Biology and Physiology of Aging Definition of Aging A normal
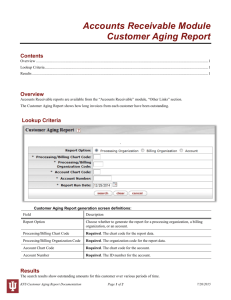
advertisement

Biology and Physiology of Aging Definition of Aging A normal process of adult life during which there are structural and functional changes that lead to a decline in the physiologic reserves of the body. With aging the body is capable of functioning normally under basal (resting) conditions; however, when stressed, organs and tissues have a reduced ability to make homeostatic adjustments and recover from injury. The concept of aging also generally includes an accompanying increased vulnerability to age-related diseases and reduced activity levels. Biology of Aging 1. Cellular Aging - Like all biologic processes, aging must ultimately be explained at the cellular level. Experiments have repeatedly demonstrated that animal cells in culture will initially proliferate vigorously, but after a period of time, cell division eventually ceases and the cells enter a quiescent stage. There appears to be a finite number of cell divisions - roughly equal to the life span of the species - after which cells will no longer divide. Human cells derived from the tissues of newborns are capable of approximately 50 population doublings. Other changes associated with cellular aging include atrophy, decreased metabolic activity, and impaired DNA repair mechanisms. Lack of DNA repair makes the cell particularly vulnerable to mutations that may induce neoplasia or trigger apoptosis (programmed cell death). 2. Theories of Aging - The underlying cause for aging is poorly understood. Nevertheless, a number of laboratory observations have provided insights into some possible cellular and biochemical mechanisms. The most important of these include: 1. Cell Damage Theories - It has been suggested that aging is the result of a gradual accumulation of cellular damage leading to harmful alterations in organ and system functions. One likely source of age-related cellular injuries is the family of highly reactive molecules known as oxygen derived free radicals (superoxide, hydrogen peroxide, and hydroxyl free radicals). Life-long exposure to free radicals may degrade cellular lipids, proteins, DNA, and mitochondria and eventually compromise vital biochemical functions within the cell. Another mechanism for cell injury appears to be the attachment of glucose molecules to cellular proteins (glycosylation) which is seen with increasing frequency in aging cells. Intramolecular cross-linking of protein molecules by glycosylation adversely affects many biochemical systems within the cell - especially biosynthesis and energy generation. Excess accumulation of glycosylated proteins in tissues seems to initiate chronic inflammatory reactions capable of producing degenerative changes in organs. 2. Program Theories - Many have suggested that the life span of animals is genetically programmed much like embryogenesis, cell division, and cellular differentiation. It has already been demonstrated that apoptosis results from the activation and/or shutting down of certain genes in response to DNA injury. The possibility that telomeres (the non-gene DNA found on the ends of chromosomes) may serve as a biological clock controlling aging is being investigated. Telomeres are important for chromosomal replication, and seem to protect vital genetic DNA from degradation. As cells divide telomeres gradually become shorter until a critical point is reached and the cell can no longer replicate its DNA. Another possible way aging could be genetically programmed is by withdrawing neuroendocrine stimulation to cells in the later stages of life. None of these theories explain the process of aging satisfactorily. Many of the observations upon which these theories are founded are difficult to resolve into cause and effect. (Does free radical formation and protein glycosylation cause aging, or are they simply bi-products of another more fundamental process?) Most cellular theories of aging also fail to factor in influences such as nutrition, exposure to environmental toxins, disease, injury, etc. In all likelihood aging is a multifactorial process involving genetically programmed events, accumulated cellular injury, as well as random environmental insults. Premature Aging A small number of genetic conditions are associated with premature physiologic aging. The best known of these is the Hutchinson-Gilford Progeria Syndrome (HGPS) - an extremely rare condition with less than 100 cases reported in the world. Affected children appear normal at birth, but within the first year of life, clinical features of the disorder usually develop. These include short stature and low weight, alopecia, muscle and skin atrophy, and abnormal facies. Children with HGPS have a "wizened old man" appearance with underdeveloped jaw, prominent eyes, and a beak-like nose. Mental development is normal. Joint and skeletal abnormalities may occur. The cardiovascular system rapidly degenerates leading to premature atherosclerotic disease which is the usual cause of death sometime during the second decade of life. The etiology of HGPS is unknown. There is currently no treatment available. Interestingly, cells from progeria patients have a greatly reduced ability to divide (about 10 doublings instead of the normal 50). Some researchers have also demonstrated lower than normal levels of antioxidant activity in HGPS cells. Physiologic Changes with Aging As noted above, aging is associated with a decline in physiologic reserves and a reduced capacity for maintaining base-line homeostasis in response to external stresses. The functional consequences of aging are independent of disease - they occur even in healthy elderly individuals free of detectable disease. The physiologic changes of aging normally become important only when a system is stressed or when there is concurrent illness. Some commonly observed organ specific changes in aging include the following: 1. Cardiovascular System - The ability of the heart to increase maximum heart rate and cardiac output during exercise declines with age. This may be due to decreased responsiveness of the heart to sympathetic stimulation. Otherwise, basic cardiac function remains fairly normal in the absence of disease. The compliance and elasticity of the myocardium and arteries decreases - i.e., they become stiffer. This may explain the frequently observed rise in systolic blood pressure during old age. 2. Pulmonary System - Decreased elasticity of pulmonary tissue, and a slight reduction in total alveolar surface area and gas exchange. It is not unusual to see a slight reduction in vital capacity and FEV. However, in the absence of disease, this rarely produces symptoms. Ciliary activity and mucous secretion by bronchial epithelium is reduced. 3. Gastrointestinal System and Liver - Slight reduction in salivary secretion and gastric acid secretion. The small intestine usually demonstrates some impaired motility in response to a bolus of food. Absorption of nutrients is slightly decreased; however, this is not likely to cause problems if the diet is adequate. Atrophic changes are observed in the mucosa of the colon. A slowing of colonic peristalsis and longer transit times may explain the increased incidence of constipation in the elderly. The numbers of hepatocytes decrease and blood flow to the liver also decreases. These changes usually do not have a significant impact on routine liver function tests (bilirubin, AST, ALT, alkaline phosphatase). However, cytochrome P450 activity by hepatocytes is often diminished in the elderly and this may reduce the ability of the liver to metabolize some drugs. 4. Urinary System - Renal blood flow decreases and there is a steady reduction in the number of glomeruli. As a result, GFR declines by approximately 1% per year after the age of 40. This adversely impacts the renal clearance of drugs in the elderly. Total body water decreases with age. This, along with decreased cardiac reserve, places the elderly at risk for fluid overload with too vigorous I.V. fluid therapy. The ability to concentrate urine is decreased and bladder capacity diminishes. This probably contributes to the frequent need of many elderly to rise at night to urinate, or to occasional urinary incontinence. Men often experience prostatic enlargement with accompanying symptoms of bladder outlet obstruction (nocturia, urinary hesitancy, and decreased urine stream). 5. Nervous System - Brain weight decreases as does cerebral blood flow. There is a modest loss of neurons and decreases in many neurotransmitters. The functional impact of these changes are not well understood. Mental fatigue and "forgetfulness" are common complaints of the elderly. While it is very difficult to distinguish these changes from early dementia, it has been pointed out that if an elderly patient complains about memory loss it is probably a symptom or normal aging since patient's with Alzheimer's disease are often unaware of their cognitive impairments. Proprioception and muscle stretch reflexes are diminished in the elderly (risk of falling). There is a reduced responsiveness to autonomic reflexes - including decreased cardiovascular reflexes that can cause postural hypotension (again, risk of falling). Special senses such as vision, hearing, taste, and smell are also impaired in the elderly. Finally, up to 90% of the elderly experience problems with sleep. Physiologic sleep patterns are altered causing a reduction in the requirement for total sleep, and a decrease in deep (Stage IV) sleep. REM sleep is unchanged. The elderly take longer to fall asleep and often wake earlier. Older adults do not tolerate sleep deprivation as well as younger individuals. 6. Endocrine System - Blood levels of insulin increase with age (probably due to decreased responsiveness of peripheral tissues to this hormone). This often results in a slight rise in mean blood glucose levels. Estrogen levels decline in women leading to the physiologic changes of menopause. This is accompanied by an increase in pituitary gonadotropins (FSH and LH). Men experience a decline in testosterone levels - although this rarely produces symptoms. Aging is also associated with a decline in other hormones such as growth hormone, tri-iodothyronine (T3), renin, aldosterone, and possibly cortisol. Impairment of temperature regulation and decreased heat production occurs with aging (increased risk for hypothermia). 7. Hematologic and Immune Systems - In the absence of disease, the total numbers and life span of RBC's, WBC's, and platelets are essentially unchanged with aging. (There is a slight decrease in hematocrit in older men due to lower testosterone levels, but women experience a slight increase in hematocrit after menopause.) However, the ability of the bone marrow to increase WBC's in response to infection, or to generate new RBC's after bleeding, is slower. Because temperature regulation is impaired in the elderly, they are less likely to develop fever with infection compared to younger individuals. The ability of B and T lymphocytes to respond to antigenic challenge is diminished in old age. 8. Musculoskeletal System - There is a steady decline in skeletal muscle mass (sarcopenia) and a reduction in muscle strength. This muscle wasting is frequently visble in the temporal regions of the head. The cause for this loss of muscle is unclear. Age-related changes in the nervous, vascular, and endocrine systems probably play some role. However, since it has been observed that heart and diaphragmatic muscle mass do not appear to decrease with age, it has been argued that decreased activity and deconditioning in the elderly may be a contributing factor. One of the most important musculoskeletal changes that occur with aging is a decrease in bone density (osteoporosis) with its attendent risk for fractures and degenerative joint disease. The rate of bone loss is more rapid in women than men (especially during the first five years following menopause). Fracture healing is often delayed because bone remodeling and mineralization is slowed. 9. Skin - The thickness of the dermis decreases and there is a loss of elasticity in the skin. Subcutaneous fat and the numbers of cutaneous blood vessels decrease. Sweat production by eccrine glands is reduced. All of these factors alter the appearance of the skin making it thinner, smoother, drier, and wrinkled. These changes also affect the barrier and protective functions of the skin increasing the risk for infection and hypothermia. Impact of Aging on Disease Presentation The physiologic changes associated with aging also affect the way many elderly present with illness. Compared to younger individuals, the elderly are more likely to present with non-specific symptoms, delayed symptoms, or a paucity of "typical" signs and symptoms. Many acute diseases (especially infections) may have a lack of localizing signs and symptoms, and instead, present with altered mental status, or signs and symptoms of congestive heart failure. Some commonly recognized altered disease presentations in the elderly include: Depression - Major depression may present without the typical dysphoria (sadness). Instead, depressed elderly often have symptoms of mental confusion resembling dementia. Silent Infections - Expected findings such as fever, tachycardia, and leukocytosis may be absent. The acute abdomen (appendicitis, cholecystitis, ischemic bowel disease, etc.) may present with a minimum of pain or tenderness. Heart Disease - It has been estimated that up to one-third of all myocardial infarctions in elderly patients present without chest pain. Instead, vague symptoms of illness, dyspnea, and sudden exercise intolerance may predominate. Congestive heart failure may present with minimal dyspnea or other symptoms - especially if the patient's activity level is decreased. Hyperthyroidism - Thyrotoxicosis in the elderly sometimes present with fatigue, decreased physical activity, depression, or mental confusion instead of the typical signs and symptoms of hypermetabolism and overactivity of the sympathetic nervous system.