Blood grouping
advertisement

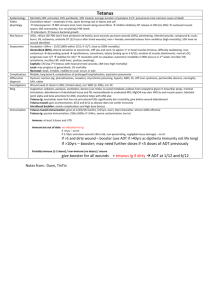
tetanus definition: It is a local infection by anaerobic organism -clostridium tetaniwhich produce their ex otoxins which affect the anterior horn cells. Causative organism: Clostridium tetani which is a gram +ve anaerobic sporeforming organism. The spore is terminal giving the organism a drum stick appearance. It can resist boiling for 40 minutes. Route of infection: 1- Wounds: specially that infected in the street or cultivated lands (contains horse or cattle dungs). 2- Badly sterilized catgut suture material which is extracted from the sheep intestine where the organism is a normal inhabitant (postoperative tetanus). 3- Umblical stump infection: tetanus neonatorum. Predisposing factors: As the organism is anaerobic so the factors which decrease tissue oxygen will favour the growth. - Shock due to tissue anoxia. - Local ischaemia due to injury of the main blood supply to the limb or due to tourniquet. - Deep wounds with foreign body or secondary pyogenic organism that consume oxygen. Pathogenesis: The organisms grow locally in the infected tissues and produce their toxins which will circulate in the blood stream and pass along the nerves to reach the spinal cord and become fixed to the motor cells producing dual action: 1- Interfere with acetyle choline - choline estrase balance at the motor end plates leading to accumulation of acetyle choline leading to tonic muscle spasm. 2- Extreme hyperexitability of anterior horn cell leading to reflex muscle spasm in response to any minor sensory stimulus. Clinical picture: The incubation period is 2-21 days depending on: 1- Previous immunization will prolong I.P. 2- Severity of the wound and infection will shorten I.P. 3- If the injury is near to the spinal cord this will shorten I.P. Local signs: - that of an infected wound (may be healed). - tender muscle - +ve smear. General signs: the patient is at first sleepy, yawing and complaining of headache, sweating and fever then the patient will pass into 2 stages: 1- Stage of tonic contraction resulting in: a- trismus: is the first reliable sign (masseter-temporalis). b- Risus sardonicus: Sarcastic smile due to spasm of the facial muscles. c- Dyspnea. d- Dysphagea due to spasm of the muscles of deglutition. e- neck retraction and stiffness. 2- Stage of convulsions: Occurs after 1-5 days in mild cases. Usually occurs in attacks, either spontaneously or after minor stimuli as light or noise. During the attack the body may take one of the following positions: a- Opisthotonos (occipito-heal position) arched back. b- Eprosthotonos (embryo position) arched forward. c- Pleurosthotonos (arched laterally). d- Orthotonos: all muscles are equally affected. During convulsions, muscles may rupture (e.g. Psoas, Rectus, pectoralis) and asphyxia may occur due to spasm of respiratory muscles. Clinical types: 1- Acute tetanus: with short I.P (bad prognosis). 2- Chronic tetanus: with long I.P (more than 15 days). 3- Local tetanus: affects a group of muscles near the infeted wound (in previously immunized patient). 4- Postoperative tetanus. 5- Cephalo tetanus (facial): affecting facial muscles only. 6- Splanchnic tetanus: affects muscles of deglutition leading to dysphagia. 7- Latent (cryptogenic) tetanus: without an apparent wound. 8- Tetanus neonatorum. Differential diagnosis: 1- Strychnine poisoning: of rapid onset, the muscles are relaxed between the attacks and the hands and forearm are often affected. 2- Hydrophobia (rabies): history of dog bite, laryngeal muscles are firstly affected and convulsion are clonic. 3- Tetany: carpopedal spasm and low calcium level. 4- Meningitis: neck muscle are affected and the cerebrospinal fluid is turbid. Treatment: A- Prophylaxis: - Active immunization with tetanus toxoids: D.P.T at 2-4-6-18 months then at 6 years. 1 ml subcutaneous. - Passive immunization: 1500 IU of antitetanic serum are given intramuscular in wounded patients. - Proper management of wounds. B- Curative treatment (of established cases) 1- antitetanic sera are given to neutralize the circulating toxin. 100000 IU are given intravenous to prevent fixation of toxins once the case is diagnosed then 50000 IU after one week. 2- Antibiotics. 3- Local treatment of wounds: started one hour after the injection of antitetanic serum. The wound should be widely opened and irrigated with hydrogen peroxide and remove any foreign body. 4- Control of spasm and convulsions: - Sedation with barbiturates. - If there is marked dysphagia a nasogastric tube is passed for feeding. - Tracheostomy is done if there is respiratory obstruction. - Convulsion may be controlled by muscle relaxants and ventilator (IPPR-intermittent positive pressure respiration). - Cooling in hyperpyrexia. 5- Care of the patient: In a quite room with care of feeding, bladder, rectum and skin. Prognosis: Depends on the period between the first symptom and reflex spasm. If less than 48 hours death Gas gangrene definition: acute specific infection of wounds which was contaminated by specific anaerobic organisms, which have prediction to grow on lacerated and dead muscles with production of gas and exotoxins that cause severe toxaemia. Causative organisms: There are 2 types which act together a- Saccharolytic group: which breaks down muscle glycogen to give the way for the action of the proteolytic groups. It includes: 1- Clostridium Welchii: which produces toxins causing haemolysis of RBCs and necrosis of the liver and kidney. 2- Clostridium edemeteins: causes extensive gelatinous oedema. 3- Clostridium septicum: causes extensive haemorrhagic oedema. b- Proteolytic group: acts on the proteins of dead muscles producting gases. It includes: 1- Clostridium sporogenes. 2- Clostridium falax. 3- Clostridium histolyticum. Route of infection: Contaminated wound with animal or human dung (wound infected in the street or during war). Predisposing factors: 1- Laceration of muscles. 2- Deep wounds. 3- Factors causing tissue anoxia-shock- ischaemia. Other pyogenic organism consuming oxygen. Pathology: a- Changes in the affected muscle at first clostridium welchii liberates its toxins causing: - Thrombosis of blood vessels. - Death of muscles. - Haemolysis of blood and the release of pigment which stain the muscle salmon red. - Together with other saccharolytic organisms lead to break down of muscle glycogen with production of gases (CO 2 + H2) which spread into tissue planes then the proteolytic organisms act on the dead muscles causing putrifaction and productions of ammonia and H2S. - Ammonia will combine with CO2. - H2S, which is responsible for the offensive odour, combines with iron which is liberated from the RBCs, forming iron sulphide which stains the dead muscle black. b- Changes in the lymph nodes: Regional lymph nodes usually have patches of necrosis without any inflammatory reactions. c- Visceral changes: - Liver: Foaming liver. - Spleen and Kidney: extensive degenerative changes as a result of absorbed toxins. Clinical Picture: Incubation period from few hours to 48 hours. a- General manifestations: - Tachycardia is an early sign. - Temperature is slightly raised but in severe cases may be subnormal. - Local burning pain at the site of wound. - Mental condition is good. - Tongue is dry and coated. - Icteric tinge due to haemolysis. b- Local manifestation: - The wound is oedematous, dark red and of offensive odour. - Crepitus may be elicited due to gas in subcutaneous tissues. - Skin around the wound is pale with purple patches. - Muscles are black and lose their contractile power. Investigations: 1- Culture from the discharge for the organism and Nagler's test. 2- Blood picture shows leucocytosis. 3- X-ray to the affected limb will show gases in the intramuscular planes. The upper limit of the gas should be noticed as the level of amputation should be above it. Treatment: a- Prophylaxis: 1. Proper management of wounds. 2. Antibiotic in large doses. 3. Antigas gangrene serum must be given in all suspected case. 10 cc ampoule of polyvalent antitoxin intramuscular. b- Treatment of established cases: 1. Antigas gangrene serum: 90 cc of polyvalent serum are given daily for 10 days (30 cc/ 8 h I.V). 2. Blood transfusion and intravenous fluids. 3. Penicilline in large doses. 4. Hyperbaric oxygen. 5. Local treatment: the wound is widely opened. All the dead tissues and foreign body should be removed and the wound is irrigated with H2O2 and left opened. In extensive cases amputation is done above the level of gas. 6. X-ray therapy may be of help.