non weight bearing transfer combined method. (Right) Non weight bearing transfer, pull up method. THERAPEUTIC EXERCISE Exercise Description Passive carried out by the therapist or the nurse without assistance from the patient Active Assistance Carried out by the patient with the assistance of the therapist or the nurse Jomar Anthony D. Maxion, BSN, RN Purpose To retain as much joint range of motion as possible To maintain circulation To encourage normal muscle function Action Stabiolize the proximal joinyt, and support the distal part. Move the joint smoothly, slowly and gently through its full rang of motion Avoid producing pain. Support the distal part and encourage the patient to take the joint actively through its ROM. PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Active Accomplished by the patient without assistance, activities include turning from side to side and from back to abdomen and moving up and down in bed To increase muscle strength Resistive An ective exercise carried out by the patient working against the resistance produced by either manual or mechanical means To provide resistance to increase muscle power Isometric/ Muscle Setting Alternately contracting and relaxing a muscle while keeping the part in fixed position; performed by the patient To maintain strength when a joint is immobilized Give no more assistance than is necessary to accomplish the action. Short periods of activity should be followed by adequate rest periods. When possible, active exercise should be performed against gravity. The joint is moved through full ROM without assistance. (make sure that the patient does not substitute another joint movement for the one intended) The patient moves the joint through its ROM while the therapist resist slightly at first and the progressively increasing resistance. Sandbagws and weights can be used and are applied at the distal point of the joint involved. The movement should be performed smoothly. Contract or tighten the muscle as much as possible without moving the joint. Hold for several seconds, and then let go and relax. Breath deeply. TRACTION Use to reduce dislocation Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Principles of Traction The client should be in dorsal or supine position For every traction, there is always a counter traction Line of pull should be in line with deformity For traction to be effective it must be continuous Weight must be freely hanging Types of Traction Straight traction – weight of the body serves as counter pull Skin traction – applied directly to the skin o Bryant’s Traction use to immobilize for < 2 years old at a 90 ° angle with buttocks off the bed o Buck’s extension For > 2 years old Halo traction – immobilize the spine Skeletal traction o Nursing responsibilities Assess for circulatory and neurology impairment It can lead to HPN Be careful to carry out nursing functions by not moving the weights AUTOIMMUNE SYSTEM Types of Immunity o Passive Natural Developed via exposure to a disease o Active Natural Transplacental transfer, IgA from breastmilk o Passive Artificial Vaccination o Active Artificial Anti Rabies Serum NEUROMUSCULAR SYSTEM Reflexes Blink reflex Rapid eye closure when strong light is shown to protect the eyes; never disappears Palmar Grasp Reflex When a solid object is placed on the palm then the baby will grasp the object To cling to the mother for safety Disappears at 3 months Step – in/ Walk – in Place Reflex/ Dance Reflex Neonate placed on a vertical position with their feet touching on hard surface will take a few quick alternating steps Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006 The Royal Pentagon Review Specialist Inc. Pediatric Nursing Placing reflex almost the same with the dance reflex except that is when you are touching the anterior surface of newborns leg Plantar Grasp Reflex When an object touches the sole of the newborn’s foot at the base of his toes, the toes grasp in the same manner as the fingers do Disappears @ 8 – 9 months in preparation for walking Tonic Neck Reflex/ Fencing/ Boxing reflex When the newborn lies on its bact, their heads usually turns to one side, the arm and the leg on the side to which the head turns extend to the opposite arm and legs contract Moro Reflex/ Startle Reflex With a loud voice or by a jarring the base of the crib, the baby will assume a c position Test for neurologic integrity Magnet Reflex When there is pressure at the sole of the foot, the baby pushes back against the pressure Crossed extension Reflex While supine and the sole of the foot is stimulated by a sharp object, it causes the foot to raise and the other foot to extend Test for spinal nerve integrity Trunk Incurvation Reflex/ Galant Reflex While in prone position and the parabvertebral area is stimulated, it causes flexion of the trunk and swing his pelvis towards the touch Landau reflex While the infant is placed on a vertical position with the hand underneath supporting the trunk the baby exhibit some muscle tone Present at 3 months Test for muscle tone Parachute Reflex When the infant is placed on a vertical suspension with the change in equilibrium, it causes the extension of the hands and legs Present at 6 – 9 months Babinski Reflex When the sole of the foot is stimulated by inverted j, it causes fanning of the toes Disappears by 2 months but may persist till 2 years old Jomar Anthony D. Maxion, BSN, RN PLM BSN 2006