Bilateral cleft Lip
advertisement
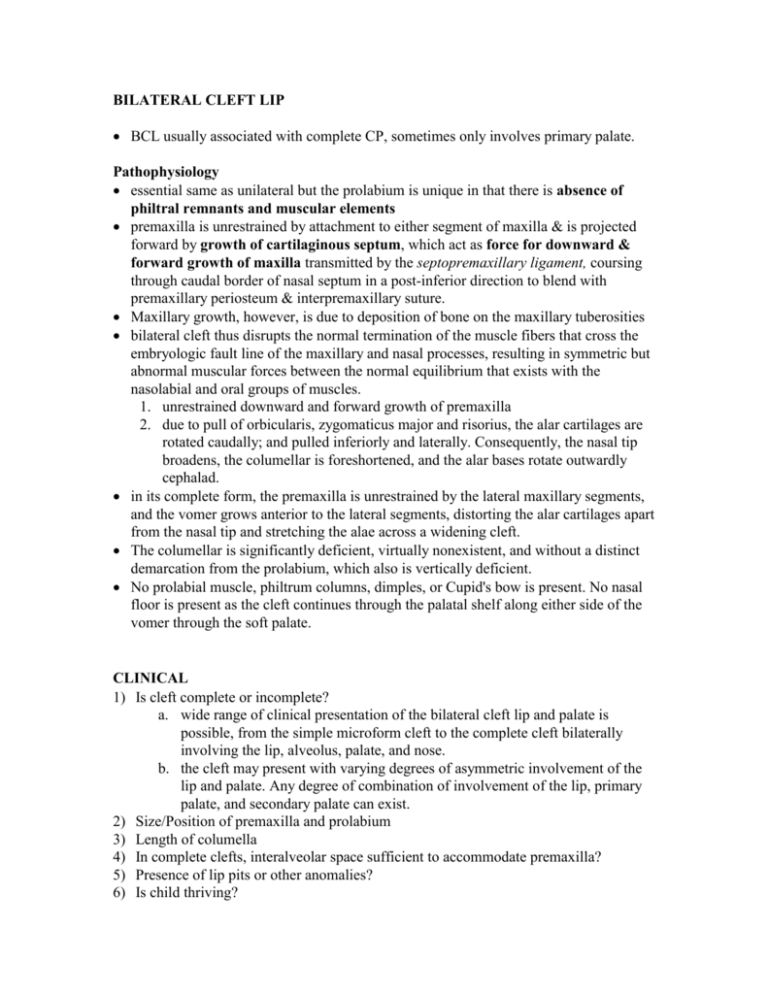
BILATERAL CLEFT LIP BCL usually associated with complete CP, sometimes only involves primary palate. Pathophysiology essential same as unilateral but the prolabium is unique in that there is absence of philtral remnants and muscular elements premaxilla is unrestrained by attachment to either segment of maxilla & is projected forward by growth of cartilaginous septum, which act as force for downward & forward growth of maxilla transmitted by the septopremaxillary ligament, coursing through caudal border of nasal septum in a post-inferior direction to blend with premaxillary periosteum & interpremaxillary suture. Maxillary growth, however, is due to deposition of bone on the maxillary tuberosities bilateral cleft thus disrupts the normal termination of the muscle fibers that cross the embryologic fault line of the maxillary and nasal processes, resulting in symmetric but abnormal muscular forces between the normal equilibrium that exists with the nasolabial and oral groups of muscles. 1. unrestrained downward and forward growth of premaxilla 2. due to pull of orbicularis, zygomaticus major and risorius, the alar cartilages are rotated caudally; and pulled inferiorly and laterally. Consequently, the nasal tip broadens, the columellar is foreshortened, and the alar bases rotate outwardly cephalad. in its complete form, the premaxilla is unrestrained by the lateral maxillary segments, and the vomer grows anterior to the lateral segments, distorting the alar cartilages apart from the nasal tip and stretching the alae across a widening cleft. The columellar is significantly deficient, virtually nonexistent, and without a distinct demarcation from the prolabium, which also is vertically deficient. No prolabial muscle, philtrum columns, dimples, or Cupid's bow is present. No nasal floor is present as the cleft continues through the palatal shelf along either side of the vomer through the soft palate. CLINICAL 1) Is cleft complete or incomplete? a. wide range of clinical presentation of the bilateral cleft lip and palate is possible, from the simple microform cleft to the complete cleft bilaterally involving the lip, alveolus, palate, and nose. b. the cleft may present with varying degrees of asymmetric involvement of the lip and palate. Any degree of combination of involvement of the lip, primary palate, and secondary palate can exist. 2) Size/Position of premaxilla and prolabium 3) Length of columella 4) In complete clefts, interalveolar space sufficient to accommodate premaxilla? 5) Presence of lip pits or other anomalies? 6) Is child thriving? 7) If CP, middle ear disease? Anatomic components Bilateral cleft lip/palate Widened alar bases Laterally flared internal nasal valves Appearance of a shortened columella with malpositioned alar cartilages Excessively obtuse columellalabial angle Vertically short upper lip, particularly centrally at the prolabium Abberent insertion of lateral lip orbicularis oris into alar-facial bases Premaxillary alveolar segment with variable degree of protrusion o Hypoplastic prolabial lip segment o Absence of normal gingival sulcus in premaxillary segment o Absence of orbicularis oris in prolabial segment o Absence of central philtral dimple, columns or philtral tubercle o Absence of cupids bow o Absence of white roll in the prolabial lip segment o Aberrant dry-moist vermillion on prolabial segment The projecting premaxilla paired premaxillary bones joined in midline at interpremaxillary suture (a component of midpalatal suture) each premaxilla articulates posteriorly with prevomerine bone and extends a short distance around it, so that premaxillary vomeral suture forms a tongue-in-groove joint premaxilla may vary in site and size, development & position. It may contain 4 incisors or only 2 moulding effect of intact orbicularis oris mm, ie primary repair is far more effective than lip adhesion except for “diminutive” prolabium where preliminary adhesion stretches prolabium to a more manageable size, creates a philtrum of normal dimension, and excess tissue may be used in columellar reconstruction Control of protruding premaxilla: Options 1) traction by external elastics with head cap 2) lip adhesion - efficient, avoids possibility of a poor definitive repair due to excessive tension 3) Intraoral devices - rarely, if premaxilla 'locked out' of arch in an anterior position one needs to reexpand lateral elements and set premaxilla back at the same time, controlled fixed-pin external traction device (Georgiade, Latham) 4) closure of cleft one side at a time : 2nd side 3 months later. Do wider side first or do narrow side first with lip adhesion of wider side. Difficult due to distortion of prolabium by first operation. 5) surgical setback involves subperiosteal section of the vomer leads to long term midface hypoplasia in patients with bilateral CL/P, a protrusive premaxilla confers an advantage during most of the growth period because the premaxilla grows at a far slower rate than the mandible. 6) Surgical excision – abandoned now Summary of management 1) If the premaxilla is well in the arch, mucoperiosteal flaps can be turned at the time of lip closure to effect fibrous union of the arches. 2) If the premaxilla is projecting, extraoral traction beginning at the time of birth is indicated. In the event of poor response to this form of therapy, the controlled fixedpin external traction device of Georgiade’s may be needed. 3) goal of orthodontics is to achieve retrodisplacement of the premaxilla in line with the maxillary arches, sufficient to allow lip closure with approximation of the lateral muscle segments across the premaxilla. Undercorrection of the premaxilla is certainly acceptable. 4) In rare cases, setback may be necessary 5) In older patients the degree of premaxillary protrusion can justify repositioning with osteotomy. A protrusive premaxilla can be repositioned after age 6 to 8 years without deleterious effect on midfacial growth. Prolabium 1) Complete bilateral cleft lip - Functionally sterile. Contains primarily immature fibroblastic tissue & fine collagen, but no mature muscles 2) Incomplete bilateral cleft lip - has near-normal muscles penetration into prolabium; muscles bundles are cylindrically bunched in remaining lip bridge, then fan out into prolabium Use of Prolabium mistakes of early procedures : 1) excise or assumed prolabium as displaced columella > lip grossly deficient horizontally excision of premaxilla invariably results in a tight lip, dish-face deformity of mid-third of fac and relative mandibular prognathia 2) deceived by deficient appearance & used flaps from lateral lip segment to supplement vertical height > lip too long & too narrow with prolabial skin trapped in the centre pin-cushioned - fail to recognise potential of prolabium to grow in width and height when attached to dynamic lateral lip elements Applications 1. provide full vertical dimension of central lip 2. lateral prolabial parings can be used for future columellar lengthening 3. an advantage to establish an oral sphincter that is in-continuity early in repair sequence, by direct suture of lateral muscle elements behind prolabium 4. modified Manchester - if white roll & vermilion of prolabium of good quality, the lateral prolabial parings may be banked for future columellar lengthening, & orbicularis oris muscle should be reconstituted behind prolabium 5. Millard - if white roll & vermilion of prolabium of poor quality, borrow these parts from lat lip TREATMENT Objectives 1. complete correction of lip & nasal deformity 2. control of relationship of premaxilla & maxillary segments 3. closure, or provision for closure, of anterior palate & subsequently posterior palate Principles. 1) prolabium is to form full vertical length of lip 2) prolabial vermilion turned down for lining 3) central vermilion built from vermilion/muscle flaps from lateral lip segments 4) vermilion ridge from lateral lip segment 5) no lateral lip skin below prolabium 6) reposition severely protruding premaxilla, surgically or nonsurgically, permits earlier & better repair of lip by relieving undue tension & also makes 1 stage repair possible 7) collapse of maxillary processes behind protruding premaxilla requires prevention or expansion with maxillary orthopaedics 8) bone grafting - secondary Anterior palate may be repaired with lip surgery or after it. If after, should be performed before premaxilla & maxillary segments become opposed by action of repaired lip Timing of repair In general, most centers prefer to perform the lip reconstruction when the patient is aged 2-4 months; anesthesia risks are lower, the child is better able to withstand the stress of surgery, and lip elements are larger and allow for a meticulous reconstruction. At PMH o Presurgical orthopaedics at birth presurgical, fabricated, passive, intraoral orthodontic palatal appliance to maintain the arch width to prevent the nearly inevitable collapse that occurs with lip repair. appliance also assists in the child's oral feeding, helping to decrease nasal regurgitation and assisting oral suction. external pressure with soft elastic tape to help maintain the premaxillary component within the arch alignment. Techniques of repair 1. straight line closures - Veau, Manchester 2. Z-plasty lower - Berkeley, Bauer upper - Millard, Wynn both – Skoog International trends 75% perform rotation-advancement flaps and 75% perform lip repair at 3-6 months 9* Veau III (Straight line closure) straight-line closure without elevation of the prolabial skin no attempt at restoring the continuity of the orbicularis oris. The central cupid's bow and tubercle is constructed from the vermilion of the lateral lip elements. prolabium reduced to width of 1cm central lip skin for lip repair and columella lengthening if wide alveolar cleft closed If prolabium is wide, fork flaps can be developed and banked in the nasal floor Essentially technique brings lateral lip into, but not beneath (ie muscle), the prolabium Manchester Single stage lip and palate repair. Emphasise the construction of a tubercle by deepithelised prolabial wings. keeps prolabial white roll and vermilion discards lateral prolabial paring does not involve repairing the orbicularis as he felt this would create an overly tight lip and maxillary retursion - long term results of extensive mm closure (Mulliken, Millard) have yet to be evaluated . Problems 1) 2) 3) 4) Creates a broad philtrum inadequately addresses the sulcus. No provision for columella lengthening using prolabial vermilion in an exposed position where there is a colour difference compared with that of the lateral segments. Occasionally, the white roll and vermilion of the prolabium are of good quality, Post op Care Steristrips - not used at PMH Logan's bow (wire arch taped across cheek to take tension off lip repair) – not used at PMH Arms splints Liquids for three weeks (Mr Baker uses spoon feed for 3 weeks, Mr Gillet allows squeeze bottle) Millard/Mulliken Repair involved complete elevation of the prolabium and reconstitution of the orbicularis across the premaxilla. lateral segments of the prolabium - "forked flaps" are banked to add columellar height at a later stage. As with Veau, the central vermilion is recreated from the lateral lip elements. lateral segments closure design like rotation advancement repair in unilateral case=brings in new white roll from lateral lip elements prolabial vermilion is advanced toward sulcus to form a tubercle, & prolabial parings are banked for future columellar lengthening best = Millard & modified Manchester (Broadbent & Woolf) both have a reduction of prolabium to a smaller philtral dimension at time of closure Excessively long lip may result from collapse of maxillary segments behind premaxilla Lengthening the columella Usage of banked forked flaps. 3 unfavourable long term features with adolescent growth spurt (McComb) 1. columella may grow too long & nostrils too large 2. nasal tip often remains too broad 3. columellar base tends to drift & a scar courses through lip-columellar angle Mulliken concluded - columella is concealed in the nose of an infant with bilateral complete cleft lip. There is no deficiency of columellar skin and no need to recruit tissue from the lip or sills. McComb's experience led him to stage the repair. The initial stage involves approximating and repositioning the splayed alar cartilages through a V-Y nasal tip "gull-wing" incision that allows redraping the overlying skin with a simultaneous bilateral lip adhesion. A definitive lip repair follows at a second stage. Two-stage repair (McComb 1990) 1st step in primary reconstruction of bilateral CLN is the use of preop orthopedics to narrow soft-tissue clefts & realign the bony platform nasal tip dissection does jeopardise blood supply to prolabium, therefore 2 stages prolabium left attached to premaxilla while nose is repaired at 1st stage : Stage 1 (3 weeks) VY gull wing incision enables 1) medial alar cartilage mobilisation and suturing, 2) columella reconstruction 3) alar width reduction tension is taken out of nasal tip by repairing nostril floor & creating long lip adhesions columella is reconstructed from tissues within nasal tip skin flaps are sutured together to reconstitute a columella that is 5mm in length Stage 2 At 3 months, prolabium is lifted away from premaxilla & mucomuscular flaps advanced to complete lip repair Disadvantage of gullwing is the scar which may complicate placement of scar for future rhinoplasties Primary correction of cleft nasal deformity 88% of units reposition the lower laterals at the time of lip repair McComb, Salyer correction of nasal deformity at time of lip repair endures, does not disturb growth, & is beneficial to nasal morphology mobilise lower lateral cartilage from overlying nasal skin, simultaneously releasing it on cleft side from piriform aperture & involving medial crus in septal area, creating a flap of lining mucosa & cartilage, with lateral portion of lower lateral cartilage advanced medially & cephalad, & medial crus advanced toward the tip. Suture-fixation +/or bolster suturing to hold the cartilage in position Other 1. Tajima repair : reverse-U incision along alar margin with a back-cut along vestibular lining at junction of piriform aperture to release plica vestibularis 2. Non-surgical moulding in early neonatal periods (Matsuo et al) 3. Post-surgical splinting for 3-4mths (Nakajima) COMPLICATIONS Complications 1. Wound infection 2. wound dehiscence a. most likely due to wound tension 3. Premaxillary malposition a. Tilting or retrusion – important to prevent excessive tension b. Prevent with use of splints 4. whistle deformity a. refers to vermillion deficiency b. prevented by using lateral muscle vermilion flaps to augment thickness of prolabium 5. Lip length asymmetry a. Inaccurate measurements b. Lack of tissue approximation 6. Lateral maxillary segment collapse medially and posterior to the premaxilla 7. Scarring