5- News Clippings January - June 2007
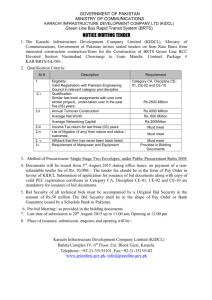
advertisement
JPMC to receive latest facilities: PM KARACHI: A Rs 3.3 billion medical complex will be added to the federal government-run Jinnah Post Graduate Medical Centre soon. The Prime Minister Shaukat Aziz said this during a news conference at Governor’s House Wednesday. The prime minister said that the “state of the art and most modern” project had already been accorded approval by the government. The project would add to the existing federal government medical facilities in Karachi, he said. This project would be equipped with latest technology and highly qualified personnel. The federal government hospitals in Karachi include National Institute of Cardiovascular Diseases and Institute of Child Health. Aziz said that the federal government hospitals in the country were limited in number and needed to be improved. He referred to the government’s programme for providing safe drinking water to the people and said that a number of steps had been initiated to increase awareness among the people about various diseases. APP adds: The prime minister said that the federal, provincial and city governments were fully focused on the development of Karachi. He said that despite the fact that the provincial government was quite self-sufficient and had Rs 20 billion in its reserves, the federal government was also playing its role in developing the city that had an annual population growth rate of five and a half percent, and a vehicular increase of 11 percent. Referring to schemes such as the K-III 100 mgd water supply project and the Lyari Expressway, the prime minister said that these had been implemented with federal government’s funding to meet the city’s water and traffic needs. Meanwhile, speaking at the Eid reception hosted at the Sindh Governor House Tuesday, the prime minister said that he had toured the city and saw a lot of hustle bustle, which was indicative of the development taking place in Karachi. He pointed out that the focus was on the improvement of the city’s electricity system, cleanliness and the law and order situation. “The law and order in Karachi has been improved a lot, but as yet, much is left to be desired as Karachi is a city of 15 million people and deserves a lot more.” He congratulated Sindh Governor Dr Ishratul Ibad Khan on completing four years, and lauded him for having worked very hard to benefit the people of Sindh as well as Karachi. He extended Christmas greetings to the Christians and said that interfaith harmony was the need of the hour in Pakistan as well as the entire world, which is also what Islam teaches. “Islam is a religion of peace, brotherhood and tolerance with no space for extremism, terrorism and sectarianism. The Muslim Ummah needs unity and Pakistan will play its role in creating uniting the Ummah.” Dr Ibad said that both the president and the prime minister visit Karachi quite frequently and takes keen interest in the development of the city. “It is for the first time that the prime minister is celebrating Eid-ul-Azha in Karachi and also the first time that any president or prime minister had visited the mausoleum of the Quaid-e-Azam Muhammad Ali Jinnah on his birthday to pay homage.” Brother of the king of Bahrain and chief of National Guard Bahrain Shaikh Muhammad Bin Khalifa, federal and provincial ministers, diplomats, high officials, leading businessmen, top bankers, sportsmen, artists, senior journalists and social workers were present on the occasion. (Daily Times-B1, 04/01/2007) HIV rate in addicts alarmingly high KARACHI, Jan 5: Facts and figures given in an official document of the National Aids Control Programme show alarming increase in proportion of HIV infection among Injecting Drug Users in Karachi. Officials believe that the country faces a shift in HIV epidemic in the country from low level to ‘concentrated’ among the Injecting Drug Users in Karachi. According to an NACP report developed with collaboration of UNAIDS – Pakistan, the fact showing the rise of proportion of HIV infection among the IDUs was also validated by several studies reporting an increase in prevalence from 0.4 per cent in January to 7.6 per cent in August 2004 and to 23 per cent and 26 per cent in January and August 2005 respectively. “This increase in levels of HIV indicates a shift in HIV epidemic in the country from low level to ‘concentrated’ among the IDUs in Karachi,” it says. According to the report, Pakistan with a population of approximately 157 million occupies an important and strategic position especially in reference to two of its neighbors China and India where HIV and AIDS has graduated to epidemic proportions. Currently, Pakistan is categorized as ‘Low-Prevalence High Risk’ country for HIV infection. The National AIDS Control Programme/ Ministry of Health using WHO/UNAIDS model estimates the number of HIV infections in country between 65,000 and 70,000; with a prevalence of less than 0.1 per cent among general population. First case of AIDS was diagnosed in Pakistan in 1986. Since then sporadic and isolated cases have been reported from the provinces. The report says in addition to the regular passive surveillance mechanism, a number of studies on size estimations, behaviour and biological aspects have also been conducted among the various high-risk groups in recent years. These are a good pointer of the trends; however generalization could be an issue. In July 2003, an outbreak of HIV infection was identified among the jailed Injection Drug Users in Larkana. Over a 10-month period (August 2003 to June 2004) the number of reported HIV cases increased from 19 to 69 among the IDUs. During the same period similar trends were observed in Karachi where seven per cent (57) of IDUs were reported as HIV positive against the total 800 screened by the Sindh AIDS Control Programme. This indicated a rise in proportion of HIV infection among IDUs in Karachi. 1 The HIV prevalence among IDUs in number of cities in Punjab and Sindh also reported increasing trends; 26 per cent Karachi, 2.5 per cent in Lahore; 12 per cent in Sargodha; 0.5 per cent in Rawalpindi; one per cent in Sialkot; and 9.5 per cent in Faisalabad. In view of the changing HIV situation among the high-risk groups, the NACP with the support of development partners undertook two major activities to study the trends and set baselines: A comprehensive national study of reproductive tract and sexually transmitted infections in Lahore and Karachi in the first phase and covering the NWFP, Balochistan and bridging populations in the second phase. Besides, a pilot study under the HIV and AIDS Surveillance Project; the first round of active surveillance has already been conducted in eight cities; preliminary reports and data are under analysis. The findings from both the survey and pilot study for active surveillance corroborated findings for each other. In line with experience from other countries, after IDUs, similar HIV trends are noticeable among men having sex with men and Hijras (transvestite) in selective geographical areas. On the modes of transmission, the data illustrates sexual transmission to be the commonest mode (37 per cent) followed by sharing of the infected needles (21 per cent); however definite mode of transmission could not be ascertained in 34 per cent (due to either misreporting or stigma). Thus both trends as well as characteristics of the epidemic are following a “typical Asian model of HIV”. “It is now required to undertake nationwide estimates of the high-risk groups, their behavorial patterns to ascertain the magnitude of the problems and also do modeling for future projections. This would help the government in further strengthening national response to address the emerging threat in comprehensive manner,” said the report. (By Hasan Mansoor, Dawn-17, 06/01/2007) Dog-bite victim dies at JPMC KARACHI, Jan 9: A 52-year-old dog bite victim from Frontier Colony, SITE Town, who was brought to the Jinnah Postgraduate Medical Centre for treatment on Tuesday, died within five hours. According to in-charge of the JPMC Accidents and Emergency Department, Dr Seemi Jamali, the victim, Banaras Ali was rushed to the casualty of the hospital with a history of severe hydrophobia and fits. After initial inquiry the patient was shifted to Medical Ward-6 for treatment in isolation, but he succumbed to the full-blown rabies only within four and a half hours stay at the hospital on Tuesday. Mr Banaras was bitten on his left leg by a dog in Orangi about eight months back, but neither he told his family members about the incident immediately nor received any vaccination against the bite, Dr Seemi stated while quoting wife of the deceased who along with a son, brought her husband to the hospital. According to the victim’s wife, the incident of dog biting was revealed to family after 6-8 days after which she started trying some home remedies, including use of kohl on the wound, which gave no result and increased the complexities. At home he used to have fits and jerky movements and lately had started getting frightened miserably during urination, the wife added. At JPMC though the patient behaved normally and talked to doctors reasonably, but when tested for hydrophobia, Mr Banaras showed positive symptoms, said Dr Jamali. Normally it takes two days to two years for incubation of rabies in human bodies. She said dog bite victims should report to the JPMC or any other health care facility for snit-rabies vaccination at the earliest irrespective of the depth of the wound. Experts say that 95 per cent of animal-bite cases involve stray dogs, therefore there was a dire need for launching campaign to create awareness about dog bite problems and control over the growing population of street dogs. As precaution, children should not be left alone with a cat or dog and people should avoid making any attempt to intervene in fight between animals or come close to sick animals. (Dawn-19, 10/01/2007) A commendable decision The recent decision taken by the Supreme Court of Pakistan regarding different cases against the Pakistan Medical and Dental Council (PMDC) should be appreciated by all those who want the country to prosper. The decision will have a long-term impact on medical education in Pakistan. It has provided an opportunity to all those stakeholders who want regularisation of medical education in the country. It is good to know that the federal health ministry recently had a meeting with PMDC officials and both have agreed to implement the decision of the Supreme Court. On its part, the PMDC should not waste time and must take all the necessary steps to implement the decision. Before moving to discuss what is needed to be done, it is pertinent to look back and see where we went wrong in this crucial area. A bureaucrat who was not even a doctor was running the affairs of the PMDC for as long as 25 years only because he had very good connections at every level of governance. He remained PMDC secretary for more than 25 years by soft-soaping different director-generals, federal secretaries of health, politicians concerned and military leadership. He destroyed medical education and training in Pakistan by collaborating with members of the medical council and owners of private medical colleges. The majority of these members were doctors, principals of medical colleges, and deans. He had the gift to exploit dishonesty present in such people. He started a system through which the PMDC stopped holding elections in medical colleges for council membership. Principals of medical colleges became members of the council automatically without any election being held. He also made sure that vested interests represent the provinces in the PMDC. He never advertised the notice of elections in the PMDC in national newspapers. He was able to select doctors from provinces as members of the PMDC through conspiratorial methods. 2 It’s time the PMDC took advantage of the current situation and improved the way medical education is imparted in our country During that man’s tenure, provincial governments were able to increase seats in medical colleges out of proportion and were also able to open medical colleges without a standardisation process. The PMDC was not able to challenge the government. The phenomenon of mushroom growth of medical colleges started in the private sector after the establishment of the Aga Khan University in Karachi. Powerful doctors in collaboration with vested interests started the business of medical education. It was an easy way to make money. All kinds of students were allowed to get admission to medical colleges. They were ready to pay any amount of fee provided they would receive an MBBS degree recognised by the PMDC. Medical colleges were opened in residential bungalows, apartments and on poultry farms. The PMDC criminally became a party to this business of exploitation. At the same time, the PMDC did not bother about the faculty situation in government sector medical colleges. The provincial governments and the principals of medical colleges increased the number of seats violating rules and regulations. The worst example was the Sindh Medical College (SMC) Karachi. In the SMC, the principal of the college, in collaboration with the department of health and some corrupt people in the University of Karachi, were able to admit hundreds of students without merit, all of whom became doctors registered by the PMDC. Instead of stopping this illegal admission process, the PMDC became a beneficiary of this business. Then this official was also involved in the bizarre racket of recognition of diplomas in different fields of medicine from different countries. Doctors with substandard diplomas were able to get registered and declared equivalent to FCPS, and became professors in different medical colleges of Pakistan. Members of the PMDC with its secretary were busy making money and obliging friends. They were not bothered about the deteriorating medical education and training process in the country. They did not start any programme for continuous medical education of doctors. They did not even plan re-licensing of doctors depending on their competence and knowledge. They were not worried about patients’ rights and the ethical conduct of doctors. The corrupt official was finally sacked by the new government of General Pervez Musharraf. The new secretary PMDC had a clear cut agenda. He started resisting the council’s wrong decisions as soon as he took over. The council soon realised that the new secretary of the PMDC would follow rules and regulations. The federal ministry of health also found itself in deep waters. The mafia of private medical education was stopped and told that it had to follow rules and regulations. Despite all that, council members took some wrong decisions regarding some medical colleges in public and private sectors for which the council has to take responsibility. They tried to please the government as the majority of its members are from the government. The Pakistan Medical Association pursued the government to come up with a new act to make the council more democratic and autonomous, benefitting patients. Unfortunately, a legal war was initiated against the PMDC by vested interests. It was against this backdrop that the battle was fought in a court of law. Now with the federal ministry of health and everyone else concerned agreeing to implement the decision, it is an opportunity that has never been there before. In this regard, the following steps need to be immediately taken: • The closure of all those medical colleges in government and private sectors that are functioning without permission of the PMDC. • The closure of all those medical colleges that will not be able to fulfill the requirement of the PMDC within six months of the Supreme Court decision. • The relocation of students from unrecognised medical colleges as per instruction of the Supreme Court. • The recognition of provincially recognised medical colleges and the holding of election of members of the medical council in these institutes. The election should be held by the PMDC as per rules and regulations. • The election of representatives from the Sindh, the NWFP and Balochistan. • The election of representatives from public sector medical colleges and universities as per rules and regulations of the PMDC. Doctors should never let their patients down. So, the PMDC must act fast to restore the dignity and honour of doctors in the community. This will only be possible if the PMDC is strict in implementing rules and regulations in the light of the Supreme Court’s decision without any fear. Once the PMDC achieves its independent role there will be a need to address the following issues in the interest of patients and the medical profession: A strong disciplinary committee should be made within the PMDC to deal with doctors’ misconduct in relation to the management of patients. A strong ethical committee should be made within the PMDC to deal with unethical conduct of doctors in relation to patients, the pharmaceutical industry, research work in hospitals, and teaching in medical institutes of Pakistan. A strong education committee should be made for planning of continuous medical education in Pakistan for doctors in public and private sectors. There is a need to develop a system for re-licensing our medical graduates according to the advancement of medical knowledge and the need of patients in Pakistan. There is a need to change the structure of the PMDC. A new act is required to decrease the number of council member. There should be more representation from outside the government through an election procedure. More power and more independence should be given to the council to act freely in the best interest of the profession. (By Dr. Shershah Syed, Dawn-Magazine-5, 14/01/2007) 3 Poor healthcare for children ALTHOUGH symposiums on child healthcare, like the one recently held in Karachi, are welcome, they do not always achieve the goal of prodding health officials to take action. Children in Pakistan, especially those living in rural areas, continue to be deprived of proper health facilities. This is borne out by UN statistics that paint a grim picture: the infant mortality rate at 80 per 1,000 live births is among the worst in the region, while the number of children who die before attaining the age of five is 101 in 1,000. Meanwhile, malnutrition and disease are responsible for 38 per cent of children, not yet five years, being underweight. Even the coverage of the Expanded Programme on Immunisation is far from satisfactory. Figures show that only 67 per cent of one-year-olds have received the necessary vaccinations. A closer statistical survey reveals that certain groups of children are more disadvantaged than others for reasons of gender and poverty. Correcting these deficiencies will require more than awareness-raising actions. Many issues relating to child health are underscored by the UN’s Millennium Development Goals to which Pakistan is a signatory. But the progress the country has made towards meeting these goals by the 2015 deadline is negligible. In order to improve the healthcare system, the government needs to first identify the stumbling blocks and then to review its own performance in overcoming these. If it does so, it will find that one of the main factors that is keeping it from achieving positive results is skewed priorities which attach little importance to social issues such as health. This together with the lack of political will to implement health goals as identified by the international community is preventing it from providing proper healthcare to millions of children across the country. (Dawn-7, 15/01/2007) When painkillers become killers KARACHI: A recent survey has shown that more than 70 percent of people taking medicine do so without either a prescription or a doctor’s consent. It is a trend that worries health experts, as many of those surveyed were using medicines unnecessarily or taking the wrong amounts of dosage. Pharmacists should not be selling medication without a valid prescription, but willingly do so to increase sales. Health experts warn that this is a dangerous trend, and that many are unaware of the long-term effects of excess medication. They have expressed concern over the matter, and argued that it needs to be addressed and stopped in order to save lives. Dr Mahmood Zuberi, Administrator, Baqi University (Fatima Hospital) said that excessive doses of painkillers usually create acidity in the stomach and the intestine, which could cause ulcers if used in the long run. He added that medical stores need to start refusing requests for such medicines without a doctor’s prescription. He feels that people do not seem to understand that it is important to visit their doctors before buying medicine from the chemists, and are unaware that the correct dosage of medicines (quantity in milligrams) is very important and should be prescribed only after a patient has been examined. Even a slight mistake in the dosage can create a serious risk. According to Dr F A Abdalli, a general physician, excessive and continuous use of painkillers will affect the circulatory system and the blood’s productivity, as well as damage the nervous system.Dr Abdalli, who practices in Gulistan-e-Johar, added that while most painkillers are not particularly strong (in terms of milligrams), their continued usage weakens the human body over time. In most cases, the signs or symptoms of health problems relating to the use of painkillers come at a later stage, although serious damage could be done well before the user becomes aware of it. Some chemists, based in the Old City, said that most of their customers asked for Disprin, Panadol or Ponston, and they used these medicines without any prescriptions. Paracetamol is the most commonly used painkiller for general aches and pains, while customers tended to buy Cataflom and Voltron for headaches. Other chemists, based in Gulshan-e-Iqbal, explained that painkillers such as Paracetamol are the cheapest on the market and the most widely purchased. They said that customers seem to believe that by taking them they were addressing the actual problem and would save themselves a trip to the doctor. These pharmacists said that many customers preferred these because they were cheap, and if they did not help they could easily switch to a different and affordable painkiller. Several chemists said that sometimes there was a shortage of painkillers on the market, though such shortages hardly last for more than fifteen days. Dr Muhammad Rafiq Khanani, Associate Professor, Dow University of Health Sciences, said that heart and kidney failure might be linked to the excessive use of such drugs and it tends to happen only when a patient uses these medicines without consulting a professional. According to him, heart and kidney failure are two of the long term observable effects of the overuse of such medicines, and the best way to stop this is to combat the misconception amongst the general public that these medicines are harmless. (By Muhammad Zeeshan Azmat, The News-2, 15/01/2007) When pharmacists get the prescription wrong KARACHI: Health experts have expressed serious concern over availability of potent drugs like Valium, Xanax, Lexotanil and other benzodiazepines over the counter as the number of cases being brought to the hospitals with adverse effects of drugs due to self-medication as well as misinterpretation of prescriptions by unprofessional drug store owners grows. Some 4-11 per cent of all hospital admissions are related to side effects or wrong intake of medicines. Unregulated drug stores involved in unlawful sale and purchase of drugs are turning into the biggest menace in the health care system. The law of not selling medicine of any kind without proper prescription has been ignored ceaselessly, although this is a significant part of the drugs act. 4 “Once a physician has prescribed the drug it is nobody’s responsibility except the patient’s to see how it is administered. Whereas a prescription must be read carefully and explained to the purchaser about the possible side effects and dosage by a qualified pharmacist at the retail store is how it should be,” observes Abdul Latif Sheikh, Director of Pharmacy, Nutrition and CSSD Services of the Aga Khan University Hospital. Some 20-25 per cent people in the city have easy access to allopathic medicines. In all developed countries, over the counter medicines hardly include regular cold preventing pain killers, yet here in our case potent psychotropic medicines are easily available to anyone without a prescription. “I have personally heard an old woman in a downtown medical store demanding ‘Titlee wali Dawa’ which was fulfilled by the person behind the counter by giving her Xanax without offering her a single word of caution,” said Abdul Latif Sheikh. Excessive non-prescribed use of psychotropic drugs like Xanax and Valium is something that has been proven at times to develop criminal behaviour in individuals. He said that it is always the discretion of the unprofessional person at the counter when handing away a drug and many a time they misread the doctor’s handwriting, the cost of which is paid by the patient, sometimes even with his life. “A simple example could be handing over antibiotics. None of the chemists guide the buyer about the correct quantity of the medicine needed. Very few people would know that nearly all antibiotics should not be discontinued before five days. It is observed that more medical cases deteriorate because of misinterpretation of prescriptions by unprofessional drug store employees than by self-medication incidences. Rampant non-regulation of the pharmaceutical retail trade sector seems to have lifted all trust in the role of health ministry’s drug inspectors. “These days all you need is to get your hands on a drug store licence which one can get as easily as the medicine itself. You need to attach the certificate of a pharmacist who has at least graduated in pharmacy and would be present at the pharmacy during business hours. But that’s about it. No one comes around to check if all these things are being conformed to or not,” says Naseer Khan, a former drug store owner in Nazimabad. “The standard parameters of storage of drugs are definitely not what we have in Pakistan. People come to us saying that Pakistani medicines don’t work on them, while if they buy the same drug at another country’s airport, they would find it very effective,” said Mr. Sheikh. He explained that the medicines are not stored at the proper temperature that is clearly labelled on the packaging and their performance deteriorates in nature once their shelf at a certain temperatures gives way. “For example, if not refrigerated and left at room temperature, insulin has a shelf life of 30 days instead of the acknowledged two years,” he said. “People complain that the local manufacturers don’t produce quality medicines. I’d say that the fault lies in the distribution channels, not the manufacturing,” Sheikh stressed. The district administration of Islamabad has recently amended the Drug Rules of 1989 and made it mandatory for all prominent medical stores to employ full-time pharmacists. A city like Karachi is definitely in need of such a move as quacks are flourishing here by the day. (By Asra Pasha, The News-4, 16/01/2007) Experts discuss high maternal mortality rate KARACHI: The department of Gynaecology and Obstetric organised a two-day symposium on ëCritical Care in Maternal Medicineí at the Liaquat National Hospital Convention Centre. Convener of the symposium Dr Shagufta Tahir explained that the department of Obstetrics and Gynaecology had organised many scientific programmes including biannual CMEs for postgraduate doctors and general participants besides workshop to develop skills of doctors. According to Dr Shagufta, theme of the symposium was chosen carefully, considering very high rate of maternal mortality 350-400 per 1,00,000 in Pakistan. The symposium was dedicated to all those mothers who died enduring labour pains, she added. She said that 70 per cent of the labour cases were attended by the untrained midwives leading to the high death rate in the country. Prof Dr Rashid Latif from Lahore consented to be the chief guest and said that he was impressed by the audienceís participations who traveled from different parts of the country to reach in the inaugural session. President of Society of Obstetrics and Gynaecology Prof Dr Farrukh Zaman presented his views on ëRisk Managementí in obstetrics. Related with the theme of the symposium, an art drama was presented by Sheema Kirmani entitled ëMeri Zindagi Ka Safarí. Sheema presented drama covering cultural, social taboo regarding the health of young girls, their educations, attitude towards child birth and pregnancy. (The News-4, 16/01/2007) The nation’s health By Ardeshir Cowasjee IT is bad. But it is one of the many ‘core’ issues facing us and must be addressed. Generally recognised is the fact that Pakistan has a damaging dearth in areas in which it should not have a dearth and equally damaging surpluses in areas in which there should be no surplus. Let us, for the moment, just take two of these extreme areas – population and doctors. The country is grossly overpopulated and the number is growing at the frightening rate of 2.1 per cent – it is estimated that there are now over ten births per minute. (As an aside, it must be admitted that far too many members of the population are illiterate, bigoted and terrorism-geared but that is another story.) As for doctors, there is a serious dearth, with a very low ratio of doctors to population, and projections are that the shortfall is on the increase. 5 A large number of the Aga Khan University faculty (of which 63 per cent are foreign qualified) got together last year with a large number of experts from various international health and medical institutions, and printed in the December 2006 Supplement of the publication ‘Academic Medicine’ was a paper written by two AKU professors, doctors Jamsheer Talati and Dr Gregory Papas entitled ‘Migration, Medical Education, and Health Care : A View from Pakistan.’ Pakistan has a current ratio of 0.473 physicians per 1000 population – the US ratio being 2.93 per 1000. There was at the end of 2005 an estimated 73,890 physicians practising in Pakistan, and some 1,700 physicians per year are lost, for various reasons, from this practising pool. Over 1000 are emigrants to greener pastures, where they earn more, have a far better lifestyle, better prospects for their and their children’s education, and international exposure. It is a move for betterment, an inbuilt right, and can benefit human society at large. Migration of our doctors is a problem but it cannot be halted. One other factor spurs emigration in our case – the poor self-image of the native land and the inordinate admiration of all things foreign. Pakistan is the third leading source of international medical graduates in affluent countries. In 2005, a survey showed that there were 12,813 physicians from Pakistan in the US, the United Kingdom, Australia and Canada. There were a further 12,200 in other countries, mainly in the Arabic-speaking nations. Saudi Arabia alone requires an additional 20,000 Pakistani doctors and we have been asked to send out to that country as many as we can spare. We lost many good doctors to migration and bullets in the closing years of the decade of the 1990s and at the start of this century when there was a spell of targeted killings of doctors on sectarian grounds. This has now luckily given way to a more rational flow – to advanced technology-inventing nations for post-graduate studies and citizenship, and to the Arabicspeaking countries for service and lifestyle. The main cause of physician deficit is the country’s inability to educate an adequate number of doctors for a burgeoning population with a complex burden of infectious and degenerative diseases, cancer and accidents, all of which are on the increase. Pakistan’s total health expenditure in 2004 was 2.4 per cent of the gross domestic product – less than on education and pathetic in comparison with defence and debt servicing. Then there is the gender factor. On an average 50 per cent of those admitted to medical schools are women. They have a high pass rate, but they also have a high drop-out rate because of marriage and childbearing. Only 38 per cent of our practising doctors are women – they are an annual continuing loss from practise. Other losses to practice are doctors who practise part time, teach in basic science departments, work in government offices, or who become governors, chief ministers, members of parliament or waft their way into other elevated lucrative positions. Apparently, there is no serious dearth of medical colleges – only a dearth of teachers, facilities and teacher training institutions. Class sizes are also a problem as in many public institutions they exceed 300 which impedes efforts to improve learning. And even access to medical education, despite income disparities, is not limited by poverty or educational or geographical disadvantage. The average total cost of providing five years of medical education is, according to the TalatiPappas paper, approximately $100,000, split between government and private colleges. The conclusion reached in Doctors Talati and Pappas’s paper is that Pakistan cannot meet its needs for healthcare given the current levels of production and dependency on physicians in the organisation of the system. To quote: “Looming physician workforce shortages cannot be easily met by increasing the number of medical schools or by enacting legislation on migration. The shortage of physicians is a problem that Pakistan shares with the developed world. The need for physicians is rapidly outstripping production globally and is forcing us to rethink medical education in both resource-rich and resource-poor countries. At the current levels of production, Pakistan and other developing countries cannot meet their current needs and will not be able to meet the needs of the developed world. . . . “Residency programmes could be improved through better assessment of inductees, a basic core programme common across nations, and free movement of residents between programmes, especially those in different countries, for part of their education. Migration causes critical impact even when numerically insignificant, but it is inevitable. It is unreasonable to expect the diaspora in high-pressure advanced environments to leave their demanding environments to work in Pakistan, unless work environments in their adopted homes provide time for engagement in their parent country. . . . “Above all, an engagement of society is essential, as technologies radically disruptive of conventional approaches and current ethics have arrived and will consume physicians’ time. Universities need to develop graduates’ sense of altruism and the need to serve resource-poor settings.” High hopes! None of the 80-odd who sit cramped around the oversized cabinet table with prime minister Shaukat Aziz and attempt to govern this country will rush to Doctors Talati and Pappas () to ask questions. However, a copy of their report is being sent to Health Minister Mohammad Nasser Khan who is said to be ‘pro-active.’ (By Ardeshir Cowasjee, Dawn-7, 21/01/2007) Sobhraj hospital lacks basic facilities KARACHI, Jan 21: The Sobhraj Maternity Hospital, the biggest maternity hospital under the management of the city district government, has been facing serious problems because of lack of basic facilities. The hospital has two ambulances and a van lying out of order and lying dumped in the compound for a couple of years. As no attempt has been made to get them repaired, the vehicles have almost destroyed owing to their constant exposure to sunlight and rainwater. An official of the hospital stated the hospital did not even have a vehicle to bring its staff to hospital in case of any emergency. There is only one pick-up still in order and the vehicle is being used for all transportation purposes. The stone-built building of the hospital constructed in 1928 also lacks proper lighting arrangement. Sanitary conditions, particularly in private rooms, in the building are fast deteriorating while there is no proper arrangement for water supply in bathrooms. In the absence of tap water, the patients, staff and visitors have to use subsoil water, which is causing damage to pipelines. 6 He said that the city government’s department concerned was apprised of the situation with request for steps to resolve all these problems. However, all that which has been done so far is the digging carried out for laying a new pipeline for water supply in bathrooms. On an average, 5,000 patients visit OPDs at the Sobhraj hospital in a month. The number of in-house patients remains around 750 in addition to the 400 maternity cases, including operation cases, a month. Most of the patients come from the poor and middle classes. The urgent requirement of the hospital is an ambulance and van to cater to the transportation needs of some 225 staff members, besides arrangement for lighting, improved hygienic conditions and safe drinking water for the staff, patients and visitors. (Dawn-14, 22/01/2007) Rickshaw noise a perennial assault on public ear KARACHI: The shabby, worn-out and undisciplined road-based public transport in the city is one of the main culprits of increasing air and noise pollution. It is generally felt that without changing the prevailing public transport culture, complete revival of Karachi Circular Railway (KCR) as well as induction of CNG buses, this city could hardly get rid of its alarming pollution. The level of both air and noise pollution in the city is crossing safe limits and turning into a serious threat not only for its socio-economic activities, but also for the health of its citizens. Besides other factors like smoke-emitting vehicles, factory fumes and burning of garbage in the open, it is the two-stroke rickshaw that is widely blamed for the alarming levels of air and noise pollution in the metropolis. The Pakistan Medical Association (PMA) Karachi Chapter’s General-Secretary, Dr Qaiser Sajjad, said that in a survey of PMA on air pollution, it emerged that noise level of traditional old two-stroke rickshaw was from 95-110db, while noise level of an airplane engine was from 120-140-db. He said that a normally human ear could tolerate noise up to 85-db and all noises above this level were harmful for human health. The unbearable noise pollution in Karachi is causing hearing problems for the citizens. Excessive noise level is also harmful for the human nervous system, leading to headaches, mood disorders, high blood pressure, depression, anger and ultimately serious coronary and heart diseases. Both city planning and healthcare experts have been demanding since long that to bring down excessive air and noise pollution levels, two-stroke rickshaws be turned into four-stroke ones, and smoke-emitting buses and minibuses be changed with wide-bodied CNG buses, and the Karachi Circular Railway system should also be revived and expanded. A local train could cater needs of several thousands of commuters and a good and cost-effective replacement of dozens of buses. Only an efficient rail-based system like KCR could lessen our dependence on the road-based transport. This will not only help unclog traffic-jam stricken roads, but also improve environment due to lesser noise and air pollution. It is matter of worry that despite orders of the Supreme Court to take action against vehicles causing pollution, concrete, sustained and visible actions were yet to be taken by the government. The smoke emitted by these vehicles is highly poisonous, spreading respiratory infections, asthma, tuberculosis, lung cancer and other serious ailments amongst Karachiites. (The News-2, 22/01/2007) Ziauddin Medical Uni students prefer internal medicine and Pakistan: study KARACHI: Ziauddin Medical University researchers have found that students chose internal medicine, surgery, and pediatrics as their first three career choices and clinical specialties were highly rated as compared to family medicine. The study was conducted in the Ziauddin Medical University (ZMU), a private medical university established in 1996. The participants were 232 final year MBBS students of the first five classes of the ZMU, between the years 2000 and 2004. The participants, 160 women and 72 men, were presented a 26-item questionnaire, which assessed areas including their choice of specialty, location preferences, and reasons influencing career choices. The findings were published in the journal ‘Education for Health’ in Nov 2006 by Nighat Huda and Sabira Yousuf. The study on career preferences of final year medical students and gender differences in career choices, also showed that although there was a growing trend among new graduates going abroad for better opportunities, a high percentage of students regardless of gender indicated Pakistan as their preferred choice of country to practice in, with the United Kingdom as the second and the United States as the third choice. Interestingly, findings from this study, particularly on choice of specialty and factors that influenced these decisions, were similar to those which had taken place elsewhere, an example of which was a study undertaken in the UK that revealed that students preferred to practice in their own country, whereas overseas student preferred to return to their homeland. Personal interest was ranked as the most influential factor in the choice of specialty. Most respondents preferred working in the public sector rather than a private or university setting, and also favored working in urban areas over rural ones. Career preferences, as the study revealed, were also subject to gender. Men and women placed significantly different importance to pediatrics and internal medicine. Among the first three preferred specialties, women chose internal medicine as the first, pediatrics as second and surgery as third. For the men, the first choice was the same as that for women, but the other two differed in which surgery was their second choice and cardiology was the third. Men and women appear to 7 prefer specialties that are congruent to their gender schemas; females generally opted for pediatrics and gynecologyobstetrics while men selected surgical specialties. The study also concluded that despite the university’s introduction of community-based activities and family attachments, a trend towards students not selecting family medicine was obvious. Likewise, the health system and medical education did not reinforce the need for general practitioners in the country and the exposure to specialties took priority over family medicine. In general, students tended to select hospital medicine over general practice. Among other factors, experiences in chosen specialties during training as well as the social milieu of the medical university, the teaching programme and role models were important influences in career preferences. Expectation of material rewards, societal appreciation of specialty and specialists, response of specialty patients to treatment, and the role of specialty teachers were also ranked highly as factors in choosing specialties. From a list of factors provided, students indicated whether there was a ‘very strong’, ‘strong’, ‘moderate’, ‘little’, or ‘no influence’ on their career choice when it came to these factors. Overall, the students rated ‘personal interest’ as the most influential factor contributing to career choice and the chi-square analysis revealed that there was a significant difference between men and women on factors such as ‘intellectual challenge’, ‘professional independence’, ‘parental preference’, ‘few specialists in the country’, ‘content of specialty’ and ‘policies/mission of the college’. According to the study, men as compared to women were likelier to be influenced by factors such as intellectual challenge, professional independence, content specialty and policies/missions of the college. When it came to the setting where they would prefer to practice their chosen career preference, the first setting was private university teaching hospital, the second was private specialists’ clinic, and the third was a public university setting. Men were more likely to choose NGOs as their first choice while women more often ranked this as their second or third choice. The researchers conclude that knowledge and understanding related to trends in career choice could lead to the identification of departments that required strengthening. For relatively new universities, such information was useful in strengthening individual programmes and planning for the future. (Daily Times-B1, 22/01/2007) Korangi’s leather tannery workers have high levels of asthma: study KARACHI: The prevalence of asthma in leather tannery workers in Karachi appears to be high and is associated with educational status, ethnicity, smoking, glove use, perceived to have allergy and duration of work, according to a study that appeared in BMC Public Health 2006. The study was authored by Khurram Shahzad of the Department of Community Health Sciences, Aga Khan University, Saeed Akhtar of the Family Health International, Pakistan Country Office, Islamabad, and Sadia Mahmud of the Department of Community Medicine & Behavioral Sciences, Faculty of Medicine, Kuwait University. A cross sectional study was conducted from August 2003 to March 2004 on leather tannery workers of Karachi. Data were collected from 641 workers engaged in 95 different tanneries in Korangi industrial area selected as sample of convenience. Prevalence of adult asthma was 10.8% (69/641) in this study population. The prevalence of perceived work-related asthma was 5.3% (34/641). After taking into account the age factor, the leather tannery worker were more likely to be asthmatic, if they were illiterate, of Pathan ethnicity, ever-smoked, reportedly never used gloves during different tanning tasks. Also, there was a significant interaction between perceived allergy and duration of work. Those who perceived to have allergy were more likely to have asthma if their duration of work was 8 years and this relationship was even stronger if duration was 13 years. Asthma is one of the most common chronic inflammatory disease of airways, characterized by hyper responsiveness to a variety of stimuli. Among the various risk factors of asthma, those of occupational origin are gaining more importance due to use of various chemicals in industries which potentially induce hypersensitivity and predisposition to asthma. Leather tanning is principally chemical preservation of raw hide by a process in which binding of various chemicals (mainly chromium salts e.g. potassium dichromate) to proteins in raw hide takes place. Chromium has potential to bind with skin proteins of tannery workers to produce complex antigens which lead to hypersensitivity. The resulting contact dermatitis could be preliminary condition to the development of bronchial asthma. Tannery workers are thus exposed to harmful agents rendering them vulnerable to respiratory tract and skin problems especially. Only male workers were enrolled who were working with tanning process (i.e. handling from raw hide to finished leather). Workers from administrative and other departments of tannery were excluded. Most of the tanneries in Karachi are located in Korangi industrial area. There are 95 tanneries in Korangi Industrial Area. Thirteen factories allowed their workers to be interviewed during factory timing. For the remaining factories, the team visited the colonies where workers lived and interviewed them there. Almost 40% to 50% of the workers associated with the tanning process were selected from each tannery as a sample of convenience. There were two major ethnic groups i.e. Punjabi (53%) and Pathan (33%). Other ethnic groups composed of Urdu, Balochi, Sindhi and Brahvi. Most of the workers were employed on daily wages (77%). Income ranged from 1,000 to 55,000 rupees per month and almost 49% of the workers had income between 3,000 to 5,000 rupees per month. Approximately 41% of the workers were illiterate, about 20% had education between 1-5 years and 35% between 6-10 years. Majority of workers were living in rented houses (59%). The mean duration of work (years) was eight. Of 641 workers included in the study, 69 (10.8%) subjects reportedly were asthmatic. Of 69 asthmatic subjects, 34 (49%) reported an association of their symptoms with work. Illiterate men were more likely to have asthma compared to those who were literate. Pathan workers were more likely to have asthma compared to workers of Punjabi ethnicity. Workers who did not report the use of gloves were more likely to have asthma compared to those who used them during different tanning tasks. Even smokers were more likely to have 8 asthma compared to those who had never smoked. The workers who perceived to have allergy, were more likely to have asthma if they’d worked for 8 years and this relationship was even stronger if the duration was 13 years. However, there was non-significant relationship between duration of work and asthma for those who did not have perceived allergy. This cross sectional study estimated an asthma prevalence of 10.8% in leather tannery workers of Karachi and, to our knowledge, is the first report from Pakistan. To our knowledge, only two studies have estimated asthma prevalence in tannery workers. Shukla et al. found a prevalence of 2.2% for occupational asthma in tannery workers in India. Ory and colleagues estimated an asthma prevalence of 38% in tannery workers in a study conducted in Kanpur, India. On the other hand asthma prevalence in our study population is higher than that reported in men in Iran (2.4%), Bangladesh (4.4%) and India (4%). Glove use was protective for asthma in our population. Latex glove use was found to be protective for two or more workrelated respiratory symptoms. On the other hand, Its use has been known to induce asthma and hypersensitivity due to latex content. Skin exposure to chemicals have been shown to play a role in initial immunologic sensitization, which is a very important link in causal chain for asthma. Comparable data on prevalence of asthma in general population in Pakistan were not available. This study showed that educational status, ethnicity, smoking status, perceived allergy and glove use are significantly associated with asthma. Further research needs to be done on asthma in general population and tannery workers in Pakistan, with use of objective tests to demonstrate occupational nature of the diseases. (Daily Times-B1, 23/01/2007) Missing factors in health education By Zubeida Mustafa THE good news from the medical sector is that Dr Azhar Faruqui, the enterprising director of the National Institute of Cardiovascular Diseases, Karachi, has taken the initiative to establish a paediatric cardiology unit at the NICVD. This will be the first of its kind in Karachi. Lahore already has one such unit. Until now, infants needing cardiac surgery did not have many choices and many of them went abroad for simple corrective surgical procedures if their lives were to be saved. Some medical professionals resent it that patients are taken to India when similar procedures can be performed here. But the fact is that the facilities here are very limited. Recently, Shabina, who runs the Garage School for children of the katchi abadis in Clifton and also arranges for the healthcare of her students and their families when needed, took Maxwell Happy, aged 14 months, to Chennai for a congenital heart problem that needed corrective surgery. Doctors in Karachi had refused treatment saying they did not have the post-operative care facilities to perform the operation on such a young child. It is therefore heartening for children like Maxwell that the NICVD will be setting up a unit for paediatric cardiology. Dr Azhar Faruqui told media representatives that he plans hiring the services of foreign surgeons and anaesthesiologists for the paediatric unit. While initially foreign expertise might be required, one hopes that Dr Faruqui plans to have his own men and women trained in this branch of medicine as soon as possible. Pakistan does not lack surgeons and physicians who excel in their field, although the declining state of medical education in the public sector has badly affected the middle cadre health professionals. But it would be a short-sighted policy to go in for foreign experts on a permanent basis rather than create training facilities to produce our own paediatric cardiologists. We return to the question posed in these columns a few weeks ago: do we really need foreign expertise? Yes, for paediatric cardiology until NICVD can train its own specialists, which should not take more than a few years. Other health institutions in the country are sending their professionals to foreign medical institutions to provide them training under an arrangement. The Sindh Institute of Urology and Transplantation invites transplant surgeons to perform specialised surgery to train their own staff. There have been other precedents. Prof John Hadfield, a British surgeon who died recently, rendered yeoman service to this country by paying annual visits to conduct post-graduate courses in surgery free of charge for the fellowship examinations of the Pakistan College of Physicians and Surgeons. He did that for 30 years until advancing age and failing health prevented him from undertaking the arduous journey. It is estimated that over a thousand Pakistani surgeons owe their post-graduate training to Prof Hadfield. It is time that we explored innovative measures in the health sector. These should be designed to train young health professionals to equip them with expertise in modern technology and knowledge in their respective fields. The idea should be to opt for methods that do not unduly enhance the cost of treatment since ultimately it is the poor man who has to foot the bill for his own treatment. It is therefore more feasible if doctors who plan to stay in Pakistan and serve their own people are trained in their own environment or as close to home as possible. We have a strange paradox here. The public-sector medical colleges and universities, which at one time produced topranking physicians and surgeons in the country, are in a state of rot with a few exceptions. Many new institutions are so appalling in terms of the quality of education they provide that it is actually hazardous to seek treatment from the so-called doctors produced by them. The private sector medical institutions are vastly superior and also seek to root their education in the local socio-cultural milieu. One would have expected their graduates to form the backbone of the health delivery system. But they failed because they are not motivated enough to stay and serve their own people. They opt for the greener pastures abroad. Hence, the first step should be to revamp and radically upgrade medical education in the public sector, which should also be tailored to indigenous conditions. If medical professionals are trained scientifically on the basis of the concept of continuing education, their performance would improve since they would understand the local needs and the people better. Some may have to be sent abroad for 9 specialised training. But many would not have to go far. The medical institutions in China seem to produce better graduates and are quite affordable too ($2,475 per annum which includes tuition and hostel). Moreover, the health statistics of the country are living testimony to the commitment of the Chinese to public health. Four indicators can be taken as the yardsticks to measure the state of health of a nation. One is the life expectancy at birth which is 71.5 years for China and 62.9 years for Pakistan. Infant mortality rate in these countries is 26 and 80 per 1,000 live births. Maternal mortality rate in China is 51 per 100,000 live births and 530 for Pakistan. And above all, the literacy rate is important to determine the capability of the people to contribute to their own health. In China 91 per cent of the people above 15 are literate. In Pakistan, this figure is 50 per cent. What is missing in our medical colleges and health professionals is the sensitivity to the importance of public health. Very few of our physicians lobby the government on public health issues. How many of the medical bodies have launched serious campaigns demanding clean water, sanitation, better solid waste management? Significantly, all of these have a direct bearing on the health of the people. It is important that a holistic approach to health be inculcated in health professionals and medical students. Specialists are certainly needed and some foreign training will improve their skills and knowledge. But better public health policies will reduce the need for medical specialists because people would not be falling ill so frequently. (By Zubeida Mustafa, Dawn-7, 24/01/2007) Civil Hospital emergency room in a disgusting state KARACHI: If exemplary sanitation and the refreshing smell of disinfectant is what you identify a hospital’s ward with, then the Emergency Ward at the Civil Hospital Karachi fails to pass that description. Negligence on part of the authorities and the public alike is clearly evident from the current state of the place. It appears as if the walls of the Emergency Ward are officially there for all sorts of phlegm and the treatment room looks more like the inside of a slaughterhouse with walls soaked beneath layers of paan stains, and an overwhelming stench coming from the drain. The stretchers, counters and operating table standing inside the treatment room are all covered with old, dried bloodstains, which is utterly and inexplicably unacceptable for medical treatments. The floor seems to have never been mopped, and clean washrooms seem too grandiose a thing to ask for in the face of these circumstances. The ward has been there for several decades and has been serving no less than 300 people a day for the past five years, a figure which is constantly increasing. Since the Civil Hospital, being the largest tertiary care unit in the city, is always short of proper funds for development work, most of the development that is evident on the premises nowadays is a result of public-private partnership endeavours. Under the same arrangement, the ward was renovated during the late eighties with the help of the Patients’ Welfare Association, a student-run NGO. That was the only development work it has undergone in the past thirty years. A former high official of the hospital revealed that a grant plan of Rs1.5 billion has already been sanctioned for the relocation and rebuilding of the ward. “The plan was generated during the term of the former Medical Superintendent of the hospital, but it has been delayed to date, due to internal conflict between authorities among other reasons,” he said. “There is a piece of land that SIUT want to grab on the premises, and the land where it is supposed to be relocated at the Chand Bibi Road requires the neurosurgery department to be demolished and relocated,” he added. Today, the ward caters to around 500 people a day, and its 35-40 bed accommodation with a team of seven doctors bears that burden. The land area outside the front of the ward has fallen victim to encroachment by fruit sellers, drug sellers, public transport, and the poor attendants of patients from other cities who have no other place to stay in the city. The encroachment not only hinders the public’s access to the ward but also at times makes it difficult for the doctors to do their duty in moments of high level emergencies. The encroachers also steal electricity from the hospital’s supply, which increases the risk of a short circuit and fluctuation inside the ward. There is a hospital drain line that passes directly above the ward’s roof, which is leaking profusely leaving the air inside the ward undesirably damp and smelly. Despite several complaints to the concerned departments, the drain has not been fixed or moved. The new contract for the janitorial services for the ward was also approved two months ago during the board meeting, but since then the authorities have been sitting on the issue and delaying it. The senior official said that he firmly believes that without relocating the ward from its existing place, there is no solution to any of these problems. Civil is the largest public sector hospital in the province, and both the public and government bear the responsibility for its pathetic state. (By Asra Pasha, The News-2, 25/01/2007) Private hospital watchdog okayed by CM KARACHI: Sindh Chief Minister Dr Arbab Ghulam Rahim met Sindh Health Minister Sardar Ahmed on Wednesday and approved the formation of a regulatory authority for private hospitals and clinics operating across the province. The approved proposal will be immediately referred to Sindh Governor Dr Ishratul Ibad Khan for the promulgation of an ordinance, paving the way for the early and effective working of the authority. It will have full power to issue licenses for the opening of any new healthcare facility and also to cancel the license in the case of a violation of the set rules and poor handling of patients etc. Rahim also approved the creation of a special public health section within the ambit of the Sindh health department. Captain (retd) Abdul Majid has been appointed Sindh public health special secretary and has the authority to look into the medico-legal, administration and drug inspectorate departments. 10 Fourteen development schemes were initiated by the provincial health department, and the need to streamline drug inspection and registration is also largely felt. Under the given arrangement, health secretary Prof Naushad A Shaikh will handle curative issues. Shaikh will hold equal status as those of his counterparts representing other departments of the Sindh government. The chief minister also approved the revised service structure for around 750 specialists associated with the Sindh health department. A three-tier formula will now be adopted, paving the way for the promotion of 17 percent of these grade-18 specialist doctors to grade-19 and the promotion of another eight percent of them to grade 20. Other specialists would remain in grade 18. Also, 49 new grade-20 posts and 56 new grade-19 posts have been created in the department, costing an additional Rs 11.717 million. This would be the fourth service structure introduced by the present government in the health sector since 2006, after the revision of the service structures for the general cadre of doctors, nurses and paramedics. (Daily Times-B1, 25/01/2007) Condoms win over other family planning methods in slums KARACHI: Forty-one percent of 404 women in squatter settlements use condoms followed by the IUD (16%), injectables (15%), the pill (12%), tubal ligation (12%) and other methods, including the hormonal implant, male sterilization and the diaphragm (4%), according to a study. The research was published by FF Fikree, A Khan, MM Kadir, F Sajan, MH Rahbar as an article ‘What influences contraceptive use among young women in urban squatter settlements of Karachi, Pakistan?’ in the journal ‘International Family Planning Perspectives’ in September 2001, and while it may be a little old, the nature of the data indicates that some observations can still be helpful. Despite being one of the first countries in South Asia to launch a national family planning program, Pakistan is exceptional in the region for its poor performance in improving contraceptive prevalence. After nearly three decades of governmentsponsored family planning programs, contraceptive prevalence has increased from 5% in 1974-1975 to 24% in 1996-1997. Paradoxically, a significant proportion of women do not wish to have additional children. For the study, interviews were conducted in squatter settlements in Karachi with Muslim women 30 years old or younger, their husbands and their mothers-in-law. Analyses indicate that women who reported using modern contraceptive methods were significantly more likely to be literate, to be exposed to an urban environment and to have had at least five live births. Women who were literate, who were of high economic status, whose mother-in-law reported discussing family planning with them and who had received family planning messages from healthcare workers were 2 to 3 times as likely to use contraceptives as were other women. In addition, women who said it was appropriate for family planning messages to be delivered through mass media were 50% more likely to use contraceptives. Opposition to family planning by husbands and mothers-in-law contributes significantly to unmet need, even among women who are receptive to family size limitation. Moreover, women in South Asia are taught that their own interests are subordinate to those of the family group. Consequently, they are likely to sacrifice their own desire to regulate fertility. In the context of family planning, women’s discussions with their husbands are strongly associated with their attitudes toward contraceptive use. In addition, the presence of mothers-in-law in the household is influential in determining family size. Women’s autonomy, defined by their decision-making abilities within their household and their mobility outside of their home, is strongly influenced by kinship and marriage relationship, by age, by religion and by division of labor within traditional patriarchal societies. Pakistani women’s ability to leave their home has an important bearing on their awareness of the world around them and could influence their adoption of contraceptive methods. Purdah dictates that the sexes be physically segregated outside the household and that women wear a veil in public. As a result, most Pakistani women lack the freedom or autonomy to move about in public and, more often than not, need a chaperone to go anywhere in public, including to a health facility. Pakistan officially condoned family planning and launched its national family planning program in the early 1960s. However, one of the several reasons stated for the dismal performance of the population program is that because of religious beliefs, the common Pakistani man does not view family planning favorably. According to the Pakistan Demographic and Health Survey of 1990-1991, 13% of women and 18% of men report “religion” as their reason for not using contraceptives. During the first half of 1996, we conducted a study in eight urban squatter settlements of Karachi. From 1984 to 1996, the Aga Khan University operated primary health care programs in six of the settlements. To be eligible to participate in the study, women had to be married, Muslim and 30 years old or younger, had to have at least two living children and had to live with a Muslim spouse and mother-in-law. Nearly one-quarter of the women in the sample were younger than 25, and 68% reported at least four live births. More than half were literate, but only 9% reported earning an income. Their spouses were generally older than they were - 4% were younger than 25 and 73% were 30 years or older; 78% were literate, and all but 3% were employed. Though 86% of mothers-in-law were illiterate, the proportion who reported working to earn an income (12%) was slightly greater than for the daughters-in-law. Consistency in reports of spousal communication about family size varied considerably among the 717 couples - while 81% of wives reported such communication, only 34% of husbands did. Reports of communication about family size between women and their mothers-in-law and between husbands and their mothers also varied. While 57% of women said they had discussed the topic with their mother-in law, only 38% of mothers-in law said they had discussed the topic with their daughter-in-law. Furthermore, 19% of mothers said they had discussed the topic with their son, but only 7% of sons said they had discussed the topic with their mother. Reports of spousal communication about family planning were quite consistent - 94% of wives and 85% of husbands reported such communication. However, 84% of women reported communication about family size with their husbands, while only 40% of husbands did so. 11 Smaller proportions of mothers-in-law than daughters-in-law reported communication with one another about family size and family planning. While 62% of women using a method reported having discussed family size with their mother-in-law, 41% of mothers-in-law reported such discussions with their daughter-in-law. Regarding discussions about family planning, 52% of women said they had talked with their mother-in-law, while only 35% of mothers-in-law said they had discussed the topic with their daughter-in-law. Even smaller proportions of sons and mothers reported discussing these topics with one another, and their responses also were inconsistent. While 22% and 10% of mothers reported speaking with their sons about family size and family planning, respectively, 8% and 4% of sons, respectively, reported having discussed these topics with their mothers. In the squatter settlements, where it is relatively easy to access modern family planning methods, we learned that after controlling for women’s education, accepting family planning messages delivered through mass media, having a mother-inlaw who discusses family planning with them and receiving family planning messages from a health care provider strongly influenced women’s likelihood of using contraceptives. However, women’s level of autonomy - based on their ability to make decisions within the family and to go out of the home unaccompanied - did not significantly influence their contraceptive use. One exception is our observation that there is not a significant association between contraceptive use and women’s discussions with their husbands about family matters, including family size and family planning, which have been found to be important for predicting fertility change. The only household communication that remained significant in the analysis was that of the mother-in-law’s reported discussions about family planning with her daughter-in-law. Thus, in the traditional Pakistani patriarchal and patrilocal family structure found in the low-income squatter settlements of Karachi, a woman’s mother-in-law appears to have a strong influence on the couple’s reproductive decision-making. (Daily Times-B1, 25/01/2007) World Health Updates Forum: Heart disease kills more women due to gender bias KARACHI: There is a misperception that heart disease is limited to men and 500,000 women die of it every year due to a lack of proper treatment as gender bias has affected diagnosis, said NICVD assistant professor of cardiology Dr Ishtiaq Rasool at the first session of World Health Updates forum Friday. Pediatric Cardiologist Prof Anita Sexana from India presented a paper on Congenital Health Disease and Dr Rajesh Sharma from Banglore talked about Pediatric Cardiology amongst others. Women believe that cancer is a bigger threat than heart disease and nearly twice as many American women die of heart disease and stroke than from all cancers combined. One in five women has some form of cardiovascular disease, 38 percent of women who have a heart attack die within one year and 40 percent of coronary events in women are fatal and most of them occur without warning. Rasool said that women develop heart disease later in life than men. Symptoms of a heart attack in women might differ from those in men, leading to misdiagnosis. Also, 42 percent of women die within one year of a heart attack versus 24 percent of men. Furthermore, 72 percent of young women aged between 25 to 40 years still consider cancer to be the greatest threat to women's health. Some women know about the risks of heart disease but do not "personalize" it. Sixty-five percent of women recognize that symptoms might be "atypical" but do not know classic symptoms. Women usually learn about coronary artery disease (CAD) from magazines and the internet and do not consult their physicians. Prof Anita Sexana said that the major heart diseases are related to congenital heart disease and rheumatic heart disease. Such diseases are found in one in 100 children and require early intervention. Also, 80,000 babies are born in India with such diseases every year and only 3.04 percent children are treated. Genetic counseling is a problematic area as mothers refuse to terminate the pregnancy if they are told that the child is suffering from a cardiovascular disease. Prof Kalimuddin Aziz said that it is a misconception that hypertension disease is an adult disease. In fact, it is also present in children. Poverty was the main cause of this disease and the risk factor was high among Pakistani children. According to Dr Maqbool Tafri, hypertension is a silent disease and does not have symptoms. People remain unaware about it unless they suffer from complications. People with HTN suffer from strokes, heart attacks, eye problems and kidney problems. In developed countries, 50 percent people suffer from the disease while in under-developed countries 70 percent of people suffer from it. Those diagnosed are not provided adequate treatment. Only three percent of Pakistanis have been able to control their high blood pressure. Furthermore, 20 percent of patients of the disease discontinue their treatment after one month of diagnosis while 50 percent of patients discontinue their treatment after six months. Prof. Mohammed Ishaq said that every year 7.3 million people die of heart attacks and 5.1 percent die due from strokes. India and Pakistan are mainly blamed for these rising statistics. The best way to prevent disease is to control the consumption of cholesterol. For example, 70 percent people in Finland have succeeded in controlling the disease. Dr. Zahid Jamal said that palpitation happens to normal and healthy people as well and drugs should be used carefully for this phenomenon. 1 in 5 No of women with some form cardiovascular disease 38% Percentage of women who have a heart attack and die within one year 40% Percentage of coronary events in women are fatal (Daily Times-B1, 27/01/2007) 12 Excess arsenic in water causes cancer: expert KARACHI, Jan 27: The estimate ratio of arsenic in water was 10 particles per billion (10 microgram per litre) in Pakistan, enough to cause various forms of cancer to one out of every 500 people, said Prof (Dr) Prosun Bhattacharaya, research leader and coordinator at the Royal Institute of Technology, Sweden, while referring to the study of Pakistan Council for Scientific and Industrial Research. While delivering a lecture on ‘Arsenic contamination in groundwater of South Asia and sustainable mitigation options’ at the geology department of Karachi University, he said arsenic was not just introduced into water through natural resources such as dissolution of minerals and ores and rock erosion but also by the industrial and organic waste, which used arsenic and its compounds as its basic ingredients. The lecture, aimed at creating a better understanding about the sources of arsenic as well as the ways to make its mitigation possible, was jointly organised by the KU geology department, Society of Economic Geologists and Mineral Technologists and the Association of Geoscientists for International Development. Dr Bhattacharaya pointed out it was the need of the hour to educate the masses about arsenic and the diseases caused by it. He emphasised that methods introduced to purify water should be easy so that the common man could adopt it. He said there were two ways to avoid arsenic pollution; one was treatment of contaminated water while the other was targeting safe water. At the end, Dr Viqar Hussain said research studies should be carried out to combat the water pollution problems. (Dawn-17, 28/01/2007) CHK, LGH fail to get promised funds KARACHI, Jan 27: The Board of Governors of the Civil Hospital and the Lyari General Hospital has demanded more funds and qualified staff for the two teaching hospitals. At its recent meeting, presided over by the Board’s Chairman, Abu Shamim M. Ariff, it was observed that under a declaration the Sindh chief minister had pledged that teaching hospitals of the province would get an amount of Rs1 billion collectively, but the authorities concerned were failing to fulfil the commitment. A source privy to the meeting said that under the CM’s special allocation, the two hospitals were supposed to get an amount of around Rs250 million for improving their overall working and undertake renovation and other physical development. The meeting urged the Sindh government to help get the long-awaited bloc-allocation as announced by the chief minister. In view of the long-standing ban on recruitment imposed by the Sindh government, the BoG decided to go for outsourcing its janitorial and sanitary services. Despite the fact that the BoG is completely an autonomous body that is also authorised to carry out appointments on grade-1 to grade-14 posts, no relevant development could be seen so far due to the ban, commented a BoG member. Now, the Board has decided that the janitorial/sanitary services would be given to some contractor, said an official communication. The meeting discussed the shortage of anaesthetics at the Lyari General Hospital, and demanded that the provincial health department be moved for the posting of qualified and trained anaesthetics at the hospital.The meeting was informed that with the induction of some more doctors, the treatment facilities at the hospital had improved considerably, but shortcomings still prevailed vis-a-vis the surgery and operation theatres in the absence of trained anaesthetics. At present, the hospital has six anaesthesia personnel and if it is provided with another 6-10 trained personnel, the OTs could be turned fully operational in three shifts, said another member. Those who attended the meeting included CHK MS Dr M. Kaleem Butt, LGH Dr Khwaja Mukhtar, Prof Younus Soomro, Dr Zafar and private members. The BoG thanked the Sindh health department for posting of more doctors made available through the Sindh Public Service Commission or the now-defunct school health services. It also thanked the government for the release or transfer of budget for maintenance and repairs. The meeting was also informed about the civil work contract for the Accident and Emergency Centre and Ancillary Service Complex, streamlining of internal audit system for CHK and LGH, and formulation of a system towards maintenance of all machineries and medical equipment procured by the government or donated by philanthropists. (Dawn-19, 28/01/2007) Ban on jobs, no funds make 62 health units inoperative KARACHI, Jan 27: As many as 62 health care units built by the city government have been lying inoperative mainly for want of staff, according to informed sources. These hospitals, clinics, rural health centres, urban health centres, maternity homes and dispensaries have been built over a couple of years or so in different towns of Karachi. However, due to shortage of funds and the longstanding ban on recruitment, the city government has failed to make the operational. A source in the city government’s health department said that construction work of all these units had almost been completed but owing to the ban on recruitment, no staff could have been appointed so far. He said that the authorities concerned were not approving the SNE (sanctioned new expenditures), obviously due to the ban and non-availability of the required funds. 13 It is learnt that at some stage, the SNEs for 19 of these unites had been endorsed by the city council but the specified reasons have rendered the city government helpless. Owing to the situation, people of the towns like, Shah Faisal, Malir, Orangi, Baldia, Gadap and Keamari, have remained deprived of the vital health care facilities which would, otherwise, have been available within or very close to their localities. Moreover, the health department requires at least 100 doctors and 300 paramedics, including nurses, dispensers, dressers, x-ray technicians and other laboratory staff, etc., for a good number of the health care units already functioning in different parts of the city. These units include the district council dispensaries. The source said that after appointment of doctors on a contract basis and posting of the doctors belonging to the nowdefunct school health programme, the treatment and other facilities at some of the 271 old health units being managed by the city government had improved considerably. It is further learnt that 45-50 of the old health units in different towns are either non-functional or under-utilised for various reasons, mainly non-availability of doctors and paramedics, medicines, equipment and furniture. When contacted, the EDO Health Dr A. D. Sajnani said that his department was making efforts towards fully reviving big hospitals, maternity homes and other such units. “We are also working for a full-fledged functioning of new health care facilities lying inoperative for want of staff and financial resources,” he added. He said he had recently reminded the relevant authorities of all the problems and, in turn, was assured that the provincial and city governments would look into the matter on a priority basis. “We will approach the provincial government for the allocation of special funds to the city government’s health department and relaxation in the ban on recruitment, particularly in the case of doctors,” he said, pointing out that many posts were lying vacant following retirement of personnel over years. (Dawn-17, 28/01/2007) Karachi AIDS patients went up 25% in 1 yr KARACHI: The percentage of AIDS patients in Karachi has increased from 0.4 percent to 26 percent between 2004 and 2005, Dr Sharaf Ali Shah said Saturday when local and foreign doctors showed different figures of alarmingly increasing infectious diseases in Pakistan during the second day of World Health Updates (WHU). “Six ministers and managers have been changed during a short span of two years. It is not possible to control a rampant disease under such conditions,” Shah said in reply to a question about corruption in this sector. The changes in the hierarchy of government officials and the payment of money by World Bank on strict conditions are major reasons why we have so far not been able to curb these diseases in Pakistan, he said. Around 20 million people get blood transfusions every year in the country; 20 percent of the blood is screened, while the remaining 80 percent could have viruses such as HIV and Hepatitis, Shah said, adding that the intervention rate is at a low five percent in the country. Sindh is especially vulnerable to the disease as people were flocking to the region from all parts of the country. “Injecting drug users, sex workers, truckers and prisoners move towards Sindh to earn,” he said. The first case of HIV in Pakistan was reported in 1986 and that was not an indigenous case. An indigenous case was detected in 1987. The prevalence of Hepatitis B and C was the highest in Pakistan. Sten H. Vermund, MH, PhD, from the United States, focused on emerging infection diseases. He said there is a possibility of the spread of Avian Influenza from human to human in the future. Three new types were found between 1997 to 2006; H5N1 in East Asia/Europe, H7N7 in the Netherlands, and H9N2 in Asia. Vermund warned that there were many diseases, which are emerging now, to which people are oblivious. He said that human behaviour, international travel, ecological factors, socio-political and economical factors, human enterprise and several other main factors affect emerging diseases. Annually, around 60 million people are infected with HIV/AIDS and 20 million people die from it. The disease infects 14,000 people daily. According to the World Bank, by 2010, 29 million of 45 million people with HIV/AIDS could be protected by effective prevention. However, he felt, the political will to curb the disease was lacking around the world. Vermund also warned that tuberculosis (TB) was resurging. He said that 8.85 million cases emerge annually out of which 1.7 million people die. In developing countries, 95% to 98% of TB patients die. TB cases in the low class and lower middle class are increasing but were declining in the high and upper middle class. He also said that the 40% of the world’s population was at risk of contracting malaria. He admonished the practise of discontinuing prevention and treatment when the disease was close to elimination. Vermund said that there are over five million drug addicts in Pakistan of which 60,000 are intravenous drug users. To avert the risk of a viral disease outbreak, he suggested that these sections of society be monitored. Control Safety Pakistan President Dr M Rafiq Khan focused on “Blood-Borne Viruses”. He said that, in Pakistan, Hepatitis B and C and HIV are the most common diseases caused by blood-borne viral infections and blood screening varies between institutions, countries, cities and regions. According to an unpublished report of the ratio of HIV infected people in Pakistan, one HIV patient was found in every 16,000 people in 1998. In 1999, the ratio was 1:9000, in 2000, it rose further to 1:4500, in 2001, it was 1:3000 and now, in 2006, the risk has increased to 1:1400. The figures were obtained by screening blood units of family donors and volunteers. 14 Sindh Medical College Associate Professor Dr Khursheed Hashim spoke on the topic, “Infection Control: why, when and how.” He opined that infection has a direct effect on the economy of the country. Half of infections around the world occur due to the unsafe water consumption. Around 80% of children around the world die due to unsafe water consumption. He gave the case of a girl who died from Typhoid, had undergone breast surgery two years before her death. He said that doctors here excel in surgery but not lacked the ability to deal with infectious diseases. He felt that local doctors could avert the spread of infection by beginning hand hygiene programs, properly disposing of all kinds of waste, taking standard precautions, being environmental friendly and by helping the Infection Control Society of Pakistan. Prof. Mughis Uddin Ahmed of the Department of Pathology (Microbiology) at the Karachi Medical and Dental College and ASH, informed the audience of the purpose, structure and functions of the Infection Control Committee. The committee would basically acquire education, perform surveillance, and research to prepare an infection control manual. Provincial Program Manager Dr Arshad Mehmood said that condoms are used in 63.9% of Pakistan, which is relatively low. (By Farhan Ahmed, Daily Times-B1, 28/01/2007) 49pc street children at high risk of HIV KARACHI, Jan 28: Various reports compiled by different child rights organisations suggest that renting children by the parents to gangs is becoming a common practice in the country with Karachi having ample contribution to the menace. These reports say these gangs use these children for beggary by paying specific amount to their parents and taking their share from the child’s earnings. “This menace is on the rise and the reason might be increasing poverty in the society,” Akhtar Hussain Baloch, regional manager of a private charity, Society for the Protection of the Rights of the Child (Sparc), told Dawn. Mr Baloch said that the gangs paid more money for a girl child than boys given the fact that girls attracted more attention of people for alms. According to him, reports such as this should come as no surprise when everyone is aware of the existence of child beggar racquets. “This nonetheless exasperates a situation where a child escapes the violent private domain to seek refuge in the sanctum of the public where all is visible, where indiscriminate violations are conducted less hastily for fear of reprise from the law,” he said. Mr Baloch said that such situations were increasing escapism among the children. They escape from a non-life of begging and abhorrent abuse at the hands of the adults of their society who are meant to protect them, he added. Referring to such reports, he said as early as four, these children beg and scavenge around rubbish dumps or industrial waste sites and took on menial jobs as cart-pushers or dishwashers working 12-15 hours a day to earn around Rs75 – enough to buy a meal. A report compiled by the Society for the Protection of the Rights of the Child (Sparc) said most children survive by prostituting themselves and stealing, making them vulnerable to contracting sexually transmitted diseases (STDs) such as HIV/AIDS. “They are also at high risk from health problems such as tuberculosis, jaundice and kidney disorders.” The report suggests that 83 per cent of street children were sniffing glue between the ages of eight to nineteen. Some 54 per cent left home at age 10-12 while 45 per cent children living on the streets are involved in crimes and 49 per cent are at high risk of HIV/AIDS. Mr Baloch referred to the United Nations Office on Drugs and Crime (UNODC) assertion that 72 per cent of all street children had no contact with and 10 per cent had no knowledge of their families. A large proportion of these children sniff cheap readily available glues to starve off hunger, loneliness and fear. He said some 35 laws pertaining to child rights existed in Pakistan but it seemed the authorities were doing a lot but to no avail. According to him, since independence successive governments had passed and promulgated 27 laws pertaining to child rights while eight laws existed already including the Female Infanticide Prevention Act of 1870. (By Hasan Mansoor, Dawn-14, 29/01/2007) Up to 7 out of 1,000 unsafe abortions end up in hospital in Pakistan KARACHI: Pakistan shares an annual hospitalization rate from unsafe abortions of 4-7 per 1,000 with Nigeria and the Philippines. This falls in the middle of the spectrum with Bangladesh at a low of about 3 per 1000 women to a high of about 15 per 1000 in Egypt and Uganda. Two countries in Latin America with recent data have rates of almost 9 per 1000. In a study that appeared in The Lancet in Nov 2006, national estimates of abortion-related hospital admissions in women aged 15-44 years were compiled for 13 developing countries. Complications from unsafe abortion are believed to account for the largest proportion of hospital admissions for gynaecological services in developing countries. The WHO estimates that one in eight pregnancy-related deaths result from unsafe abortions. In the developing world as a whole, an estimated five million women are admitted to hospital for treatment of complications from induced abortions each year. The WHO estimates that 68,000 unsafe abortion-related deaths occur annually; that about one in eight of all pregnancyrelated deaths result from unsafe induced abortion; that about 19 million unsafe abortions take place each year worldwide; and that abortions happen to women of all ages, throughout their reproductive years. Estimates have also been made of the disability burden of unsafe abortion (disabilityadjusted life years [DALYs]), integrating the loss of productive life resulting from both death and illness. These estimates show that unsafe abortion is responsible for the loss of about 5 million years of productive life, or 14% of all DALYs lost from pregnancy-related conditions. However, in view of the limitations of the 15 available evidence base and estimation methodologies, this burden has probably been greatly underestimated. For example, the effect on women who have complications but who do not seek or receive medical care is likely to be underestimated; the long-term impact of unsafe abortion on women’s health, through increased risks of infertility, fistula, and other sequelae, is also difficult to quantify. Although not included as part of the national estimate, exploratory interviews in Pakistan show that private facilities treat large numbers of women for post-abortion complications-31,000 annually in 72 surveyed facilities. The Egyptian study was designed to cover public-sector facilities only and did not obtain information on treatment in the private sector, but it is likely that some women are obtaining care for abortion complications from private facilities. In both these countries therefore, the number admitted to hospital for induced abortion has been underestimated. In the other 11 countries, these estimates include both the private and public sectors and are therefore reasonably complete. All the studies rely on data obtained between 1989 and 2003, with most from the late 1990s. South-central Asia: The rate is estimated to be 4 per 1000, based on data for Pakistan in 2002 (7 per 1000) for public hospitals only and for Bangladesh in 1995 (2.8 per 1000) for all facilities. Although no speci. c data are available for the rate of abortion-related hospitalisation in India (where abortion is legal under broad criteria), a 2002 study provides evidence of a continuing large number of unsafe procedures. Southeast Asia: The rate is estimated to be 3 per 1000, based on that for the Philippines in 2000 (4.4 per 1000), similar abortion provision in other countries of this sub-region (Indonesia, Thailand, Burma, and Laos),27 and safer conditions in countries where abortion is legal and accessible (particularly Vietnam). Western Asia: Little information on abortion complications exists for this region. The rate is assumed to be 8 per 1000, based on data for countries in neighbouring regions that are culturally and demographically similar: e.g., the estimated abortion hospitalisation rate of 7 per 1000 for Pakistan and the estimated rate of 15.3 per 1000 for Egypt, both for public hospitals only. The estimate also takes into account the fact that abortion is likely to be highly unsafe given the restrictive and clandestine context within which the procedure takes place, with the exception of Turkey. The annual rate of admission to hospital for treatment of complications from unsafe abortion varies from a low level in Bangladesh (just under 3 per 1000 women aged 15-44 years), to moderate levels in Mexico, Nigeria, and the Philippines (5-6 per 1000), to higher levels in the other nine countries (8-16 per 1000). The rates for Pakistan (7 per 1000) and Egypt (15.3 per 1000) are likely to be substantially underestimated since data from most private sector facilities were not available. The rates in Egypt and Uganda are the highest of the 13 countries, at just over 15 per 1000 women. In Peru and the Philippines, information on abortion trends is available because estimates have been made for 1989-1998 and 19942000, respectively, using comparable methodologies. In both countries, the abortion rate changed little, but the rate of admission to hospital for complications fell. In each country, access to safer abortion methods (particularly misoprostol-only abortions) and to better-trained health-care providers improved over time and contributed to a reduction in the proportion of women admitted to hospital after an unsafe abortion. In Peru, the rate dropped from an estimated 10.9 per 1000 to 8.6 (an annual fall of 2.3%), while in the Philippines, the rate fell from 5.1 per 1000 to 4.4. One important change has been increased use of the drug misoprostol which, when administered clinically, is highly effective although when self-administered and less closely monitored is less effective, and could result in the need for hospitalisation). This change began around 1990 in some Latin American and Caribbean countries, and has since expanded to other countries in this region. Misoprostol is beginning to be used in parts of Asia and increasingly in sub Saharan Africa, although it still accounts for a small part of abortion service provision. Increased use of this has resulted in less frequent use of the most harmful methods of unsafe abortion such as the insertion of solid objects and use (oral or vaginal) of caustic or otherwise damaging substances (including some based on herbs and plants). Overall, increased use of the drug especially by well-trained individuals is expected to lower abortion mortality and to reduce severe morbidity. However, the numbers of abortion-related hospitalizations might fall much more slowly than the rates: in Peru and the Philippines, the number fell by 0.8% and 0.4% per year, respectively, compared with a drop of 0.3% per year in the rate in each country. The introduction of misoprostol is one of the most significant factors accounting for declines in the severity of abortion complications and in the hospitalisation rate in recent years. However, factors that counter these trends include the practice of health-care providers encouraging women who use misoprostol to attend a clinic for the abortion procedure, and the effect of long-term campaigns by women’s health advocates that lead to increased willingness of hospitals and healthcare providers to treat incomplete abortions, and to a lessening in women’s fears of seeking care. Nevertheless, unsafe abortion in the second trimester continues to be the source of serious complications since it still accounts for a substantial proportion of women admitted to hospital for induced abortion complications in some countries, for example in Kenya and Nigeria. The evidence shows that the health burden of unsafe abortion is large. Even so, rates of hospitalization underestimate the true burden because a large proportion of women with abortion complications do not obtain medical care. Surveys of key informants in all three major regions of the world suggest that an additional 15-25% of all women undergoing abortions have complications but do not obtain the necessary healthcare. (Daily Times-B1, 29/01/2007) 16 FEBRUARY Injury that brings shame: giving back their dignity KARACHI: Sakina was married before she reached adolescence, perhaps 12 or 13, but her marriage was not consummated till she was ready to conceive at 15. Three pregnancies followed of which two ended in miscarriages leaving her with an injury that caused her “to leak stools and urine”. She had developed what doctors call obstetric fistula and began to suffer silently and in shame. She was then sent to her mother by her in-laws. A preventable and treatable condition, fistula is caused by prolonged labour, explains Dr Shershah Syed, a leading gynaecologist. “The pressure caused by the baby’s head against the lining of the birth canal perforates the wall of the rectum and bladder leaving the mother unable to control her excretory functions.” The woman becomes incontinent causing unimaginable psychological trauma and social ostracism. He has seen scores of women who were abandoned by their husbands or become outcasts. Skina’s fistula was repaired recently, free of charge at Koohi Goth Maternity Centre. The man behind this centre, with squeaky clean wards and a cheerful ambience for the really poor, 12 kms from the city centre is Dr Syed himself. The centre is located within the confines of a katchi abadi in Malir. For well over a decade, he and his team of doctors have been organising free camps all over remote Pakistan for women having obstetric and gynecological problems. Fistula was one of the disabilities he noticed increasingly women complain of. To stop fistula from occurring, there is need for bringing change in certain risky traditional practices. Foremost, is stopping child marriages and delaying the age of first pregnancy. Along with that access to timely emergency obstetric care (EmOC) is as important. In January 2006, the UNFPA launched a national campaign to end fistula in Pakistan. Seven regional centres -- at Karachi, Islamabad, Multan, Quetta, Larkana, Lahore and Peshawar – were set up where repair of fistula is carried out free. Koohi Goth is one, where since March 2006, 86 successful procedures have been done. The biggest hurdle in getting the women to come to the centre is men, according to Dr Ayesha Haq, who works at the centre. ''Although we provide free transport, treatment, accommodation and food, men are unwilling to let their women live away from home for extended periods.” The procedures may sometimes take months, even as long as six months where multiple injuries need to be closed. (By Zofeen T. Ebrahim, Dawn-18, 03/02/2007) We weren’t consulted over new private hospital law: PMA KARACHI: The Pakistan Medical Association (PMA), Karachi and the College of Family Medicine, Pakistan denounced the approval of the private hospitals/clinic regulatory ordinance in a press conference Friday. "We are not against the regularisation of private hospitals and clinics. What we are opposing is that the main stakeholders were not consulted for its approval," said Dr Qaisar Sajjad, PMA Karachi's honorary general secretary, while speaking at the conference. Innumerable problems existed in government hospitals and the government should concentrate on solving them rather than stepping into the private sector without consulting the doctors or owners of these private hospitals. Sajjad was concerned that the revised draft ordinance that was approved by the chief minister without the consulting the PMA and the College of Family Medicine who were not included in the committee formed for the ordinance. "When the government was in contact with the PMA, we being the sole representative body of the medical profession, took initiative and organised several brain-storming sessions," he said. Several queries were raised in these meetings and the formulation of standardised regulations for all private health entities were agreed upon. He said that the former Sindh health minister had also called a meeting but nothing was done despite repeated verbal and written requests to the health department. He said that the PMA has never been against licensing private hospitals, clinics and laboratories, however it believes that the government should first form strong legislation against all types of quackery. Secondly, he said, the standard of laboratories and blood banks in government hospitals needed to be improved. The problems of doctors and paramedical staff should also be solved. The recent implementation of the new service structure for doctors in the Punjab should immediately be implemented in Sindh and other provinces. College of Family Medicine secretary general Dr Aziz Khan Tank echoed these views and said, "We have not heard anything about the ordinance since 2005. It would be totally undemocratic as it would be promulgated without being presented in the assembly." He said that the family medicine sector provided one of the biggest services and yet, the government had not consulted them. "Our general practitioner system is the cheapest in the entire world as it costs less that a dollar," he said. "There is a difference between rural and urban general practitioners and the government has formulated the ordinance without sorting out their differences and problems and neither were the owners of community hospitals and homeopathic practitioners consulted." They demanded that the draft ordinance be reconstituted before being promulgated so that authentic rules were framed with consultation from all stakeholders, including reputed people from the civil society, judges, advocates and journalists. (Daily Times-B1, 03/02/2007) Doctors in the dark about new laws KARACHI: A majority of doctors is unaware about the licensing authority ordinance, which is soon to be promulgated by the government to regulate private hospitals and clinics. An “amended” draft of the ‘Private Hospitals Accreditation and Licensing Authority’ was recently approved by the governor and sent to the provincial law department that will formally issue it in the shape of an ordinance, official sources told Daily Times last Saturday. 17 While more than half of the doctors, many senior practitioners, Daily Times contacted were unaware about these new laws they did have strong opinions about the state of affairs. “The government should establish an autonomous and independent body, funded by all the hospitals,” recommended Prof Rasheed Jooma, adding that this ordinance should be promulgated as similar ones had been successfully formed in the Punjab. “Government hospitals need monitoring to ensure staff attendance,” said Dr Hayat, a pediatrician at Abbasi Shaheed Hospital. He believed that private hospitals should be monitored as “they are employing less qualified doctors for meager amounts.” ASH medical officer A Hashmi, who said that all private hospitals had gone commercial and there was no check on their performances. He said that private hospitals pressured doctors into creating huge profits by overcharging. The government should involve private practitioners in making rules to regulate medical stores, but not in the formulation of the ordinance, he said. Dr Matiur Rehman, a private practitioner in Askari 4, said that the ordinance was more about registration rather than regulation, and the government had only taken this step to calm people who had long been complaining about private establishments. “This law will not necessarily work as registering all hospitals and clinics in the city is very difficult,” he added. JPMC’s Dr Aleem Kadar fully supported the ordinance. “There is a certain chance of rivalry, because here, people often use their positions for personal conflicts hence professional people should be on the regulatory board,” he said. (By Farhan Ahmed, Daily Times-B1, 04/02/2007) Gutka makers arrested KARACHI, Feb 4: The Sharafi Goth police on Sunday raided a house in Mansehra Colony and arrested four men on the charges of making Gutka, a hazardous stuff which has been formally banned by the government, said a police official. “We got reports that some people involved in Gutka-making have changed their location from some other part of the city and started their activity in Mansehra Colony at which we conducted a raid,” said Malik Ishaq, SHO of Sharafi Goth Police Station. During the raid, police recovered 5,000 Gutka sachets and impounded the entire raw and packing material, he said. The arrested men were identified as Kamran, Waqas, Naeem and Kamran Saeed. (Dawn-15, 05/02/2007) PMA questions JPMC plaza construction KARACHI: The Pakistan Medical Association (PMA) expressed concern on Monday over the federal health ministry’s plan to construct a 13-storey plaza on the premises of Jinnah Post-Graduate Medical Centre (JPMC) at a cost of Rs 3.6 billion. Addressing a press conference at PMA House Karachi, PMA Secretary General Dr Habib-ur-Rehman Soomro said that the federal government decided to construct this plaza without considering the requirements of the hospital, the needs of patients, the environmental impact, or the utility of government buildings in Karachi. “The federal health ministry in collaboration with big businessmen and the builders mafia, is planning to build a shopping plaza and a five-star hotel on JPMC land after the Elite Plaza is completed,” Soomro said. The JPMC originally had 62 acres of prime land for a postgraduate centre. However, more than 18 acres of this land is presently part of a katchi abadi. A big chunk of this had been allotted by the federal government for the construction of a hotel. Soomro said that it was very distressing that the government did not conduct any public inquiry and environmental study before starting the construction of the plaza. Instead of horizontal development of the hospital in the entire 62 acres, powerful people in the ministry were minting money at the cost of the people of Karachi, he said. Soomro demanded that the City District Government Karachi (CDGK) and KBCA authorities stop the construction of the plaza. The PMA secretary general also expressed concern over the isolation of the Sindh Medical College (SMC) from JPMC. He said that SMC students were no longer welcome in JPMC because of the “policies of the Dow University of Health Science (DUHS).” He said that the vice chancellor and his team was only interested in constructing buildings on the DMC and JPMC premises and had totally failed in organizing medical education at SMC. Clinical classes of SMC students were not being conducted for the past two years and medical education was in shambles. Soomro demanded that PMDC take notice of the present system of education at SMC and compel health department to provide the required faculty. He further said that Sindh government hospitals in New Karachi, Liaquatabad, Korangi and Saudabad should be affiliated with SMC, and all doctors with FCPS Diploma at these hospitals should also be given faculty status as per a previous decision of the health department. Online adds: It is to be mentioned here that the federal government had planned to build two medical towers in the country to cater to the health needs of the affluent. The construction of the first of the two elitist medical towers has been started. The prime minister inaugurated the construction within the premises of PIMS Hospital, Islamabad, on January 23. The project will cost Rs 2 billion. (Daily Times-B1, 06/02/2007) 18 Rs70m ISD project in final stage KARACHI, Feb 9: The up-gradation of the Institute of Skin Diseases has entered its final stages and work is expected to be completed in two months. The unique features of the Rs70 million project comprise a state-of-the-art allergy centre, two separate clinics for Sexually Transmitted Diseases, clinics dealing with HIV/Aids and leprosy patients, a library and a small auditorium. The director of the institute, Dr Sikander Azam Mahar, said the project was unique as the country had only one allergy centre operating in Islamabad. The institute’s STD clinic, the only one in Pakistan with a lab facility, would be improved, he said. “We are making a new lab and purchasing latest machines which are not available anywhere in the country for the treatment of skin ailments. On average 5,000 patients report daily at the OPD. Of them, over 1,000 patients come with allergy complaints. Right now, it’s hard to make the right diagnosis since the institute lacks modern lab facilities. A state-ofthe-art allergy centre would fill this gap and patients would receive appropriate treatment,” he said. The entire building is being renovated and the new computerised system will be in place soon. After the makeover, the institute will have a micro-drum abrasion machine for acne treatment, facilities for cryotherapy and electro-cauterisation to treat skin growths and photo-chemotherapy (puva) to treat white patches on the skin. Dr Sikander said that the project was the result of his 20-year-long association with Professor Dr Adeebul Hasan Rizvi, who he said, was doing a great service to the nation. One of the oldest skin hospitals in the country, the 50-bed Institute of Skin Diseases, is being refurbished and upgraded with the support of Sindh government and philanthropists. It receives patients from all over the country and also from Afghanistan. They are provided with medicines and treatment free of cost. Earlier called the Skin and Social Centre, the institute started off as an STD clinic in 1940s for sailors and later turned into a full-fledged skin hospital. Of 64 doctors working there, 34 are skin specialists. The institute also provides diploma and postgraduate training, which is at the moment stands suspended due to renovation. (Dawn-18, 10/02/2007) The burden of cardiovascular diseases AT the beginning of the 20th century, cardiovascular diseases (CVDs) were responsible for less the 10 per cent of deaths worldwide. Today they account for 30 per cent of the total global mortality. The matter of concern is that 80 per cent of this mortality now takes place in the developing countries, most of it in South Asia. According to the World Health Organisation (WHO), in 2001 CVDs were the number one cause of death worldwide, and the situation remains the same to date. South Asia, with 1.4 billion inhabitants, is home to one-fifth of the total global population. This region, historically known as the Indian subcontinent, comprises India, Pakistan, Bangladesh, Nepal, and the Maldives. It is also called the Saarc region. More than half of its population lives below the poverty line. The extremes of poverty and affluence are a characteristic feature of the region where a section of the population is aging and has a high CV mortality rate. Validated national estimates of the cause of specific mortality are not available in any country of this region. The available data is based on combinations of different data sets. In the Urban setting the cause of death is extrapolated from death certificates issued by hospitals, while in the rural setting the surveys of the cause of death provide the necessary information. Limited epidemiological data exists in various quarters in the region. International agencies, including the WHO, have a clear idea about the extent of the CV disease burden in South Asia. Studies conducted on South Asian migrants in the West show that they have higher CV mortality compared to the reference native population. In 2003, the prevalence of the Coronary Heart Disease (CHD) in India was three to four per cent (in the rural areas – twofold higher compared to 40 years ago) and eight to 10 pre cent in the urban areas –six-fold higher compared to 40 years ago). This amounts to 29.8 million affected (14.1 in rural and 15.7 million in urban areas). This is based on population cross sectional studies which are comparable to 31. 8 million affected derived from the extrapolation of the global burden of the disease study. These numbers are likely to be underestimated as they do not account for those with silent myocardial infarction or asymptamatic CHD. Deaths from CHD in India rose from 1.17 million in 1990 to 1.59 million in 2000 and are expected to rise to 2.03 million by 2010. CVD accounted for seven per cent deaths in Nepal and 40 per cent in the Maldives in 1998. The National Health Survey of Pakistan (1990-94) has revealed that circulatory diseases (heart attacks and strokes) account for 12 per cent of the total mortality with over 100,000 deaths annually. In addition to the high rate of CHD mortality, the other alarming feature is the younger age of individuals falling victim to CHD in South Asia. The disease manifests almost 10 years earlier on an average in South Asia compared to the rest of the world. As a result our region suffers a tremendous loss of productive working years due to CV deaths. An estimated 9.2 million productive years were lost in India alone in 2000. This will be increased to 17.9 million productive working years by 2030 -- almost 10 times that of the US. Currently, morbidity and disability related to major non-communicable diseases (hypertension, diabetes mellitus, hyperlipidemia, obesity and smoking) account for 60 per cent all deaths and 47 per cent of the global burden of the disease. These rates are expected to rise. It is projected that 89 million will die of CV Disease in our region in the next 10 years. Sixty million such deaths are likely to take place in India alone. RISK FACTORS: Though the exact cause of CHD is not fully known, the risk factors predisposing the individual as well as the community to CHD are well established. These risk factors have been the focus of interest and extensively studied. They are the following: 19 1. Hypertension Hypertension is the commonest chronic disease in South Asia, just like in the rest of the world. Globally about 20 per cent population is affected with this disease. The prevalence is high in South Asia. Hypertension is prevalent 20 to 40 per cent in urban and 12-17 per cent in rural adults and was affecting an estimated 118 million inhabitants in India in 2000. This number is projected to almost double to 214 million in 2025. Similarly, the 1990-1994 National Health Survey of Pakistan revealed that one-third of the Pakistan population over the age of 45 had hypertension and 18 per cent of the subjects over the age of 15 fell into the hypertensive range. There are an estimated 14 million hypertensive in Pakistan. Hypertension is especially common in urban obese females. Similar trends are found in Bangladesh. In Sri Lanka the prevalence is some what lower. 2. Diabetes mellitus The prevalence of diabetes and its adverse health effects have risen more rapidly in South Asia than in any other region of the world. India has a higher number of people with diabetes than any other country, with estimates ranging from 19.4 million in 1995 to 32.7 million in 2000. In Bangladesh, the prevalence of diabetes in the urban areas is double that in the rural areas (eight per cent v four per cent) and increases with affluence. The International Diabetes Federation (IDF) gives an estimate of 12 per cent prevalence in Pakistan, with a total of 8.8 million people with diabetes in 2002. In Sri Lanka, the 1999 census report records diabetes prevalence as eight per cent in the rural areas and 12 per cent in the urban areas. The projections for 2020, based on modelled estimates by the WHO, show a marked escalation of diabetes-related burden in South Asia. The number of people with diabetes is expected to rise by 195 per cent in India between 1995 and 2025 to reach 57.2 million in 2025. Pakistan is expected to have about 14.5 million people with diabetes by that year, becoming the 5th largest diabetic nation of the world. 3 Dyslipidaemia The relationship of hypercholestrolaemia with the incidence of CHD is well established. The south Indian population suffers from what is best called dyslipidaemia. The distinctive dyslipidaemic pattern of reduced concentrations of high density liporotein (HDL) cholesterol and high concentrations of triglycerides characterise the metabolic profile, and abdominal obesity charactrises the phenotype of the urban adult in South Asia. The low levels of HDL cholesterol result in dangerously high ratios of total cholesterol to HDL cholesterol, even at concentrations of total cholesterol that would be considered acceptable in western populations. HDL cholesterol ratios of >4.5 exist in 73 per cent of urban men and 54 pre cent of urban women and in 52 per cent of both rural men and rural women; these men and women have total cholesterol values in the range of 4.7 mmo1/1 to 5.2mmo1/1. 4. Cigarette smoking In 2002, a national survey of tobacco use reported that the Indian subcontinent, second only to China in both production and consumption of tobacco products, had an alarming rate of current tobacco use of 56 per cent among Indian men between the ages 12 and 60. In a survey of sixth and eighth graders attending school the prevalence of tobacco use (any history of use or current use) was two to three times higher among sixth graders compared with eighth graders, suggesting a distrubing new wave of smoking among India’s youth that forebodes serious future public health consequences for the Indian subcontinent. Similar trends are present in Pakistan and Bangladesh. Unfortunately, the poor and the young are especially vulnerable to this menace. 5. Physical activity A recent hospital-based cases control study from two urban centres in India suggested that daily moderate intensity physical activity (for example, the equivalent of brisk walking 35 to 40 min per day) is associated with a 55 per cent lower risk of CHD. It has been seen that the prevalence of leisure time physical activity was substantially lower among South Asians (6.1 per cent of control arm patients) compared with the rest of the world (21.6 per cent). 6. Chronic kidney diseases Concomitant with the rise in the prevalence of diabetes and hypertension is an increase in the prevalence of chronic kidney diseases, also recognised as an independent risk factor for CHD. A study from Pakistan reported a prevalence of 15-20 per cent of impaired kidney function among people of 40 years of age or older. Data from India suggest a prevalence of chronic kidney disease of 0.8-1.4 per cent in the urban areas. CONCLUSION: The exact data regarding the above-mentioned problems is not available in South Asia, therefore their exact magnitude cannot be estimated; but the available evidence suggests that the burden of CVD is rising and is definitely a serious threat to the health resources and socio-economic growth of our region. The health burdens of non-communicable diseases are high in South Asia, though there are differences among countries and within urban and rural areas of each country, depending on the level of developmental and epidemiological transition. Many of these disease burdens occur in the productive mid-life period and will, therefore, adversely affect workforce productivity and economic development. The main obstacles to dealing with this challenge include illiteracy, extreme poverty, the lack of political will, myths and taboos and the widening gap between the rich and the poor. (By Prof. Muhammad Ishaq, Dawn-The Magazine-5, 11/02/2007) ‘Smoking, environmental pollution trigger asthma’ KARACHI: While environmental allergins (pollen, indoor/outdoor fungi) excessive exposure to chemicals (occupational hazards), excessive drug use like a profuse intake of aspirin, are the main causes of asthma, factors like smoking (especially second-hand smoking whereby one is condemned to inhale the smoke generated by another smoker) and environmental pollution exacerbate the disorder. Other catalysts of the disease are emotional stress and excessive atmospheric humidity. This information on the disease was imparted by Dr Saleemullah, Consultant at the Abbasi Shaheed Hospital, Karachi. The lecture, titled “Asthma”, was held under the joint aegis of the Health Awareness Society and the Distinguished Secretaries Society of Pakistan (DSSP) at a local hotel Saturday evening. Dr Saleemullah said that asthma was as neglected as it was common. 20 He said that the biggest hurdle to proper treatment was the fact that many people did not like to disclose or own that they had the disorder. It was treated as some kind of a stigma. Quoting global figures, he said that 300 million people across the world were afflicted with the disorder with 180 million deaths annually. It was feared, he said, that this figure would rise by 20 percent over the next ten years. Quoting the findings of a research study conducted in 2002, he said that the overall prevalence of the disease in Pakistan was 5 percent of the population, with Multan having the second largest number of cases after Karachi. Of these 5 percent, he said, five percent were children. On account of the disorder, children missed school for days at a stretch affecting their learning process and examination results while adults had to miss work whereby thousands of man-hours of work were lost, resulting in major economic losses to the country and society. This was a major impediment to national productivity, he said. Among the sufferers, he said, 74 percent of the adults and 67 percent of the children took their condition for granted, adding that a lack of education and lack of awareness reflective of the state’s apathy, were to blame here. Another result of the lack of education and awareness, he said, was that 87 percent of adults and 88 percent of the children had no knowledge of inhaled cortisteroids which otherwise was a highly effective treatment. Another 53 to 55 percent of the children were embarrassed to admit that they were suffering from the disorder. He said a major hurdle to countering the disorder on a national scale was the fact that often people concealed the fact that they were suffering from the disorder. It was a kind of a social stigma. This attitude, he said, was highly unwarranted as it is nothing to be ashamed of or embarrassed by. True there is no long-term cure for it but it can be very easily controlled and it just need not be a lifethreatening or terminal disorder. There are two kinds of medicines to treat the disorder, namely, controllers and relievers. Total control over the disease, he said, could be achieved among 70 percent of the affected population. All symptoms, like sleep disturbances resulting from the disorder, he said, could be easily countered. Cheryl Matthews of the DSSP and Dr Saima conducted the proceedings. (By Anil Datta, The News-4, 11/02/2007) Drug prices and healthcare THE Patent Act, 2005, which was approved by the Indian Parliament, has been a contentious piece of legislation, opposed by many activists, who have accused the government of giving in to the international pharmaceuticals lobby. The act ensures that India meets its World Trade Organisation (WTO) obligations under the agreement on Trade Related Aspects of Intellectual Property Rights (TRIPS). The act provides patent protection for the actual product — the pharmaceutical composition — rather than for the process of making it. Before the Act came into force, India’s generic-drug makers had ensured the supply of low-cost alternatives to expensive branded drugs, to patients not just in India, but in several developing — and increasingly, even the developed — countries. Indian firms supply almost 85 per cent of the AIDS drugs that the international health NGO, Medecins Sans Frontieres (MSN, in French, or Doctors Without Borders) uses to treat 60,000 HIV patients in about 30 countries. Interestingly, the Indian Patent Act has now come under the assault of an international drug major, Novartis, which has filed an appeal in the Madras High Court, challenging the rejection of its patent application for the leukemia drug Gleevec (imatinib mesylate) by the patent office in the southern Indian city. The patent office in Chennai has rejected the application on the grounds that it was a new form of a known substance; the act says that a patent can be granted only for a truly innovative advance, and not for ‘evergreening,’ which is basically an attempt to patent minor or frivolous improvements in a drug. Novartis has asked the high court to strike down the specific section as inconsistent with WTO’s TRIPS agreement. The Swiss multinational’s bid to challenge the section questioning ‘evergreening’ or ‘frivolous patents’ has evoked anger among international healthcare activists, who claim that if Novartis’ appeal is upheld, Indian generic firms may be prohibited from producing cheaper versions of the drug. Patients have to spend about $2,500 for a month’s course of Gleevec, whereas Indian generic makers sell the drug at onetenth the price, the activists argue. MSN had urged the European Parliament to investigate the matter, and some members of the European Parliament (MEPs) have called on the parliament’s health committee to seek “civil society action against Novartis.” The Swiss multinational is also being sued by Mumbai-based Cancer Patient Aids Association, which has demanded damages from the company, following an article written by its chief executive, accusing generic companies of possibly funding opposition by patient groups in India. Novartis, which has not faced opposition elsewhere in the world, has assured South African Aids activists that its move to challenge the Indian Patent Act will not affect their access to cheap generic drugs from India. ***** INDIA’S generics-drug makers have been in the news for all of 2006 following their aggressive acquisition of firms in Europe and North America. The country’s largest drug-maker, Ranbaxy Laboratories, bought eight foreign companies, including Romania’s Terapia, for which it paid $324 million. 21 Ranbaxy is now in the race to acquire the generics business of Germany’s Merck, which has been valued at around $5 billion. The Indian firm will achieve a turnover of $5 billion in only about five years, but is making huge acquisitions abroad. Two other top Indian pharmaceutical companies – Cipla and Dr Reddy’s Laboratory (DRL) – are also interested in acquiring Merck’s generics business. DRL has also been picking up a lot of European firms of late. The Hyderabad-based company paid $570 million for Germany’s fourth largest generics company, Betapharm. It also paid nearly $60 million for the Mexican active pharmaceutical ingredients (API) business of Roche, a Swiss multinational. According to Dr Anji Reddy, chairman, DRL, all these are part of its strategic initiative to emerge as a mid-sized global pharmaceutical company. Nicholas Piramal India Ltd (NPIL), a Mumbai drugs major, bought a unit of Pfizer’s based in the UK, a few months ago. NPIL’s chairman, Ajay Piramal, says the company is now planning to acquire firms in the US, and is willing to invest up to $200 million for a unit. The company is now among the top-10 pharmaceutical outsourcing companies in the world, and in about two years, custom manufacturing will add up to about half of its revenues. Sun Pharmaceuticals, another mid-sized Indian drugs company, is also eyeing the US market, and has kept apart half a billion dollars for overseas acquisitions. The company, which has seen 30 per cent growth, hopes to sell about $100 million worth of drugs in the US every year. Another Indian company, Unichem Laboratories, is investing about $25 million in a Brazilian pharma firm, and also plans to acquire companies in Europe. Bangalore-based Kemwell, recently bought a Pfizer plant based in Sweden. Subhash Bagaria, chairman and managing director, Kemwell, notes that the company will widen its pharmaceutical business by making strategic global acquisitions. Indian pharmaceutical companies are expanding their custom manufacturing business, as the sector is experiencing phenomenal growth. Industry analysts estimate that contract manufacturing and research services is likely to expand into a $170 billion business in just two years, and Indian and Chinese companies could account for about 40 per cent of the outsourced market for APIs, finished dosage formulations and intermediates. The pharmaceutical sector in India accounted for the bulk of both inbound and outbound mergers and acquisitions (M&A), worth about $2.2 billion. The largest was the $736 million acquisition of Indian firm Matrix Laboratories, by Mylan Labs of the US. ***** INTERNATIONALLY, the pharmaceutical industry is facing many problems. The cost of bringing out a new drug has become prohibitive. It ranges from $500 million to $2 billion. Blockbuster drugs – ones that fetch over a billion dollars in revenue every year – are also becoming difficult to churn out. The big drug multinationals are facing a lot of flak from activists and even governments. Many countries are facing a crisis on the healthcare front, as their costs are soaring. Margins in the industry are facing a huge squeeze, as governments, insurance companies and consumers are refusing to pay more. Consequently, many international firms are going in for contract research and manufacturing (CRAM), outsourcing tasks to contract research organisations (CROs). Indian CRAM and CRO units are reaping a rich harvest, as they take up assignments on behalf of international drug makers. The Indian pharmaceutical industry has been growing at a compound annual growth rate (CAGR) of 13.6 per cent. Revenues by 2010 will add up to $12 billion, and exports will account for half of it. Indian drug companies are aggressively expanding in the US and other markets. About 100 pharmaceutical plants in India have been granted approval by the US Food and Drugs Administration (FDA), the largest number for any country. Indian companies have also filed the largest number of Drug Master Filings with the FDA, adding up to almost 30 per cent. They also account for the largest number of patents approved by the FDA for marketing of drugs in the US. India’s pharmaceutical industry is strong in generics, and this is one of the fastest growing segments in the drug sector. Generics account for a fifth of the $300 billion international drug business. With nearly 35 top branded prescription drugs likely to go off patent over the next couple of years, the generics business is expected to double. But Indian companies are also focussed on research and development, and R&D budgets are soaring. About $250 million is being invested in research, and the figure is expected to cross the $1 billion-mark in just around eight years. International majors are also outsourcing research activities to Indian firms, as the costs here are significantly lower. Frost & Sullivan, an international consultancy, estimates that about $1.2 billion worth of outsourcing of drug discovery to India is taking place currently. An additional $1.6 billion is being outsourced for clinical development in India, which includes clinical research, clinical trial management, and statistical analysis. Another growth sector for the Indian industry is the emergence of bio-generics, and many of the top biotech firms have started acquiring rivals in the US and Europe. Last week, Reliance Life Sciences — part of the Mukesh Ambani controlled Reliance group — announced the acquisition of GeneMedix of the UK for $63 million. (By Anand Kumar, Dawn-Economic & Business Review, Page-V, 12/02/2007) 22 Strict ban on smoking in offices likely KARACHI, Feb 10: The Sindh government has decided to activate its task force on curbing smoking to ensure “strict implementation of prohibition of smoking at public places and transports”, said sources in the Sindh health department. It is learnt that the chairman of the task force (health secretary) has convened a meeting of high-ups from various government departments and agencies, as well as private sector representatives on February 15. Chest physicians, pathologists, ENT specialists and members of medical practitioners’ bodies and the civil society forums have long been voicing their concern over the increasing trend of smoking. They call for discourage smokers, particularly children and teenagers. They believe that using tobacco in any form or disguise is dangerous to the health. The ‘Prohibition of Smoking and Protection of Non-smokers’ Health Ordinance’ was promulgated in the country in 2002 under which smoking at places of work or in public service vehicles was banned. The aim was minimising the effects of smoking on non-smokers’ health. The February 15 meeting will look into the matter of smoking at public places and suggest measures to ensure that all offices and establishment displayed board/banner inscribed with words: ‘No-smoking Zone’ and ‘Smoking is an Offence’ or ‘Smoking is Prohibited by Law’. The meeting will also review the progress of the implementation of the ordinance and take appropriate measures to create public awareness through workshops, conferences, symposiums and publicity through press and electronic media, besides suggesting different campaigns on the issue, the source said. PMA CONCERNED: The Pakistan Medical Association, Karachi, has expressed concern over the opening of two lounges dedicated for smoking at the Parliament House, Islamabad. In a statement, PMA General Secretary S. M. Qaiser Sajjad said the federal government had imposed a ban on smoking at all public places but it could not be observed or implemented in a true sense as yet. He demanded an immediate halt to the creation of smoking lounges at the Parliament House, and called for an effective ban on smoking during duty hours at all government offices, hospitals and concerns. (Dawn-15, 12/02/2007) 36-bed hospital in Surjani KARACHI: A 36-bed hospital had been completed in a two-year duration in Surjani Town with all major departments, and residents of Surjani, Khuda Ki Basti, Manghopir, Lyari Expressway and adjoining areas will benefit from medical facilities near their homes, said Sindh Minister for Local Government, Katchi Abadis and Spatial Development Muhammad Hussain Khan, while addressing the annual parent-teacher convocation of the Brooks Education System, Surjani Town, on Monday. Hussain, who is also the MPA from this constituency, said that the revival of the Surjani Town project and posting of a separate project director for the housing scheme would prove vital in accelerating the pace of development of the project. Primary schools for both girls and boys were being established in every sector of the town. The building of the Boys Degree College has been constructed while the one for girls will be established very soon." Projects worth Rs 55 million were underway and 90 percent of the town's sectors had been provided potable water. A separate water reservoir is almost complete, which will ensure continuous water supply and release the extra burden on Khawaja Ajmer Nagri pumping station. (Daily Times-B1, 13/02/2007) Smoking ban to be strictly enforced KARACHI, Feb 15: Provincial government’s anti-smoking task force on Thursday resolved that there would be a complete ban on sale of cigarette in areas surrounding educational institutions. In a meeting, the committee comprising senior representatives of various government departments and agencies decided that efforts would also be made curb smoking in intra-city public buses at the earliest. Sindh Task Force for the Implementation of Prohibition of Smoking and Protection of Non-Smokers Health Ordinance, 2002, met with provincial secretary for the Health department, Dr Noshad A. Shaikh, in the chair and discussed ways to eliminate smoking and other tobacco uses in places of public work and public service vehicles and to protect the health of non-smokers. The meeting was told that unless concerted efforts, with the support of senior government officials, were made a significant success could hardly be achieved, said a source privy to the meeting. In line with the ordinance in question, the task force decided that no person shall himself or by any person on his behalf, store, sell or distribute cigarettes or any other such smoking substances within an area of 50 meters from any college, schools or educational institution. The CCPO and other senior officials would be urged to cooperate in the implementation of the decision and further ensure that persons below 18 were not sold cigarettes. While observing that no-smoking was being exercised in intra-city public vehicles, the participants of the meeting stressed the need for prohibiting smoking in buses and other modes of public transport. It was also decided that government medical superintendents, heads of all medical care facilities down to the BHU level should ensure complete implementation of the anti-smoking ordinance in their respective jurisdictions. Secretaries and heads of various government departments and offices were also urged to ensure that 2002 ordinance was not contravened in the Sindh secretariat and other government offices. If needed, some zone or section could be reserved 23 for smokers in the departments, the source added, saying that government officers concerned should also arrange for separate smoking corners in hotels and restaurants. It was further decided that some sort of literature highlighting the adverse impacts of smoking would also be prepared and distributed among the students with the collaboration of the Sindh education department, while on the other hand the Sindh Information department would also be urged to ensure that any advertisement pertaining to cigarette smoking did not appear on the electronic media in a duration other than 12 midnight to 6pm. The meeting was attended by senior officials of the home, education, law, information and transport departments, local governments, and representatives from the PMA, the pharmaceutical sector and the CAA and senior officials of the health department, including Dr Shakeel A. Mullick. It was also decided at the meeting that the CCPO and one representative each from the PMA and the transporters association should be co-opted in the 14-member task force. Discussing measures required under the 2002 anti-smoking ordinance, the meeting called for action against persons resorting to smoking at public places. Under the law, a person can be fined Rs1,000 for a first time violation and the penalty can be increased up to Rs100,000 in case of second breach. (By Mukhtar Alam, Dawn-17, 16/02/2007) AKU accused of negligence KARACHI: The family of a teenage boy has accused the management and staff of the Aga Khan Hospital (AKU) of putting the life of their only child in danger, a charge the hospital has rejected. According to patient Aariz’s father Khursheed Ali Shaikh, his son has been held hostage at the AKU for the last three days. He said that the doctors at AKU were negligent in the treatment of their child as a result of which Aariz is now in a “do-ordie situation.” Shaikh said their ordeal started when they decided to take Aariz to the AKU on September 17, 2006 for a regular check-up. They said the entire treatment was not supposed to exceed two to three days. “He was suffering from a common flu, and we took him to AKU where we met Dr Fauzia who told us that Aariz needed to be admitted to the hospital for a maximum of three days. But it has been five-and-a-half months during which his health has deteriorated on several occasions. But now we don’t even know what condition he is in,” said his mother Nighat Khursheed. Aariz’s uncle, Dr Sikander Ali Shaikh, claimed Aariz was having fits, which is a sign of epilepsy. Dr Sikander is a working general family physician who specialises in cardiology and burns. “Once at AKU, Dr Fauzia said that treatment would cost them Rs 45,000. When we admitted him his blood pressure was normal at 110,” Dr Sikander said. He said Aariz was admitted in the special care unit, which is a mini ICU, where no doctor was available for several hours to look after him. He said the family filed a formal complaint against the negligence of the doctors and the paramedics. “However, five months have gone by and now all the doctors and paramedics simply laugh at us,” he said. Aariz’s mother said the condition of her child has deteriorated. “He has been on the ventilator for the last six months. He has acquired all kinds of infections and no one is bothered for him.” Dr Sikander said that Aariz had developed bedsores that have become full-grown critical wounds. “The bedsores have grown to such a size that you can fit your fist in it. His spinal column is also showing,” he said. Aariz’s father said that doctors have already advised them to prepare themselves for his son’s death. He also said that the hospital billed the family Rs 5,000,000. “They stopped me from coming to the hospital since Tuesday after I discovered his hands tied up and blood dripping from them. I asked them what they were doing and someone then brought them down. Ever since that they have stopped my entry,” Dr Sikander said. Mrs Khursheed alleged that the AKU Security Operations manager also threatened her. “He threatened me with dire consequences when I tried to enter the ICU. He also threatened me to kill me and break my legs and said they will bury my son as a destitute. He also threatened to lodge an FIR against my entire family and also to take us to court,” she said. For its part, the AKU issued its version of events and accused the Khursheed family of harassment and violence. The AKU said the attitude of the family had become unreasonable. The father and uncle of the patient were continuously interfering in the treatment process and clinical management of the patient. According to an AKU handout issued Thursday: “They are using abusive language with the ICU staff, causing harassment to all the staff and have threatened to abduct and kill many of the staff members including doctors and nurses. They are regularly creating scenes in the critical patient care area, which interferes with the working of the medical, and nursing staff in providing care to other patients as well. Various teams of management have met with the patient’s father and uncle to counsel them for not adopting such behaviour and to cooperate with the care providers. But despite these efforts, they continuously display aggressive behaviour. Given the current state of affairs, it has become impossible for the hospital medical staff to continue providing care to other patients in ICU. “Due to the unreasonable attitude, use of abusive language especially for the female nursing staff and threats to kill them, the father and uncle of the patient were denied entry to the ICU as per hospital policy,” AKU said. It also said that as an ethical and socially responsible organisation, the Aga Khan University Hospital believed in delivering safe and effective care to patients and the same is being done in this case. Unfortunately, the disease process itself is very complex and non-responsive with extremely poor prognosis. “It is extremely sad for AKU care providers and administration to observe such wrong allegations being posed against it by the family of the given patient despite best efforts, both medically and financially, to help Sheikh Aariz Ali to fight this disease,” the hospital said in its statement. (By Khurram Anis, Daily Times-B1, 16/02/2007) 24 The poisoning of air, water THE relevant laws exist on paper, yet the wanton destruction of the environment continues unchecked. Pesticide and fertiliser run-off from farms is poisoning watercourses and groundwater aquifers across the country, while untreated industrial and household effluent is being discharged into streams, rivers and the sea. Air and noise pollution in major cities is approaching catastrophic levels and whatever remains of the forest cover is being decimated at an appalling rate. The toll on human health is mounting by the day, and animal and plant species are in the process of being wiped out. All this despite the existence of a comprehensive piece of legislation in the form of the Pakistan Environmental Protection Act 1997, a landmark law that recognises the direct link between conservation and long-term prosperity. The problem clearly lies in enforcement and this is where the state must focus its efforts. As things stand, those with influence can flout the law at will. Poor water quality is of particular concern. A report released on Thursday by the World Wide Fund for Nature-Pakistan in collaboration with several other organisations brings home the truth about water contamination in the country. Citing good sources, the report reveals that nearly 250,000 children die each year from waterborne diseases, which are also responsible for up to 40 per cent of all hospital admissions. In Sindh and Punjab, 36 per cent of the population is exposed to arsenic levels that are five times higher than WHO limits. It is estimated that every third Pakistani consumes water that is not safe to drink, while “99 per cent of industrial effluent and 92 per cent of urban wastewater is discharged untreated into rivers and the sea.” The profit-driven and those unmoved by human misery should remember that all this comes at a price. Health costs related to unsafe water stand at 1.81 per cent of the GDP, or 114 billion rupees. An ailing workforce is less industrious than a healthy pool of labour, and the costs associated with low productivity are borne not just by the state but also big business. The time to enforce the environmental protection laws is now. (Dawn-7, 17/02/2007) Winning the war on polio THE tragic death of a doctor on Friday in a bomb explosion as he was on his way to the Bajaur Agency to counter claims that the polio vaccination was not an “infidel vaccination” is a shocking incident that should serve as a wake-up call for the authorities. Health officials have been struggling in the NWFP to counter propaganda by the clerics who use illegal FM stations to spread lies — like polio vaccine renders one sterile — but Friday’s incident shows how far extremists can go to “protect” their absurd beliefs and convictions. It is this obscurantist mindset that has deterred officials from eradicating polio in the province. Pakistan is one of four countries in the world where the disease is endemic. Last year saw 39 cases of polio reported from the NWFP, up by 11 recorded in 2005. According to the Guardian, 24,000 parents in the province refused to take the vaccine on religious grounds despite health officials showing fatwas signed by Qazi Hussain Ahmed and Maulana Fazlur Rahman endorsing the vaccine. This shows the kind of challenges the authorities are faced with in tribal areas where no amount of reason or logic can change opinion. That it has reached such dangerous proportions where a doctor can be so brutally killed for doing his job is frightening. Part of the problem lies in the government’s ambivalent attitude towards the administration of the tribal areas and their integration into the national mainstream. Local Taliban have established their own form of governance. They have passed decrees like disallowing girls to go to school, punishing men for shaving their beards and on a more extreme levels, carrying out public executions of those they consider infidels or spies. All the while the government has turned a blind eye to this blatant disregard of the state laws and now finds itself in a bind. It can continue to turn a blind eye to these aberrations and excesses only at a great peril to peace and sanity or take the bull by the horn and confront these fanatic elements. One hopes it chooses the latter, especially since children’s lives and future are at risk unless firm steps are taken to rein in the bigots. (Dawn-6, 19/02/2007) Inquiry into case of epilepsy patient KARACHI, Feb 19: While parents and a private hospital appear to have locked horns over the issue of a 15-year old epilepsy patient, Aariz Ali Shaikh, the Sindh health department has decided to conduct an inquiry into the matter. Aariz, according to his mother, was admitted for a three-day epilepsy-related process about six months back, but has been failing to recover. She attributes the failure to a patient-unfriendly attitude on the part of the Aga Khan University Hospital. “My son has become a complicated medical case due to the apathy of the doctors, related staffs and administrative hostilities effected by the hospital,” she said and added that the parents and other relatives were neither being allowed to meet the patient nor they were being kept formally update on the condition of Aariz. A source in the health department said that the AKUH authorities had now approached the department to hold a medical board enabling the shifting of the patient, who is already on ventilator in the ICU, to some government hospital. It informed the health secretary in a letter that Aariz had been left unattended by his parents, added the source. In view of a prolonged allegation and counter-allegation exercises undertaken by the parents and hospitals, now the health secretary had decided to hold a broad- based inquiry to reach the bottom of the problem. While the patient is likely to be kept at AKUH in the given situation, the inquiry committee comprising professionals and specialists from the Dow University of Health Sciences and other departments will start work in a day or two, confirmed Dr Noshad A. Sheikh. In the meantime, the AKUH once again denied the allegations made by the parents and said that the patient continued to be provided compassionate and safe care for the last 156 days of hospitalisation in spite of the abusive and aggressive behaviour of the family. (Dawn-19, 20/02/2007) 25 Mother demands help KARACHI, Feb 20: The mother of a 15-year old epilepsy patient who is reported to be in critical condition at a private hospital has urged human right bodies and influential quarters to stand with her to see her ailing ward. The parents on Tuesday maintained that they were not allowed to see their son in the ICU of the hospital. According to the mother, she had not seen her ailing child in seven days and appealed to human right bodies and those at the helm of affairs to help then get justice and ensure early recovery of Aariz’. On the other hand, AKUH personnel said a counselling session with the family was attempted on Tuesday but with no success. However, the parents were welcome to see Aariz, who the hospital said, continued to get compassionate and safe care on the 157th day in the ICU. Dr Mairaj Shah, Manager Clinical Affairs at AKUH, told Dawn the parents were never stopped from entering the ICU and on Tuesday too they were treated very politely by the staff concerned. He said the hospital management had even agreed to a session with the family members outside the ICU. It was agreed between the family and the AKUH staff that first the parents and an uncle who is a doctor may visit Aariz, in ICU and then sit together with senior hospital personnel. He claimed the family did not turn up and left of their own will. He maintained that in view of the family’s attitude, the hospital had decided that only the parents of the patient would be allowed to see him and inquire about his health and treatment from the doctors in ICU. Sources in the provincial health department said the medical superintendent of Sindh Services Hospital had been asked by the provincial health secretary to constitute a medical cum enquiry board to look into the matter. The health secretary also advised the EDO Health of the city government to visit the hospital and assess the situation. (Dawn-19, 21/02/2007) Smoking ban IT is heartening to see the provincial government’s anti-smoking task force resolve to curb the menace of smoking in public places, transport systems and around educational institutions (Metropolitan, Feb 16). Pakistan ratified the WHO Framework Convention on Tobacco Control in 2004, which calls for a comprehensive, multilevel approach towards tobacco control and prevention of tobacco use among all population groups. Sadly, there seems to have been very little effort on the part of the government in the past in undertaking serious steps to curb this addictive menace. Tobacco use is the number one preventable cause of cancers of various organs, as well as cardiovascular, respiratory, and other diseases and we as a developing nation cannot afford the costs associated with this addictive behaviour. I pray that this new resolution is strictly enforced and not be just another resolution akin to the ban on the sale of guthka which is still freely available in the market. DR SEEMA I. HASSAN (Dawn-6, Letter to the Editor, 21/02/2007) Govt urged to enforce ban on gutka, betel nuts KARACHI, Feb 21: Speakers at a seminar on cancer among children have urged the government to strictly enforce the ban on gutka and betel nuts because they were contributing a great deal in causing oral cancer among children. The seminar, organised by the Children Foundation, was addressed by health experts Dr Aziz Tank, Dr Syed Fahim Ahmed, Dr Rashid Viyani and Dr Ashfaq Siddiqui. Besides, Children Foundation’s chief Ali Hasan Sajid also spoke. The health experts said South Asia had largest incidence of cancer among children as compared to rest of the world. They said normally not more than 110 out of a million children were diagnosed suffering from cancer elsewhere, but this ratio was far greater in Pakistan and the rest of South Asia. They said poverty was a great hindrance in diagnosis and treatment of cancer because only diagnosis and preliminary tests cost more than Rs25,000 in the country. They said children had greater immunity towards cancer and other lethal diseases as compared to elder people but most of cancer cases among children could not be registered because of an outdated medical information system and lack of public awareness.The speakers appealed to the parents to keep a vigil on their children and if they notice white shine in the eyes of their children or they become victims to persistent fever they should consult medical practitioners. They stressed that it was easier to save the precious lives in the early stage. It was disclosed that some 4,207 cases of cancer among children were registered across the country and the number was on the rise alarmingly mainly due to use of gutka and betel nuts. (Dawn-18, 22/02/2007) Fighting polio on two fronts THE MMA government in the NWFP has to step in and stop certain clerics’ drivel on the polio vaccination or run the risk of facing a serious health crisis they may find difficult to deal with. Already their inaction has cost lives — 39 polio cases were reported last year in the province. But the incidence of the disease cannot be brought down without dealing with the vicious campaign of falsehood and canard being carried out by a section of the clerics bent on frustrating the anti-polio drive. Having access to illegal radio stations to spew their venom, such elements are determined to go to any extent to stop the spread of what they call the “infidel vaccine”. The killing of a doctor earlier this week in Bajaur is proof of their viciousness. And now a cleric in a village in Swat is preaching that Islam prohibits finding a cure for a disease before its outbreak in the form of an epidemic and that those who die in an outbreak are martyrs. Such ludicrous claims have produced expected results: during an anti-polio campaign on Wednesday and Thursday in Swat, some refused to have their children 26 vaccinated. It is difficult to reason with such illiterate fanatics but the government will have to find a way to win over support in favour of an enlightened view of things. As it is, health officials in certain areas have postponed the anti-polio campaign for security reasons after the doctor’s death in Bajaur. If put off indefinitely, this could have disastrous effects. The authorities cannot allow clerics to hijack a public campaign and jeopardise children’s health and well-being in the process. They have a responsibility to contain the polio virus and must press ahead with the goal of a polio-free Pakistan. Each time a polio case is detected, it is a reminder of the government’s failure to implement a comprehensive strategy to wipe out the disease. A more effective approach is needed to achieve the goal. (Dawn-7, 23/02/2007) Health officers under town nazims KARACHI, Feb 22: Sindh Health Minister Syed Sardar Ahmad said that all town health officers in the city would be brought under the administrative control of the respective town nazims. During a visit to the town office in Gulberg on Thursday, the minister said that instead of keeping the town health officers answerable to the executive district officer (health), they would be given under the town nazims concerned, so that healthrelated complaints and problems of any town could be sorted out within the town immediately. Syed Sardar said that the government had made it a point that citizens should be provided with good healthcare facilities near their residents. (Dawn-17, 23/02/2007) PM to initiate controversial project today KARACHI: Prime Minister Shaukat Aziz arrives in the city on Friday (today) for the ground-breaking ceremony of a multistory medical tower on the premises of the JPMC. Prof Mashoor Alam, Medical Superintendent, of the Jinnah Postgraduate Medical Center has described the idea of its construction as a pragmatic move which would ensure a better future for medical professionals as well the general public. The proposed complex with fourteen floors is said to have fully-equipped operation theatres, surgical and general wards, with 2000 beds, and complete diagnostic facilities available under the same roof. According to Prof Alam, the project should be viewed in optimistic terms and criticism for the sake of criticism should be avoided. He said that nearly all the present buildings inside the compound have lived out their life and construction work is going on inside almost every ward, which causes a lot of problems ranging from risk of injury during the rush hours of the day to hygiene issues for patients. “What this place lacks is planning on the outset. If the building of the hospital is rebuilt in an organised manner a lot of things would become easier to manage,” he said. On the other hand, a number of senior members of the Pakistan Medical Association (PMA) hold a completely different view about the proposed project. The PMA, strongly opposing the project, says that the health sector in Pakistan is completely devoid of any preventive strategies and due to their absence, every year a huge economic burden comes from implementing techniques to control the outbreaks and hasty methods of medical intervention. Despite all this, there is still a huge loss of life. The PMA says that the best remedy for ensuring prevention of diseases is a sound education system. “Instead of investing in the education system and making fool proof legislation for a smoothly operating health system, the government is intent on spending merely on improving the look of the building. “This is totally unnecessary extravagance for a third world country like us. Instead, the money could be used to save millions of lives,” the PMA says “If this hospital is turned into a complex, I am sure we would not be allowed to even walk on this side of the road,” fears Mansoor Hassan, whose father is currently hospitalised at the JPMC. He said that he has come from Morro and is heavily indebted and is undoubtedly spending a thousand rupees on medicines of his terminally ill father. “I have no idea how am I going to pay this debt back. I don’t even know if I would take my father back with me alive,” said a tearful Hassan, adding, “What would people like me do if we are made to pay for the hospital rents as well.” (By Asra Pasha, The News-3, 23/02/2007) WB team stresses check on HIV/Aids KARACHI, Feb 23: A World Bank delegation called on Sindh Health Minister Syed Sardar Ahmed here on Friday and expressed concern over a surge in the number of Aids cases in the province. There is a need to improve the Aids control programme, the minister was told.Sources privy to the meeting between the delegation, headed by Anabella Abreu, the chief of health, nutrition and population sector, and the minister said that apprehensions were also expressed towards the pace of payments to the NGOs working for HIV/Aids control in the province. Ms Abreu said that activities of sex workers and the jail inmates indulging in unnatural acts appeared to be big reason behind the spread of Aids. Observing that delay in payments to NGOs was also a cause of their affected efficiency in checking the disease, he urged the minister to ensure a system of timely and convenient release of funds to the NGOs, besides better facilitation, a source added. 27 Syed Sardar Ahmed told the delegation that government was taking measures to prevent and control Aids in the province. He was of the view that unsafe administration of injections was the major factor contributing to the spread of the disease in Sindh. He said that there was no shortage of funds for taking preventive measures against diseases, including the HIV/Aids, but the government would not allow misuse of funds at any stage. He said that the newly appointed Special Secretary (Public Health), Dr Abdul Majid, had already been directed to ensure more steps for prevention of the killer disease in the province and also coordinate with NGOs in an effective manner to achieve the goal. Meanwhile, the health minister has directed the officials concerned to simplify the payment system and ensure release of outstanding amounts to the NGOs within 15 days. He also directed them to link financial assistance with the NGOs’ performance. (Dawn-19, 24/02/2007) Stray dog issue a bone of contention KARACHI: A number of drives aiming to purge neighbourhoods of stray dogs have recently been launched in various towns across the city. Many city areas launch drives all year round to counter the menace of dog bites, a major source of rabies in human beings. The Jinnah Postgraduate Medical Centre (JPMC) - the city’s best health facility in the public sector handled 11,400 dog bite cases in the year 2006, up from around 10,800 cases in 2005, according to the hospital sources. This shows that instead of posting a drop, the rabies cases have been recording a steady rise in the city, which has caused great concern. There is no denying that rabies is a horrifying disease, leading to a painful death. Children are the main victims of this terrible malaise. The need to control the stray dog population is therefore an understandable demand of many citizens. However, animal lovers, question the methods used to achieve this aim. Vets describe the mechanism used for killing these dogs as inhumane and particularly painful. They believe that the authorities must also try to identify where the main source of the problem lies. Stray dogs largely breed and grow in numbers where they find leftover food and garbage. This is mostly found near areas heavily populated with restaurants. The vendors throw leftover food into any empty, open spaces away from their stalls. Their justification, however, is that they are left with no option but to dispose of leftover food from their area of operations. “What can we do if there are no garbage containers around? We cannot keep the leftovers in here. Ultimately we dispose off them in any open area that we find,” said one food vendor at Burns Road. Right or wrong, the fact of the matter is that they do not have any option but to do so. The educated strata of the society, however, are no different. Several people dispose off their garbage on any barren land near their houses. Rarely do people know where the garbage containers, near their homes, are placed. This is one of the major causes of an increasing number of stray dogs within residential localities. But is the brutal killing of stray dogs an effective means to deal with the rabies problem? Many would say that their removal is necessary but the method adopted by the government for this certainly needs to be reviewed and altered. Former City Nazim Naimatullah Khan started a campaign in 2005 to eliminate stray dogs from all the 18 towns of the city. These killings came as a result of an increasing number of dog bite cases or dogs suspected of being rabid, a disease transmitted through the saliva of infected dogs. This strategy is based on poisoning the dogs to death. The poison used is magnesium sulphate, which is mixed in meat and left at places where these stray dogs are most likely to be found. It is basically a form of slow poisoning whereby the dogs suffer internal bleeding with muscular incisions and ultimately die. This strategy has a number of flaws. Many pets and birds also fall victim to poisoning as a result. Many consider this to be the most heartless strategy adopted to do away with dogs. According to the Pakistan Animal Welfare Society (PAWS), killing is not the answer. On the contrary, there is a possibility that such a method of killing dogs can cause great environmental hazards and a setback to our ecological system. Also, this method of killing has been scientifically proven to be an ineffective strategy in reducing the stray dogs’ population in different countries. In many cases, bodies of these dogs are often left to rot at the place of death. Even when they are collected, they are dumped in some place not too far from the city limits. Mahira Omer, who works with PAWS, says that dogs are an important part of our urban ecology. She said that they breed and grow up in a certain locality that they become familiar with. If these dogs are to be removed, dogs from another area would soon replace them. In an unfamiliar area, in which new faces abound, there will naturally be more dog bite cases. Even more dangerous is that fact that “An ecological disaster starts paving its way when the poison from the dead dogs find its way into the birds, insects, soil, grass and ultimately into us,” explains Omer. There is a need to realise that poisoning the dogs is not the only viable option left. Moreover, according to Pakistan’s Prevention of Cruelty to Animals Act, 1980, killing animals in this manner has been prohibited and has been termed “inhumane and against the law”. The eradication of stray dogs requires patience from the concerned authorities. The World Health Organisation (WHO) has advocated Animal Birth Control (ABC) in many countries as a ‘safe and humane’ method of reducing dog population. According to this programme, street dogs are captured, given sterilised vaccination against rabies and released back to the area from where they were captured. Vets also say that this is a kinder method of reducing the dog population and controlling the spread of rabies. Neutered animals are also likely to be less aggressive. For the ABC programme to work effectively, it requires 70 per cent of the total stray dog population to be neutered. Countries like Indonesia, India and China are already successfully implementing this policy and have reduced the number of rabies cases to a great extent. Ultimately, the only way to successfully control stray dogs and rabies cases is a well-implemented and thought-out strategy. A necessary part of this has to be a proper survey to determine the number of stray dogs on the street. Simply poisoning or shooting dogs is not necessarily the answer to this problem. (By Sidra Rafique Gooda, The News-2, 24/02/2007) 28 44th annual JPMC medical symposium: Brain doctor to head city’s biggest hospital KARACHI: Neurosurgeon Prof Rashid Jooma was announced as the new executive director of the Jinnah Postgraduate Medical Centre Friday at the opening of the hospital’s 44th annual medical symposium on ‘Epidemic Challenges in the Developing World’. Prof. Mashoor Alam Shah is the outgoing director. Prof. Tasnim Ahsan has been made the joint director and will be in charge of postgraduate training, the school and college of nursing and the schools of physiotherapy and occupational therapy. During the previous director’s tenure, the government had announced the creation of three additional top posts with Dr Tasnim Ahsan as the chief of medicine, Prof. Jooma as chief of surgery and Dr Mussarrat Hussain as dean. It was not clear with Friday’s developments what the status of these positions would be with Prof. Jooma’s appointment as the new director. “I will try to bridge the gap between public demand and hospital resources,” said Prof. Jooma. “When I leave I would like to see JPMC a better hospital than it is now.” Prof. Jooma’s focus will be new services instead of new departments. He said that the government was already providing JPMC assistance but that aside from material resources the focus should also be on human resources. It is likely that he will work towards new maxillofacial services and a breast cancer clinic amongst others. When pressed to comment on the changes that he was aiming to bring about, Prof. Jooma said he would be in a better position to speak after a short while in office. He joined JPMC in 1987. The symposium was inaugurated by Federal Secretary Health Syed Anwer Mehmood with JPMC’s top doctors in attendance, including Prof. Mashoor Alam Shah, Prof. Musarrat Hussain, Dr. Abdul Rab and Dr. Seemin Jamali. The symposium comprises more than 20 hands-on training workshops on basic and advanced laparoscopic surgery, cardiopulmonary resuscitation, primary and advanced trauma support, stress management, oculoplasty, cosmetics and other current issues of medical and surgical importance. The scientific sessions, spanning two days, will also include thematic, plenary, invited and memorial lectures. More than 200 free papers and 25 scientific posters will be presented. In his presentation, Dr. Mussarat Hussain stressed that psychologically the citizens of Karachi and their doctors will have to recognize and change behavioral diseases such as jealousy, extremism and intolerance which are behavioral infections. “An epidemic does not only mean an infection but we have to be watchful of our behavior as well,” he added. In his presentation on epidemics, Dr Abdul Rab referred to the looming water wars in the region. The largest number of people living very close to each other is the Afghan population in Pakistan and this population has a 30 percent rate of the TB disease, he said. This is because an Afghan family lives in an area of 8x12 and each family has more than 12 children. When one person coughs they spread the disease. “Furthermore, oral carcinomas are on the rise in the country in areas such as Lee Market,” Dr Rab said. “I know a pan wallah who earns Rs 50,000 a day and another one in Sindhi Muslim Housing Society who earns Rs 30,000 a day.” Dr Rab referred to a fatwa issued by a cleric against polio vaccines and condemned the murder of a doctor who was working with a polio team in the NWFP. “This year has been an active one,” said Prof. Mashoor Alam Shah while referring to the renovation of the accident and emergency ward. JPMC treats an estimated 180,000 patients yearly and there has been an overall increase in the number of patients, major surgeries and deliveries from 12.5 percent last year to 15 percent this year. An estimated Rs 244.9 million have been spent on thirteen development projects. Also, an institute of neurosurgery is being built at a cost of Rs 150 million and Rs 370 million worth of equipment has been bought for various wards and operation theatres. Two generators have also been installed for the entire hospital. The latest electron microscope has been installed for basic sciences. Roads, drainage lines and water lines are being constructed and the main lab has been modernized. The hospital has a staff of 400 qualified. Around Rs 150 million has been pledged for repairs to the residences for doctors, nurses and paramedics. An operation theatre for the ENT department has been constructed and the prime minister’s program to counter hepatitis is underway. Ambulances, staff cars, trucks, a road-sweeping machine and a tractor have been added to the hospital’s fleet of vehicles. Furthermore, the Rs 8.6-billion JPMC towers have been approved by the Planning Commission. In the first phase, three towers will be built at the cost of 3.3 billion rupees while in the second phase one tower will be built. (By Farhan Ahmed, Daily Times-B1, 24/02/2007) Century-old leprosy centre to be upgraded KARACHI, Feb 24: The city government has decided to develop its century-old leprosy centre in Manghopir as an infectious disease centre. Speaking as the chief guest at city government leprosy hospital in Manghopir on Saturday, City Nazim Mustafa Kamal declared that the 110-year-old leprosy care centre would be upgraded as the Institute of Infectious Diseases, where research would be conducted on leprosy, hepatitis, AIDS and thalassaemia. He said the planned institute would serve as a school for sanitary inspectors, health inspectors and food inspectors to obtain various diploma courses, while doctors, nurses, and paramedical staff would be involved in research works related to infectious diseases. 29 Mr Kamal, along with Sindh Planning Minister Shoaib Bukhari inaugurated a modern eye operation theatre, laboratory and dental unit at the centre where the World Leprosy Day was being observed. Addressing the gathering, the nazim said it was the present government that paid attention to the centre and now changes had started taking place. The new lab was first of its kind in the government sector in the province, which would enable diagnosis of leprosy disease, he remarked. Shoaib Bukhari said the provincial government, which had already approved the establishment of the institute, would extend financial cooperation for the upgradation. District Coordination Officer Fazlur Rehman, Dr Ruth Pfau, Dr Waqar Kazmi, Dr Khalid Javed, Dr Nusrat Shaukat, Dr A.D. Sajnani, Dr Muhammad Ali Abbasi, representatives of non-government organisations were also present. (Dawn-17, 25/02/2007) Health of the state By Dr Sania Nishtar The divide in opinion about the construction of a medical tower in Islamabad; the indication that another one is in the pipeline for Karachi; signals that investment is underway in high-tech medical equipment; the organ transplantation bill and concerns expressed after its tabling and the debate around the much-hyped medical tourism raise two important questions about the role of the state in health sector. First: what is the role of the state agencies with respect to 'health' within a 'social sector context'? And second: what is the role of state agencies with reference to the emergence of health as a 'sector' within a 'market economy' in Pakistan? These two dimensions of health may seem interlinked, but they are, for all practical purposes, separate paradigms and warrant specific lines of planning and implementing arrangements. In a nutshell, the first question is linked with the Alma Ata ethos, the 'Health for All' strategy, the charters of Ottawa and Bangkok. Pakistan is a signatory to all. In line with these, the country places health as an essential prerequisite as well as an outcome of sound development policies. The answer to the first question is also embedded in the 'spirit' of Pakistan's commitment to meeting the Millennium Development Goals and reflected in the country's strategy papers -- the Poverty Reduction Strategy Paper, Medium Term Development Framework and the current Health Policy of 2001 -- their weaknesses notwithstanding. Trying to answer question one in the context of these parameters, it is clear that that answer has to be embedded in reducing mortality and morbidity and the disparities therein and striving to attain a good standard of health by all people in Pakistan. What is the role of state agencies in this context then? Foremost, it is to set the vision for the sector within the constitutional framework of rights and privileges, values and principles. It is also to integrate the public and private sectors to deliver that vision. Operationally, this would entail a two-fold exercise. First, and ideally, it would be to deliver health services as a public good to the people of the country. Pragmatically, however, in resource-challenged countries it is not possible to deliver all health services to all citizens and therefore the role of the state in countries such as Pakistan is to outline a range of services it will deliver as a public good. These services may be termed as an essential national health package. In the delivery of these services, the state needs to be clear about the coverage and the choices concerning these services, most importantly, about the means and mechanisms of their provision. State agencies in health also need to deliver all services not classified in the above category but classified under article 38 of the Constitution as social protection measures. Both these objectives can be pursued by modernising public financing and provision of health services in order to make them efficient, effective, responsive and accountable so that they can provide the bulk of care through their own infrastructure or by leveraging the infrastructure of the private sector. This should underpin the creation of a National Healthcare System in Pakistan and this is primarily the foremost role of the state in the health. True there is a private sector dimension to this role under question one, and one that needs to be separated from what will be discussed under the second question. Here the private sector assumes importance because it can assist and augment the state's health delivery agenda, for example, in using private clinics and NGOs to get essential services delivered. It can also mean involving the civil society in strategic planning, in autonomous governance arrangements (as in the case of hospitals) and 'contracting out' management. In this framework, the role of the state should be one of legitimate regulation, creating an enabling environment and developing appropriate systems and procedures for public-private engagement with attention to safeguards. This calls for enhancing the capacity of state agencies for playing a contemporaneously appropriate and effective stewardship and governance role in the health sector. The other role of the state under question one is quality assurance of private sector healthcare through regulation. The private sector in Pakistan is huge and has many well documented problems with quality. It is the government's duty to facilitate the private sector in general and this holds true for the health sector as well. But the government also has a fiduciary responsibility in this regard given that health is one of the social services. Therefore, the key challenge is to foster, promote and strengthen private sector healthcare delivery and balance it against quality and patient safety while safeguarding the interests of the poor and the marginalised. With respect to the role of the state, therefore, it means addressing two issues. The first relates to quality assurance and links it with the need to create a regulatory mechanism for quality such as a national institute of healthcare quality. The other relates to developing means of using public funding to ensure that poor people who access health services through private providers are not disadvantaged or discriminated against. This in turn relates to factoring in waiver and exemptions in the existing social protection mechanisms at the level of private providers. The second question is related to the role of the state agencies with reference to the emergence of health as a 'sector' within a 'market economy'. Here 'private' has a 'commercial connotation'. As a way of contextualising the discussion that follows, it may be opportune to point out here that the healthcare industry is the world's largest industry with global revenues estimated at $ 2.8 trillion. Perhaps it is the largest industry in Pakistan as well. In this context, we need to consider a number of important things. 30 First, the much talked about 'medical tourism' which can present an opportunity for hospitals to fuel growth by tapping the potential of the international patient market. In relation to the role of the state, an important caveat here is that public resources earmarked for health should not be used to promote medical tourism at the cost of essential health services because there is little benefit in serving the equity objective in health, except indirectly, through improvements in quality. But because this is an industry, the private sector should be encouraged to analyse opportunities, spearhead sectoral development and formulate strategies to improve competitiveness. In this context, however, the level of facilitation by the state should be guided by the potential that medical tourism holds in Pakistan with reference to fueling growth. A careful analysis shows that medical tourism has limited potential in Pakistan for a number of reasons. The success of medical tourism depends on many factors: high degree of sophistication of indigenous health systems, high quality of healthcare at low costs, an expatriate-friendly environment and a well developed tourist industry. Based on these criteria it is clear that medical tourism industry will not have an emerging trend in Pakistan at least in the short to medium term. On the other hand, Pakistan is unfortunately being ranked amongst the few countries where transplant related-tourism is burgeoning -an issue brought increasingly to the limelight recently in the aftermath of the tabling of the organ transplant legislation. What will be the role of the state in this situation? Clearly, it is to build ethical safeguards through policy and legislative measures and their effective implementation so as to curb the existing unfortunate practices being used and promoted by huge vested interests. The second important area is the agreement on the liberalisation of services which is a part of the international trade negotiations taking place under the World Trade Organization (WTO). Pakistan is a member of WTO and a signatory to the Agreement on Trade in Services (GATS). Under this, member countries agree to make services trade more open to other countries with the essential aim of further liberalising services that have traditionally been under the public domain. The main concerns about GATS have been along the lines of concentrated ownership and about rules that affect the ability of the government to hold companies providing services accountable. In addition, mainstreaming of curative services on free market principles and the promotion of high-end care would be at the cost of prevention in which the private sector has no incentive to invest in any case. In the wake of these potential challenges, the government must enhance its own regulatory capacity to look at these contemporaneous globalisation-related issues because they impact the delivery of health services. The third area where market mechanisms cross cut with health is in the area of the export of generic drugs. Pakistan has a fairly large local pharmaceuticals manufacturing industry. Growth of the sector as an industry in the neighboring countries raises the question as to how we can enhance our revenues and pursue export targets by strengthening this industrial base. In the post-TRIPS scenario, with stronger patent protection, governments are under obligation to enhance research and development base of the local industry. In this context, the question as to how this can enhance the above mentioned objective becomes even more important. Here it must be recognised that manufacturing and export are dependent on the economic policy framework, patent regime and other regulatory arrangements in a country and that a range of actors in the state's system outside of health such as trade, investment, intellectual property rights and consumer protection have roles in this area. However, at the same time, it must also be recognised that pharmaceuticals are one of the critical inputs into the health system and that the foremost role of state agencies is to ensure the sustainable supply of quality, efficacious and safe drugs. What is the overarching role of the state here then? It is to bring clarity in agency roles, responsibilities and prerogatives in relation to pharmaceuticals as a critical input to health systems vis-a-vis pharmaceuticals pursued as an export target. The fourth area is that of institution-based private practice. There have been many attempts in various parts of the country aimed at mainstreaming this approach on the premise that this will enhance institutional efficiency. Some of these have been successful as in the case of Punjab Institute of Cardiology whereas others such as in the case of NWFP have been unsuccessful for reasons that are beyond the scope of this discussion. Increasingly, many a times a case is made for the use of public money earmarked for health on tertiary care infrastructure on the premise that it promotes institution-based private practice. In this regard, the role of state agencies is to ensure that such investments are made only if they can improve performance and efficiency to meet the equity objective in health. Finally, another commercial consideration in health is one of private health insurance. Questions relating to its potential in Pakistan have frequently emerged. Here it should be recognised that private health insurance is just one of insurance arrangements in health and that its growth is generally paralleled with economic growth in general and growth of the formal employment sector in particular where employers subscribe to health benefits. Through the current foreign direct investment policy of the government of Pakistan and the Insurance Ordinance 2000, an enabling environment has been created for the insurance industry in general. However, the health sector cannot benefit from this significantly because of a number of limitations: fragmentation of the provider market and the predominance of the workforce in the non-formally employed sector being the foremost of them. As a result of this, health insurance agencies do not find the incentive to operate in the country. This is evidenced by the current situation: Group health insurance is offered by seven insurance companies and individual health insurance by only one company. In this context therefore, the state can pursue measures to give financial incentives, albeit with safeguards to regulate the operations of private health insurance agencies. This should be done with the realisation that many other factors influence the growth of private health insurance. There is an important caveat here: easing of insurance regulations and opening up of the sector should be on the premise that employer-provided health insurance is not a substitute for the state's role in financing health. In summary, health should be regarded as a fundamental human right and a key component of the social sector. In this era of liberalisation, however, health sector also cross cuts with market mechanism in many areas and stands out as an industry. As markets create opportunities to enhance efficiencies in the health sector in Pakistan, with indirect possibilities of benefiting the under privileged, the state needs to be cognizant of the potential that markets have in creating inequities. The state must also regard its responsibility for social welfare as a priority to bridge them. (By Dr. Sania Nishtar, The News-PolicyIII, 25/02/2007) 31 Kidney trade — a haven for the country’s destitute KARACHI: Pakistan has, in recent years, witnessed a major growth in the organ trade. With figures estimated at US$15 million, the country has acquired a shameful reputation as being a ‘Gurda Piri’ (kidney retail market). The stakeholders in this arena have given a mixed reaction on the legislative proceedings in this direction which has taken place after years of struggle by the medical community. A number of lawyers and doctors have lauded the move of passing the comprehensive bill on Transplantation of Human Organs and Tissues Ordinance, 2007; however, some experts see contradictory statements in the text of the law, which were quite strikingly obvious too. Dr. Farhat Moazzam, Pediatric Surgeon and an active member of the Sindh Institute of Urology (SIUT) team is one in pursuit of the proposed transplant ordinance and also of the paradoxes that it comprises. “We greatly welcome the step of passing of this bill, but it should be delayed anymore this time. Besides, this important issue seems to be off little significance to the legislators, otherwise it would have been a proper law not an ordinance after years of lagging behind our neighbors at having a law that regulates such significant medical procedures,” said Dr. Moazzam. Kidney transplant is not an emergency operation in most cases. Everywhere in the world, laws restrict donation of organs to non-blood relative recipients. If a patient could not provide a genetically related donor, then according to law they have to resort to life-long dialysis. Even in many Asian countries, the law restricts donation of organs to people of other nationalities. This act has been criminalised in Iran, India, and many Middle Eastern states. Because of the absence of any law, people from across the world come to Pakistan to get kidney transplants since finding a willing kidney donor here is just as easy running into people who would donate blood. This resultant situation from lawlessness has the onus of Pakistan harboring an entire organ wholesale market, commonly known as Gurda Piri. “People out there putting their organs on sale are not actually donors but vendors to be correctly called. This is an embarrassing situation to reflect upon the socio-economic state of this society where all the asset people are left with their own organs when faced by a financial constraint,” she said disapprovingly. She is visibly concerned about the aftermath of organ donation for the donor, as majority of them are financially forced to sell their organ and getting the post-surgery care and regular follow-ups is a luxury of course. “In this business, it’s the vendor who pays the biggest price. They don’t realize the value of good health and end up making money on their own body parts. This shows how vigilant they are of their health. One of the reasons of rising renal failure incidences in the country is the kidney trade. If the government does not take steps to curb this, the government will be posed by the threat of kidney disease epidemic which is no small economic burden at all,” she said. There are websites and emails adverting renal transplant along with different packages with a classification of different packages for local and foreign patients respectively. These packages are inclusive of the hospital stay and recovery period follow-ups and range from $13000 to $ 8000 for foreign and local recipients, respectively. This business is currently believed to be worth US$15 million in Pakistan according to a survey conducted in 2006. The largest fraction of money goes to the surgeon in this case, while the vendor hardly receives Rs 15-20,000, which is practically inadequate to give him the health insurance for the rest of his life to live without an important organ. Pakistan is a signatory to the World Health Organization (WHO), whose guidelines for organ and tissue transplant urge the member states to proceed any transplant surgery which reek of commercial transactions, also terming it below human dignity to put parts of human body up for sale. “It is very important for us to restrict this activity as it is detrimental to our society, both in terms of economy and reputation,” concluded Dr Moazzam. (By Asra Pasha, The News-5, 25/02/2007) Leprosy Hospital to be upgraded to institute KARACHI: City Nazim Syed Mustafa Kamal has announced the upgrading of the city government’s Leprosy Hospital in Manghopir as the Institute of Infection Diseases, saying that it would be the first of its kind in the province to conduct research on Leprosy, Hepatitis B & C, AIDS and Thalassemia. It would also serve as a school for Sanitary, Health and Food inspectors as well as offering diploma courses and research facilities to doctors, nurses and paramedical staff on infectious diseases through its modernised laboratory, he added. He was addressing a large gathering at the hospital on the World Leprosy Day on Saturday. It may be mentioned that a modern eye operation theater, laboratory and dental unit have been completed at an estimated cost of Rs 10 million in one year time. In his address, Mustafa Kamal said that the Leprosy Hospital bears historical significance as it has been serving the people for the last 110 years. “During this period, no one took the initiative to upgrade this hospital, however, the present Haq Parast leadership has taken concrete steps to transform it into an institute,” he added. He said it was not necessary to observe the World Leprosy Day by just holding public gatherings, rather the occasion demands for taking some concrete and practical steps to serve the ailing humanity. He said he had announced these projects last year on the World Leprosy Day and now these stand completed. 32 The Nazim said that the newly established laboratory was one of its kind in the entire province to identify leprosy diseases before it strikes a patient, adding that such a testing facility was only available in Islamabad. Private sector hospitals like Aga Khan Hospital has such facility but middle and poor class people could not afford the test fees, he added. Mustafa Kamal said that the newly established dental unit and eye operation theater would also serve leprosy patients as well as the common people of the area. He said he was delighted to see that over 150,000 patients had benefited from the general OPD section which was revived on his instruction. Besides upgrading Leprosy Hospital, the government was also providing healthcare facilities to the people residing in a large number of Goths in Manghopir, which proved that the present city government was serving the people without any discrimination, he added. (The News-5, 25/02/2007) Fire traps in hospitals EVEN for the fittest of people, escaping a raging inferno can be an ordeal not always rewarded with success. Besides the flames, the perils of smoke inhalation, structural collapse and stampedes are all hurdles in the way of survival. These threats become magnified when buildings lack emergency exits and firefighters proper equipment — something that is sadly the norm across the country. There is no knowing how many lives could have been lost on February 18 had the PNSC building in Karachi caught fire on a working day. Even though there was no dearth of fire engines, none were equipped to tackle a blaze on the upper levels of a 15-storey building. Fortunately for the few people trapped inside, navy and army helicopters were on hand to assist in their evacuation. Now imagine a conflagration in a large hospital with thousands of patients, attendants and staff members present on the premises round the clock. Consider particularly the plight of those confined to bed, many of whom may not even be fully conscious, and the worst-case scenario does not bear contemplation. What would be the fate of Karachi’s Civil Hospital which lacks not only emergency exits but also adequate fire extinguishing equipment? Awakened to the peril by the PNSC blaze, the hospital’s board of governors decided this week to install fire escapes on a priority basis. While it is a relief that the CHK board has belatedly taken notice of this serious omission, it has to be ensured that the plan is followed through to its logical end. In case there is a shortage of funds, the Sindh government must provide these forthwith. Hospitals and other in-patient healthcare facilities throughout the country need to be surveyed to ascertain whether they conform to fire-related safety standards. Assessments must then be followed up with action. (Dawn-7, 25/02/2007) Racing against time on Rafiqi Shaheed Road By Sabeen Jamil Life is unfair in this city for the underprivileged. And nowhere does this become more obvious than in government hospitals. And now it has even become a task to reach them in the first place. Jinnah Postgraduate Medical Centre (JPMC), one of the two major public hospitals of the city, the National Institute of Cardiovascular Diseases (NICVD), the National Institute of Child Health (NICH) and the Kidney Centre, are all located on the same road – the narrow, broken and uncarpeted Rafiqi Shaheed Road, mostly occupied by huge pipes and terrible traffic jams. What happens next? Only the patients and their attendants can tell. Nasima Bibi, 25, had never thought that she would have to give birth at home without a trained gynecologist in a city like Karachi. It is common in her hometown, Mianwali but she thought things would be better in a big city. Her frequent visits to the JPMC had convinced her of a safe labour. Fatefully, during the seventh month of her pregnancy she slipped in the bathroom and was rushed to the hospital in a taxi from her home in Usmanabad. She reached Shahrah-e-Faisal in 25 minutes but due to the customary day-time-traffic-jam at the Regent Plaza signal couldn't reach JPMC, just 3km away. It took them 15 minutes to cover that distance. Time waits for no one and Nasima delivered her now three-month old daughter in a taxi just minutes away from the hospital. Both mother and child are safe and healthy now but the experience of having delivered her child in a cab will haunt her forever, "Will I ever reach the hospital or am I going to die unattended? Was all I could think at that time," she recalls. For Shakeel Ahmed, selling birds at Empress Market, life was simple until one morning his father had a severe heart attack. A call from his home in PIB colony telling him that his father was lying unconscious destroyed his calm. He rushed to the Edhi counter in Sabzi Mandi No. 2 for the ambulance but was told to wait for an hour as there were no ambulances available. Considering his father's condition he opted for a rickshaw. Working at Empress Market he knew that the route from the Market would be bottlenecked at that hour therefore he opted for an alternate route through Jail Chowrangi to a narrow street at the back of Lines Area and successfully reached NICVD in 20 minutes. This rerouting however, made no difference, as at the signal in front of NICVD he had to stop for 12 minutes. "If I were driving that rickshaw I would have ran the constable over who wasn't listening to me at all." With the help of some motorcyclists he got out of the jam and reached the hospital violating the signal. "I brought my father here in tears. The heart attack was severe and the doctors told me he was brought just in time. Who would have been responsible if I were late by five minutes?" he questions blaming the City Government for allowing stalls at the Empress Market for 50 rupees and blocking the main route to the NICVD in return. "They don't care if a human life is at stake. All the care for is making money." Such cases are not a rarity. The emergency wards at these hospitals especially at JPMC and NICVD are full with patients arriving late to the hospital due to traffic jams outside the hospital. Most come in serious health conditions and sometimes die for not having received timely treatment. At NICVD alone, according to the hospital data the ratio for broad death (death before reaching hospital) is approximately 40 percent. Only two months into the New Year, the statistics are scary. "In 2007 alone 153 cases of broad death have been registered so far," states Dr Anis Memon, Consultant Cardiologist NICVD, citing delayed arrival due to traffic jams as one of the major reasons for BD adding that ratio of deaths in Emergency ward due to delayed arrival is 10 percent. "That approximately makes 50 percent deaths due to late arrival, mostly because of patients being stranded in traffic." 33 In terms of heart attacks and heart failure, early treatment is essential. Dr Zair Hussain, In Charge Emergency ward NICVD, observes, "Out of 300 to 500 patients visiting Emergency ward daily, generally speaking 20 are heart attack patients and 150 serious patients needing immediate treatment." The immediate treatment includes Cardio Version depression within the initial 10 minutes in case of accelerated heartbeat called vented circulation. "If this is not done the patient dies immediately which is what normally happens to patients in broad deaths." Similarly injecting up streptokinase for clot thinning is essential for early treatment in heart attacks. Though it can be injected within six hours of the attack but, "The early you get yourself injected the less are the chances for heart damages," Dr Zair states. Despite so much emphasis laid on early treatment by the doctors, patients fail to reach the hospital in time. Such situations are not panicky for patients and their attendants only, the ambulance drivers taking them up to the hospital too become a part of the ordeal. For Muhammad Yusaf, ambulance driver for Ali Akbar Trust at Jinnah Hospital the traffic problem starts once he is out of the hospital gate. He adds that the problem is maximum during the daytime and becomes more intense during VIP movements. "We keep on honking but never find a way out," he complains recalling how he was stranded for half an hour at Regent Plaza signal to take a patient for CT scan to Saddar but due to VIP movement the road was blocked and the patient expired in the ambulance. "He was a head injury patient and the doctors said that he could have been saved if had reached the hospital in time." The drivers from other services too have hundreds of similar stories to share. "We come across such cases everyday, so much so that we don't even remember them now," says Tariq Mahmood, driver at Edhi ambulance service. For ambulance drivers getting emergency patients out of traffic jams is always a Herculean task. One they perform daily, specifically, at Kalapul, Army Headquarters, the road to Pir Bukhari Dargah (broken and having potholes) where the link road from Gora Qabrastan touches Shahrah-e-Faisal, and from Lucky Star to Shahrah-e-Faisal. The patch of road from Regent Plaza signal to the JPMC is equally identified as the most time-taken road to cross due to heavy traffic. Though there are no exact estimations of the number of vehicles passing through this road daily but according to rough estimates by Regional Traffic Authority buses of 25 routes cross the Rafiqi Shaheed Road with three rounds done by each on daily basis. The number of cars, taxis, rickshaws, motorcycles, water tankers and ambulances passing through the road is unimaginable and the congestion on the road unavoidable. The patients, ambulance drivers and the hospitals' administration collectively propose formulation of an underpass or a flyover specifically at Regent Plaza as one solution to the problem. Diversion of mini buses from this road and formulation of emergency lanes specifically for emergency vehicles is also requested to the traffic authorities. The DIG Traffic Falak Khurshid however straight away discards any such possibility on account that "Eighty percent patients come to these hospitals through public transport so diverting public buses from this road is an absurd idea," he says sternly. The DIG is adamant that delayed treatment to patients because of being trapped in traffic is not a problem at all. "I have never received any complain about this nor have ever known anyone dying on the way to the hospital because they were trapped in traffic," he says furiously and strictly criticizes the data of Broad Deaths at NICVD in this regard. "A person coming in an ambulance and that too to NICVD is obviously a heart patient and in a serious condition and if he dies on the way, traffic is not responsible," he declares while rejecting the proposal of an emergency lane for the ambulance giving the narrowness of the road. "If a problem lies with the road, I am helpless. Making a road is not my job," he declares firmly. And though constructing roads is usually the responsibility of a single department, surprisingly in case of Rafiqi Shaheed road multiple agencies are involved. According to the EDO Transport and Communication (TNC) Muhammad Ather, two years back four action plans were proposed by the Department to resolve the issue. The plans included making an exclusive entrance at the back of NICVD opposite the NAB office, widening of the road from Kalapul to the Naval Heights, which assists traffic from Korangi and Defence. The 30ft road narrows to 10ft when it reaches JPMC due to the encroachments. The plan was to remove the encroachments and widen the road that directly lead to JPMC. The third proposal was widening of the Bazarta lane that is adjacent to the Aisha Bawani school from Shahrah-e-Faisal to facilitate the traffic from Drig Colony and Malir. That too had encroachments. And the fourth proposal was the widening of the Rafiqi Shaheed road by acquiring some of the land from the hospitals and Cantonment. Practically, however except for the exclusive entrance at NICVD, no plan could be implemented. Why? The blame game starts from here. According to the NICVD sources, despite several applications to the authorities, no heed is ever paid to the problem. Only very recently an emergency door was allowed at the back of the hospital in front of NAB office but that too is of no use because given the sensitivity of the area it was allowed to work as a one-way track only therefore is rarely used. Sources told Kolachi that the issue has been discussed a number of times at Governor level including the City Government, Nazims, IGs, Traffic authorities, Transport and Communication Department, the Welfare Services and the Cantonment Board but no concrete plan could ever be devised. The TNC holds Cantonment Board responsible in this regard. According to Mr Ather this is a sensitive belt because of the Naval residential areas therefore land acquisition proposal is always rejected. Moreover the roads proposed for the widening fall under the area controlled by Army Cantonment Board and those roads are full of encroachments. When the proposal to remove them was put forward the Army refused saying they were given on lease. "It is ridiculous how a road can be given on lease. These encroachments are on roads and roads are never leased but no one can challenge them," maintains Mr Ather, the NICVD sources though hold the City Government equally responsible for their lack of concern in this problem the City Nazim, Cantonment and Army personnel are responsible for this, the sources charge. 34 The other central characters of the story (the Cantonment Board, Nazim Saddar Town Muhammad Dilawer and relevant Army personnel) were unavailable for their comments on the issue. How big a budget is required to solve this problem? Which department is responsible for solving this issue? Who is responsible for "not" getting the problem solved? Why is the road not being widened? A head injury patient bleeding profusely, trapped in the traffic on the verge of death never seeks answer to such questions but we should in respect to his right to live. (By Sabeen Jamil, The News-41, 25/02/2007) 44th annual JPMC symposium: ‘Shahra-e-Faisal the most dangerous road for accidents’ KARACHI: A Jinnah hospital project on road traffic accidents recorded 9,300 in four months while the police data for one year recorded 600, said JPMC Director Prof Rashid Jooma Saturday, adding that Shahra-e-Faisal is the most dangerous road in the city. Jooma, who is the principal investigator of the Road Traffic Injury Research & Prevention Centre, explained that it appeared that the police were only collecting data on the serious accidents which is why their numbers were so low. There are two to three points on Shahra-e-Faisal, M.A. Jinnah Road, in SITE area and Mauripur Road where the most accidents take place. All road traffic accidents related to injuries are recorded from the five major hospitals in the city - JPMC, Abbasi Shaheed, Civil hospital, AKUH and Liaquat National - where 30 research assistants work 24 hours in shifts. The project will last until December this year, said program manager Ameer Hussain. Safety engineers will then recommend how changes can be made to avoid these accidents from happening. The project works with SUPARCO and a GIS system and a complete report will be made public after it is presented to the governor. Dr Jooma also elaborated on the JPMC telemedicine project which is planning to make Nawabshah, Jamshoro and Larkana sub-centers. The telemedicine project initially targeted 18 districts in the interior of Sindh but recently their number went up to 24 after their boundaries were changed. The project, which started a little less than two years ago in Shikarpur and Khairpur, provides the centres a desktop computer, an EMR, X-Ray scanner, video phone, and high-speed internet connections. An ISDN line connects five districts to Karachi while one hospital in Shikarpur is connected via satellite. Consultants are available for poor people and people from the rural areas who have no access to such expertise otherwise. The project also trains paramedical staff and local doctors who are updated on diseases such as Dengue and Hepatitis. The project works in two ways. In one, a doctor who encounters a difficult case can sent the details to the larger center which provides advice. The patient’s records are followed. In the second option, videoconferencing is used for patients who are not getting better with the first option. Part of the hiccups involve the poor connectivity of ISDN lines but there are no such problems with the satellite service. People in the rural areas have started coming to the centers after they hear that they can access some famous doctor from there and there was an increase in the number of patients in 2006. “We are aware that telemedicine is not a treatment and just a way to allow treatment,” Jooma said. But it is still a step forward as some patients who would never dream of leaving their village have been persuaded to travel for treatment to the bigger centers. “We persuaded them via videoconferencing and just guided them on which train or coach to take to reach the city and ask for JPMC,” he said. “Videoconferencing gives patients confidence so much so that the Dermatology practice has increased exponentially with around 100 consultations per day in the course of five hours. SUPARCO has installed a satellite dish on the JPMC roof which allows them to see the data such as scans without necessarily downloading them. Dr Jooma admitted that the technology was indeed expensive. “There is no firm serving telemedicine in Pakistan while in India there are half a dozen,” he pointed out, adding that JPMC was looking to American technology which is cheaper. (Daily Times-B1, 25/02/2007) Preventing Aids A WORLD Bank team recently called on Sindh’s health minister to express alarm over the mounting figures for HIV/Aids patients in the province. The existing Aids control programme, they said, needed improvement. The Bank is providing millions of dollars to the government to stop the spread of the infection and is justifiably concerned over the lack of progress on this count, especially the slow release of funds to NGOs that are fighting this scourge. There is good reason for the government to heed the team’s advice which should apply to the other provinces as well. At the moment, Pakistan has a low HIV prevalence rate — about 0.1 per cent of its adult population is believed to be infected with the deadly virus. This is nothing compared to statistics for some other countries, including India where the number of HIV/Aids patients is in the millions. But there is no room for complacency. There are several high-risk groups in Pakistan, such as long-distance truckers, commercial sex workers, prisoners and drug addicts using shared needles. Moreover, unsafe health practices like the transfusion of contaminated blood are also responsible for the transmission of the infection. Apart from this, what is also contributing to the spread of Aids is poor awareness of the disease and the tendency not to discuss it openly because of the social stigma associated with it. There have been some positive moves to counter this conservative trend, such as the formation last year of an association consisting of HIV/Aids victims. But more such steps are needed to raise awareness and disseminate information about Aids. At this stage, when Aids is still not a major problem, dissemination of the relevant information could go a long way in discouraging promiscuous behaviour and making it much easier to implement measures aimed at preventing Aids. (Dawn-7, 26/02/2007) 35 Steps suggested to prevent HIV/Aids spread KARACHI, Feb 26: Speakers at a seminar on Monday stressed the need for collaborative efforts on a priority basis to avert any generalised spread of HIV/Aids in the country. They suggested scaling up of interventions in high-risk population and focusing on male and female sex workers, prisoners, truckers, etc. The three main transmission routes of HIV are sexual contact, exposure to infected body fluids and tissues and infected foetus or baby during prenatal period. The observations and expert opinions came at the seminar organised as part of the third annual international symposium by the Dow University of Health Science (DUHS). Chief guest, retired chief justice Saiduzzaman Siddiqui, speaking on the occasion, said that extra-marital relations and homosexuality were being considered as the major source of the HIV/AIDS spread, but such a trend could be countered through the social code of life as prescribed by Islam, which condemns all such acts. Highlighting the constitutional safeguards available to an HIV-positive/Aids patient in the country, he said that access to reasonable health service to sustain and enjoy life was a basic right of every citizen whereas the budgetary allocations for health services exposed government’s apathy towards constitutional obligations. He observed that the size of the allocations for healthcare was nowhere close to the ideal “Health for all” notion. Talking about HIV/Aids stigma, the former chief justice said that it was severer than those associated with other lifethreatening conditions and extended beyond the disease itself to providers and even volunteers involved in looking after the HIV/Aids patients. Lack of knowledge on the part of masses vis-a-vis HIV/Aids had resulted in the isolation of patients and discriminatory treatment, he noted, adding that health care workers even in highly knowledgeable societies were often labelled public health threats and lost their livelihood. He observed that the patients’ right to privacy was upheld internationally. Measures like screening of high risk groups of people for Aids virus antibodies and counselling and education of those showing test results positive might help limit the risk that could contribute to transmission of the virus. He expressed the view that people should be tested only when the purpose of the tests, its range of reliability, and its potential for social harm was clearly explained, and with the individual’s consent. However, things should be handled with care and it should also be kept in mind that any third party knowledge of results being positive might cause stigmatisation and discrimination and jeopardise important civil rights in such areas as housing, employment and access to health care, he cautioned. Justice Zaman also highlighted the rights available to people with HIV under the American HIV Patient Bill of Rights, and said that the Bill provided a useful guideline to formulate rights of HIV/Aids patients in Pakistan. In his key-note address, Sindh Advocate General Anwar Mansoor Alam said that the national HIV/Aids policy was almost ready for approval and could be adopted if HIV/Aids posed a real threat to the health of individuals, families and communities in Pakistan. He said that the presence of a number of vulnerabilities and the risky behavioural patterns suggested the need for urgent prioritised and coordinated action to avoid the emergence of the virus like an epidemic. Poverty, gender inequalities and low level of education and literacy all contributed to HIV vulnerability in the country but other related factors that could increase vulnerability at the individual level included unemployment, social exclusion or marginalisation, physical and/or mental abuse and gender-based discrimination should also be taken into consideration, he said, adding that delayed response to these activities were placing people at risk of HIV infection as well. He was of the view that HIV/Aids pattern emerging since after the report of first Aids case in the country in 1980, there was a dire need to put things in order so that citizens could be cautioned and protected by law, in addition to being protected by the socio-economic dependency. “With the epidemic continuing to spread at alarming rates in many parts of the world, particularly Pakistan, it is important that HIV/Aids policy explores new and creative measures for dealing with the challenges facing it,” he remarked. Vice-chancellor of DUHS Prof Masood Hameed Khan, said that 50 to 60 per cent people were suffering from one or another illness in Pakistan, hence the health problems were on the up swing and claiming heavy toll in the health care system and causing losses in the economy of people, besides government. “Illiteracy is the root-cause of all problems, therefore, it is need of the hour to promote education and it should be given top priority by all stakeholders,” he added. Director of the Ojha Institute of Chest Diseases Dr Ashraf Sadiq discussed HIV/Aids in relation to TB, and said spread of the former fuelled prevalence of the latter by promoting progression to active TB and increasing risk of reactivation of latent TB. In both the diseases, patient loses his immune system and becomes more vulnerable to the other diseases. He suggested that programmes for HIV/Aids and TB in Pakistan should be interlinked to combat these health problems. Dr Sharaf Ali Shah, Project Director at the Institute of Infectious Diseases, DUHS, said that Pakistan was at present experiencing concentrated HIV spread and there was a serious threat of ‘generalised epidemic’. As such, he added, there was a need for strengthening the prevention and control programmes in the country. Prevalence of HIV among the most at risk exceeds five per cent, while the HIV infection among the injectable drug users in Karachi had jumped from 4 per cent in January 2004 to 26 per cent in 2005. He pointed out that Sindh had reported the maximum number of HIV/Aids cases in the country, i.e. 1,212 cases out of which 1,109 were HIV-positive and 103 Aids cases. Mehtab Akbar Rashidi, Dr Srichand Ochani, Prof M. Zaman Shaikh and Zahid Saeed Syed also spoke on the occasion. At one scientific session of the symposium on diabetes mellitus, Prof Paul Thornally of UK expressed the view that the advanced technology and treatment methods should be applied in diabetes patients to improve their quality of life. 36 Prof Samad Shera and Prof M. Zaman Shaikh discussed the root-causes of diabetes in children under the age of 10 years. They stated that it was increasing due to obesity and excessive use of cold drinks, fast food and oily foods, besides lack of physical activities. In a session on gastroenterology, Dr Altaf Anwar stressed the need for importing and employing latest instruments for diagnosis and treatment of gastrointestinal diseases so that millions of people suffering from such disorders could be provided proper treatment. (Dawn-19, 27/02/2007) ‘Thiamine therapy may help patients with Type-II diabetes’ KARACHI: People with Type-II diabetes may be able to benefit from Thiamine therapy, said Prof. Paul J. Thornalley of the University of Essex while talking at a symposium on vitamins B and diabetes Monday. Thornalley discussed metabolic dysfunction in diabetes and the development of vascular complications. Thiamine is one of the B vitamins, a group of water-soluble vitamins that participate in many of the chemical reactions in the body. The dysfunction of a particular type of cells and impaired glucose tolerance in thiamine deficiency indicates that thiamine therapy may have a future role in prevention of type 2 diabetes. “More immediately, given the emerging multiple benefits of thiamine repletion, even mild thiamine deficiency in diabetes should be avoided and thiamine supplementation to high dose should be considered as adjunct nutritional therapy to prevent dyslipidaemia and the development of vascular complications in clinical diabetes,” said Thornalley. “Accumulation of triosephosphates arising from high cytosolic glucose concentrations in hyperglycaemia is the trigger for biochemical dysfunction leading to the development of diabetic complications,” he said. “This may be prevented by disposal of excess triosephosphates via the reductive pentosephosphate pathway.” This pathway is impaired in experimental and clinical diabetes by mild thiamine deficiency. The expression and activity of the thiamine-dependent enzyme, transketolase - the pacemaking enzyme of the reductive pentosephosphate pathway, is consequently decreased, he said. Dr Naila Rabbani delivered a presentation on “High dose B-vitamins therapy for the prevention of diabetic complications”. Rabbani is a senior research officer in the Disease Mechanisms and Therapeutics Research Group. Prof. A. Samad Shera was the chairperson at the symposium. Baqai Medical University Professor of Medicine and Baqai Institute of Diabetology and Endocrinology Director Prof. Abdul Basit was the co-chairperson. The conference was held to address the latest research on the role of B-Vitamins in the prevention of diabetic complications, such as nephropathy, retinopathy and neuropathy. Diabetic neuropathy is defined as the presence of symptoms and signs of peripheral nerve dysfunction in a patient with diabetes, for example numbness in hands and feet, tingling and burning sensations, gloves and stocking felling etc. the research has established that in the course of diabetes, some 20% to 90% of individuals eventually develop neuropathies. The factors attributed to diabetic neuropathy can be grouped into those having a definite role for example poor glycaemic control meaning high blood sugar level and the duration of disease and those with a probable added influence for example hypertension, age, smoking, hyperinsulinaemia, and dyslipidaemia meaning abnormal lipid profile. Diabetic neuropathy requires medical attention because of its adverse effect on quality of life. Nephropathy is a syndrome characterized by oedema and large amounts of protein in the urine and usually increased blood cholesterol; usually associated with glomerulonephritis or with a complication of various systemic diseases. (Daily Times-B1, 27/02/2007) President orders ‘action’ against AKUH KARACHI: President General Musharraf has ordered the Secretary, Health, Sindh, to take appropriate action against the Aga Khan University Hospital (AKUH) in the case of Aariz Shaikh, who has been in the hospital for the last six months. As alleged by his mother Nighat Khursheed, in a petition, Aariz’s parents were not only stopped from meeting their only son but were also denied entry into the hospital premises. Reports suggest, these orders were issued from the President’s secretariat after receiving a petition from the parents that their only son, who was admitted to the hospital for epilepsy treatment, had developed grave medical complications due what the parents claimed to be negligence on the part the hospital staff, including the senior surgeon. The petitioners had appealed to the President of Pakistan to take action against the AKUH for imposing a ban on the entry of the parents and family members of Aariz and also to save the life of thier only son. Nighat Khursheed said that despite the President’s special attention, the secretary, health, and the hospital staff had not yet lifted the entry ban slapped on the parents. She further said that it was ironic that the Secretary, Health, visited the hospital and told the Press about patient’s “satisfactory condition”, which speaks volumes about the apathy of the state functionaries on such a sensitive issue. Aariz’s mother held the Health secretary responsible for not maintaining impartiality on this issue and, instead, being biased in favour of the hospital’s version of the story, which, she said, was an absolute distortion of facts. Meanwhile, the Aga Khan Hospital has denied all the accusations of negligence in this case. (The News-2, 28/02/2007) 37 Three dengue cases reported in fortnight KARACHI, Feb 27: After receiving information that three new dengue fever cases were reported in a fortnight in the city, the Sindh Health Department has begun measures to meet a possible outbreak of mosquito afflicted diseases in the province. A senior heath department official said on Tuesday two female and a male patient were admitted in a hospital between February 12th to 24th, with a history of high fever, rashes and bleeding. They were diagnosed as dengue positive cases. The two females aged 23 years and 15 years hail from Mahmoodabad in Karachi, and Mirpurkhas respectively. The male patient is 7 years of age and is a resident of Manghopir, Karachi. All of them were discharged by the hospital after treatment lasting two to four days, the official said, adding that the cases could be stray or isolated cases or the result of some end-winter periodic rains. The Special Secretary of Public Health Wing of the Sindh government, constituted a vigilance committee headed by Additional Secretary Dr Shafqat Hussain Abbasi, to check cases of dengue haemorrhagic fever in Sindh. All the administrative heads of government and private hospitals and healthcare centres have been directed to report all DF cases to Dr Abbasi or Dr Shakeel A Mullick, deputy secretary, in writing or on the phone a source said. Last year, 4,600 patients suspected to be suffering from dengue were admitted in Karachi hospitals after an outbreak, while 150 patients were admitted in hospitals in the interior of Sindh between June and December. Of these, about 1,600 patients tested positive for dengue virus, while there were 54 dengue related deaths including 50 in Karachi. The dengue virus is transmitted to human beings through the bite of female “aedes egypti” mosquitoes, which breeds in fresh water and is easily identified as it has white stripes on its body, said an expert in mosquito borne diseases. The Sindh health department has issued instructions asking executive district health officers to start preventive campaigns from March for recycling of underground tanks. Other preventive measures include ensuring cleanliness in vulnerable areas and anti-mosquito fogging before sunrise and sunset. For homes instructions were given that there should be indoor residual spraying of between 20 to 25 houses around a patient house to interrupt the further transmission of viruses. All stored water containers should be kept covered at all time in houses, while the government should also ensure the efficient disposal of all solid waste/garbage to avoid mosquitoes spreading dengue. (By Mukhtar Alam, Dawn-17, 28/02/2007) MARCH Threat to public health TWO highly detrimental factors have crept into our society: plastic shopping bags and false morality: writes Mr Ayaz Amir in his column ‘Useful trades’ (Feb 9). These have become so pervasive that even a person with an average understanding does not miss the significance of his message. I would, however, like to add that one more pernicious taboo has also infiltrated our culture as an obsession, i.e., betel-nut and its by products, such as betel-leaf (paan) and ‘gutka’, that are equally causing severe damage to its social fabric. For the last few years some ingeniously unscrupulous people in order to make quick buck have produced many byproducts of substandard betel nuts by mixing certain intoxicants: one of the most harmful of which is ‘gutka’. (Not long ago customs authorities had impounded a huge quantity of such inferior betel-nuts whose ultimate fate is still not made public). The other derivatives of betel-nut are different types of ‘paan masalas’ mixed with some cheap dry fruits served specially in functions as a fashion. It would be interesting to know that some ‘paan’ shops because of adding certain additive drugs have become so popular that customers always prefer only their products. Although in the past betel-leaf — whose main ingredients are green leaf, betel-nut, ‘katha’, lime with sugar and certain fragrances — was used in urban centres but over the years its usages have spread to every nook and corner of the country. The huge consumption of betel-nut and its by-products is evident from mushroom sprouting of ‘paan’ shops all over the country, including the small towns and far-flung villages. These outlets serve not only cigarettes and ‘paan’ but also sell different types of intoxicants, including the most lethal ‘gutka’. Now the use of these dangerous substances has become so widespread that even while travelling one can find every second person, whether pedestrian or driving a vehicle, chewing betel-leaf or ‘gutka’ and occasionally spitting on the road, at times hitting some innocent passerby. Unfortunately the users do not only create terrible impression by chewing ad infinitum but are also oblivious of the dreadful impact they do perpetrate on their health and the hygiene of surroundings. The more obnoxious scenario is depicted at public places, in general, and government offices, in particular, where, despite spittoons, people prefer spitting on the walls and stairways as a matter of right, leaving it blood-red. The betel-leaf and betel-nuts are not only a serious health hazard with, of course, financial implications for its user, but chewing this substance also disfigures his person. In addition, the country loses every year a lot of precious foreign exchange on import of this stuff. Although the production and use of ‘gutka’ has been officially banned, due to negligence of law-enforcers this unlawful business is flourishing day by day and with this is increasing the number of patients having mouth and lung cancer. 38 In order to discourage the use of these hazardous products, the government should organise campaigns in association with NGOs working in this field and the print and electronic media. Besides, penal action should simultaneously be initiated against those who are involved in illegal activities of its manufacture and sale. Furthermore, Dr Javaid A. Khan’s suggestion, in his letter ‘Tobacco investments’ (Feb 9), that tobacco is the single largest preventable cause of decease and death in the country and, therefore, investment in this sectors has to be discouraged also merits serious consideration. MANZOOR H. KURESHI (Dawn-6, Letter to the Editor, 01/03/2007) Preventing dengue fever NOW is the time to prepare for a possible outbreak of dengue fever. Of late, three patients have tested positive for the virus in Karachi. Last year, 4,600 people with symptoms of the vector-borne disease were admitted to hospitals in the city. Out of these, 1,600 were diagnosed as dengue-positive. Several cases were also reported in other towns and cities. It is possible that in the rural areas the actual figure for dengue cases could have been higher than reported because disease detection and surveillance methods are poor in these areas and several cases could have escaped the authorities’ notice. The winter months meant a brief respite from the dengue virus, but now, the mosquito-breeding season is once again here. Unfortunately, the country’s health delivery system is not adequately equipped to handle dengue cases, especially those complicated by hemorrhaging that has often proved fatal. Experts have warned that if not checked, the disease’s mortality rate could increase to 20 per cent of all dengue-positive cases. Although its symptoms can be treated, there is no cure for dengue fever. Only preventive measures can curb its spread. Apart from large-scale fumigation of vulnerable areas by the relevant authorities, there are steps that can be taken at an individual level to protect against mosquito bites. Application of mosquito repellent and the use of netting and long-sleeved clothing are some protective measures. Moreover, water containers must be kept covered and no standing water should be left in open receptacles like wash basins. Setting up neighbourhood committees to oversee the fumigation of stagnant pools of water would also go a long way in restricting mosquito-breeding. All this can only happen with greater awareness which is sadly lacking at the moment. Educating the people about dengue fever and how to guard against it is necessary for preventive steps to prove successful. (Dawn-7, 01/03/2007) Last dengue outbreak cost Sindh, city heavily KARACHI, Feb 28: The dengue epidemic outbreak, which prevailed for about six months in the city last year, not only affected 4,750 individuals and claimed 50 lives, but also left behind considerable financial obligations to be fulfilled by the Karachi city and Sindh governments. According to provincial and City District Government Karachi officials, both health departments had to bear the cost of blood test of suspected dengue patients and cost of platelets provided to six private hospitals and the blood banks. The entire financial implication of the dengue epidemic in the city could amount to around Rs7 million. This does not include the expenditures incurred on special anti-mosquito fumigations or fogging campaigns undertaken by the city government. The officials said there are fears there might be another epidemic of dengue fever, when the provincial and city governments are still reimbursing payments claimed by healthcare centres against their services for testing and treatment of the patients. The private blood banks approved by the city government, Fatimid, Hussaini and Bismillah Taqi, have submitted bills of about Rs3 million for supplying platelet packs, while the Aga Khan University, Dr Ziauddin and Liaquat National hospitals submitted bills amounting Rs3.6 million, the officials said. The federal government decided in October to exempt 20 per cent custom duty and 15 per cent general sales tax on the import of kits used for diagnoses and platelets, particularly to control and contain dengue fever and dengue haemorrhagic fever because of increasing reports of dengue fever cases and some deaths, According to Sindh health department officials, the relief ordered by the prime minister in the case of importers in monetary terms came to about 48 per cent, which was quite substantial and led to a downward revision in the then existing rates of laboratory tests for the dengue virus and platelet bags required for treatment of patients. In the last week of October, hospitals and blood banks handling suspected dengue patients were informed by the health minister that they should not charge Rs600 for the test from the patients as the cost would be reimbursed as soon as the bills were received. The minister had also asked the health concerns in question not to charge more than 50 per cent of the cost of platelet, while the remaining 50 per cent would be paid by the Karachi city government on presentation of bill. The sources said some institutions charged Rs910 for the test. The officials said one hospital had charged an extra Rs300 from each patient. This institution which is a private university hospital, has submitted a bill for Rs3 million for testing all the patients who reported at its OPD. The same sources added that another blood bank which had submitted a Rs2.5 million bill was another cause for concern for the authorities. Apart from these bills which are liabilities for the city and provincial governments, the CDGK also spent about Rs350,000 on acquisition of kits used for test and preparation of platelets. The city government also spent a considerable sum on procurement of machines and vehicles for fogging in various parts of the city, and the insecticides used for elimination of mosquitoes. There are fears that the threat of another dengue epidemic is looming. A city government health official when asked about it said that initiatives had been taken and citizens would be asked to take preventive measures. The Executive District Officer Health, Dr A D Sajnani said that residents of flats and high-rise buildings would be required to practise these measures. He said by the end of March the city government would be in possession of 33 machine mounted vehicles, which would increase to 40 by June. Dr Sajnani insecticide spray will begin soon to eradicate mosquitoes, particularly those carrying the dengue virus. (By Mukhtar Alam, Dawn-17, 01/03/2007) 39 13.7m children given polio drops ISLAMABAD: The Ministry of Health issued a statement on Wednesday, saying that over 13.7 million children under the age of five were given polio drops this month. Overall, 49 districts were targeted in the recent anti-polio drive. These districts had been classified as high-risk areas in terms of threat of the disease. The government tried hard to ensure that no child was missed during the drive, said the statement. “Polio anywhere is a threat to children everywhere,” it said. In April, polio and Vitamin A drops would be given to an estimated 28 million children in the districts that were not included in the recent drive. These drops would protect children against pneumonia, diarrhoea and measles. Out of the 13.7 million children served the drops in the recent drive, 2.2 million were under the age of one year. In 2006, international experts acknowledged that Pakistan was on the verge of eradication the disease entirely and it could be the next polio-free country. The statement said that cross border transmission of the disease remained one of the main challenges, which was being addressed through special vaccination posts on five entry points on the Pak-Afghan border. The number of polio cases in Pakistan has been reduced from over 20,000 in 2005 to only 40 in 2006 and 65 percent of polio cases were reported in districts. (Daily Times-A2, 01/03/2007) Centralised blood bank on cards to meet emergencies KARACHI, March 2: The City District Government of Karachi is in the process of setting up a centralised blood bank to deal with any emergency need during outbreak of diseases or accidents and disasters, said health department sources. Likely to go functional in three to four months, the blood bank would cost around Rs130 million and provide three different safe blood component packs to people on subsidised rates, added a source, saying that the bank is being established in the office of defunct DMC (East) premises near Quaid-i-Azam mausoleum. It was learnt that high standard machines and analysers were being imported for the purpose from abroad while a plan for new building had almost been finalised. The central bank would have some satellite centres as well. Loss of blood put lives of patients at stake and they solely depend on volunteer blood donors in absence of any centralised blood bank, the sources said adding that the proposed would provide a good store of safe and separated-out blood components, packed cells, platelets and plasma needed to fight against infections, help heal wounds and meet other medical needs. Sources said heavy reimbursement being made by the government to private blood centres for their services to patients in the wake of dengue epidemic had also made the government to think for setting up its exclusive collection and supply establishment. Confirming the bank project, Executive District Officer (Health) Dr A.D. Sajnani told Dawn that efforts were being made to start the bank with around 1,000 packs drawn from human blood completely screened against diseases like hepatitis and AIDS in order to meet the needs generated in times of emergencies. It would be run through donations from healthy volunteers on exchange basis and not through professional blood donors, he added and expressed hope that the bank would start functioning in June. He said all related works were being completed at a fast pace to meet any crisis. “We have decided to run the bank on no profit and no loss basis and estimate that our blood packs would be available to people at almost half of the market price,” he added, informing that no one would be deprived of any blood supply for his or her inability to pay the cost of blood. (Dawn-17, 03/03/2007) CDGK spending Rs3 billion on health sector KARACHI: City Nazim Syed Mustafa Kamal has said the city government is spending over Rs3 billion in the health sector to provide maximum healthcare facilities to Karachi’s citizens. He has also asked concerned officials to take necessary measures against various diseases in advance. After 20 years, the city government officials have for the first time started the cleaning of storm and sewarage drains and spraying anti-germ medicines. The Nazim was presiding over a meeting in his office on Friday in which officers of the Health Department briefed him about the ongoing cleaning and spray drive. They said the work on removing sludge in all storm and sewerage drains in the city is in full progress. Kamal also said that the stock of anti-germs medicine should always be available in huge quantities. In his address, he instructed all those present to engage town nazims, UC nazims and councilors in this ongoing campaign to eliminate the breeding of mosquitoes in their respective areas. He said the city government had planned a comprehensive plan that includes spraying different area day and night until April 22. If need be, it will continue after April 22 to ensure that mosquitoes and germs have been completely eliminated. He added that the participation of the public in this campaign would be beneficial for everyone. (The News-4, 03/03/2007) Civil hospital’s trauma centre hits hurdles KARACHI, March 3: Construction has not started on Civil Hospital Karachi’s trauma centre even after a year because the CHK management and health department officials have failed to address stakeholders’ concerns. A brainchild of former CHK medical superintendent, Professor M. Saeed Quraishy, the trauma centre project was approved by the Executive Committee of the National Economic Council (Ecnec) a year ago. The project was called Accident & 40 Emergency and Ancillary Services Complex. The objective was to deal efficiently with the increasing number emergency cases. The three-year project was in the headlines recently when it was reported in the press that the Services Hospital would be demolished to establish the trauma centre. After facing stiff opposition from all quarters regarding demolition, the concerned officials reverted to the original plan, that of building the trauma centre on Chand Bibi Road. The 7,222 square yards earmarked for the project includes the present eye and neurosurgery departments, the quarters housing city government employees and paramedical staff of the hospital. Medical Superintendent of CHK, Dr Kaleem Butt says to date the management has failed to find alternate space for the two departments and this was why the project was being delayed. “We will do nothing that will affect these departments’ services even for a short time. These departments will eventually be a part of the trauma centre,” he said. Meanwhile unrest prevails among doctors of these departments. “When the plans for the trauma centre were made, no suggestions were sought from us. We came to know about the project from the Press,” complained Dr Junaid Ashraf, head of the neurosurgery department. He warned the unit required close proximity with the operation theatre and CT scan. If all three are not in close proximity, shifting the unit even for a short period would seriously hamper its function and endanger patients’ lives. He supported the trauma centre, but observed that it shouldn’t be built by dismantling existing services, which, he said, were equally important to the community. Besides, the department would also lose the CPSP’s recognition and the status of a postgraduate centre for training when its services, facilities, academic and teaching activities would be curtailed. Dr Adrees Adhi, in-charge of the ophthalmology department, Unit 2, CHK, also shared Dr Ashraf’s concerns and said shifting would be detrimental and affect patients. The in-charge of Unit 1, Dr Ziauddin Ahmed Shaikh, has been working at CHK for 20 years and is the project director of Prevention of Blindness in Sindh. Expressing doubts over the promise that the project would be completed in two years, he said: “The department was shifted to the present location in 1989 and was meant to be a 7-storey building. But, even after 18 years the building is still functioning on the ground floor. With this track record, is it possible to build a 9-storey structure in two years,” he asked. The eye unit of CHK is the only government referral centre for eye diseases in Sindh. It is equipped to perform all sorts of complicated surgeries. Thousands of patients come from Balochistan, southern Punjab and interior Sindh. The doctors working in units being considered to temporarily house the eye and neurosurgery departments, are apprehensive the shifting will affect their departments. Chairman Board of Governors CHK and Lyari General Hospital Abu Shamim Ariff, said only an option that did not affect other departments’ services would be exercised. The project’s design will be submitted by the end of March. The trauma centre project, which has no detailed study report, according to health department officials, would be completed on 50:50 cost sharing basis between the federal and the provincial governments. The federal government allocated Rs50 million last year and Rs37.5 million this year for it while the provincial government has allocated Rs150 million this year. The CHK would get the funds as soon it starts work on the project. The annual recurring cost of the project is Rs150 million to be borne by the hospital. Interestingly, the first trauma centre in the city was constructed almost a decade ago near Ojha Sanatorium on University Road. Owing to financial constraints, the building was sold to the private sector. (By Faiza Ilyas, Dawn-17, 04/03/2007) Kidney sale scam Medical board to examine complainant BAHAWALPUR, March 5: A five-member medical board was constituted on Monday to examine the victim of an alleged kidney removal and sale scam unearthed here recently. The board, ordered by DPO Arif Nawaz, will be headed by medical superintendent of the Bahawal Victoria Hospital Dr Khalid Majid, while radiologist Javed Kamran, Surgeon Prof Farooq Ahmed, Dr Salman Ahmed Waris of urology department, and Prfo Dr Naheed Fatimah will be its members. Dr Majid has asked police to produce the victim, Samia Bibi, for her medical examination before the board on March 7 at the BVH. Inspector Farrukh Javed of Nowshehra Jadid police station told Dawn telephonically on Monday that police had entered the arrest of two accused, Abdul Hamid and Allah Bakhsh, in their record, who were already in custody. The interim bail before arrest of the main accused, Shakil, husband of Samia, and his father Ismail was extended by the court up to March 8. Meanwhile, a lawyer, claiming to be Samia’s counsel, alleged at a press conference here that three doctors had fraudulently removed her kidney. The lawyer, Malik Qasim, flanked by Samia and her mother Bashiran Bibi, read out a lengthy statement in which he took a strong exception to surgeon Prof Ashraf Niazi’s statement given at a press conference a few days back in which he had claimed that the victim was without her right kidney since her birth. He alleged that two doctors, Ahmad Saeed and Sohail Anjum, had removed Sania’s kidney with the connivance of her husband with mala fide intention, and they were involved in the scandal. He said the accused, Shakil, had admitted before a panchayat (before the registration of the case) that he had purchased a new tractor with the amount he received as the price of her wife’s kidney. He claimed that the accused had also mentioned the names of the two doctors who removed Samia’s kidney, and promised to pay compensation money to his wife. Advocate Qasim further alleged that radiologist Javed Kamran in Samia’s ultra-sound report, dated Nov 13, 2006, had stated that her right kidney was missing. He said the doctor never mentioned in the report that Samia’s kidney was missing since her birth. 41 Regarding the absence of kidney removal arrangements at the BVH, the lawyer said that Dr Shabeer Ahmed of Ahmedpur East was involved in several cases of human organ removal, and he did the obnoxious surgery at his clinic without the required facilities. He also alleged that police was conniving with the accused because of political influence. He said the medical documents provided by Prof Ashraf Niazi were fake which were prepared to conceal the facts of the case. He demanded that chief justice of Pakistan and Punjab chief minister should take notice of the matter and immediately remove the three doctors from the service. He also demanded that the case should be referred to an independent medical board comprising top experts of the country so that the accused could be fully exposed. POSTING: Senior police officers in the rank of deputy inspector general will be posted as city police officers in Rawalpindi, Multan, Faisalabad and Gujranwala soon. According to police sources, in these four cites one SSP operations and one SSP investigation will be posted with city police officers. Regional Police officers will work in seven regions of the province while Capital City Police Officer in the rank of additional inspector general of police will work in Lahore city. Except these five cites, district police officers in the rank of SSP will work in 30 districts. (By Majeed Gill, Dawn-5, 06/03/2007) Healthcare regulation awaits enforcement KARACHI, March 5: A draft ordinance pertaining to the improvement, safety and quality of patient care at private hospitals cleared by the Sindh chief minister about 40 days ago is still awaiting promulgation. On the other hand the grievances of public continue to rise. Under the proposed ordinance an accreditation and licensing authority will be set up in Sindh for hospitals, clinics, laboratories, physiotherapy centres, pathologists, nursing homes, maternity homes, diagnostic clinics and other health providers, including hakeems. According to health department officials, the body will be autonomous and regulate privately run health care facilities besides evaluating the organisations’ performances in areas that affect patient care. Government officials believe the proposed regulation is of critical importance to formulate and implement certain standards for quality assurance in private sector healthcare and link those to the cost being charged from patients. Our concern is to make private hospitals services affordable and cost effective and regulate diagnostic and service charges, said an official. Inquiries reveal a draft vetted by the law department and approved by the chief minister during his meeting with the provincial health minister and health secretary on January 24 is lying in Governor’s House. The officials concerned were not ready to come on record why the promulgation plan has been delayed again. The passion for the regulation seen earlier among government quarters seems to have waned, as the private sector hospitals, including charity and teaching ones, do not like to be regulated, said health experts. Some amendments have already been made in the original draft ordinance in consultation with representatives of some private health establishments. The revised draft ordinance was sent to the Governor House, the accreditation authority in the case of private hospitals and clinics will be a fully autonomous body, with its headquarters at Karachi, and will be headed by a chairman, who will be nominated from the private sector by the chief minister. Earlier, the health secretary was suggested as chairman of the new authority, while the vice-chairman was to be taken from private hospital side, a source said, saying that the chief minister will also nominate two persons of medical eminence as members in the authority. The members of the committee should be the vice-chancellors of public and private medical universities, two persons of medical eminence, one representative each from the Pakistan Dental Council, radiologists’ society, Private Hospitals’ Association Karachi, one representative each of Family Physicians or General Practitioners, Pathological Laboratory Association, Unani, Ayurvedic and Homeopathic Association. A grade 20 director/secretary will also be appointed in the authority which will be empowered to give accreditation to health providers and inspect in check list form by medical auditors, call for any medical information from health providers and make relevant regulations. On the other hand patients want checks on private hospitals and demand inquiry or inspection against private hospitals, as in the absence of any regulatory body, according to them; the private concerns are free to charge patients at will. A senior college teacher said that it was negligence on the part of two private hospitals, including one teaching hospital that his father, who was injured in a road accident, became a complicated medical case. The management of one private hospital discharged my father when he was on oxygen, he adds, mentioning that he had to take loans from friends, banks and colleagues to pay for treatment. Another patient who underwent eye-surgery at a private hospital on Stadium Road claimed that despite surgery and post surgery continuous treatment one of his eyes had lost vision due to the negligence and ineptness of the hospital staff in question. Bad manners by the staff and doctors, lack of interest in patient and not informing a patient about his condition, waiting for hours despite prior appointment, out-of-order equipment and questionable tests giving dubious readings, increase in checkup charges and other fees on one pretext or the other, literal extortion of large sums of money in emergency cases, not 42 allowing patients to talk over telephone with their doctors were some of the daily occurrences or encounters experienced by patients and their relatives at hospitals. A health department source said the authorities come across reports about such complaints repeatedly, but they are unable to intervene as they don’t have powers to do so. (By Mukhtar Alam, Dawn-17, 06/03/2007) Pakistan experiencing shortage of medical doctors KARACHI: “Pakistan is facing a shortage of 50,000 doctors needed to attain even a level of one doctor per 1000 patients,” said the Federal Health Secretary, Syed Anwar Mehmood. He has registered his concern about the patient/doctor ratio in the country. This affects public access to quality health care. In his key note address at the Convocation of Jinnah Medical and Dental College (JMDC), he said that there were no more than 75,000 to 80,000 medical graduates serving the country. The issue is extremely crucial and needs to be addressed without any delay, as the population is estimated to reach 250 million by the year 2025. Supporting the government’s decision to promote private sector involvement in the medical education, the health secretary said that the public sector is also playing its role, and that the government is not oblivious about its responsibility to ensure provision for quality education. “Medical education needs a boost in terms of quality, curriculum and modification,” he said. The Federal Health Secretary said Pakistan Medical and Dental Council needs to play a progressive and proactive role rather than just regulating the situation. The Vice Chancellor of Karachi University and the chief guest on the occasion, Dr Pirzada Qasim Raza Siddiqui, said that the country was experiencing major changes as health and education were the top priorities of the government. He appreciated the fact that change registered in the country was specifically with regard to higher and professional education. It was thus up to the young professionals to avail the opportunity besides utilising their skills to benefit patients and the less fortunate segments of the society. He also referred to available opportunities for the local medical graduates in the field of public health (community medicine), primary health care compassing paediatricians, obstetrics etc. The Chairman of Sohail Trust, Dr Tariq Sohail presented the welcome address. Principal of JMDC, Prof. Azhar Hussain, and Vice Principal Dr Deobarah Lobo also addressed the programme. (The News-2, 06/03/2007) PMA opposes medical, dental college at JPMC KARACHI: The Pakistan Medical Association (PMA) has condemned the decision taken by the Federal Health Secretary, regarding the opening of a new medical and dental college on the premises of the Jinnah Postgraduate Medical Centre (JPMC). “It seems that the health secretary and his advisers are in a hurry to make easy bugs in the minimal possible time,” said a press release issued by the PMA on Monday. “The PMA believes that it is not the duty of the Federal Health Department to open medical and dental colleges and construction of high rises, which is purely a provincial and local matter,” it said. “The JPMC is a postgraduate medical centre and it should be developed as postgraduate medical institute in all aspects of medicines (nursing, midwives, paramedics, and allied branches of medicines),” it said. According to the PMA, instead of playing its prime role, the Ministry of Health has involved itself in these kinds of ventures, without conducting any need assessment of the project, and neither the feasibility report of the project has been made public,” it said. It said that the Federal Health Department with the collusion of ‘vested interest group’ is launching this project without proper planning, thinking and keeping the need of the people. The PMA said that the Ministry of Health should concentrate on eradication of polio, malaria, tuberculosis hepatitis and HIV. It said that the Health Department should be stopped from carrying out the project and appealed to doctors, health workers and the citizens to come forward to stop the implementation of the proposed project. (The News-2, 06/03/2007) 25,000 deployed for hepatitis vaccination, PA told KARACHI: Sindh Minister for Health Syed Sardar Ahmed has said that 25,000 health workers have been deployed to carry out hepatitis B & C vaccination under the Expanded Programme of Immunisation (EPI) in the province. He told the Sindh Assembly during question-answer session on Tuesday that the federal government was also funding the programme to control hepatitis B & C, which was being monitored by district Nazims and DCOs. Opposition members claimed that hepatitis B & C cases had increased in the province, while the government was doing nothing in this regard. Syed Sardar Ahmed said that following reports about the rise in such cases he visited Larkana, Jacobabad and Shikarpur to take stock of the situation. He, however, claimed that the situation had been brought under control as only a few such cases were detected in these districts. Syed Sardar Ahmed said that the Sindh government has deputed doctors throughout the province to implement its Health for All programme. He said 761 doctors have been appointed in Grade 17, adding that more than 200 doctors have been posted in rural areas. Besides, the government has planned to appoint 333 doctors in Grade 18 and 475 in Grade 17 besides 150 nurses this year, he said and claimed that the health sector was being accorded priority for the first time in 50 years. 43 The minister said that owing to over-burdening the Health Department has been bifurcated and now the Public Health wing has been separated and working under a secretary. The government was planning to introduce health insurance in all the districts and a German expert would be arriving to brief the department about this system, he said and added that under the devolution programme the government was providing funds to district governments for purchasing medicines under the supervision of DCOs and EDOs Health. Sardar Ahmad said that under the Sindh Rural Support Programme, a private-public partnership has been introduced to hand over two to three Basic Health Units to NGOs, which would assume administrative control of these BHUs, including hiring senior doctors and paramedical staff. He said that the structure of Board of Civil Hospitals was being revived and now the people inducted in the board would be working voluntarily and without any payment. GUTTER BAGHICHA: Sindh Minister for Local Government Muhammad Hussain has said that the Guttar Baghicha land was allotted to KMC Officers Housing Society and the provincial government had constituted a committee to investigate the affairs of the society and its membership. Disclosing this on the floor of the Sindh Assembly, he said that the land was given to society on the court order. He, however, added that most of the Guttar Baghicha land had been occupied during the last 15 years and some portion of the said land was being used for industrial and other purposes. He said that the membership of the housing society would be scrutinized, adding that the committee would determine as to whether the society members were the employees of the local government. He said that the Kidney Hill land issue was pending in the court and no efforts were being made to reach any outside-the-court settlement. It was also being investigated that the said land was being used for the purpose for which it was allotted, he added. MMA MPA Nasrullah Shaji, on a point of order, pointed out that 62-acre Kidney Hill land had been occupied by the land mafia, while it was allotted for the park. The market value of this piece of land was estimated to be billions of rupees, he said and urged the city government to construct a park on this land. Shaji also pointed out that 450 acres of Guttar Baghicha land had also been occupied and demanded that this land should be taken back from the grabbers. AFGHANS: Sindh Minister for Mines and Mineral Irfanullah Marwat categorically said that the government did not detain the Afghans who had returned from Saudi Arabia after performing Hajj. He was replying to MMA’s Yunous Barabi who claimed that more than 1,000 Afghans were arrested following their arrival in Pakistan after performing Hajj and they were still detained, including more than 200 women and aged people. Marwat said that these Afghans happen to be foreign nationals and under the law no foreign national was entitled to obtain NIC and Pakistani passport. He said these Afghans had travelled to Saudi Arabia on Pakistani passports, adding, it was being investigated as to who provided them passports and visa and as to how they managed to obtain NICs. (The News-3, 07/03/2007) We can overcome dengue problem in five years KARACHI: “I expect that we will overcome dengue virus fever within five years form now. The control efforts in Karachi during the last outbreak proved more effective than those employed in Mumbai or Delhi. In other parts of the world where dengue broke out, it did not vanish well before 10-15 years However, if we work in the same manner with all stakeholders hand in hand, supporting each other, the five year target would be achieved,” said the Health Secretary. He was addressing a meeting of EDOs and other health department officials at the Sindh Secretariat. The meeting was headed by the Special Secretary Health, Dr Abdul Majid, in which matters relating to health policy towards dengue virus control were discussed. Dr Shehla Baqi of the Civil Hospital, Karachi, insisted that fumigation/fogging be kept at low priority by health professionals and government both. “The root cause of the disease needs to be identified. It is pools of water which is not even filthy in case of Aedes Aegypti mosquito which is the disease carrier,” she said. She stressed that people need to be educated about how to keep such places mosquito-free, keeping mosquitoes out of their living spaces, and disposal of solid waste. She also demanded of the officials present that they ensure that prices of mosquito repellants should be regularised as they become outrageously high during the outbreak season. An official from the malaria control department said that fogging had produced no results so far at killing the Aedes Aegypti. The spray contents are only effective for anopheles, the malaria-producing mosquito. The EDOs from different districts of Sindh informed the panel that most of the fogging machines provided to them were either entirely out of order with no government support to repair them or they get worked up very soon. The EDO of Sanghar demanded that a central collection unit should be established in Nawabshah and Hyderabad as it becomes a much delayed process for many smaller localities of the interior of Sindh to send their samples for diagnosis to Karachi as the reports are not received before a week’s time. Dr Faruq Hassan, a haematologist by profession, working at a private facility, informed the panel that the disease control strategy was based on three steps, namely, diagnosis, treatment, and research. “Research in our case is totally missing without which it is impossible to devise an effective strategy to fight it back,” he said. (The News-4, 07/03/2007) 44 CHK and LGH may be run by volunteers KARACHI: The Sindh government is considering making changes in the structure of the governing bodies that run five teaching hospitals in the province, including Civil Hospital Karachi and Lyari General Hospital. Provincial minister for health, Syed Sardar Ahmed, explained to the Sindh Assembly Tuesday, in response to a supplementary question, that the government had decided to form boards of governors in teaching hospitals to run their administrative and financial affairs. The boards of governors in five teaching hospitals of the province were formed in 2005 through an ordinance promulgated by the governor. The people appointed to these boards were paid a salary but the government later discovered that this was not making them effective. These people only appeared to be concerned with collecting their salary each month, he said. The decision was aimed at giving financial and administrative autonomy to the hospitals. The enlisted hospitals were the civil hospitals of Karachi, Hyderabad, Nawabshah, Larkana and Sukkur in addition to the Lyari General Hospital of Karachi. “The government is considering reviewing its decision and appointing volunteers to the managing boards instead of paid staff,” the health minister said. In all developed countries, volunteers belonging to NGOs were successfully running public hospitals, he added. In answer to another question, the minister said that the government had recently signed an MoU with a non-government organization, Sindh Rural Support Programme (SRSP), giving it administrative and financial control of basic health units in 10 districts of the province. These district governments had also separately signed same MoUs with the organization. The SRSP would have a supervisory and monitoring role in the BHUs, and the government would put the entire annual budgetary allocations for these BHUs at its disposal. If this venture proves successful in these 10 districts it would be expanded to others. At present, the BHUs at the union council level, have not taken on female doctors and are open only from morning to 2:00 p.m. Under the new formula, the SRSP would group three BHUs at one place and appoint a male and a female doctor for one that would work round the clock. The doctors would paid at least be around Rs 32,000 per month. These developed BHUs would, however, not be able to perform major surgery of cardiovascular work. (By Razzak Abro, Daily Times-B1, 07/03/2007) WKD today: kidney disease a silent killer KARACHI, March 7: Are your kidneys okay? This question may offend you, but will surely make you pause and think about your kidneys. Pakistan and other countries around the globe are observing the second World Kidney Day today, Thursday, March 8. Experts fear thousands of Pakistanis may be affected by early stage kidney diseases and not even be aware about it. Kidney disease is a silent killer; it can cause a loss of up to 90 per cent of a kidney function before one feels sick. So it’s good to know about your kidney’s health right now. “The WKD is perhaps more relevant to Pakistan where the number of kidney patients is rising rapidly. At least 10 million people are affected in the country,” notes Dr Tazeen H Jafar, head of the nephrology section at Aga Khan University. “The consequences of this serious condition are debilitating and may lead to the need for lifelong dialysis or transplantation, both of which are prohibitively expensive for most patients. The condition can cause heart attacks, strokes even premature death. The World Kidney Day was jointly launched for the first time in 2006 by the International Society of Nephrology and the International Federation of Kidney Foundation in response to the alarming prospect that chronic kidney and other major chronic non-communicable diseases will claim the lives of 36 million people by the year 2015. The World Health Organisation has recommended a goal of reducing deaths from chronic diseases by two per cent every year over the next decade. Human kidneys, are two bean-shaped organs the size of two fists, located on both sides of the spine just above the waist. They are amazing organs that play a crucial role in keeping people alive as well. The kidneys are responsible for filtering the blood to separate waste products and maintain fluid balance through the production of urines. It is said that one kidney must function properly for life to be maintained. Some of the most common kidney diseases and conditions are: polycystic kidney disease (an inherited disease), nephrosis (disturbance in the filtration function), lupus nephritis (inflammation), diabetic nephropathy, rhabdomyolysis (a disorder involving injury to the kidney), kidney stones and renal tubular acidosis. According to Dr Tazeen, kidney disease sets in silently with no symptoms associated with its early stages. Therefore, patients go unnoticed until the disease is fairly advanced. Then it is too late to prevent complications. “Unfortunately, this is the most common scenario among patients in Pakistan,” she said. She said it is important to know that kidney disease is easy to detect with simple, routinely available blood and urine tests. All individuals at high risk for kidney disease such as those with hypertension, diabetes, aged 50 years or over, smokers, and family history of kidney disease should undergo annual testing for early detection. The public health mandate for World Kidney Day is clear: government needs to urgently introduce reforms in health care system to address the detection and prevention of chronic kidney disease given the escalating burden of this condition and those associated with it, she emphasises. 45 Dr Abdul Manan Junejo, a consultant nephrologist and faculty member at Jinnah Postgraduate Medical Centre, says the WKD mission is to raise awareness that kidney disease is common, harmful and treatable. This year’s theme is a simple slogan “Are your kidneys ok?’’ He says that studies around the world have shown that even in better educated and developed countries less than five per cent of the population can provide accurate answers to questions about where the kidneys are and what they do. In the Pakistani context, Dr Junejo observed that diabetes is the leading cause of chronic renal failure, followed by high blood pressure as the second most common cause. Hypertension is both a victim and culprit because it can originate from kidney malfunction and also cause kidney disease. Chronic glomerulonephritis and stone disease are also common in the country. Good management of kidney can be achieved by strict control of high-blood pressure, vigorous control of blood sugar in diabetic patients, quitting smoking, avoiding misuse of drugs and obesity. Control weight, eat more vegetables and fresh fruits, reduce salt intake and avoid junk foods, Dr Junejo suggests. Dr Khemchand Moorani, in-charge Pediatric Nephrology ward at the National Institute of Child Health stresses on the need for screening tests to detect kidney diseases in children. Maternal ultra sound, urine DR for protein, red blood cell and pus cells, serum creatine and bicarbonate tests may help diagnose kidney failure and renal tubular acidosis which can lead to stone formation. He calls for the dilatation of kidney and ureters on antenatal U/S and subsequent work up and management to prevent long term effects of urinary tract obstruction like urinary tract infection, stone formation, hypertension and renal failure. He says there are various management processes in case a child develops renal failure. He also stresses on prevention methods like early diagnosis of vesico-ureteric reflux, posterior urethral valves, calculi and other congenital renal anomalies which result in kidney failure. Medical professionals are of the opinion WKD an international approach to address chronic kidney diseases (CKD) as a major public health problem. The risk of premature death, primary from cardiovascular disease is, on average, 1,000 times higher in patients with CKD than the risk of developing end-stage renal disease. Various hospitals, health care bodies and NGOs have organised seminars, conferences and walks in connection with WKD in the city during the week. The Sindh Institute of Urology and Transplantation is also holding a public awareness symposium at its premises on Thursday. (By Mukhtar Alam, Dawn-17, 08/03/2007) Tackling kidney problems WORLD Kidney Day, which was observed round the globe on Thursday, holds special relevance for Pakistan where at least 10 million people are said to suffer from chronic kidney diseases and related problems such as renal stones. Some conditions are hereditary while other risk indicators include diabetes, hypertension and obesity. Given that nearly 15 per cent of the population is diabetic or hypertensive, there is an imminent danger that the problem may become even more acute in the future. Lack of access to clean drinking water is also a factor in Pakistan. Since kidney disease can be a silent killer, diagnosis is often delayed until an advanced stage of suffering, by which time treatment options may be limited to dialysis and eventual transplant. At the same time, the high medical costs involved are beyond the reach of many people. Though some institutions are doing a remarkable job in providing free or subsidised care, they alone cannot cater to a burgeoning patient population. The growing incidence of kidney disease, both locally and internationally, has other implications for Pakistan as well. The country is fast becoming a hub for the illegal organ transplant trade and kidney donors are in great demand. Riven by poverty, people are selling their kidneys for a hundred thousand rupees or even less, with the bulk of the profits going to middlemen and unscrupulous doctors. With post-operative care invariably poor and often non-existent, some donors are unable to return to a normal, productive life and may end up spending more on treatment than what they received for the sale of the organ. By allowing donations by people not related to the patient, the recently promulgated Transplantation of Human Organs and Tissues Ordinance does little more than regularise this unethical practice. The need of the hour is to legalise cadaveric donations. (Dawn-7, 09/03/2007) We’re not putting our money where our mouth is for AIDS: study With a substantial increase in the number of reported HIV cases, little work has been done to understand how resources have been distributed and what factors may have influenced allocation within the newly introduced Enhanced National AIDS Control Program of Pakistan, said a recent report by scientists in a health services journal. The study sought to identify issues that influence allocation of resources within public health programs and to identify perceptions of decision makers about the process of resource allocation specifically within Pakistan’s Enhanced National AIDS Control Program. The research was undertaken by S. Husain from the Department of Health Sciences, Health Systems Division at Aga Khan University, and published in the journal BMC Health Services Research. The researchers conducted a qualitative study including in-depth interviews of decision makers at provincial and federal levels responsible for allocating resources within the bureaucracy. Not all of the study participants considered HIV a priority issue and external funding for the program was accepted because of poor foreign currency reserves and donor agency influence rather than local need. Political influences from the federal government and donor agencies manipulated distribution of funds within the program. These influences occurred despite the existence of a well-laid out procedure to 46 determine allocation of public resources. Lack of collaboration among departments involved in decision making, a pervasive lack of technical expertise, paucity of information and an atmosphere of ad hoc decision making were thought to reduce resistance to external pressures. “Development of a unified program vision through a consultative process and advocacy is necessary to understand the goals to be achieved, to enhance program ownership and develop consensus about how money and effort should be directed. Enhancing public sector expertise in planning and budgeting is essential not just for the program, but also to reduce reliance on external agencies for technical support. Strengthening available databases for effective decision making is required to make financial allocations based on real, rather than perceived needs,” wrote Husain and colleagues in their report. Although Pakistan has a low reported prevalence of HIV, an enormous potential for viral spread exists. Given this potential, implementation of comprehensive strategies including preventive activities, surveillance systems to detect cases early and provision of treatment and care for HIV positive individual becomes imperative. These are all present in the current Enhanced National AIDS Control Program. There are however, operational and financing aspects that distinguish this program from other healthcare programs within the public sector. These include extensive donor funding and public-private partnerships, with NGOs serving as primary service providers within the program. These are the findings and conclusions the researchers arrived at. Study participants considered the existence of an unambiguous hierarchical system of allocating public money, with welldescribed responsibilities, authorities and a separation of power at each level of decision-making an asset. The effective functioning of this system however, suffered due to a paucity of information, lack of trained manpower and political and bureaucratic influence; issues identified in other studies focusing on the decision making structure within the country. This was thought to result in allocation of resources through incremental budgeting and gut feeling with limited, if any, use being made of cost-effectiveness data, feasibility, scientific literature and public opinion. Virtual non-usage of decision making tools to determine optimal allocation resulted from a poor understanding and knowledge of the utility of such tools, along with limited expertise in efficient budgeting. This, the researchers determined, increased reliance on external assistance and expertise, thereby exposing the system to pre-determined priorities and limiting the autonomy of local decision makers. An enrichment of public sector expertise in planning and budgeting through staff trainings and attracting technical expertise by revising public pay scales is essential to make decision-making more rational, evidence-based and justifiable, and to reduce dependency on external agencies for technical support. Lack of valid information, considered an obstacle by most decision makers, identifies a need for strengthening both the public health database (Health Management Information System) and research by the local scientific community. An in-depth analysis of factors that resulted in this relative success could serve to pinpoint strengths within the system that could be enhanced to promote local influences to guide allocation of resources. According to the researchers, Federal level respondents and program managers considered HIV a high priority issue because of its potential for spread and the high cost of neglect associated with the disease. Provincial reluctance to accept the program resulted from an underestimation of disease risk and perceptions that “market influences” rather than local need determined program existence. This difference in perceptions, the researchers surmised, may have resulted from the continuous sponsorship by program managers and donor agencies at the federal level. Federal retention of grant components, which, as explained to the researchers, was a result of institutional capacity and bureaucratic jurisdiction, was perceived as interference at the provincial level. The promulgation of an extensively financed program where partners fail to share the program’s vision may have created problems in achieving program targets. The NACP opens new challenges for developing and maintaining public-private partnerships in an atmosphere charged with scepticism. (Daily Times-B1, 11/03/2007) Ensuring safe blood IT can be matter of life and death. Family members of a patient in urgent need of a blood transfusion often have no recourse other than to approach private blood banks, many of which are poorly equipped and staffed by unqualified personnel. In the absence of a deep-rooted culture of voluntary donation, such institutions tend to depend on professional donors including drug addicts who fall in the high-risk category for blood-borne diseases such as HIV and the more deadly forms of hepatitis. This is particularly disturbing in a country where an increasing number of addicts are injecting drugs and sharing needles. Malaria too is widespread in the country and there is the danger that blood sold to private banks may carry the disease. Lack of quality control and proper blood-screening facilities further compound the problem. While some progress has been made lately in terms of the registration of private blood banks, much more needs to be done to ensure the availability of safe blood. A welcome development in this connection is the move by two German organisations to establish 28 regional blood transfusion centres in all four provinces as well as Azad Kashmir. The proposed centres are likely to be established on government premises in urban and rural areas, and will be well-equipped to screen blood for communicable diseases such as HIV, hepatitis B and C, syphilis and malaria. Following initial discussions and surveys, set-up assistance and operational funding may soon be forthcoming from the German Development Bank and the German Society for Technical Cooperation. The government must extend full support in making this generous offer a reality. Campaigns promoting voluntary blood donation should also be given priority. With diseases such as thalassaemia on the rise, the demand for blood transfusions will only increase in coming years. The time to act is now. (Dawn-7, 12/03/2007) 47 Govt hospitals need proper sanitation KARACHI, March 11: The government hospitals including the Jinnah Postgraduate Medical Centre and the Civil Hospital Karachi badly need an effective infection control strategy through improved cleanliness and sanitary conditions, and a better public image by treating patients with more care, respect and dignity. The private hospitals of Karachi are not only visited by well-to-do people, but also by the patients of middle income and even low-income groups despite their back-breaking bills as they found the hospitals neat and their staff polite and attentive. The big government hospitals of Karachi like the JPMC and CHK are almost at par with these costly private hospitals in terms of buildings, medical equipment, facilities and services of senior professors, but due to lack of hygiene and cold attitude of staff they lacked general confidence of patients. Despite these shortcomings, the JMPC and the CHK are catering healthcare needs of millions of poor and low-income people belonging not only to Karachi, but also other parts of the country, and a little care to improve their cleanliness and attitude of staff could make them popular and acceptable for millions of more citizens. A visit to both hospitals would tell volumes about the lack of seriousness of administration towards proper hygiene and more importantly to the vital issue of infection control. It is regrettable that two manholes on the main road leading to the JMPC main building, and a gutter each in front of the National Institute of Cardiovascular Diseases and the National Institute of Child Health are without covers. The corridor between the department of thoracic surgery (Ward-19) and ENT department (Ward-15) at the JMPC is littered with tones of construction debris and refuse. The primary objective of any hospital is not only to properly diagnose and treat patients, but also control infection to ensure safety of patients, their attendants and visitors, as well as, doctors, nurses, paramedics, other hospital staff and medical students. The stay of patients in government hospitals is longer as compared to private hospitals, due to the lack of strategies to cope with hospital infection result in delayed recovery of patients. Sometimes a patient is cured from one disease, when he catches another infection due to unhealthy atmosphere at hospitals. It is common practice in our major government hospitals to rely on heavy use of antibiotics, while this costly dependence could be easily reduced if proper infection control strategies are carried out. Even improved general cleanliness and sanitary could bring a substantial difference. According to experts, patients contract infections at the hospital in many ways, including surgery, bacteria-ridden catheter tubes, unhygienic conditions and most importantly unwashed hands. The excessive use of antibiotics in our hospitals is directly related to higher rate of infection due to improper hygienic conditions. It is said that some 70 per cent of the bacteria that cause hospital-acquired infections are resistant to at least one of the drugs most commonly used to treat them. People infected with drug-resistant organisms are more likely to have longer hospital stays and require treatment with second or third choice drugs that might be less effective, more toxic and more expensive. Antibiotics kill the bacteria that cause infections. But today, antibiotics are not working as well as they did in the past because the bacteria have started resisting the antibiotic. This is called antibiotic resistance. When antibiotics are misused, overused or underused, the bacteria causing the infection can become stronger. The infection that is being treated may get worse and require a more powerful antibiotic in the future. The more powerful antibiotics reserved for treating only the very serious infections in the past are now being needed to treat more common infections. It is common observation that majority of toilets and washrooms in OPD areas as well as wards are extremely dirty in both hospitals. Generally, they lack proper plumbing work and their water taps and basins not in working condition. There is no provision of soap for washing hands. Proper sanitation can prevent common infections. It is extremely necessary that hospitals have flawless sanitation. It is a must that patients, their attendants and hospital staff must wash their hands with soap after using toilets, as human excreta always contain large numbers of germs, some of which may cause diarrhoea. To ensure proper sanitation in hospitals, there should be sufficient toilet facilities for patients, their attendants and hospital staff. There must be a wash basin with clean water and soap facilities. It is strange that these hospitals are spending millions of rupees monthly on drugs, but they are not ready to spend a few hundred rupees to provide soap for washing hands in their toilets. The corridors and waiting areas of almost all government hospitals in Karachi need cleanliness. In corridors and staircases of the JPMC some empty tins of ghee and some plastic drums are seen to dispose off refuse and litter, but these dirty and uncovered garbage bins create more infections. Free roaming of peddlers, tea and juice sellers, hawkers and even beggars in corridors of both the hospitals offer a pathetic picture of their administration. These peddlers even roam into wards freely during visiting hours. The administration of these hospitals needs to focus on effective infection control through improved cleanliness, especially in corridors and toilets. A more polite and caring attitude of hospital staff, especially junior doctors, technicians, paramedics and clerks could further improve efficiency of these hospitals. (Dawn-14, 12/03/2007) 48 Law soon to regulate hospital business KARACHI, March 13: Sindh Health Minister Syed Sardar Ahmad has said that an ordinance meant to regulate the business of hospitals in the private sector will be promulgated soon. He was talking to newsmen after attending a presentation about universal health insurance coverage for the inhabitants of Sindh, which was held in his office on Tuesday. The minister said that there was a dire need to have some legal provisions in the case of private hospitals, clinics and diagnostic centres in the province as complaints about their unethical and unsafe operations were on the rise, but the government was not in a position to initiate legal action against defaulters in the absence of relevant laws. “My office receives complaints against private hospitals almost every day but I cannot order any inquiry,” he said, adding that the final draft ordinance to regulate and accredit private healthcare facilities was with the Sindh governor and promulgation was expected any moment. Coming to the introduction of the social health insurance scheme in Sindh, the minister said the government felt that such an insurance coverage would help provide better health facilities to the people of the province. He said that an insurance coverage policy was already in place for the Sindh Secretariat employees, while the other employees of the government, which numbered around 0.45 million, also needed similar coverage. He said the government would not charge insurance fee from the employees and the masses, but would contribute on their behalf to the insurance company. It is understood that the Sindh government will spend some amount additional to what it is already paying for medical allowances and reimbursement of medical bills, he said and added that a lot of money was available with the Zakat Funds, Baitul Ma'al, besides the funds coming in from international development banks. Though a lot of relevant working for the introduction and implementation of the insurance coverage was to be undertaken, “I think the government could start with some sort of pilot projects, focussing largely on rural area inhabitants”. The presentation meeting was attended by the secretaries of various government department, former health minister Dr S. M. Rub, and the chairman of the sub-committee on health insurance, Abdul Karim Lodhi. A team of the insurance company, which is already running a social health insurance coverage pilot project in the NWFP, maintained that in the first phase of the programme a pilot project could be introduced for Sindh employees for 3-5 years period. The consultant of the insurance firm, Dr Bernd Appelt, however, indicated that some statutory sickness fund would also be needed to be established for even availability of insurance funds, in addition to having mandatory accreditation of health providers in the public and the private sector and legal framework for hospital management. The insurance coverage will be aimed at providing good quality health-care to employees and their dependents without making them to pay some thing additional, while on the other hand government would also need not to pay additional amount for specialised hospitals. It was further said that the social health coverage scheme will ensure flow of additional money to government teaching hospitals, improved health services for employees. At present Sindh government is spending three million rupees for social health insurance cover for about 27,000 Sindh secretariat employees and their dependents. (By Mukhtar Alam, Dawn-17, 14/03/2007) Two more dengue cases confirmed KARACHI, March 13: The president of the Infection Control Society of Pakistan, Dr M. Rafiq Khanani, said on Tuesday that two more cases of dengue fever were confirmed during the last week in the city. He told Dawn on Tuesday that he had reports that two blood samples of patients were detected positive for dengue virus and as such the number of dengue positive cases reported during the last 40 days reached five in the city. He said two patients admitted with the history of high fever and rashes at a private hospital had also been confirmed as dengue positive in the last fortnight. However, Dr Shafquat H. Abbasi, additional secretary health and focal person on dengue disease in the Sindh Health Department, said no hospital confirmed new dengue cases in the recent days, except three patients who were given treatment at the AKU and found dengue positive in February. He said a patient with the history of high fever had been admitted to the Civil Hospital, but his blood report was awaited, while personnel of the Ziauddin Medical University on Tuesday informed him that two patients with symptoms similar to that of dengue fever patients were detected dengue negative cases. However, Dr Rafiq Khannai feared that there were possibilities of two to three folds increase in the numbers of dengue fever or dengue hemorrhagic fever cases this year. He stressed that a system should be established under which not only the data pertaining to dengue were collected but at the same time response and interventions should also be ensured. (Dawn-17, 14/03/2007) No skin off their backs which is why Civil hospital needs a bank KARACHI: It's not something patients can buy but it's really expensive and comes from their own body: skin. And nothing is more precious to a burns victim. "The mortality rate could go down from half to one-forth if we get a skin bank," said Dr. Abdul Sami, a plastic surgeon at the burns centre, at Civil Hospital Karachi. He and his colleagues are pressing for a skin bank where a patient's skin can be taken from an uninjured part of their body, grown and then applied to the damaged area. "We are desperate for a skin bank to save the lives of patients." A skin bank would keep and cultivate different types of skins which could be provided to the patients with different degrees of burns. 49 The number of burns cases are increasing at an alarming rate, he said, adding that most of them were third-degree burns cases. These patients in particular, and those with more severe burns always need skin cultures. In a skin bank, 'culture skin' is produced from a small part of unaffected skin from the patient's body and grown to one meter long over the course of a month. During the initial one month after a patient's surgery other types of skin are used to cover the burnt part of the body and then the cultured skin is applied. Any type of skin has to be applied so the patient doesn't lose body heat from the exposed area. Some types include biological skin, bovine skin, bio-synthetic skin (one type of which is Integra) and bio-bran skin. They can be used for up to two weeks but are extremely expensive. A 20 by 60 cm piece of Integra costs around 700 pounds, said plastic surgeon Dr Shariq Ali, head of the burns centre. He also clarified that such skins were not available in Pakistan. “Normally, we have to pay up to Rs 100,000 for the bandages for burns patients each month,” he said. “How can we possibly afford the Integra type treatment.” Pig skin is used abroad, but is for obvious reasons not an option in Pakistan, he added. "For 40 to 50 percent of burns cases, these skins are a must because the patients will die without them from the loss of energy from the exposed area," he said. Doctors need to reduce water and electrolyte losses for burns patients by covering the exposed area. "The concept of using Amniotic membranes for burns patients is twenty-five years old but we don't even have this technology." Skin is not only required for major burns injuries but can also be required even for one percent burns cases on the hand, neck, genital organ or any other sensitive part. In fact, if these areas are not covered, the patient could be handicapped for life. A burns patient requires three times more calories than an uninjured person. Sami said that the doctors at the burns centre had the know-how for a skin bank but lacked the facilities, which was the only impediment. "In the meantime, our centre uses the method of tangential excision in which we take unaffected skin and graft it to the burnt part," he said. Grafting reduces deformities caused by an uncovered burns wound, added Dr. Saleem Akhtar. (By Farhan Ahmed, Daily Times-B1, 16/03/2007) Epilepsy patient dies KARACHI, March 16: After undergoing six months of treatment, epilepsy patient Aariz Ali Shaikh, died at the Aga Khan University Hospital in the early hours of Friday. His aggrieved father, Khurshid Ali Shaikh said Aariz, 15, was his only son. He was buried after Friday prayers at Azizabad graveyard. He said he still maintained that his son walked into the hospital and turned into a complicated case due to negligence of the hospital. He added that he and his family would sue the hospital. The family, according to Mr Khurshid, visited Aariz on Thursday and was happy to see him breathing naturally. The father said around midnight he was called by the hospital to come. He said his son breathed his last before them. He demanded that a medical board, constituted by the health department, should furnish its report without any delay. Sindh Health Secretary Noushad Shaikh said the medical board had not submitted the report to him till Friday. The AKU hospital spokesperson said Aariz in an acute epileptic state was admitted in September 2006, directly to the ICU through AKUH Emergency. For nearly six months he was kept alive on a ventilator. The official said it was disappointing that the hospital’s compassion had been responded with distorted facts and false allegations. (Dawn-19, 17/03/2007) A basic right By Dr Shershah Syed To get free primary and emergency healthcare services are the basic right of all the citizens of Pakistan. The Constitution of Pakistan guarantees this right to all the people living in the country. All previous governments claimed to work towards securing these rights for the people but had no political will and desire to change the situation. They did a lot of lip service to improve the condition of common patients and spent millions of rupees for the benefit of vested interest groups. Even now millions of rupees get wasted on the government’s family planning programmes, family health projects, the establishment of kidney centres, government funding for unplanned liver transplant programmes, and the foundation of substandard medical universities, and may also go waste on the construction of medical towers in Karachi and Islamabad worth multibillion rupees. It seems that from the Provincial Health Department to the Federal Health Secretariat and from the Health Minister to the Prime Minister, all are busy with other things instead of trying to improve the condition of poor patients. A country with a lot of resources and manpower has no planning to address the real issues of health. In Pakistan, 80 per cent Basic Health Units (BHUs) and 70 per cent Rural Health Centres (RHCs) are not functional. A majority of Mother and Child Health Centres (MCHC) and hospitals are understaffed and are not providing the required services. Because of a poor healthcare system in our country, one child dies every minute from EPI diseases, diarrhea and acute respiratory infections. Four hundred thousand (400,000) infants die in their first year of life every year, 40,000 young women die because of the pregnancy-related complications and about 350,000 women suffer from maternal morbidity. Eighty per cent of births take place at home with no or unskilled birth attendant. Pakistan stands at number six with a very high prevalence of tuberculosis in the world (177/100,000). We have 500,000 of new malaria cases every year, 25 per cent of our children are of low birth weight and 45 per cent of them are anaemic because of low iron in their food or their foods is often infested with worms. Thirty-four per cent women are under weight while 65 per cent women are anaemic in child bearing age. Hepatitis B, C and HIV/Aids are on the rise. Most men, women and children have no access to emergency healthcare services in case of accidents, emergencies in cardiovascular ailments, chest diseases, and eye and head injuries. 50 What the government is doing? The government is spending millions of dollars in collaboration with Unicef, the World Health Organisation (WHO) and other national and international agencies to eradicate polio. It has systematically destroyed the EPI programme because of corruption and ill planning. The government is apparently spending money on prevention of blindness, hepatitis B, C, HIV and on many other projects without any proper planning on a long-term basis. Donor-driven projects are not addressing the real issues of the country and instead have become another institution for organised corruption. The government’s own spending on health is without any direction. Ten per cent of our population is attending tertiary and secondary healthcare centres where the government is spending its 85 per cent of health budget, while 90 per cent of our population which is supposed to attend primary healthcare centres is receiving 15 per cent of our health budget. By spending on tertiary healthcare services, mainly on salaries, construction and purchasing, the government is only serving the people with vested interest. Unfortunately, big interest groups among doctors and planners are the main beneficiary of this situation. Young, competent and trained doctors with a competent qualified paramedical staff are migrating to other countries for greener pastures. What should be done? There is a need to declare emergency in the healthcare system. The government should have a goal to activate the BHUs, the RHCs, and the THQs on an emergency basis. Instead of half-baked glorified MBBS quacks we need an army of trained nurses, midwives and paramedics. These centres should be staffed and equipped with basic things to provide care to patients with the help of health workers. The EPI programme should be strengthened and millions of dollars spent on polio should be utilised by organising EPI programmes on scientific grounds. We don’t need medical towers at the JPMC and the PIMS, neither do we need construction of medical universities, expensive vice-chancellors and advanced chemical laboratories with electron microscopes in government hospitals where the simple urine and blood tests cannot be conducted. How to activate BHUs, RHCs and THQs? Nurses and midwives are required to provide basic healthcare and EPI at BHU and RHC levels. They should be trained and skilled enough to provide preventive services to people and give primary care to patients. The Pakistan Medical and Dental Council (PMDC) should act as per requirement of our people not for the benefit of owners of private medical colleges or the politicians who are responsible for mushrooming of medical colleges. The PMDC should make a rule that all fresh graduates will work in the rural areas for one year after completing their house job. Providing a good working environment is the government’s responsibility. They should get proper salaries, residences and equipped centres with paramedic support. This force of young medical graduates with nurses and midwives can change the existing situation in Pakistan. The College of Physicians and Surgeons of Pakistan (CPSP) can also play a very effective role by implementing the decision taken by the last council of the CPSP. The council decided that the 4th year trainee of the FCPS should work for six to 12 monthx in the RHCs, the THQs and district hospitals. The government should make sure that these competent physicians, surgeons, obstetricians, gynaecologists, paediatricians and other specialist doctors enjoy a working environment where safety is guaranteed and facilities are provided to treat, manage and operate on patients. When Prof S. M. Rab was Provincial Health Minister, he initiated a plan to attach Sindh’s government hospitals to medical colleges of the province. The idea was great, but unfortunately after he left the whole plan was abolished. In Pakistan, selected district and Taluka Hospitals should be attached to medical colleges. Qualified doctors should be included in the faculty. Their salaries should be increased and they should be made responsible for the smooth running of these centres in collaboration with medical colleges and tertiary referral centres. At present, hundreds of doctors with FCPS part-I are looking for slots in different branches of medicine and have no place to go. In many teaching units the number of trainees is even higher than the number of patients in different wards. These small steps can bring revolutionary changes into the lives of our people who are living in the rural areas or city slums. (By Dr. Shershah Syed, Dawn-The Magazine-5, 18/03/2007) CDGK to introduce bylaws for hospitals KARACHI, March 18: The City District Government of Karachi will introduce bylaws in a month or so to register and regulate private hospitals and healthcare institutions and make them follow an ethical framework, said sources in the government. A city government health department official said there was no system in force at present. The CDGK feels that its responsibilities include making bylaws for private hospitals under Section 192 of the Sindh Local Government Ordinance 2001. He said the high-ups wanted measures to be taken to regulate the medical centres operating at primary, secondary and tertiary levels and save people from fleecing and negligent handling of patients. He said it was strange that the government had a system of issuing trade licences even to beauticians and barbers, but had no mechanism to regulate private hospitals in the megacity. Source privy to the draft “Regulation and Ethics for Private Hospitals/Health Institutions/Private Units and Clinics bylaws 2007” said that efforts were on not only to regulate the health practitioners and establishments in the formal sector but also to discourage quackery, control unethical medical practices, and also to curb the unethical advertisements of any product or practice/facility which was not scientifically accepted. The proposed bylaws will pave the way for classification of private hospitals according to the services they have been providing or will provide to the patients or people coming for treatment or diagnostic purposes. A hospital with more than 50 beds and providing outdoor and indoor services in major medical, surgical, obstetrical or any 51 other discipline will be considered as a major general hospital, while a hospital with single care like orthopaedic, eye, cardiac care or gyne and obstetrical care will be taken as hospital having special discipline. Under the rules, any person or group of person or company who intends to use any place for the purpose of hospital, medical institution, unit, clinics or similar purpose will be required to apply to the EDO (Health) for registration and shall also submit a block plan showing the actual area of land intended to be used and the location at which various functions, including OPD, wards, OT, etc are to be carried on. No building for hospitals, medical institutions, health units and clinics would be required to have ample parking facility for staff and visitors, separate entrance and parking facility for emergency rooms and ambulances, waiting lounge in OPD, Emergency room and in wards, emergency exists in case of fire, sufficient number of certified fire fighting equipment in each room. Moreover it would be ensured that any operation connected therewith was not likely to be a nuisance or health hazard to the people residing in the locality. All hospitals shall segregate their solid waste on the basis of hazardous and nonhazardous and notify their amount and nature to the EDO, added the source. The draft bylaws also emphasised hiring of medical and paramedical staff for hospitals, medical institutions, health units and clinics on a permanent basis or temporary as visiting physicians after verification of their qualification and registration with the Pakistan Medical and Dental Council or nursing council. The word specialist or consultant shall only be used or placed according to the qualification and experience approved by the PMDC. The EDO will have the power to cancel registration and licence at any time if a hospital is suspected to be a source of communicable and contagious disease by having an employee. (By Mukhtar Alam, Dawn-13, 19/03/2007) PMA session on dengue Prevalent indifference intensifies threat KARACHI, March 18: If the looming dengue threat is to be thwarted, groups and committees should go out and check on mosquito breeding places in neighborhoods.With the prevalent indifference, there is every possibility that dengue this year will cause more death and disease. This warning came from doctors at a scientific session on dengue organised by the Pakistan Medical Association on Saturday. The speakers included Dr Shehla Baqi, in charge of the infectious diseases unit (isolation ward), Civil Hospital Karachi, Dr Naseem Salahuddin, infectious diseases department head of Liaquat National Hospital, and PMA General Secretary Dr Qaiser Sajjad. Addressing the gathering, Dr Naseem Salahuddin said prevention was the only solution since no vaccine for dengue existed. Countries like Cuba, Malaysia and Singapore had considerably reduced dengue incidence by using public health measures. “We can do it, too, if everyone knows about the disease, vector and how to prevent and control it in homes and community. For this, government and media must do their job. People should set up committees at mohalla level for the purpose,” she said. Recalling the past dengue episode which claimed 50 lives and affected 4,500 people in Sindh, the experts expressed apprehension that this year dengue’s attack would be harsher in the absence of preventive measures. They warned that the people who had a previous history of dengue fever should be more cautious this year as they were vulnerable to a severe form of the disease. “Karachi is now a hyper-endemic area where three serotypes are present. After a fall in cases, there will be an increase in dengue cases in later months. The disease will spread to more cities and there will an upsurge in morbidity and mortality,” said Dr Naseem Salahuddin. From her last year’s experience at the Liaquat National Hospital, where 336 patients were admitted, she said male to female ratio was 70:30. She said if the patient had classical dengue symptoms, doctors should not waste time on dengue tests and start treatment. They shouldn’t show hastiness in administering blood or platelets if patient’s condition was stable and there was no bleeding. A lot of money was wasted last year on platelet kits owing to the poor management on part of doctors, she said. About the history of dengue, Dr Shehla Baqi said it was described in the 18th century and the virus was isolated in 1944. It came to Asia in 1950s and its first episode in Pakistan occurred in 1994. As the management of this infection was predominantly supportive, the emphasis should be on prevention. Dr Qaiser Sajjad said though the government aimed to launch ambitious health projects, it was not ready to spend money on provision of basic health facilities. For instance, he said, the government should set up a laboratory for viral diagnosis as none existed at present. He admitted that doctors’ mishandling caused complications in many patients last year and they needed to be educated about the disease. Fluid management was the best supportive treatment and no anti-viral and antibiotic should be given to dengue patients, he said. (By Faiza Ilyas, Dawn-15, 19/03/2007) Advertising of drugs ACCORDING to a report, the bylaws that the city government of Karachi plans to introduce to regulate private healthcare institutions will also seek to curb the unethical advertising of any product/facility which is not scientifically accepted. This is a welcome move. If one were to believe the claims made by the ads that have been appearing on various television channels, one should never worry about falling ill. The many ‘miracle drugs’ advertised make tall claims about the wonders they perform. After the availability of such easy cures, one is forced to ask why diseases are so rampant in this country. The fact is that the drugs advertised are spurious and many actually harm people’s health. Hence the need for a ban. It is wholly unethical for the media to propagate these so-called magic cures just to earn some easy bucks. 52 The impending bylaws should prohibit the publicity of any drug in the media, even if it is scientifically accepted. It is time everyone, including the government, were reminded of the importance of the Drug Act of 1976, which is still in force. To protect consumers from the onslaught of advertising by manufacturers, the law bans the advertising of drugs and treatments in the media except in medical journals that are read mainly by health professionals. This is based on the precept that in health matters the consumer is not qualified to decide about the medicines that are suitable for him, this being a decision to be taken by his physician/surgeon. Given the onslaught of the market economy and the preponderance of the advertising business, it would be ethically and morally wrong to allow the pharmaceutical companies to play with the public’s health by encouraging self-medication which is on the rise and which would receive a fillip if drugs are freely advertised. (Dawn-7, 20/03/2007) Contaminated water kills 200,000 children annually KARACHI, March 19: Fifty-six million people of the country do not have access to clean drinking water, and 200,000 children die of waterborne diseases every year. The situation in Karachi is not much different. The percentage of the total dissolved solids (TDS) in water samples taken from Saddar (15146mg/l), Landhi (21748mg/l) North Nazimabad (3485mg/l), Lyari (9928mg/l) and Malir (3485mg/l) is alarming as the maximum concentration of TDS allowed by the World Health Organisation (WHO) is 500mg/l. This was mentioned at a seminar held in a hotel here on `Drinking Water Quality Assessment in Karachi, Hyderabad and Kotri’, organised by the Environment Protection Agency (EPA), Government of Sindh. The Secretary for Environment and Alternative Energy Department (EAED), Mir Hussain Ali, was the chief guest on the occasion as EAED Minister Dr Saghir Ahmed was unable to make it to the event. Dr Abdul Haleem Yousafzai, a scientist, carried out the water assessment survey on the behalf of EPA for which their team collected 1000 water samples from Karachi, Hyderabad and Kotri. Sharing the findings of the survey, Dr Yousafzai said the poor water supply system and improper industrial and domestic waste disposal had added to the already worsening situation. He pointed out that the percentage of TDS and chemical oxygen demand (COD), apart from the metallic ions, was found seriously high in most areas of Karachi. The percentage of TDS in some areas of the city were: Saddar (15146mg/l), Landhi (21748mg/l) North Nazimabad(3485mg/l), Lyari (9928mg/l) and Malir (3485mg/l). Dr Yousafzai said that about 80 per cent water samples taken from Gulshan-i-Iqbal Town had fecal coliform bacteria almost 8.6 percentage points more than 30MPN/dl (a standard set by WHO). Dr Iqbal Mohammad Bhangar, director of the National Centre of Excellence in Analytical Chemistry, in his presentation highlighted how the increase in population had a direct impact on the water shortage problem. He also mentioned that 56 million of the country’s population was deprived of clean drinking water, and that almost 200,000 children died annually thanks to the waterborne diseases. Dr Yar M. Khawar, dean faculty of natural sciences Jamshoro University, Dr Zahida T. Maqsood, professor of the Department of Chemistry, University of Karachi, M. Suleman Chandio from Karachi Water Supply Board and Prof Abdul Rashid Memon, director of the Institute of Environmental Engineering and Management, also discussed various issues pertaining to the water management problems, hazards faced caused by it and possible solutions to it. Souvenirs were given to the speakers at the end of the day by the chief guest. (By Meera Jamal, Dawn-19, 20/03/2007) Negligence costs life KARACHI: A blast, inside a diagnostic laboratory near Lyari General Hospital (LGH) as it broke into intense flames due to leakage from a gas pipeline, resulted in incineration of a teenaged boy and the owner sustaining 59 per cent burns. The sources informed that Amir Hussein 16, worked as a part-time technician at the AS testing lab owned by Abid Hussain. The gas pipeline inside the lab was profusely leaking for the past few weeks. Despite lodging several complaints with the authorities concerned, the problem was not being tended to. A team of SSGC came to visit the place on March 5 and left without mending the damaged pipeline and advised the complainant to contact a supervisor named Noman. The man could not be contacted despite several efforts and the same day a fire broke into the lab. Amir who was the eldest child of his parents with three younger siblings put up a fight with death, yet succumbed to his burn injuries on the third day from the incident. Abid Hussain is lying in a local hospital in a highly critical condition with little hope of survival. There has been no word of condolence or apology from the SSGC. Both the victims belong to very modest families and yet they have been left to bear the expense of treatment without any compensation offered. The mobile of the said supervisor was still off when this correspondent tried to contact him. They have urged the govt to take the culprits to task and arrange some compensation for the families of victims. (By Asra Pasha, The News-2, 20/03/2007) Hazardous waste: hike in fees opposed KARACHI, March 20: Private hospitals paying a city government contractor for safe hospital waste management, find the yearly 10 per cent increase in fees a burden. An office-bearer of Private Hospitals and Clinics Association said on Tuesday that in a situation when a limited number of health centres were utilising the incineration plants run by the Karachi District City Government, a regular increase in charges was a burden on environment friendly health facilitators. 53 He said promotion of safe hospital waste management practices was still a far cry in Karachi due to lack of coordination among different agencies. According to unofficial estimates, the 3,500 hospitals, health centres, laboratories, and clinics operating in the city generate about 25 tonnes of hazardous waste daily, but only 125 to 140 hospitals and medical centres are availing the city government’s incineration facility or have their own medical waste burning system. As such, only 20 per cent of medical waste is disposed scientifically, while the remaining is either handled with municipal solid waste or recycled or reused for financial benefits, said a source, adding that individuals exposed to hospital waste were potential health risks. Under the Pakistan Environmental Protection Act, 1997, hospital waste falls within the hazardous waste category and institutions improperly handling it can be prosecuted, an environmentalist said. The hospital association member said that the pathetic situation could be addressed only when individuals, including doctors, government agencies and policy and law makers worked equally to ensure a safe environment for people. Since we are paying the governments, they should also favour us by deferring the 10 per cent increase very year policy. He also claimed due to this reason the city government’s incineration plant was operating at around 25 per cent of its capacity. The CDGK’s Solid Waste Management Mepartment District Officer, Khalid Javed, said this policy was approved by the then KMC about five years ago. The hospitals were initially placed in five or six categories, and minimum charges fixed between Rs1,000 to Rs5,000 per month in 2002. He said no significant improvement had been observed during this period as far as the number of hospitals utilising the government’s incineration plant was concerned. An improvement can only be expected once environmental protection agencies and city government officials coordinate with each other. He also said rules need to be improved and enforced fully. (By Mukhtar Alam, Dawn-17, 21/03/2007) Inaguration of work on JPMC tower Law to regulate drug trade on the anvil: PM KARACHI: A draft of law regarding an Independent Drug Regulatory Authority has been placed before the parliament for necessary debate and ultimate adoption. Prime Minister Shaukat Aziz, giving details of the proposed law, said it will be followed by creation of independent entities in the context of drug pricing, regulation, quality, and other factors. Prime Minister Aziz said this on Wednesday while performing the formal ground-breaking of the Jinnah Post-Graduate Medical Complex Tower. Speaking on the occasion, he said that the Rs3.3 billion project was the first of its kind of healthcare infrastructure programme initiated in Karachi by the federal government over the last 30 years. The project, to be completed in three years’ time, is envisaged to provide all medical care and diagnostic facilities under one roof tower spread over an area of around 10 acres on the JPMC premises. The Prime Minister, addressing the doctors, nurses, paramedics, and other staffers of the Jinnah Post-Graduate Medical Centre, announced an additional amount of Rs20 million for maintenance work at the facility with particular focus on cleanliness and hospital waste management. “This facility will be an icon where Hi-Tech medical assistance will be provided to complicated cases,” he pointed out. Shaukat Aziz said the present government was keen to improve the quality of life of the masses and, therefore, had adopted a multi-pronged approach with equal focus on prevention besides raising the national healthcare budget. The Prime Minister maintained that equal attention was also being accorded training and education of quality healthcare professionals besides addressing the issue of quality drugs at affordable rates. (The News-2, 22/03/2007) Strict action ordered against sale of Gutka KARACHI: The Provincial Police Officer, Sindh, Jehangir Mirza has expressed deep concern over the reports being received from the press and other sources that the sale and production of ‘Gutka’ and ‘Babul’ is going on unchecked. Mirza said that directives were already issued for legal action against the menace but news stories being published in various newspapers shows that the nuisance is still in progress. He has once again ordered the Capital City Police Officer, Karachi and Regional Police Officers of Hyderabad and Sukkur to take immediate legal action. Also ensure that the sale and production of ‘Babul’ and ‘Gutka’ is brought to an end. Furthermore, they should personally monitor the action taken besides proper coordination with the city and district nazims and the civil society organisations to make the campaign more effective. (The News-4, 22/03/2007) ‘City to have world class medical tower in 3 years’ KARACHI: Prime Minister Shaukat Aziz performed the formal ground breaking ceremony of the Jinnah Postgraduate Medical Complex (JPMC) Tower in Karachi on Wednesday. The project, which is to be completed in three years, is designed to provide all medical care and diagnostic facilities under a single roof. It is spread over an area of around 10 acres of land within the JPMC premises. Speaking on the occasion, Aziz said that the Rs 3.3 billion project was the first of its kind in the healthcare infrastructure programme initiated in Karachi by the federal government. “This facility will be an icon where hi-tech medical assistance will be provided to complex cases,” he said. He announced an additional amount of Rs 20 million for maintenance work at the facility with particular focus on cleanliness and hospital waste management. 54 The prime minister said that the present government was keen to improve the quality of life of the masses and had therefore adopted a multi-pronged approach with equal focus on prevention and on raising the national health care budget. Referring to the scheme for across the board accessibility of masses to potable water, hepatitis, HIV/AIDS and TB control programmes, he said that the government’s basic strategy was based on prevention, but equal attention was being given to training and education of quality health care professionals and to the provision of quality drugs at affordable rates. Aziz also said that major health sector reforms were underway. “A draft law regarding the formation of an Independent Drug Regulatory Authority has been placed before the Parliament and it will be followed by the creation of independent entities for drug pricing, regulation and quality among other issues,” he said. The JPMC’s doctors, nurses, paramedics and other staffers were present on the occasion. A Sofitel Hotel in Clifton will be built by industrialists Siddiq Sons and Yunus Brothers at a cost of three billion rupees on the plot of the former MidEast Hospital and the prime minister performed its ground-breaking ceremony Wednesday at Governor House. “We need not only a 5-star but also 4-, 3- and 2-star hotels as well to suit various categories of people,” he said. Two other projects were also on the agenda, Textile City and the JPMC Towers. Earlier, Prime Minister Shaukat Aziz chaired a meeting to review the law and order situation in Sindh soon after his arrival from Gwadar. Also, Alladin City, a complex of resorts, will be developed at an hour’s drive from Karachi. It will have a port and a private airport. The ceremony was attended by Governor Ishrat-ul-Ebad, Chief Minister Dr. Arbab Ghulam Rahim, Federal Minister for Tourism Nilofar Bakhtiar, Provincial Minister for Labour and Industries Adil Siddiqi, Accord Group Middle East Managing Director, Christophe Landais and a large number of industrialists, investors and financiers. The Sofitel Hotel, is reflective of the ever-increasing trade ties between Pakistan and France, the PM said, adding that visitors for religious tourism will be given a good package with a liberal visa policy. He said Lahore is also going to have new hotels which are now under construction. The PM declared that whatever the government will do, it will do within legal and constitutional bounds. He referred to protest demonstrations and rallies by lawyers and said the Sindh administration had handled the situation efficiently. (Daily Times-B1, 22/03/2007) Healthcare ordinance KARACHI, March 22: The Association of Private Hospitals and Clinics has called for early promulgation of an ordinance to regulate functioning of private sector healthcare centres in the province. A meeting of the association chaired by its President Dr Muhammad Ali Shah observed that the draft of the proposed ordinance had been forwarded to the Association by the provincial health secretary. The draft had since been endorsed by the APHC, said a press release. The meeting also condemned all those forces which were trying to distort the draft. The meeting reiterated its unanimously view that there should be legislation to monitor the functioning of all hospitals in order to improve the standard of healthcare. It said that the monitoring body should be a self-regulatory authority and should have representation of all stake-holders, both from public and private sectors.— (Dawn-17, 23/03/2007) Moving fast on the polio front THE NWFP health authorities’ inability to deal with Maulana Fazalullah of Swat whose rabid views on polio vaccination is threatening the lives of those who aren’t getting immunised is disappointing. It is imperative to rein in this cleric who is carrying on a campaign against polio vaccination by calling it an insidious western sterilisation device meant to restrict the world’s Muslim population. He is not alone in this ridiculous insinuation but he seems to be the one causing the most problems. Last month, around 1,000 children were not immunised during an anti-polio drive, their parents having come under the influence of the cleric’s nonsense. According to a health official, one affected child can put as many as 2,000 others at risk. The severity of the problem makes it incumbent on the government to step in and sort the matter out immediately. On Thursday, the provincial health minister said that a high-level delegation would speak to the cleric and try to bring him on board the vaccination campaign by telling him that it is essential to save children’s lives. In other parts of the province, some headway was made when clerics were convinced by jirgas, which had been approached by health officials, to explain that there was nothing wrong with polio vaccination. Then in September last year, the government got a fatwa passed by respected members of the ulema who endorsed the vaccination drive. Armed with all this, the government should take on those opposed to vaccination. What it needs is a steely resolve. It should try to engage Maulana Fazalullah in a dialogue but if that does not work it should take firm action against him, like dismantling his illegal radio station. It must do it all very fast as the detection of each new polio case endangers many. (Dawn-7, 24/03/2007) Ibad bans licences for new medical stores KARACHI, March 24: Sindh Governor Dr Ishrat ul Ibad Khan on Saturday ordered imposition of a ban on issuing licences for new medical stores in Sindh. A well-placed source said the governor gave this order to control sale of fake drugs in the province and suspend issuing new licences to medical stores or chemist shops till a strategy was evolved to ensure enforcement of Federal Drug Act. Speaking at a meeting on the sale of fake or spurious disease in Sindh, Dr Ibad called for strict vigilance of medical stores. He directed the concerned quarters to prepare a strategy by next week to control the manufacture and sale of fake drugs in the province. The meeting was attended by health minister Syed Sardar Ahmed, Sindh Ombudsman Yousuf Jamal, health 55 secretary Naushad Sheikh, law secretary Ghulam Nabi Shah, DG Health Dr. Hadi Bux Jatoi and representatives from federal health ministry. According to the source, there are 25,000 medical stores in Sindh. Under devolution of the government, now licenses are issued by the EDO at district level, but monitoring is not done by the district or city government. Drug officers belonging to the federal and provincial governments, whose number is limited, inspect the medical stores and collect samples of drugs for testing. Karachi has only six drug inspectors, who report to the provincial health department, while their salaries are paid by the city government. Under the law, the provincial health department is not empowered enough to take action against the quarters involved in manufacturing, packing or refilling spurious or substandard drugs. The health authorities have to lodge an FIR with the police. The governor also directed to review possibilities of outsourcing the drug inspection system. He said chemists selling fake drugs should be taken to task and given exemplary punishment. He was of the view the concept of wholesale chemists be done away with and only distributors and retail shops be permitted to sell medicines. Dr Ibad also stressed the need to upgrade drug testing laboratories in Sindh and to increase their numbers. He also instructed to compile the data of all chemist shops. (By Mukhtar Alam, Dawn-17, 25/03/2007) City has only 13 food inspectors for 15 million people KARACHI: The Regulation and Quality Control department of the city government has only 13 food inspectors to monitor thousands of shops and a huge list of daily commodity items. The summary to induct more officials had been pending for over eight months now. The shortage of staff not only encourages adulterators, but also forces innocent citizens to use substandard items which lead to a number of diseases. A lot of food inspectors were also transferred to other official assignments (such as monitoring polio vaccination drives in different towns) after they failed to perform their duties. Moreover, the department has only one laboratory for testing items collected, and even these operations are on a very limited scale. The District Officer (DO) Regulation and Quality Control, Dr Abdul Jabbar, told Daily Times that the previous district officer had moved a summary to induct more staff in the department some eight months ago but no action had been taken thus far to resolve the issue. “Due to the shortage of staff, we barely manage to respond to public complaints regarding adulterations and quality checks. Inspectors not only redress public complaints, but they also visit different markets regularly. Moreover, they make surprise raids to monitor quality control,” Jabbar said. Apart from hiring more inspectors, the DO had also proposed to increase license fees for businesses and to include more commodity items in the official list in order to meet current needs. The executive district officer (EDO) Health, Dr A.D. Sajnani, said that the department was working on this. The number of inspectors would be increased to 36 in the first phase, and two food inspectors will be deputed in every town to monitor quality control, he said. Responding a question about whether food inspectors were trained, Sajnani said that they were trained in Lahore earlier. After the establishment of a training institute at the city government’s Leprosy Hospital in Mangophir, however, food inspectors and sanitary inspectors will be trained there. This institute, the EDO said, would be made functional from the next fiscal year. Currently, the city government issues food quality licenses under the “West Pakistan Pure Food Ordinance 1960” which was adopted in 1965. Each item is charged at the rate of Rs 10-20, as per the Act, which has not been revised for more than 40 years. The Regulation and Quality Control department is responsible for checking the quality of ingredients in daily commodity items, including edible oil, spices, salt, pulses, fresh milk, yogurt, confectionary items and bottled water. Staff collect samples during field visits, and send it to the laboratory for testing. If test reports point towards adulteration or abysmal quality, challans are issued to shopkeepers who submit fines in the relevant court. Shopkeepers interviewed by Daily Times complained that food inspectors visited their jurisdictions only for collecting extortion. People who fail to fulfill the inspectors’ demands are threatened with dire consequences, including police raids. “I have not seen any food inspector for the past six months. I’ve heard of some of them visiting the neighbouring market once a month, though,” Zakir Ali, the proprietor of a general store in Empress Market, said. Farid Malik, a shopkeeper in Gulshan-e-Iqbal, said that he had not come across any food inspections in his area. In Baloch Colony, a sweet confectioner said that the area food inspector visited his shop, as well as neighbouring outlets once a month (or sometimes after two months) to “collect his share” (extortion). A majority of the shopkeepers interviewed said that they had not seen any of the 13 inspectors of the CDGK. They therefore had no reservations about selling substandard daily commodity items. (By Jamil Khan, Daily Times-B1, 25/03/2007) Tuberculosis up by 30pc in Attock ATTOCK, March 25: The city nazim Attock has expressed concern over the phenomenal rise in cases of Tuberculosis (TB) and urged the government to take strict measures to control it and ensure proper treatment of those infected with the deadly disease. Rana Shaukat Ali Khan expressed these views while speaking at a rally, arranged by the district TB Association (DTA). The rally, in which a large number students, teachers, doctors, lawyers, social workers, religious and political figures participated, started from the Madni Chowk and ended at the Kutchery Chowk. 56 The nazim said the incidence of TB was increasing in the district due to a number of reasons. One was that the district lacked any hospital exclusively devoted to the treatment of TB. Another reason was the absence of precautionary measures to prevent the spread of the deadly disease. Reports indicate a 30 per cent increase in the number of TB- infected patients at the district headquarters (DHQ) hospital Attock this year as compared to last year, he said. Elaborating on the reasons for the spread of the disease in the district, he said one factor was the influx of a large number of Afghan refugees and their commercial activities. They had established carpet weaving centres in residential areas exposing people to fumes from chemicals used in the dying process. These fumes were not only injurious to ones lungs but also caused bone damage. There was no mechanism to dispose of the residual chemicals, which were left clogging drainage lines outside residential areas. He said that in the far-flung areas of the district, TB had reached epidemic proportions due to poverty, an unhygienic lifestyle and the use of contaminated water for drinking purposes. “The increase is really alarming,” he warned and blamed the local health authorities for not paying enough attention for treating patients and controlling the spread of the disease. He pointed out that there was not a single TB hospital in the district. Nor were there any isolated wards at the DHQ hospital Attock or the five tehsil headquarters (THQ) hospitals. Ironically, the only exclusive ward for TB at the DHQ hospital Attock was closed down without any rhyme or reason and was now being used as to store drugs by the health department, he deplored. As a result, TB patients were being admitted to other wards of the hospital, posing a huge health risk to the other patients, who were needlessly being exposed to this deadly disease, he said. Negligent behaviour has also been observed at other health care institutions in the district, including the THQ hospitals and rural health centres, he said. Even an illiterate man knows that the TB infection spreads because of close contact with a TB patient, therefore, it imperative that the disease is treated in isolation, he stressed. (Dawn-2, 26/03/2007) PMA welcomes ban on medical stores KARACHI, March 25: Pakistan Medical Association (PMA) Karachi Chapter on Sunday welcomed Sindh Governor Dr Ishratul Ibad Khan’s decision to ban licenses for new medical stores. The PMA demanded that the presence of a qualified pharmacist be made mandatory for medical stores, and licenses of all medical stores in Sindh having no qualified pharmacist should be cancelled henceforth. PMA Karachi General Secretary Dr Qaiser Sajjad, in a statement, said that more than 95 per cent of medical stores in Sindh, especially Karachi, were being run by non-qualified persons, which was a great threat to the health and lives of people. The PMA office-bearer said that no check on medical stores had resulted in a rising trend of self-medication, as all types of drugs were available in these medical stores, without even the production of a prescription from a registered medical practitioner. He said that in many cases non-qualified staff of medical stores was involved in quackery, selling fake and expired medicine and even selling wrong medicines. He said that open sale of sleeping pills was behind many incidents of suicide, especially amongst women. The Pakistan Medical Association (PMA) demanded that a compressive survey on medical stores should be started in the whole province, including Karachi, and the licenses of those medical stores running without the services of qualified pharmacists should be cancelled. (Dawn-14, 26/03/2007) Establishment of brain bank stressed KARACHI, March 25: There is a need for establishing a brain bank in the country for collection of human brain material for research and this goal can be achieved in collaboration with local neuroscientists, pathologists, neurologists and neurosurgeons. These views were expressed by the vice-chancellor of the University of Karachi, Dr Pirzada Qasim Raza Siddiqui, on Sunday while speaking at the inaugural ceremony of the first IBRO Associate School of Neuroscience Pakistan, organised by Dr Panjwani Centre for Molecular Medicine and Drug Research (PCMD), KU, in collaboration with the IBRO and the Aga Khan University Hospital at the auditorium of International Centre for Chemical and Biological Sciences (ICCBS), KU. Speaking on the occasion, Dr Pirzada said that in the last few decades experts in basic research in the field of human brain pathology had come to rely more and more on the availability of human brain specimens. “Although alternatives to using human brains, such as animal experimentation, animal tissue culture and computer simulation are widely used, ultimately we need human brain tissue, whether for understanding the basic structure of the brain for investigating the changes that occurs in the common neuropathologies”, he added. Dr Pirzada said that brain banks had been established around the world to provide such tissues, but it was becoming more and more difficult to obtain the material. He said that Pakistan was now affiliated with the International Brain Research Organisation (IBRO) and would avail the advantages of being the member of this prestigious international organisation. He said he was pleased to announce that a society for neuroscientists of the country named Pakistan Society for Basic and Applied Neuroscience (Pasban) would be launched during this mega event, which would help boost research activities in 57 the related area. IBRO chairman Dr Laurence Garey said that the IBRO was an independent international organisation dedicated to the promotion of neurosciences around the world. The IBRO was founded in 1960 in response to the growing demand from scientists in many countries. The IBRO represents the interests of nearly 61,000 neuroscientists in 112 countries around the globe. Over the years, IBRO has set up a number of active programmes to stimulate international contacts in brain research. Symposia and workshops are sponsored on the basis of competitive applications. Under the publication programme, the IBRO publishes the journals ‘Neuroscience’ and ‘IBRO NEWS’. The IBRO membership directory is also available on its website. The organisation also offers post-doctoral fellowships and travel grants to students from less-favoured countries, Dr Laurence said. The acting director of the ICCBS, Dr M. Iqbal Choudhary said that it was impossible to understand the biological functions of brain without having the knowledge of chemical processes occurring in that part. Pakistan is the sixth most populous country of the world, having terrible rate of mental diseases, including epilepsy, schizophrenia, multiple sclerosis (MS), Alzheimer and Parkinson disease, he added. Presenting the vote of thanks, Dr Fatima Shad of the PCMD said that this was the first time when Pakistan was going to be part of this prestigious organisation, having active programmes to stimulate international contacts in brain research. (Dawn-15, 26/03/2007) Pesticides, health and environment PAKISTAN has basically an agrarian background and agriculture is mainstay of our economy. About 70 per cent of its population depends directly or indirectly on agriculture and approximately 68 per cent of its industries are agro-based. Pakistan possesses high potentialities to grow almost all types of tropical and sub-tropical field and garden crops in abundance. Cotton, wheat, paddy, sugarcane are the major crops of the country other than the fruit and vegetables. Use of pesticides is increasing day by day. Around 45 multinational companies in association with local agents by way of import, and other 13 local pesticide manufacturing plants are meeting the pesticide requirements of the country. As the use of pesticide in controlling pests to avoid crop losses is increasing, number of pesticide toxicity cases also increasing so there is immense need to develop other methods for adequate plant protection. Impact of Pesticide on Health: In course of struggle between mankind on one side and insects, pathogenic organisms and weeds on the other, the newly developed chemical pesticide gave hope that the ultimate weapon had been found and these being poisonous substances were found to be quite dangerous if not handled carefully and cautiously. Pesticides however, can be categorised in groups in view of their chemicals properties, which dictate relevant sets of precautionary measures for safety and curative treatments against their injurious effects of different types and intensities. Some of the classical members of following groups are used in Pakistan: Chlorinated Hydrocarbon Pesticide: (1) Aldrin, (2) BHC (lindane/gammexane), (3) Chlordane, (4) DDT, (5) Dieldrin, (6) Endrin, (7) Heptachlor, (8) Thiodane. Organophosphate Group: (1) Ethion, (2) Usathion, (3) Arathion, (4) Thimet, (5) Imecron, (6) Formathion, (7) Azodrin, (8) Nexion, (9) Arbicron, (10) Diptrex, (11) Diazinon, (12) Imidan, (13) Lebaycid, (14) Malathion, (15) Methyl Parathion, (16) Metasystox, (17) Phosdrin 18) Sumithion, (19) Nexagan, (20) Disyton / Solvirex. Pesticides industry: Presently, the basic manufacturing facilities for pesticides do not exist in the country. However there were two manufacturing units for the production of Dichloro Diphenyl Trichloro Ethane (DDT) and Benzene Hexa Chloride (BHC) in Pakistan, located at Kala Shah Kaku (Punjab) and Nowshera (NWFP). The total installed capacity of these two units for DDT and BHC were 2,020 and 2,310 MTPY respectively. These units are closed for last many years because both pesticides have been banned for use in Pakistan. The problems need to be addressed by the state as officially banned pesticides are still available in the local market. Pesticides used at present are either organic or inorganic in nature. Organic group contains natural plant oils, nicotine and pakerthsun as natural pesticides. It also contains synthetic pesticides as compound of chlorine like DDT, BHC and endrin, aldrin, dialdrin, heptachlor etc. Twenty four pesticides, including above compounds, have been banned in Pakistan. Since pesticides were subsidised ( their imports till 1979), 75 per cent share was passed to private sector while the government retained remaining 25 per cent. However, since February 1985, all subsidies were withdrawn and private sector was fully made responsible for imports, distribution and sales of pesticides throughout Pakistan except Balochistan province. Pesticides were imported under generic names from 1991. By the year 2000, the local formulation exceeded the imported pesticides several times. Production capacity: Presently, the installed capacity for the formulation of various types of pesticides is more than the local requirement. There are about 40 companies involved in the formulation of pesticides. The local formulation product includes liquid pesticides, powder and granules that contribute 67 per cent in the local market. Most of the raw materials including active ingredients as well pesticides in finish form are being imported. The sector growth rate is three per cent. Imports of pesticides: Liquid pesticides account for 95 per cent of the total consumption. Remaining five per cent are powder, dust for granules. Insecticides account for 88 per cent, herbicides 11 per cent and fungicides one per cent of the total pesticides used for plant protection. Additional quantities of pesticides are used for public health and household. Future Prospects: This sector lacks production of base chemicals. Few ingredients are produced in Pakistan especially base chemicals used in the pesticides for the protection of cotton crop. Around one billion dollar (Rs60 billion) is spent on the cotton crop and others every year from sowing to harvesting. The share of plant protection for the cotton crop is 33 per cent or $ 0.33 billion. This shows the importance and need for local pesticides industry. Ill effects of pesticides on health and environment.: Due to extensive use of pesticides there is an extensive need of: risk 58 identification. After determining and identifying the risk factors and its impact on health and environment we have to plan to search appropriate measures for reduction in the use of pesticide without affecting the crop quantity and quality;safe use and handling of pesticides; development of appropriate alternative methodology; study of acute and chronic effects of pesticides on health and environment. During the past decade, the public has grown concerned about agricultural pesticides use. Exposure to pesticides, even at low doses, is associated with a wide variety of health effects, and these compounds are now commonly found throughout our environment. Despite some important advances, federal pesticides regulatory programmes have failed to prevent an overall increase in pesticides use, risks, and reliance. This not only threatens public health and the environment, but it puts farmer’s livelihood in jeopardy. Farmers using the pesticides that are legal and safe and also effective for crop production, later come to know that they are discovered to be hazardous. In the long run, both farmers and public will be the best protected by a fundamental restructuring of pesticide policies and agricultural and education programmes to minimise pesticide use and rely instead on non-chemical, biologically-based methods that prevent pest problem. A wide variety of alternative agricultural tools are available to reduce pesticide use and reliance, including those used in integrated Pest Management (IPM) and sustainable organic farming system. Various alternative pest management techniques are: Scouting and monitoring for pest and natural enemy population levels; precision pesticides application equipment; rotating crops and planting cover crops; switching to biologically-based pest control products: conservation tillage, irrigation management, and soil-building. (By Dr. Aftab Turabi, Dawn-Economic & Business Review, Page-III, 26/03/2007) Ebad for setting up hospital regulatory body KARACHI: Sindh Governor, Dr Ishratul Ibad has directed the expedition of legislation that would bring the government as well as private hospitals and clinics within the ambit of legal regulations. He also directed the provision of healthcare facilities to the people in an improved manner. A high-level meeting held at the Governor House under the chairmanship of Ishratul Ibad reviewed the progress in this regard, said a statement here on Sunday. Senior Provincial Minister for Health Syed Sardar Ahmed, Advocate General Anwar Mansoor Khan, Principal Secretary Muhammad Saleem Khan, Secretary Health Dr Naushad Shaikh, Additional Advocate General Qazi Khalid Ali, Special Secretary Javed Hanif and others were present for the meeting. Ibad directed that regulations for maintenance of better environment at Government hospitals be formulated, and also that the an autonomous authority for private hospitals and clinics be established. The provincial secretary briefed the meeting about the progress made in regards to the above directions of the Sindh Governor. It was informed that a well-reputed person associated with the profession of medicine will be appointed as chairman of the proposed authority, while the vice chancellors of Dow Medical University, Liaquat Medical University, Jamshoro and one from a private medical university will constitute its members. Representatives of the Pakistan Medical Association, Dental Association, Private Hospital Association and Association of Family Physicians will also be part of the authority. Steps aimed at making the management board system in government hospitals effective were also reviewed in the meeting. The Governor also issued directives for the improvement in the functioning of these boards as well as for an improvement in the performance of the hospitals. (The News-2, 26/03/2007) Damp homes could cause asthma KARACHI: Damp and mould-infested houses could be the cause of permanent asthma in children, say researchers. Poor housing conditions are already linked to the illness, but there is debate whether they cause asthma, or simply trigger attacks. Finnish researchers writing in the European Respiratory Journal say they have proved this after surveying the homes of more than 300 children, BBC reported. However, the UK asthma experts are still not convinced that mould can cause asthma. Asthma is now the most common chronic disease of school-age children, and rates have risen steadily in recent years in industrialised countries. Dr Juha Pekkanen, from the National Public Health Institute in Kuopio, suggests that as many as one in five cases of child asthma may be caused by moisture and mould in the home. His team found that the severity of asthma increased alongside the severity of the damp in living areas. In all, the homes of 121 asthmatic children were compared to those of 241 non-asthmatic children. As well as a detailed interview and allergy test to rule out specific asthma triggers in the environment, experienced civil engineers ranked all the houses in terms of the level of damp and presence of mould. Everything from leaks, condensation and damp stains to peeling on the surface of walls was recorded. Evidence of serious damp or visible mould was seen two to three times more often in homes inhabited by asthmatic children. Mould and damp in ‘non-family’ parts of the house, however, was not linked to the illness. The researchers said this was clear evidence that mould and damp caused asthma in children, as opposed to worsening or triggering attacks in children whose asthma had another underlying cause. Dr Pekkanen said, “Damp in the home does more than merely exacerbate existing asthma - it can contribute to the onset of persistent asthma.” He called for doctors to be aware of the link when treating child asthmatics. However, not all experts are convinced that the evidence points to a cause for asthma. (The News-3, 26/03/2007) 59 PMA appreciates ban on new medical store licenses KARACHI: Pakistan Medical Association (PMA) Karachi Chapter welcomed on Sunday the ban on licenses for new medical stores imposed by Sindh Governor Dr Ishratul Ebad Khan and demanded that the presence of a qualified pharmacist at medical stores should be made mandatory. The PMA further proposed that medical stores without a qualified pharmacist should have their licenses revoked. PMA Karachi General Secretary Dr Qiaser Sajjad said that more than 95 percent of medical stores in Sindh, especially Karachi, are run by unqualified people, which posed a great threat to the health and lives of patients. He claimed that the lack of regulation on medical stores had resulted in the rising trend of self-medication since people could purchase all types of drugs from medical stores without having to show a doctor’s prescription. In many cases, he said, unqualified medical store staff are involved in quackery, selling fake and expired medicine and even selling wrong medicines. The PMA demanded that a comprehensive survey on medical stores should be started in whole province. Dr Sajjad lauded the efforts of the Sindh Health Department against fake drugs and congratulated Special Secretary of Health Dr Majid for a successful raid in Mehmoodabad on the other day and recovery of Rs 15 million worth of fake drugs. (Daily Times-B1, 26/03/2007) 2.5 million TB patients in Pakistan, says WHO KARACHI: According to the WHO there are 2.5 million tuberculosis (TB) patients in Pakistan which means that every year 171 persons are infected with the disease.This was revealed at a scientific session on TB, organised by the Ojha Institute of Chest Diseases, Dow University of Health Sciences (DUHS) at its campus on Monday. The Vice Chancellor DUHS, Prof Masood Hameed Khan informed the audience that TB was considered to be an incurable disease however the advancement in medical science has made it possible to cure it if the disease is diagnosed in time. “The alarming spread of TB is due to poor health conditions, adulterated food, contaminated water and low immunity.” Prof Masood further said that in order to overcome this disease we need to launch an organised campaign against it to create awareness. “This campaign may start with the support of NGOs at schools, colleges, universities and union council levels. Media can also play an organised role in this connection,” he suggested.The Director of Ojha Institute of Chest Diseases and TB expert Dr Ashraf Sadiq informed the audience in his presentation that there were 16.2 million TB patients throughout the world. Every second, a person gets infected from the disease and thus every year some 8.5 million persons get affected by this. Developing countries are most affected by TB and Pakistan ranks 7th among the most affected countries. The speakers included eminent health experts like Dr Faizullah Shafqat, Prof Zaman Shiekh, and Dr Sharaf Ali Shah. The experts also presented their papers on TB, situation in Pakistan, TB and AIDS, TB and Diabetes, diagnosis, prevention and treatment regimes. (The News-2, 27/03/2007) 250,000 new TB patients every year KARACHI: Approximately 250,000 people develop TB every year in Pakistan. Around 75 percent of them belong to the most economically productive age group of 15-54 years, experts said Monday, during a scientific session organized at the Dow University of Health Sciences (DUHS) as part of World TB Control Day. They also stressed on the need for proper awareness of TB symptoms among physicians, as well as the general public, in order to protect people with weak immune systems. Speakers said that diabetes, HIV/AIDS, as well as other health conditions compromise the resistance power of patients, ultimately enhancing their vulnerability to the bacteria that cause tuberculosis. They also said that prolonged fever and a persistent cough which do not respond to other treatment should not be ignored at any cost. People, particularly children below the age of two years, living in crowded conditions were said to be among the high-risk groups. DUHS VC Prof. Masood Hameed Khan said that the university was thinking of mandating TB diagnosis and treatment training for all house officers and post-graduate students enrolled at DUHS. (Daily Times-B1, 27/03/2007) CHK Burn Centre lacks facilities to tackle electrocution cases KARACHI: The Burns Centre at the Civil Hospital Karachi (CHK) does not have an ICU therapist, a trained anaesthetist, or a nephrologist (to decide when dialysis should be done if the kidneys fail). The centre also does not have a tissue expander, or a useable ECG machine, Dr Abdul Sami, a plastic surgeon who works at the CHK Burns Centre, told Daily Times. All of these, Sami said, are required for treating patients who suffer from electrical burns. “Currently, we’re only able to save the lives of 25 percent of the patients who come in to the burns centre. If we had all the required facilities, however, we could save the lives of 50 percent of patients. This is the benchmark that private hospitals boast of,” Sami said. People who suffer electrical burns require a nephrologist and an orthopaedic surgeon, above everything else. Oftentimes, the shock damages the patient’s kidneys. “We try to save the kidneys by increasing the flow of urine,” Sami explained. 60 “Damage to the kidneys causes myoglobin to block the urine tubule, increasing the percentage of toxic elements in the patient’s bloodstream. Despite all of this, however, the ECG at the centre is obsolete.” The blockage of the urine flow could also result in Metabolic Acidosis, which raises the serum potassium in the blood and damages the heart. The burns centre needs a dedicated nephrologist for such patients. Moreover, a patient who’s tissues have been damaged extensively due to an electric shock needs to be watched by surgeons every second. “The patient could start bleeding from anywhere at all. For instance, if the current passes through the fingertip and travels up the arm, the patient could start bleeding from the armpits after a couple of hours or even days, indicating that tissues have been damaged all over,” Sami said. “A dressing set should be kept by their bedsides all the time, because timely dressing could save the patient’s life.” The CHK burns centre, however, does not have the required dressing sets available around the clock. “Sometimes, if some part of the patient’s body has to be amputated, an orthopaedic surgeon has to be called in from the CHK. The burns centre does not have a dedicated orthopaedic surgeon. Moreover, the CHK trauma centre is always very busy, and surgeons are not available on time. By the time they do come in, the patient is dead,” Sami claimed. Apart from all this, the centre has only one physiotherapist. The other two are ‘helpers’, the plastic surgeon said. The head of the department (HoD) at the CHK Burns Centre, Dr. Shariq Ali confirmed some of this. “We don’t have a dedicated therapist right now. It’s a gap that we’re trying to bridge,” Ali told Daily Times. “The anaesthesia department at the Dow Medical University provides us with an anaesthetist. We don’t have one working full-time at the centre.” No burns centre anywhere in the world has a nephrologist, Ali maintained. “When one is required at the CHK burns centre, however, we call them in from the Sindh Institute of Urology (SIUT). We get orthopaedics from the CHK. And while we don’t have an ECG machine, we call people in from the CHK who perform an ECG by some technical method.” “We cannot use a tissue expander due to the cost. One tissue expander costs Rs 35,000, and it isn’t reusable. It has to be thrown away after each use, and a fresh one has to be used each time.” “All these facilities are a part and parcel of the CHK and are provided by the Dow University of Health Sciences (DUHS),” said Dabir-ur-Rehman, the head of Friends of Burns Centre (FOBC), an NGO which works for collecting donation for the burns centre. “The centre has three physiotherapists right now,” Rehman said. “All the instruments are sterilized, and dressing bundles are present around the clock.” Rehman also claimed that the centre had an ECG machine, and four qualified ICU technicians present 24/7. “The plastic surgeon would have more information about tissue expanders. Orthopaedic surgeons, however, are always on call,” he said. The CHK medical superintendent, Dr Kalim Butt, denied all knowledge about any of these facilities at the burns centre. “I don’t have the details,” he said. Daily Times was unable to get in touch with the Sindh Health Minister, Sardar Ahmed, despite repeated attempts. (By Farhan Ahmed, Daily Times-B1, 27/03/2007) CHK board puts free food idea on hold KARACHI, March 27: The board of governors of the Civil Hospital of Karachi (CHK) and the Lyari General Hospital (LGH) on Tuesday deferred a proposal about free supply of food to the attendants of patients at the CHK. A source privy to the meeting of the board told Dawn that the board members were informed that an NGO was willing to arrange free meals for persons accompanying patients at the CHK in a manner similar to what was in vogue at a couple of federal government-run health institutions in the city. It was learnt that the NGO had asked for the provision of space within the limits of the CHK for the free food service, which involved some construction works as well. A couple of members observed that a team of the board should visit the premises where the NGO was already extending such services and also look into other relevant aspects in order to ensure a fool-proof system beneficial to patients, without putting the government or the hospitals under any obligation, added the source. It was also not known that what would be the definition of attendants. In addition to about 2,000 in-house patients, a number of patients visit the OPDs as well. However, a CHK press release said that the attendants of patients would be supplied with free food by the local NGO in the near future. The BoG met on Tuesday with its chairman Abu Shamim M. Ariff in the chair. Among others, Secretary for Health of Sindh Prof Noshad A. Sheikh, Vice-Chancellor of DUHS Prof Masood Hameed Khan, medical superintendents of the CHK and the LGH, Dr M. Kaleem Butt and Dr Mukhtar Khawaja respectively, Abdul Sami Khan and Kauser Pervaiz also attended the meeting. The meeting was also informed that works pertaining to an exclusive supply of electricity to the new 14 operation theatres complex of the CHK was in progress. The new complex having, among other facilities, central sterilisation department, modern television video system attached to the Dow University of Health Science auditorium to telecast the live surgery processes for undergraduate and postgraduate students will become functional next month. The meeting resolved that the Sindh Home Department will be approached for full-fledged and permanent security arrangements for the CHK and the LGH. Fire-escape staircases and other civil works related to fire emergencies or fire-fighting matters were taken up with the Works and Services Department of the government and an on ground development was likely soon, the meeting was told. The committee was also finalised at the meeting to evaluate the shortfalls or bottlenecks related to the “Accident and Emergency Centre” and “Ancillary Services Complex” of the CHK. (By Mukhtar Alam, Dawn-17, 28/03/2007) 61 USAID provides $2.7m to fight AIDS spread ISLAMABAD: The Director of the United States Agency for International Development (USAID) in Pakistan, Jonathan Addleton, has provided $2.7 million to Pakistan HIV and AIDS Prevention and Care Project (PHAPCP) by awarding grants to three organisations to help stop transmission of HIV/AIDS among the most vulnerable segments of society in Turbat, Peshawar and Karachi. Over the past year, the USAID-funded project has been helping local organisations to implement transmission prevention activities in Rawalpindi, Lahore, Multan, Karachi and Larkana. "I am very happy to announce that three new sites are being added in the current year with three new partners," Addleton said at the grants award ceremony. "With this grant, the United States reaffirms its commitment to improve the health and quality of life of Pakistani people. This is the moment to redouble our efforts to prevent the further spread of this fatal disease," he added. Though Pakistan has a low prevalence of HIV/AIDS, it faces a high risk of the disease becoming more widespread. HIV/AIDS in Pakistan has now reached the stage of being an epidemic concentrated in certain segments of the population and efforts are needed to prevent the disease from becoming widespread within the general population. (The News-5, 28/03/2007) Three trauma centres to be set up on motorway ISLAMABAD, March 28: The health ministry has planned to set up three trauma centres on the motorway where all basic facilities will be provided, including a mobile operating unit. Speaking at the inaugural ceremony of the filter clinic (OPD) at Pakistan Institute of Medical Sciences (Pims) here on Wednesday, Health Minister Mohammad Nasir Khan said this service would help save precious lives and reduce morbidity. He said the ministry in collaboration with the tourism ministry was also planning to start health tourism to invite patients from other countries to come here for treatment. Tele-medicine system is also being started in the hospital, the minister said, adding that provinces would be encouraged to start such a project. He said the government had provided all basic health facilities at Pims for patients and appreciated the hospital staff for their professional commitment and dedication. The government has focused on provision of primary healthcare facilities to the people and started several programmes in this regard, he added. Mr Khan said the government had allocated huge amount for the health sector as improvements in this sector could only be achieved through maximum allocations and investment. He said the filter clinic (OPD) would share the burden of patients with the old OPD of the hospital. It had a capacity to serve 1,200 patients daily. The clinic consists of 12 units including laboratory, ECG room, pharmacy, administration unit and waiting areas for 250 people. Pims Executive Director Fazle Hadi said several new projects had been planned by the hospital to provide better healthcare to the patients. He said the project concept (PC-I) had been prepared for installation of MRI in Children Hospital while the new medical ICU had already been established in the hospital. He said the filter clinic would be run by the Pims administration. Managing Director, Indus Pharma, Zahid Saeed said facility at filter clinic would be maintained and improvement would be carried out as and when required. The annual turnover of patients at the filter clinic will be around 350,000, he added. Besides Health Secretary Khushnood Akhtar Lashari, senior officials of the ministry were also present on the occasion. (Dawn-2, 29/03/2007) Spraying alone will not help THE city nazim has directed the health department to spray insecticide in all towns and union councils of Karachi and the work is in full swing. It is encouraging that the administration has come to recognise the importance of public hygiene and its own responsibility in ensuring it. So seriously has this work been undertaken that, we are told, abundant of fumigation material and insecticide have been procured for this purpose. Will this really help the city get rid of diseases that can be traced directly to mosquitoes and unsanitary conditions? The health officials of the city government would be better aware of how little such measures have helped in the past. A few months ago, when the city was struck by a serious attack of dengue fever, the nazim had reacted by getting the city fumigated. But the incidence of the disease did not subside until the weather changed and winter came to the citizens’ rescue. It is time our health department understood that diseases can be prevented not so much by fumigation as by draining out stagnant water, preventing water from accumulating in pits and ditches, clearing up garbage by efficient solid waste management strategies and improving the drainage of sewer water. Unfortunately this is not happening. Karachi continues to be a garbage dump and even posh areas have garbage heaps lying around. Although the city government has arrangements for garbage collection and the staff to attend to it, the work is not done because there are vested interests who prefer that the garbage is left lying around for scavengers to collect and sell cheap to the recycling industry. The sewerage system has been the victim of corruption and inept planning. The mess the rains created in Karachi last summer testified to this. All this needs a radical approach and spraying insecticide alone will not help. (Dawn-7, 29/03/2007) Proposed ord for private hospitals redrafted KARACHI: The Sindh government has prepared another draft for the establishment of a Sindh accreditation authority for private hospitals, clinics and laboratories, Daily Times has learnt. According to the sources in provincial law department, some changes were made to an earlier draft. The governor has yet to promulgate it as an ordinance (Sindh Accreditation for hospitals, nursing homes, maternity homes, diagnostic clinics, laboratories and other health providers Ordinance 2006). 62 According to the new draft, the authority shall consist of the health secretary (who will be the chairman) and the members will be the additional health technical secretary, DUHS vice chancellor, Liaquat University of Medical & Health Sciences Hyderabad vice chancellor, Isra University Hyderabad vice chancellor, Ziauddin University Karachi chancellor, Baqai Medical University Karachi chancellor, two medical experts from the interior of Sindh nominated by the governor, one representative of the Pakistan Dental Association, one representative of the radiological society, two representatives of the Private Hospitals Association, one representative of Family Physician (General Practitioner), one representative of the Pathological Laboratory Association, one representative each of the Unani, Ayurvedic and Homeopathic Association and a director. The tenure of nominated members shall be for a period of four years and the authority’s headquarters will be in Karachi. The authority’s proposed job is to inspect, audit and accredit health providers. The inspections may take place every two years to check for compliance with the provisions of the ordinance and make recommendations to the owners, directors, or administrators of the health services. A health provider already in existence shall not continue for more than six months from the date on which the ordinance comes into force unless an application for its continuance has been made under the ordinance. Any person intending to open or establish a hospital, nursing home, maternity home, diagnostic clinic, laboratory etc or any person intending that a hospital or clinic already in existence should be continued as such shall submit an application to the authority, provide all relevant information and documents and pay the fee as may be prescribed by the rules. If the authority receives a complaint it may conduct a inquiry. If the authority finds that the rules have been violated in any way it can suspend the license or certificate but not before hearing the license holder. If the accreditation of an establishment is cancelled, the affected health provider shall cease to function. If an appeal is filed, then it shall cease to function till the dismissal of the appeal. According to the amended draft, an accreditation standards for hospital fund will be set up for the authority. (By Farhan Ahmed, Daily Times-B1, 29/03/2007) Rowdy students force Fuuast closure KARACHI, March 29: Academic and non-academic activities were suspended in the Federal Urdu University of Arts, Science and Technology on Thursday following maltreatment of staff by three students belonging to a regional students organisation. The teaching and non-teaching staff said, a lab assistant asked a student appearing in the practical examination in the chemistry lab to show his identity card. The student along with two colleagues forcibly entered the laboratory and maltreated the staff. A few women teachers who were present tried to pacify the angry students. The students became even more violent and threatened to kidnap them and burn them with acid. The teachers fled scene. Earlier, the chairman, business administration was mistreated by members of the same students’ organisation. The non-teaching and teaching staff of Fuuast strongly condemned the incident and said such incidents had become a routine. They demanded that the authorities rusticate the students responsible for maltreating teaching and non-teaching staff. They warned that until action was taken, academic and non-academic activities would remain suspended. (Dawn-17, 30/03/2007) NAB arrests OT technician posing as doctor KARACHI: The National Accountability Bureau, Sindh, has arrested an operation theatre (OT) technician, Akram Nadeem, for posing as a doctor and running his own clinic. Nadeem, a Grade-9 employee at the Sindh government's Qatar Hospital, ran his own clinic called Al-Rehman Al-Raheem in Arafat Town, North Nazimabad. He had earlier been running the Hussain Medical Centre, where he not only treated patients, but also performed surgeries. Nadeem's second wife, Sumera, worked with him at the North Nazimabad clinic. According to NAB, the accused had built up illegal assets worth Rs 4.6 million through cheating and forgery. Some of the property was in his name, while the rest was in the name of his wife. NAB Sindh has obtained a 10-day remand for Nadeem from an accountability court. (Daily Times-B1, 30/03/2007) Rangers to be redeployed at civil hospital KARACHI, March 30: Sindh Minister for Health Syed Sardar Ahmed told doctors and other staff of the Civil Hospital on Friday that Director General Rangers Maj-Gen Javed Zia had assured him about deployment of Rangers at the hospital immediately after Eid Miladun Nabi (SAW). He regretted manhandling of certain hospital staff by some emotionally charged visitors of a patient in a recent incident. The minister met members of the joint Board of Governors of the Civil Hospital and Lyari General Hospital in the office of its Chairman Abu Shamim Arif. He inquired about the sanitation, health and construction at the CHK and Lyari General Hospital during the meeting. He also took a serious note of the fact that neither he was informed of the poor security at the hospital nor did the administration, including the Board of Governors, make any alternative security arrangements at the CHK. He said incidents like manhandling would not be allowed to reoccur, and said that presence of Rangers personnel on the CHK premises would be made a permanent arrangement to ensure security of both patients and staff. 63 He also urged doctors, paramedics and other staff to realise their responsibilities towards patients and discharge the same with all diligence and sincerity. The minister issued directives to the Works & Services officials to carry out repairs to improve sanitary conditions and plug leakage of pipelines on a priority basis, besides ensuring neat and clean toilets and washrooms. Noticing heaps of construction debris elsewhere at the hospital, the minister expressed annoyance and directed officials to complete all works within two months or face appropriate action. He asked Medical Superintendent Dr Kaleem Butt to get the stand-by power generator operational forthwith. He also took notice of the illegal offices of various NGOs on the hospital premises and directed the board members and MS not to allow encroachments. He appreciated some NGOs for serving meals to attendants of patients from far flung areas but advised the NGOs to written permission form hospital administration in this regard. Abu Shamim Arif briefed the minister about the BoG’s performance and mentioned that planning has already been done for varied envisaged schemes. (Dawn-17, 31/03/2007) APRIL DUHS plans city-wide TB screening KARACHI, March 31: The Dow University of Health Sciences (DUHS) will start screening the population for tuberculosis in various towns of Karachi in phases from May, said Prof Masood Hameed Khan, Vice-Chancellor of the university, on Saturday. Talking to Dawn, Prof Khan said that DUHS wanted to adopt a more practical path in the case of TB, and that was why it had planned to form a core group on the subject and undertake a massive awareness and treatment campaign. He said that initially the select group of university’s faculty members and students would go in one town of the city to test people for detection of TB and provision of necessary treatment. After detection, patients will be given options of either reporting to the Ojha Institute of Chest Diseases (OICD) for treatment and medication, or to get the facilities at their doorsteps through the DUHS teams, he added, saying that respective town nazims will also be taken into confidence and would be requested to extend relevant support. The vice-chancellor said that the university will utilize a mobile diagnostic unit, already available with it, for the purposes of sputum and blood tests and relevant radiological tests. The treatment will be extended free-of-cost, he remarked, informing that prior to the fielding of staff for conducting tests, area people will be educated on the subject and handed over relevant literature so that those in the risk group could volunteer themselves for screening against the contagious disease. Earlier, speaking as chief guest at a seminar on tuberculosis, organized by DUHS, Prof Khan said that students of Dow Medical, Sindh Medical College and Nursing Institute could get themselves registered as working volunteers in the screening campaign. He said that 22 countries of the world were most affected by TB and Pakistan was seventh on the list. He noted that organizing seminars for awareness of TB was good but there was a need to review the strategy for controlling and eradicating the harmful disease, which was largely preventable. Among other speakers, director of OICD, Dr Ashraf Sadiq, said that for ages TB was considered to be an incurable disease, but now a cure was possible if it was diagnosed at the right time. The alarming spread of TB is due to poor situation of health, impure and substandard food, polluted drinking water and low human resistance against the disease. Some of the medical practitioners made presentations on the topics of TB situation in Pakistan, TB and renal diseases, role of media and ulema in control of TB, TB and diabetes and diagnosis, prevention and treatment of TB. Professor Zaman Sheikh said that diabetics might be affected by TB because their resistance powers decreased with every passing day. If the weight of such patients decreases rapidly, they should have TB tests done, he suggested. He further said that if a person felt severe pain in any part of the body, he should not ignore it and must assure a proper check-up from any good physician because TB may be in any part of the body besides the lungs. Dr Faizullah Shafqat, Dr Nisar Rao, Dr Zafaryab Hussain and Dr Rubina Naqvi also spoke at the seminar. (By Mukhtar Alam, Dawn-17, 01/04/2007) Screening for TB THE plan of the Dow University of Health Sciences (DUHS) to screen people for tuberculosis in Karachi is an ambitious but welcome one. For a variety of reasons, the TB detection rate has remained unsatisfactory in Karachi and most other parts of the country. By mobilising medical teams consisting of doctors and students to test possible TB patients living in certain areas, the DUHS will be employing a proactive method of spreading the message of TB awareness and the need for immediate detection and treatment. If this proves successful — DUHS will start with one township — the project can be replicated by medical teams in other parts of the country. It cannot be stressed enough that TB is a highly contagious disease and unless contained at the early stage of its onset, it can be transmitted to many people living in the same neighbourhood, especially a crowded one. It has been estimated that in Karachi, where slums abound, the number of people likely to contract TB this year will be about 21,000 (32 per cent of all the cases projected for Sindh) and perhaps more if the detection rate falls short of expectations. 64 It is unfortunate that despite extensive coverage by the DOTS programme, under which a TB patient takes his or her medication under supervision and does not leave off midway through the course, the number of people with the disease in the country has continued to mount. Every year there are 250,000 to 300,000 new cases of TB while approximately 50,000 people die of what is both a preventable and curable illness. The stress must be on timely diagnosis and prompt treatment. For this, it is important that the health authorities ensure that testing facilities are accessible to all and that the cost of treatment, which can be beyond the reach of the poor man, is kept affordable. (Dawn-7, 03/04/2007) Shortage of anti-rabies vaccines PARTICIPANTS in a workshop in Peshawar on rabies were right in demanding that the government manufacture antirabies vaccine to save the lives of people bitten by stray rabid dogs. They contend that as many as 150,000 people are bitten by stray dogs every year, of which up to 5,000 people die of rabies because they do not receive timely treatment. Despite forming a National Rabies Control Programme five years ago, the government has yet to allocate funds for it which would make it functional. At the moment, most of the anti-rabies vaccines are imported, but unfortunately, they are very expensive. This explains why very few hospitals have an adequate stock of them. With the cases of dog-bite growing, it is imperative that hospitals are adequately supplied with the required vaccine. The government should consider ensuring the local manufacture of the vaccine. But until that happens, it should have a sufficient quantity of these imported as they are urgently needed to save lives. The quality and efficacy of the vaccine are important considerations in treating a condition that can prove fatal unless treated with the right kind of vaccine. WHO recommends using a cell culture vaccine (CCV) which can be imported from India. This will be a cheaper option as well. One cannot address the rabies issue without dealing with the stray dog problem. Past efforts like killing stray dogs have not worked. There is much evidence to show that this cruel method is ineffective and must be discarded in favour of animal birth control programmes. According to WHO, effective immunisation of 70 per cent of dogs in a given area can break rabies’ transmission. This can yield more promising results than the past practice of killing stray dogs. This must be adopted for better results. (Dawn-7, 06/04/2007) Oral cancer epidemic in the making KARACHI, April 6: Karachi has the highest incidence of oral cancer in the world. With the increasing number of oral cancer cases, the city may witness an epidemic in the coming years. The government immediately needs to check the widespread use of betel leaf (paan), betel nut (chalia), tobacco and their various concoctions such as gutka and manpuri, as the disease now affects the younger population. These facts came to light in discussions with different doctors. They included the Head of Karachi Cancer Registry and Aga Khan University Pathology-based Cancer Registry, Dr Yasmin Bhurgri; Head of ENT Department, Jinnah Postgraduate Medical Centre, Professor Dr Tariq Rafi; Head of ENT Department, Civil Hospital Karachi, Dr Javed Alam; Head of Pathology Department Sindh Medical College Dr Serajuddaula Syed and General Secretary Pakistan Medical Association Dr Qaiser Sajjad. Cancer of oral cavity, according to Dr Bhurgri, ranks sixth in the world in both sexes. It is the third most common cancer in men in developing countries. However in Karachi, the malignancy ranks second in both genders. The incidence, she claimed, is the highest in the world. Dr Bhurgri proved this in her research paper, Cancer of the Oral Cavity -- Trends in Karachi South (1995-2002), which was published in Asian Pacific Journal of Cancer Prevention in 2005. A total of 2,253 oral cancer cases were registered in Karachi South for the 8-year study period, accounting for 8.8 per cent of all cancer cases. The study was divided into two parts; from 1995 to 1997 and 1998 to 2002. According to the study, the Age Standardised Rates (ASIRs) per 100,000, from January 1 1998 to December 31, 2002 in Karachi South were 21.3 in males and 19.3 in females, whereas the ASIRs per 100,000 from January 1, 1995 to December 31, 1997 were 14.2 and 14.6 in males and females, respectively. “The second part of the study is under publication, which further confirms that Karachi has the highest incidence of oral cancer in the world. The city also has a high rate of cancer in the pharynx. Besides, a large number of head and neck cancers can also be attributed to paan, chalia, tobacco and gutka,” she said. The study showed oral cancer was found to be equally common in men and women; the most common site was the mucosa cheek (55.9pc), tongue (28.4pc), palate (6.8pc), gum (4.4pc) and floor of the mouth (1.4pc). About 30pc of cases occurred in patients 40 years and younger and 23pc in patients 65 years and older. A strong socio-economic factor, with a poorer, low-literacy profile, was found to be associated with oral cancer in the entire study period. The increasing number of oral cancer cases in the city was confirmed by Professor Dr Tariq Rafi of JPMC and Dr Javed Alam of CHK. At JPMC five to six cases of oral cancer are reported every day, while CHK has eight to 10 cases of oral cancer every day, with the same number of patients with pre-malignant conditions. People often seek medical help very late, making treatment more costly and complicated. This increases the chances of recurrence while minimising years of survival. According to Dr Qaiser Sajjad, teenagers, especially girls, are now becoming victims of oral sub-mucous fibrosis, a pre-malignant condition. The severity of the situation can be gauged from a study conducted last year by students of Department of Social Work, University of Karachi (KU). It says 93per cent children of 50 government and private schools in Saddar Town spent their pocket money on buying chalia or supari and 7 per cent on paan and gutka. Though chalia does induce a mild sense of excitement, several brands of chalia and saunf supari were found to be laced with narcotics, according to a KU research study. Dr Serajuddaula Syed points out most of the chalia being sold in the market is of very cheap quality and has fungus, making it harmful for human consumption. The colours added to the compound have also proved to be harmful. 65 However, it doesn’t mean chalia or paan without tobacco is safe. In many studies paan chewing and chalia have proved to have sufficient evidence of carcinogenicity and are independent risk factors for the disease. While the burden of oral cancer is increasing on public sector hospitals, which have limited resources, no preventive measures are being taken to check the widespread use of chalia, manpuri and gutka, especially among school-children. “This is a grave situation. If preventive measures are not taken, oral cancer may take the form of an epidemic in coming years,” says Dr Tariq Rafi. (By Faiza Ilyas, Dawn-17, 07/04/2007) Compulsory licensing of life-saving medicines THE state of a nation is determined primarily by the health of its people. To describe the state of health care in Pakistan as poor would be an understatement indeed. It is a common knowledge that there is a clear lack of doctors, health facilities and most importantly, availability of reasonably priced medicines. The underprivileged members of our society, cannot even think of enjoying medical care though they mostly remain in need of such a care. It is a cruel joke indeed then to see the business of health care prospering like it does. Recent reports suggest that pharmaceutical companies earn huge profits from the sale of essential medicines. The profits result directly from the prohibitive prices of medicines many of which are life saving and a necessity. A WHO report has ascribed the price increase mainly to two factors-. shortage of medicines in the market and patenting of drugs. The patenting of drugs has remained a controversial issue and gained a notoriety with the nonof AIDS medicines in Africa due to restrictions imposed by patent law. Yet, this law remains the only legal remedy available in securing inventors' inventions; that it adds to the cost of manufacturing drugs is indisputable. Researchers of drugs commit an immense amount of resources- both human and financial--in developing these drugs and the patent law helps them in recouping those costs by selling the drugs at a premium. All good and fair. However problems arise when the premium afforded to pharmaceuticals come at the cost of an entire nation's health. The purpose of medicines and of healthcare is to cure and this must always take precedence over the recouping of costs and making profits. The exorbitant prices for patented life-saving vaccines jeopardise the lives of millions in developing and underdeveloped countries where these medicines are mostly used.. An outcome such as this is unfair and provisions have been included in the law to counter this and allow the access of medicines to those in urgent need. That these provisions are hardly ever availed is another question entirely. The TRIPS--the treaty that governs patent law globally, has extended the powers of the statutory body to issue compulsory licenses to third parties for the manufacture of patented drugs. Such a license is premised in view of public interest and to protect health of masses. In particular such licenses can be granted, under law, with matters relating to national security, nutrition and health of the public or for the development of the national economy. These licences can have a positive impact on a society. In legal terms, compulsory licensing allows a government to issue a licence to a company or a government agency, the right to use a patent without the consent of the patent holder. The objective of granting compulsory licences is to prevent the abuse of monopoly granted by the patent and to safeguard the public health. A patent is granted to provide legal protection to an invention from getting infringed. However, this legal protection is subjected to a time period of four years after the date of grant of patent for bringing the patent into utility. Hence, where a patent has not been exploited in a manner, which contributes to the promotion of technological innovation and to the transfer and dissemination of technology, the government has the power to decide that a government agency may exploit the patented invention. The government before taking any decision, shall give the owner of the patent an opportunity of being heard if he wishes so. Though, in the circumstance that the patent holder refuses to let a compulsory licence be issued or if he allows licensing but not on reasonable commercial terms, the government shall have the power to grant the compulsory license without the consent of the owner of the patent. Here the third party has to present evidence that the patent holder had been approached for his consent before coming to the government. The system of compulsory licensing is an integral part of the patent law and one that is present in most countries of the world including Pakistan and the Britain from whom we inherited the Patent and Designs Act 1911. This system is a century old and was incorporated in the UK Act of 1907. It is principally founded upon the idea that a government must safeguard the interests of its people, which most importantly includes their health. In the Patents and Designs Act, 1911, there are provisions vide Sec22, 23 and 23A, whereby any person interested may present a petition to the government alleging that the demand for a patented article in Pakistan is not being met to an adequate extent and on reasonable terms and praying for the grant of a compulsory license, or, in the alternative, the revocation of the patent. This remedy is also available in the new Patents Ordinance, 2000 vide Sec 59, whereby the controller has the power to grant compulsory licences. The exploitation of the patented invention shall be limited to the purpose for which it was authorised and shall be subject to the payment to the said owner of an adequate remuneration taking into account the economic value of the government authorisation, as determined in the said decision. There is a widespread misconception that a country can issue compulsory licence only in the case of an emergency. The Doha Declaration on Public Health confirms that countries are free to determine the grounds for issuing compulsory license and a great deal of flexibility is legally on offer. However the onus is on the proposed user to make necessary efforts and avail this flexibility. This, however, does not mean that the entire system of patent law is invalidated by the provisions on compulsory licensing. According to Sec 59(2), a nonlicence shall not be issued if the owner of the patent satisfies the controller that circumstances exist which justifies the nonor insufficient exploitation of the patented invention. Thus it is the existence of a framework that includes respect for patent law along with compulsory licensing that allows for the establishment of a much fairer legislative system. 66 Example: To illustrate the current situation and how compulsory licensing would prove to be a useful way in improving access to medicines in developing countries; let us use the following example; a thousand children die of dysentery every day in Uganda and Kenya who are neighbours. Yet a child in Uganda has a much better chance of surviving the disease than a child in Kenya. The reason is that Ciprofloxacin, an antibiotic that kills the `shigella bacteria’ that causes dysentery, sells for just seven US cents per tablet in Uganda whereas in Kenya the same drug is priced at $2.42, pushing this lifesaver far beyond the means of parents of the children suffering from dysentery. The simple reason for this vast price difference is that Kenya has laws respecting patents and Uganda has not. Let us take another example; an antibiotic used in the treatment of respiratory and sexually transmitted infections (Azythromicin), - most highly prevalent diseases in developing countries--, costs $2.70 per 259gm capsule in Kenya where it is patented and marketed under the trade name Zithromaxg. However, in India where pharmaceutical products are harder to patent, many generic manufacturers market Azythromicin and because of competition, the Indian retail price for Zitgrinax is over three times cheaper than the trade price in Kenya ($84). Now if the Kenyan government were to issue a compulsory licence for Azythromicin, generic versions of the drug would be able to treat five to seven times more patients within the same budget. In attempting to justify their position and role in hindering access to essential medicines, multinational pharmaceutical companies continue to claim that lower prices for drug therapies in developing countries would be a serious threat to their research and development funding. This is, however, a very weak argument indeed. Although the majority of the world's population lives in developing countries, these countries represent only a small proportion of the global pharmaceutical market. It is even more startling to note that compulsory licences have been issued in the richest countries of the world. Licenses issued: Canada-- On February 2006, Canadian generic firm Biolyse requested the the ministers of health and industry to add Osteltamivir to the list of pharmaceutical products eligible for compulsory licensing for export. On July 2006, the Canadian government announced granting this licence. United States: The anthrax scare in the fall of 2001 led DHHS Secretary Thompson to seek a large enough stockpile of ciprofioxacin (Cipro) to treat 10 million people. This quantity was far greater than the supply and Bayer lacked the capacity to produce it in a timely manner. On October 16, Senator. Schumer asked Thompson to issue compulsory licences to generic manufacturers. Germany: A licensing agreement was reached between Roche and Chiron. Roche had been attempting to get the German government to get it to issue a compulsory licence for patents on "Blood screening HIV probe" held by Chiron. Malaysia: The Malaysian government issued a compulsory licence to Indian companies to import generic variants of didanosine (ddl), zidovudine (AZT) and lamivudine+zidovidine (Combivir). Indonesia: On October 5, 2004, Indonesia issued a compulsory license to local companies for the manufacture of generic versions of lamivudine and nevirapine, until the end of the patent term in 2011 and 2012, respectively. Thailand: On November 29, 2006, the Thailand government announced a compulsory licence to import (from India) and locally produce Effavirenz. Cameroon: On January 2005, the non-profit corporation Essential Inventions requested the minister of public health to grant a government use/ex officio compulsory license of the patents relevant for importation, manufacture or sale of generic versions of the following medicines used in the treatment of HIV/AIDS: Nevirapine (brand name Viramune Lamivudine (brand name 3TC*) Fixed dose combinations of Lamivudine and Zidovudine (Brand name Combivirt) Ghana: On October 26 2005, the minister of health issued a government use compulsory licence for importation into Ghana of generic HIVmedicines. Eritrea: On June 5 2005, the minister of health issued a compulsory licence for importation into Eritrea of generic HIVmedicines. Zambia: On September 21, 2004 the Zambian minister of domestic trade and consumer affairs issued a compulsory license for lamivudine, stavudine and nevirapine. The license was granted to Pharco Ltd., a local producer to produce a triple fixedcombination. at a maximum royalty rate of 2.5 per cent. Why not Pakistan? The question arises, why Pakistan lags behind in the growth of its economy, protection of its nations health and most significantly, in protecting its pharmaceutical industry? Weak growth: A major flaw in Pakistan pharmaceutical industry has been its failure to develop indigenous basic drug manufacturing expertise. This failure stems from the lack of largeeconomies and extensive facilities required for manufacturing of basic drugs. Other than this, there is the issue of non-existent research and development culture in the pharmaceutical industry, which in turn discourages innovation and creativity. The imposition of GST too has played a crucial role in pushing up medicine prices. For instance, in December 2001 the government had announced a drug price increase of three on controlled and four per cent on decontrolled category of drugs respectively. But the prices went up by 40 per cent. Such increases in drug prices are due largely to the tricky policies of the government. Strong growth of Chinese pharmaceutical industries (20 per cent per annum), relatively lower labour costs, existence of large number of profit oriented research and development institutions and liberal tax holiday regime are among the main factors that have given China a competitive edge over Pakistan. Likewise, the threat from the Indian pharmaceutical industries stems from the better developed quality products and superior quality of R&D, the financial and scientific benefit of which is siphoned back into the development of new products. 67 Suggestions: It is true that drug prices all over the world, including the US, have registered a sharp increase. However, in Pakistan many additional factors, including ruthless manipulation of market forces, have further complicated the issue. It would be instructive hem to quote Article 38(a) and (d) of the Constitution of Pakistan which says: "The State shall secure the wellof the people, irrespective of sex, case, creed and race, provide basic necessities of life such as medical relief for all such citizens as are permanently or temporarily unable to earn their livelihood on account of infirmity, sickness or unemployment. " Therefore, the government here needs to take necessary steps to improve the pharmaceutical infrastructure. The government should develop the infrastructure and expertise required for basic drug manufacturing. Secondly, it should ensure local production of drugs whose patents have run out to lower the prices of drugs. And lastly, it should allow import of basic raw materials from India in view of the latter's expertise in this sector till Pakistan's pharmaceutical industry comes of age. Despite of all this, many developing WTO member countries have granted compulsory licenses for patented essential medicines and it is crucial time that Pakistan must ensure that drugs are available in domestic markets at affordable prices as lives and health of millions of its people depend on access to these medicines. (By Karimullah Adeni, Dawn-Economic & Business Review, Page-VI, 09/04/2007) Dire need for a skin bank in Pakistan Plastic Surgeon, Dr Abdul Samee stated that there is an urgent need for skin banks that will help reduce medicinal charges and ensure speedy rehabilitation of the burns patients. Currently there are no skin banks in Pakistan. Dr Samee said a skin bank will be used to grow skin in laboratories. This will be transplanted onto the affected body after two weeks. “During this two-week period Bovine skin could be used to cover the burnt body and to protect it from more damages,” he added. Currently, the bodies of burns patients in Pakistan are covered with bandages wrapped around the affected areas, he explained. This process takes a lot of time and the patient is given heavy and costly medication. He said that with the presence of a skin bank, the rehabilitation process could be accelerated and made cost-effective. While elaborating on the need for skin banks, he said that generally the skin functions in four different ways. “Conduction, radiation, convection and evaporation are the four processes of the skin.” He said in cases of burns, evaporation through the body is stopped but other functions remain operative. As the burnt body will not be able to process this objective, it will grow weaker and weaker, he added. In such cases, the affected body will become the target of weight loss, ultimately raising the metabolism of the body. “If a patient has lost 30 per cent of his weight then there are 90 per cent chances of his mortality regardless of how much of his body was burnt,” Dr Samee said. Moreover, he said burns patients need a special environment of 80 degrees Fahrenheit until the skin has healed. Such patients cannot go out in the open because bacteria will attack their bodies and create deformities. According to Dr Samee, the human body takes two weeks to reject any foreign skin on it. Protective skin, artificial or that of some animal, can protect the body from more damages. During a period of two weeks, the affected part of the skin will be grown in the laboratory so that it can be transplanted over the burnt part. In his view, this period of time is enough for the patient to develop a bed for the transplantation of new skin over the affected one. “Scars left on the burnt body generally have no elasticity. If the patient is a child then his body growth will be adversely affected.” But, he added that skin banks will enable surgeons to reduce chances of that happening enormously. Furthermore, the tissue expander is another way to grow skin, said Dr Samee. Water, he explained, is injected into the skin layer to inflate it. In this way extra skin can be obtained to transplant it over the burnt part of the body. “Due to the unavailability of a skin bank, even smaller burnt parts of the body such as face and hands become subject to deformity which could otherwise be prevented.” Dr Samee said. He remarked that even neighboring India has skin banks and other facilities in this regard. Sometime back provincial minister for health had announced that a skin bank would be established in Karachi. A great number of problems of burns patient will be solved if this promise is fulfilled by the concerned authorities. (By Qadeer Tanoli, The News-20, 10/04/2007) ‘Public health victim of misplaced priorities’ KARACHI, April 11: The public health issue is a victim of misplaced priorities and widespread corruption. It’s time the government realised that what the country needs is an efficient primary and emergency healthcare system and provision of basic facilities and not lavish expenditure on tertiary care centres and elite medical towers. This was stated by Honorary Secretary General Pakistan Medical Association Dr Habib-ur-Rehman Soomro at a press conference held for the PMA’s annual health report release at PMA House. He was accompanied by PMA members Professor Dr Tipu Sultan, Dr Samrina Hashmi and Dr Qaiser Sajjad. Commenting upon the government measures for health uplift, Dr Soomro said in a country where 70 per cent of the population has no access to primary and emergency care, 1.2 million people die of water borne diseases annually, a child die of some disease every minute and 70 women die of pregnancy-related complications every day, the government has no justification to spend money on lavish projects. “It’s a shame that Iran and Bangladesh had successfully eradicated polio with six and four rounds, while new polio cases are still being reported in Pakistan despite having more than 62 rounds of vaccination. Diseases like hepatitis and malaria are on the rise while the public is ignorant of the emerging HIV/AIDS threat,” he said. 68 The government, he said, should spend on basic needs first. One of the requirements for provision of primary healthcare is the availability of paramedics and nurses. “At the moment, there is a dearth of paramedics at all health units in rural areas. More ironic, perhaps, is the fact that the government has adopted a policy of appointing doctors on contract, bypassing public service commission,” he said. He condemned government inaction against the manufacturers of fake drugs and quakes and claimed that there are 600,000 quacks in the country. He also expressed concern over the flourishing kidney trade in the country and said Pakistan is the only Muslim country in the world where there is no law on organ transplantation. “The kidney trade has reached the Rs1 billion mark,” Dr Tipu Sultan added. About medical education, he said medical colleges in public sector are in pathetic state but the government is bent upon building medical universities. He demanded an end to government interference in Pakistan Medical and Dental Council and make it an autonomous institution. The PMA demanded an increase in the health budget up to six percent of the GDP; appointment of midwives, paramedics, doctors and nurses at health units on emergency basis; provision of clean water and improved sewerage system; strengthening of Expanded Programme of Immunisation and medical education; appointments on merit; career structure of doctors working in public and private sector and regulation of private hospitals and clinics for public benefit. (Dawn-18, 12/04/2007) People in Malir at risk due to dumping of deadly pesticides Parveen Fatima, 50, died of leukemia at Patel Hospital, Gulshan-e-Iqbal on October 24, 2006. Scientists suspect the cause of her death might be the deadly pesticides dump in the Malir town, adjacent to Mohammadi Girls Secondary School where she was a teacher a few years ago. Fatima is not the only one at risk. Next to the school is Prince Aly Boys Secondary School. Children from both the school where she taught and the one next to it are at risk. The deadly pesticides identified as Dichloro-Diphenyly trichloroeethane (DDT) has been dumped by the agricultural department decades ago. It is suspected that this has seeped into a water tank situated in the school adjacent to the dump, making children and teachers vulnerable to pesticide poisoning since the tank happened to be the only source of drinking water in the school. Teachers of Mohammadi Girls High School said children were usually drowsy and complained of skin rashes. But they were apparently oblivious of the dangers of pesticide poisoning. In an internal memo, the Sindh Environmental Protection Agency (SEPA) also confirmed a few years ago that children’s lives were at risk due to pesticide poisoning. However, no government action has been taken on this. Fatima, who earned a Masters degree in first class from the University of Karachi, was diagnosed as suffering from leukemia in 1998 by hematologist Dr. Hamid at the Aga Khan University Hospital (AKUH). She was teaching at Mohammadi Girls Secondary School at that time, unaware that her life was at risk. “The children who studied at the school in Malir and drank the contaminated water from the tank are at potential risk of having cancer, hormonal imbalancement (such as giving premature birth) and disrupted neurobehavioral functions,” Dr. Kaneez Fatima Shad, Professor of Molecular Medicine and Neuro-Physiology at Dr. Panjwani Center for Molecular Medicine & Drug Research, University of Karachi, told The News. DDT, the best known organic pesticide, is nearly insoluble in water but has a good solubility in most organic solvents, fat and oils. That is why it has the capacity to accumulate in the adipose tissues (fat) of all living beings, including humans. There is not a single organism on the planet that does not contain DDT. This property makes DDT as a very potential candidate for increasing risk for cancers at various sites and disrupting endocrine (hormonal) functions in humans, says Prof. Shad. “Yes there is a great possibility that the teacher (Parveen Fatima) may have suffered from blood cancer and died due to drinking the water from the school tank in Malir, which was polluted from the dumped DDT,” Prof. Shad added. DDT is stored in all human tissues but the highest concentration occurs in fat. It has been calculated that it would take between 10 to 20 years for DDT to disappear from an individual if its exposure is totally ceased, but its main metabolite DDE would persist throughout the life span, explained he doctor. DDT was first synthesized in 1874 but its insecticidal properties were not discovered until 1939 and the low price of DDT contributed to its world wide use. In the early 1960s about 400,000 tons of DDT were used annually world wide (70-80% was used for agriculture). All soils have a strong absorptive capacity for DDT that is related to their organic matter content. DDT is toxic to fresh water and marine organisms, fishes, and birds. On the basis of ecological considerations, Sweden was the first country to ban the use of DDT in January 1970 which was followed by almost all countries except few developing countries such as India, Pakistan and Indonesia etc. The current intakes of organochlorine insecticides in Asia are up to 100 times greater than those in more developed countries, and the estimated intake of DDT by children is reported to be 100 times greater than the admissible daily intake (ADI) established by the Food and Agriculture Organisation (FAO/WHO) in 1985 at 0.02mg/Kg of body weight. “The best method to move off DDT is to avoid using it as there is no safe way of disposing it off without being accumulated in the body and disrupt our normal physiology,” says Prof. Shad, adding “Long term accumulation of DDT in humans’ results in the neurons to fire spontaneously, which in severe conditions leads to spasms and eventual deaths.” After hue and cry from the media, the authorities have buried the DDT in the soil instead of incinerating it that could contaminate ground water bringing miseries to the entire people of Malir. “Karachi, Hyderabad, Kotri, Dadu and some other cities of Pakistan have stores of DDT. Either there are stores or these 69 have been buried in the soil. Malir Court and some administrative offices of Malir have been built on the heaps of DDT and other obsolete pesticides,” says Dr. Iqbal Saeed Khan, former director of SEPA and additional secretary, Local Government, Katchi Abadis & Spatial Development, Government of Sindh. “People in Malir complain of persistent smell of DDT and feel drowsy. They are not as dynamic as they should be. Since DDT is a persistent organic pollutant and is non-biodegradable, therefore, its disposal needs a scientific way, including burial by placing it in impervious drums so that water and moisture should not interact with it,” he explained. “These pesticides were dumped/ stored by the agricultural department some 20 years ago and left at the mercy of nature. They hamper in neurotransmission i.e. the function of brain and nerves. Besides, they are cancer producing and the people who are exposed to its prolonged exposure continue to suffer and their offspring are also likely to suffer,” cautions Dr. Khan. “The persistent organic pollutants which are discharged in water bodies are ultimately locked in the food chain and hence the human sufferings are perpetual,” he explains. “During the Vietnam War, a persistent organic pollutant namely Agent Orange was sprinkled over the jungles of Vietnam to defoliate the trees so that the hidden Vietcong guerillas become visible to bomber planes. It is being reported that a host of children who are taking birth are having protruding eyes and a number of diseases of the nervous system.” It is feared that the human toll in Malir will become higher with the passage of time. In most instances, the victims will only realize until it is too late. So far, there has been no government action plan in place to deal with the situation or remove the toxic pesticides from their present resting place, say officials. (By Shahid Husain, The News-13, 14/04/2007) Poisonous rivers The indifference shown by the government of Sindh and the provincial environment protection department towards the danger posed by the unchecked dumping of hazardous chemical waste such as dichloro-diphenyl-trichloroethane (DDT) in the Malir river area of Karachi is depressing. DDT has been banned worldwide for about three decades now after it was discovered that it is known to cause cancer. However, like many banned chemicals and pesticides it seems to be in use in Pakistan. And not only is it used here, it is disposed off in a most dangerous manner, with the government and the environment protection authorities looking the other way. Obviously, the first issue that needs to be examined is what a dangerous pesticide like DDT is doing in Pakistan in the first place. The answer to that is perhaps found in the fact that when it was developed and introduced for commercial use after World War II, it was highly effective against a variety of crop pests and those insects (mosquitos for example) that were known to spread disease through the transport of pathogens. It is perhaps because of these qualities that the pesticide is still in use in Pakistan . However, that still means that it needs to be stored and disposed off in a reasonably safe manner. It should be noted that residues of the toxic chemical can stay in river water for as long as 28 days. The best way to do that is to burn the pesticide in an incinerator. But that is unlikely to happen in a country where most hospitals lack even basic waste disposal equipment. One also suspects --and there is considerable circumstantial evidence to support this -- that the Malir dumping is not an isolated case but only the proverbial tip of the iceberg. In fact, hazardous chemicals and untreated effluent from factories are being dumped every day into the rivers and streams by industrial units with the environmental protection departments turning a blind eye to this rampant poisoning of the country's freshwater resource. In Punjab, the Ravi and various streams that flow into it, the Hudiara drain being a good example, are all heavily polluted thanks to this unchecked dumping of chemical and toxic waste. Similarly in Sindh, numerous sources of drinking water have levels of pollution so high that drinking their water can cause death. This is precisely what happened in the Manchar lake pollution case of 2004 when dozens of people were killed and hundreds more fell seriously ill after irrigation officials released water from the lake into the Indus because of the impending monsoon. The result was catastrophic and a general warning was issued to residents of Hyderabad to drink only boiled water. It is astonishing that even the deaths of dozens of innocent people failed to move the Sindh government and its environment protection department to take any kind of remedial or preventive measures. For instance, to date, not a single official was charged with negligence in the Manchar lake scandal, and if they were the action was not made public. Once the hue and cry over the deaths died down, everything went back to business as usual. Also, a case involving bone deformities among several residents of a small village near Manga Mandi in Lahore in the late 1990s, caused by the groundwater becoming contaminated because of fluoride poisoning, was as quickly forgotten as it burst onto the national media. No one remembers what happened to those people and no one knows whether their polluted drinking water source was ever made safe for human consumption and whether the Punjab government came good on its promise to treat all those who had been affected. After all, what are the authorities waiting for? There is a law -- the Pakistai Environmental Protection Act of 1997 -- in place to check much of this pollution and it is about time that the federal and provincial governments began to implement it in earnest. (The News-7, 17/04/2007) ‘Save children from cancer’ Demand for strict ban on use, sale of betel nut KARACHI, April 18: The government’s indifference in the face of increasing oral cancer cases, especially among younger people, makes it all the more important for the managements of educational institutions to take their own line of action, make children aware of the health hazards of pan, chhalia (betel nut) and gutka and prohibit their sale in the institutions. This was stated by Pakistan Medical Association’s General Secretary, Dr Qaiser Sajjad, while addressing a large gathering of schoolchildren at the PMA House. The event was first in the series of programmes to make children aware of the health risks involved in chhalia consumption. Criticising the government for failing to provide primary healthcare, he said that health and education were not on the priority list of the government which was evident from the fact that the government had failed to provide clean water to its 70 citizens. As a result, three million people contracted waterborne diseases every year and 250,000 children died because of the same reason. “This situation puts greater responsibility on citizens. They should educate themselves about health issues and help create a better environment for future generations,” he remarked. Talking about the widespread use of chhalia and gutka and its health risks, he said oral cancer was the second largest form of cancer after lung cancer in Pakistan. The number of its victims was rapidly increasing, especially among young people. “In view of persistent government apathy over the issue, educational institutions should come forward and warn students about its health risks as more and more teenagers were falling victim to sub-mucous fibrosis (SMF), a pre-cancerous condition,” he said. Making it very clear to the impressionable minds that there was no difference between ‘clean’ and ‘bad’ chhalia as far as the health risks they posed, he said it had been scientifically proven that chhalia was an independent risk factor for cancer. He showed the audiance various images of people suffering from SMF. Talking to journalists, he said the PMA had asked the government to ban the sale, manufacturing and advertising of chhalia and gutka. The association, he said, would support parents who had any child suffering from SMF and want to fight against the school administration for allowing the sale of chhalia in their institution. PMA President Dr Naseer Baloch and member Dr Aziz Khan Tank also spoke. (Dawn-18, 19/04/2007) Biomedical waste hazards being ignored With only three incinerators in the 15-million strong megapolis Karachi, one of them often dysfunctional, and every large hospital generating 0.5-2 kilograms waste per bed a day, of which 0.1-0.5 kg is categorised as biomedical waste, citizens, sweepers in particular, are being continuously exposed to deadly diseases such as Hepatitis B and C and HIV/AIDS. “Hospital waste comprises ordinary and infectious waste and if the later is not scientifically disposed of, it becomes threatening to health workers, sweepers, scavengers and transporters in particular and environment in general, and can cause hepatitis B and C and HIV,” Dr Syed Abdul Mujeeb, Incharge Blood Bank and an assistant professor at city’s premier public sector hospital, the Jinnah Postgraduate Medical Centre (JPMC) told The News. “The biochemical waste, if not incinerated, is spread by stray dogs and cats, becomes part of drinking water, causing waterborne diseases such as diarrhea and also lead to air borne diseases,” he said. “In fact, every source of biochemical waste, including hospitals and laboratories, should have incinerators,” he said. However, the grim reality is such that sans the Aga Khan University Hospital, Liaquat National Hospital and Civil Hospital Karachi, no health facility in the mega city, which provides the major chunk of the exchequer’s revenue in the form of taxes, can boast of an incinerator. Moreover, to add to the problem, the incinerator at the Civil Hospital Karachi is often dysfunctional. Even when in working condition, its fumes make the lives of patients and doctors at the psychiatric ward miserable. Hospital waste is classified as either regulated medical waste (RMW) or non-regulated medical waste (NRMW). RMW generally includes laboratory cultures, bulk blood and other biological products, clinical laboratory waste, and items that are generated in the course of patient care that are soaked or saturated in liquid or dried blood. NRMW includes all other solid waste generated by healthcare facilities such as incinerator exhaust, utility wastes and trash. The World Health Organization (WHO) guidelines on hospital waste management stress that responsibility for proper handling of hospital waste rests not only with the hospitals and health services but also with municipal authorities that are largely responsible for the final disposal of the waste. The Karachi Metropolitan Corporation (KMC) had installed two incinerators, each with capacities of 10 tons of waste per day at Mewa Shah, Lyari. But, “the KMC incinerators which have a capacity to burn 10,000 kgs of waste per day manage to incinerate only 1,000 kgs per day which comes to 35 hospitals from Karachi,” according to a study conducted by Dr Pritpal Singh, Dr Amir Omair and Dr Salman Safdar a few years ago. In fact, elsewhere in the civilized world there are consultants and advisors hired for waste disposal, but, in Pakistan, the dangerous game of disposing biomedical waste through sweepers continues unabashed. “There are different types of items and they have to be handled in a specific way. The top priority goes to sharp objects such as needles, blades and glass, together known as shrapnel because they are very dangerous because even a prick injury to the person disposing the waste and can transmit disease,” Dr Shafiq-ur-Rehman, professor of surgery at Civil Hospital Karachi said. “In our country, we don’t have the concept of handling the sharp objects. Normally, they are thrown in plastic bags and obviously they cause damage to other people. Standard practice is that they should be placed in a solid plastic dispenser after cutting off their edges and these are then sent to the incinerator,” he said. Ironically enough, such facilities do not exist in the city as elsewhere in the country. “Such practices are lacking in the majority of city hospitals. We don’t have colour-coded bags which signify the infectivity of the disposable items. We don’t have any department of hospital waste disposal and it is left on the sweepers who are at risk,” he cautioned. (By Shahid Husain, The News-13, 1way.arp ar 71 rp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp a arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp arp l ones. The new practice has been adopted following a recent exercise under the “central purchase of general medicines and other items.” According to CDGK sources, tenders were invited by the city government in mid February this year for the supply of 781 items, under group-1 of the tender relating to medicinal, laboratory, surgical and disposable items. At some later stage, about 193 items were either dropped by the purchase committee or no bid was submitted against them. “Only 211 (36 per cent) contracts were cleared by the central purchase committee on the basis of lowest quoted rates, which could be considered as truly in line with the recognised objectives of any tendering process,” said a health department source. While the EDO Health maintains that all the purchase deals, involving over Rs300 million, have been struck in a transparent manner keeping in view saving, other relevant quarters have expressed some reservations, saying that the government was, perhaps, about to ignore the purpose of open tendering. The EDO also heads the central purchase committee which, according to him, has examined all quotations a week before the same were submitted for his approval. Marketers and the parties familiar with the procedure of hospital purchases claim that the purchase committee, which mostly operates from a city government hospital, has failed to observe the rules and standard procedures. Their style of selecting suppliers, distributors or manufacturers on the basis of single quotation or under the garb of quality and essential items will definitely pave the way for an underground cartelism in future, they say, adding that on the other hand, the companies will also lose confidence in the tendering exercise, according to a contractor. It was stated that the committee ignored the practice of collecting competitive rates and went for selecting suppliers through negotiations with and recommendations from a handpicked group of personnel. A good number of items were given to a couple of firms which were the only parties offering the rates, instead of re-tendering to invite more as per the prescribed rules. Finally, the items would be termed essential ones, it was further said. Some quarters are also not satisfied with the examples of essential items, indicating that the items like vitamins (B or C), calcium, non-specific anti-allergic nasal drops, non-specific astringent eye drops, and non-specific soothing skin powder are termed essential only to please the favourite parties. In the tablet category, 43 out of 127 were approved on the basis of rates. The committee approved only 16 out of 116 items in the injection category for which the lowest rates were received while the rest of the injection supply were approved under the head of ‘quality’, ‘single quoted’ or ‘essential’. A distributor has been approved for supply of about 71 items out of which only 19 were the lowest quoted. In addition, the firm will do a business with a turnover of about Rs37 million with the city government during the financial year as 51 of its items have been selected on the basis of quality or single quotation, according to supply position document approved by the central purchase committee. Another party has been selected for the supply of about 55 items, mostly in the categories of surgical, disposable and dressing material. The party will supply 25 items worth Rs16 million only on the basis of quality and single quoted items, as transpired from the official documents. When EDO Health Dr A. D. Sajnani was contacted for his comments, he said that the committee adhered to the rules and worked in the interest of the city government. Sensing any shady deal or dubious exercise in regard to medicine purchase meant for the devolved health institution of Sindh government and defunct KMC and DMC or District Councils was not appropriate, he added. The committee constituted for the purpose was all competent and comprised personnel of integrity with diverse medical specialities, he maintained, adding that if any discrepancy was detected in the bidding and allocations of supplies, he was ready to be held accountable. Dr Sajnani observed that many things had improved considerably as far as medicine purchases were concerned. In reply to a question, he said that he personally entered into negotiations with some of the suppliers and manufacturers to get their quoted rates reduced further. Many of the deals pertaining to ‘quality’ or ‘essential’ items were approved on the recommendations of medical superintendent and doctors sitting in the committee. These committee members, he pointed out, were not only the endusers but they also knew the worth and effectiveness of medicines and hospital materials as they possessed considerable experience in the profession. (Dawn-18, 26/04/2007) Outcast HIV patient turns social activist ISLAMABAD: Thrown in jail, deported and ridiculed — Nazir Masih’s struggle as the first person in Pakistan to be publicly outcast as HIV positive has led him on an often arduous journey from outcast to activist. The 52-year-old Masih has overcome his problems to help Pakistan’s “hidden” HIV/AIDS sufferers who get little help from the government — officially only 4,000 people here have the virus but UNAIDS says up to 80,000 are infected. “When I was first diagnosed as HIV positive 17 years ago, I used to wish I was dead. I thought it would be better for me and my family than to suffer a life of stigma and ostracism,” the diminutive Masih told AFP. 72 Masih was working as a helper for an Arab family in Abu Dhabi when a mandatory HIV test for renewing visas came back positive. “Having spent years away from my wife, I did have sex with another woman. It was a mistake but the scale of the punishment was too severe for the act,” he says when asked how he contracted HIV. “I was thrown in jail and later deported to Pakistan,” he said. Back in his homeland, the nightmare continued. A quack doctor told him that his condition was the same as syphilis and took most of his money for useless treatment, forcing him to sell his house. Lesions began to appear on his skin. And then, he says, local newspapers found out about his condition and turned his life into a circus. Health officials alerted to the “threat” posed by Masih descended upon his house and told his wife to avoid all contact with him. This was the first time someone with HIV/AIDS had been outcast in Pakistan, says Nasir Afraz, deputy programme manager at the government’s National Aids Control Programme, although the first confirmed case here was in 1987. “They really upset my family. My wife was told not to give me any food or even touch my clothes,” said Masih. “They made a complete mockery of me.” By 1998 he said he was contemplating suicide when he was contacted by a Christian charity. With their help he set up an office in his bicycle shop and with a small team of workers he began an initiative to reach out to HIV sufferers and educate poor communities about the virus. He had only five patients at first — and not all of them welcomed his help. “I have taken a lot of abuse from HIV patients. One man who was HIV positive got really angry and threatened me with a gun,” he said. In 2001, with the help of outside funding, Masih set up the New Light Aids Control Society in Lahore. Today it provides 124 people with free anti-retroviral therapy, counselling and financial aid. Masih’s dedication has also motivated others. In 2003 Nawaz Ahmed was working as a mobile technician in Kuwait when tests proved he was HIV positive. “Because of the stigma associated with HIV and AIDS, I didn’t tell people I was HIV positive but once I saw the work that Nazir was doing it motivated me to act too. I started working at New Light in 2004,” he said. Masih says the official response to the growing HIV problem in Pakistan is inadequate. “Our government has ignored the HIV problem rather than attack it,” he said. “They have testing facilities and they have been providing anti-retroviral therapy since 2005 — two years after New Light — but the government makes no effort to engage the population.” Bettina Schunter, an HIV and AIDS official for the United Nations Children’s Fund said the number of people living with HIV/AIDS in Pakistan was likely to be 70,000-80,000, about 20 times more than the number actually diagnosed. “We know the people are there, we just haven’t officially found them yet,” Schunter said. But Afraz of the National Aids Control Programme denied that Pakistani authorities were not doing enough. “We have nine treatment centres across the country, about 650 patients are registered with us. Right now we are in the process of scaling up treatment and services for HIV patients to meet deadlines by 2010,” he said. (The News-4, 26/04/2007) CDGK sets aside more money for health in draft budget KARACHI: A draft budget of Rs 43.108 billion for the financial year 2007-2008 was presented in the City Council session Saturday amid chaos. The surplus budget of Rs 493.99 million against last year’s surplus of Rs 365.74 million indicated that Rs 43.602 billion as revenue against expenditure of Rs 43.108 billion. The city government’s draft budget for the year 2007-08 includes the allocation of Rs 513.91 million for the newly establish Municipal Services department and increases in health, transport and communication, information technology, literacy and water and sewerage. The city government proposed Rs 3.145 billion for health while last year it had earmarked Rs 2.869 billion. The literacy department allocation has gone up to Rs 58.09 million from last year’s Rs 8.53 million. The city government set aside Rs 220.18 million for information technology from last year’s Rs 56.07 million and the Karachi Water and Sewerage Board will get Rs 7.885 billion up from Rs 5.305 billion last year. Furthermore, development expenditure has also increased from Rs 10.134 billion against last year’s Rs 7.259 billion as the allocation for Tameer-e-Karachi Programme had reduced Rs 5.2 billion as it was Rs 9.893 billion last year. City Council suspends belt-wielding member for 3 sessions: Salman Mujahid Baloch, a member of the treasury benches in the City Council, was suspended for three sessions Saturday for using his belt to beat a female opposition member during the session held Friday. Nonetheless, chaos reigned again at the City Council session Saturday as charged opposition members demanded stern action against all treasury members involved in assaulting them Friday. The proceedings, which lasted only 40 minutes, were suspended twice for five-minute intervals over the uproar from the opposition benches that shouted slogans and waved banners and placards stating their demands. Opposition leader, Saeed Ghani, demanded that an F.I.R. be registered against all those members involved in the attack and that their membership be suspended. Leader of the House, Asif Siddiqi, said they were concerned about what happened but members of the opposition kept shouting against the government so much so that no one could be heard. However, during both adjournments, the treasury benches left the House to avoid a confrontation on the floor. At one point, convenor Nasreen Jalil repeatedly asked and then shouted at opposition members to sit down but they refused. The 73 aggravated members even lodged their protest at her desk and showed her the bandaged hand of Haji Yaqoob who was injured. Upon this, Jalil announced that the member of the treasury benches, Salman Mujahid Baloch, who attacked an opposition member with his belt (widely published in newspapers) would have to be suspended from three sessions. She asked for the formation of a committee to include members from both sides to conduct a joint inquiry into the issue and submit a report of her for further action. Amid the uproar, the convenor asked for the tabling of a resolution regarding the handing of the city government’s draft budget 2007-08 to the budget committee and asked members to submit their suggestions and proposals within the next six days. The resolution was approved on a majority basis as the opposition members did not participate in the counting. The session was adjourned till May 14. Later on, Jalil held a press conference in the committee room of the City Council Secretariat and said that the code of conduct committee met in the morning and decided to suspend Salman Mujahid Baloch from the next three sessions. “We are condemning the incident as it is not in our policy to assault any member of the council even women,” she said. Opposition leader Rafiq Ahmed and Saeed Ghani told journalists separately that they feared that the committee proposed by the city naib nazim would not do justice to the matter. “The inquiry should be conducted by a judiciary committee as a majority of the treasury bench members were involved in the attack,” they said. They said they will not attend any more sessions of the city council till the government gave them proper security and Saturday they had come to the house to lodge their protest against the misbehavior of the treasury members. (By Jamil Khan, Daily Times-B1, 29/04/2007) MAY World Asthma Day 5pc Pakistanis suffering from disease KARACHI, April 30: Like elsewhere across the globe, various scientific and public awareness programmes have been planned by health care organisations and asthma educators in the city to mark the World Asthma Day (WAD), which is observed every year on the first Tuesday of May. The first WAD was celebrated in 1998 in more than 35 countries. The WAD theme for this year is “You can control your asthma”. It is claimed that about 300 million people, including 7.5 million Pakistani adults and children, worldwide have asthma. Recent estimates have shown that an additional 100 to 150 million persons are likely to have asthma by 2025 throughout the world, said an expert, adding asthma can be controlled through proper management of the disease. Researchers believe that people with asthma have trouble breathing as their airways become inflamed due to various factors like polluted air, increase in air particulates because of unplanned soil erosions and industrial emissions, and inhouse deposits left by dust mites. For education and awareness among people, Aga Khan University will organise a seminar on May 2 at its auditorium. Speakers include Dr Javaid A Khan, Dr Suleman Haque, Dr Javed Hussain and Dr Anwar Shafi.On Monday, a couple of chest specialists said at a press briefing five out of every 100 persons in Pakistan suffered from asthma. The sitting was organised by Asthma Awareness Programme. Dr Sohail Akhtar and Dr Naseeruddin Mahmood maintained that asthma was one of the most common chronic diseases in the world. Recent estimates have shown that an additional 100 to 150 million persons are likely to have asthma by 2025, according to the doctors. They said that it was now understood that asthma was a two-component disease, consisting of both airway inflammation and airway smooth muscle dysfunction such as bronchoconstriction. These symptoms are recurrent, and vary in severity over time. They reminded that asthma symptoms were intermittent, but the underlying disease was always present. “For many patients, medication must be taken every day and sustained at the correct level to control symptoms, improve lung function and prevent attacks. Medications may also be required to relieve acute symptoms”, they said. (Dawn-18, 01/05/2007) Preventing thalassaemia THE demand for introducing legislation making it mandatory for couples to have themselves tested for thalassaemia before marriage has been consistently ignored by our parliamentarians, which is why Senate chairman Mohammedmian Soomro’s support for such a law raises few hopes. Perhaps, our lawmakers do not realise the suffering of thalassaemic patients, mostly children, who, during their limited lifespan, have to undergo frequent blood transfusions and endure health complications that impact adversely on the quality of life. In fact, in an environment where carelessness is the defining feature of public healthcare, many children often contract other dangerous blood-borne diseases through the transfusion of infected blood. Bone marrow transplant offers a cure but it is both costly and risky. Besides compatible donors are hard to find. This makes it necessary for the focus to be kept on prevention, especially in a country where thalassaemics usually come from a poor background and cannot afford quality healthcare. Legislation for premarital screening must, of course, be accompanied by a strong public awareness campaign aimed at making the risks of having thalassaemic children clear to couples planning to marry, especially if they are cousins. It is true that cultural taboos obstruct an open discussion on the subject. But shying away from it will result in more and more 74 children being born with a genetic blood disorder that makes their lives hardly worth living. In this scenario, ties of kinship should not be a leading consideration. We should follow Iran’s example. For all that country’s conservatism, couples in Iran are required to undergo premarital screening. Over the years, this, together with genetic counselling, has resulted in a 70 per cent reduction in the projected number of infants being born with the disorder. There is no reason why Pakistan cannot follow suit. (Dawn-7, 02/05/2007) Promised kidney centre for workers not yet operational KARACHI, May 1: A 50-bed kidney centre has yet to become operational despite the fact that promises of the muchneeded health facility for the city’s working class was made about 10 years ago on May Day. The then government had promised that kidney centres would be established in the provincial capitals and Islamabad for provision of diagnostic and dialysis facilities to workers, as most of them suffered from various kidney conditions, especially stone formation. A heath official associated with the Sindh Employees’ Social Security Institution (Sessi) said his institution had been unable to treat all kidney patients at its hospitals. Under the social security scheme, he said, there were around 325,000 secured workers with 1,625,000 dependents who were given specialised medical care at the Sessi hospitals. Although the building had become ready three or four years back, the kidney centre is yet to be made functional. “Almost every month we hear that the centre is being made functional in a couple of weeks,” said some workers in Landhi area, where the building is located. They urged the government to do the needful before the equipment became rusty. Out of the five promised kidney centres, one at Lahore and another at Quetta have been made functional. The Quetta kidney centre is run by a private management. It is learnt that the recurring expenditures, including the staff salaries, of the Karachi kidney centre will be borne by the Workers Welfare Fund, Islamabad, for at least two years. The decision about withholding the centre or handing it over to the Sindh government or to the private sector would be made two years after the centre had started working, said a source privy to the goings-on in the kidney centre. Relevant quarters attribute the inordinate delay in the commissioning of the project to bureaucratic inefficiency, uneven flow of funds and some improper tendering for the procurement of equipment. The Workers Welfare Fund was originally tasked to make the centre, located near District Jail, Landhi, operational by June 2000. After a lot of correspondence, the posts of specialists, technical hands and paramedical and administrative staffs were cleared by the federal government, following which recruitments were supposed to be finalised in February 2006. However, things did not go as they had been planned and only 12 to 15 personnel, including one medical superintendent, had been selected who were yet to assume duties, said a source. A visit to the centre showed that various equipment and laboratories as well as wards had been put in place at a cost of Rs150 million with the objective of undertaking diagnosis, dialysis, surgery, lithotripsy, intensive care and relevant tests. These facilities can be run only by experts, who have yet to join duties. Once the centre is operational, it is likely that about 40 to 50 patients will be given renal dialysis treatment everyday in addition to OPD facilities and consultations. Kidney Centre Project Director Dr A. Haseeb Qureshi, a senior doctor employed by Sessi, said the project had great employment opportunities. Since the WWF had agreed to allocate funds for payment of salaries and allowances to doctors and other staff in its 2007-08 budget, recruitment process had once again been initiated, he said. According to Dr Qureshi, the second phase of recruitment for which ads have already been placed in newspapers will commence with the interviews of candidates on May 10. “We hope to finalise the appointment of about 150 medical and paramedical staff by the end of May,” he said, adding that tentatively the kidney centre would be made functional in the first week of June. About the purchase of equipments, he said 90 per cent of equipment had been procured and their installation was in progress. Twenty dialysis machines, lithotripters-CR, ultrasound machines, motorised-belt for ICU, ventilators and monitors had been commissioned. The 50-bed centre with general and private wards have a complete laundry unit on its premises. All workers registered with Sessi and the Workers Welfare Sindh along with their dependents will be treated there free of charge. The annual expenditure to run the kidney centre is estimated at Rs85 million. However, if the Sindh government or Sessi did not agree to provide the recurring budget, the feasibility of the centre could be assessed again after two years and it might be run on a no-profit-no-loss basis, the sources said. (By Mukhtar Alam, Dawn-15, 02/05/2007) Govt help for private hospitals on Aids KARACHI, May 2: The provincial Aids control agency has decided to extend its test, treatment and counselling facilities to patients of HIV or Aids registered with private hospitals. A source in the Sindh Aids Control Programme (SACP) said that it was sure that the number of people living with HIV in the province had been on the increase, adding that such people were not in the government network for any systematic care and attention for various reasons, making it difficult to say how many of them needed or had been receiving antiretroviral (ANT) therapy.Against estimated 35,000 HIV positive cases in Sindh, only 1,778 HIV infections, including 108 full-blown Aids cases, have been reported to the SACP till March 31, 2007. Of them, 134 are registered with the control programme for ARV treatment, CD4 test (a cell count meant to check the immune system of people living with HIV/Aids), and other purposes. 75 The patients were either shy of contacting doctors or did not have the courage to be tested and treated for HIV/Aids due to social taboos, he added, saying that in such a situation it was not possible to say how many of them needed or were receiving antiretroviral therapy. According to health circles, well-off male migrants who visit sex workers abroad and had the likelihood of infection transmission within them, after returning home contact private practitioners or hospitals for relevant tests. But it is not known how many of them are found positive or provided with treatment (definitely a costlier one), added the source, saying “had the hospitals made it a practice to report the number of patients suffering from HIV/Aids or referred them to the provincial Aids control programme for a follow-up and treatment, things could have proceeded more easily and in a scientific way.” It is said that low knowledge about HIV/Aids among the general adult population/vulnerable groups, high prevalence of risk behaviour, limited use of condoms and poverty are the main causes of the prevalence of the disease. The SACP focuses on the high risk population, advocacy, blood safety, prevention of sexually transmitted infections, care and support. The Provincial Programme Manager on HIV/Aids control, Dr Arshad Mahmood, said that there were over 26 voluntary counselling and testing centres for confidential HIV/Aids testing with the facilities for pre- and post-test counselling, while another 46 STI clinics had been established at teaching and district headquarters hospitals for management of the infection in question. Besides, a centre of excellence is functioning on the premises of the Services Hospital, Karachi, where patients registered with the SACP are treated and provided relevant facilities and counselling on a regular basis, he said, adding that another similar centre had been established recently at Larkana, which would be functional as soon as the relevant medical staff was trained. He said that another centre of excellence was being set up at the Jinnah Postgraduate Medical Centre, while a centre for prevention of mother-to-child transmission of the virus was also being set up at the Civil Hospital, Karachi. Dr Mahmood said that it had been decided in principle to provide medicines and CD4 cell count test facilities to patients coming from any institution, including private hospitals. The idea was not only to attend to the patients, provide them with services required for the treatment and prevention of infections and follow ups and counselling to their families, but to also ensure a scientific access to all HIV/Aids patients, he said. He said that it was also under consideration that a network should be developed with the support of private hospitals and medical practitioners to get at least the number of HIV/Aids cases they had been handling, so that a real assessment of the situation and quantum of the infection could be , instead of planning and working on the basis of estimates only. (By Mukhtar Alam, Dawn-17, 03/05/2007) Mothers abandoned in their twilight years By Zofeen T. Ebrahim KARACHI: Lives soured by neglect, shunned by relatives, given scant attention by the government, a growing number of mentally challenged women and children have found a safe haven in Edhi Centre for the Mentally Ill Women in North Karachi. Theirs is a tale of shame, remorse, human neglect and abandonment. Bent double, octogenarian Khatoon Begum is a victim of physical violence and the perpetrators are none other than her own family. Defending her son, she says: “It’s my daughter-in-law who hits me with whatever she can lay her hands on. It can be a rolling pin, a broom or even a pair of tongs. If not that then she will kick me.” The indignity of living a life where she’s an unwanted person in her own son’s house brings tears to her eyes and she cries uncontrollably. “For the last 22 years, since my husband died, I’ve not seen a day’s peace. I’m not even dependent on them for money as I get my husband’s pension all of which I give to them, then why can’t they treat me like a human being? I’m probably the most unfortunate mother. I do try to keep myself busy in prayer, but even that does not bring me solace. Sometimes I just feel like dying. I am sure that will bring me peace.” What should have been the responsibility of the state, is taken over by people like the Edhis. “Our leaders cannot look after the youth, what to talk of the aged,” rues Anwar Kazmi, secretary to Abdul Sattar Edhi and his companion for the last 40 years. Their North Karachi centre, built over 10 acres, was set up in 1986 with just 50-60 mentally ill women. Over a span of 21 years, the number has swelled to accommodate 1,540 of which 600 are above 40. Around 40 died this year mainly due to old age. “Relatives of only four came after they were informed, to pay their last respects, not to take the bodies. It was left to us to prepare their last rites and bury them,” says Anwar Kazmi,. In just five months, this year, 370 women were admitted to the Edhi Centre, of whom, he says, 30-40 were young and healthy, both physically and mentally, and thus sent to the Sohrab Goth centre for destitute women. “For the life of me, I never thought I’d be spending the latter part of my life here,” says Rashida Anees, 57. For Anees, once a teacher at schools like Mama Parsi and Habib Girls, this centre is her salvation where she has been living since 1999. According to her, her two brothers and their wives didn’t want to keep her or her younger sister, 55-year old Shakira, after the death of their parents. Extended family system which meant three, and in some cases four, generations living together, is fast diminishing in this cosmopolitan town of Karachi. “It’s time to face the bitter reality. Ours is a society at crossroads. In this age of the internet and cable TV, through which we imbibe the western cultural values coupled with increased economic difficulties is taking a toll on the joint family system,” explains Kazmi. At times, he says, families do take care of the mentally challenged woman for as long as they economically can. “But when it becomes impossible, many let their aged parents adrift.” 76 While they may be kept under lock and key (which the Edhi authorities say is done for their own security) but here they are not beaten up or ignored. Their daily needs, including their health needs, are met; they get three square meals a day, are kept clean, given clothes to wear and are taken care of. Bilquis Bano, 52, may have three “happily married” sons but she’s been living at the Edhi home now for 21 years, since the North Karachi centre opened. “I had dishonoured my family because my husband slapped me with a divorce. My brother brought me here in 1986,” she says, adjusting her dupatta on her bald head. The last time the sons took her home was on Eid. In charge of her room, comprising 60 women suffering from various degrees of mental anguish and of different ages ranging from 35-year-old Saba Ashfaq to the vitriolic Mumtaz Begum, 70, Bano helps with the daily chores like taking care of the sick, bathing them, helping them change clothes and wash up; taking them to the toilet and ensuring that everyone takes her medicines. “The centre is run by public philanthropy. We have no dearth of funds and these women are taken good care of,” says Kazmi. “We have very little paid staff as the healthy ones take care of those who are sick. “Most of these women are from the lower-middle class, who have been dumped by their very kith and kin. If you ask me, except for a few who have been admitted to the Pagal ward (ward for the mentally sick), not one of these belong here. They need to go home, to their loved ones,” says Waseem Fatema, a staff nurse, who knows each and everyone of the inmates by name and has their personal history at her fingertips. Neatly dressed, hair made up with a bit of make-up, Zainab Shafiq, 35, who is watching the women interviewed joins in. “If the Edhis didn’t have this place, where would people like us go?” She cannot thank the couple enough for keeping her. With two brothers and two sisters, she was sent here by her sisters-in-law two years ago. A Master’s in psychology, she says: “I never thought I’d get such a good first-hand experience working with mentally challenged patients, and so many of them!” “These emotionally disturbed people need to live among their loved ones. Staying away from home and their family and living with others like them only aggravates their condition,” is how Dr Naseem Atique, the doctor sees the situation. According to her most women have been thrown out or have come of their own volition because of quarrels between mother-in-law and daughter-in-law. “With less tolerance, in the power struggle, the strong one stays at home, the weaker one is shoved out to fend for herself.” Ironically, not a single woman spoken to blamed the sons or the brothers for their predicament. It was always their wives who were the evil doers. Most believed the latter had cast an evil spell on their men who were unable to see right from wrong and unable to make sane decisions. Ninety-eight-year-old Ramazan Bibi is one such mother, who refuses to admit that her three sons have dumped her at the Edhi centre. Squatting on toes, she slides to come closer and be heard. “She has three sons, two of them abroad, and one here, but nobody wants to keep her. After the death of her husband, she worked in different houses as a domestic help and ensured all three of them completed their education,” explains Dr Atique. “They don’t know I’m here and in any case I’m here for a short while, till my nephew finds me a place,” defends Bibi. She has been here now for a year, and has spoken a number of times to her sons. (By Zofeen T. Ebrahim, Dawn-17, 03/05/2007) Trainee nurses forced to do night duty KARACHI, May 4: First year students of Civil Hospital Karachi’s (CHK) Nursing School are forced to do night duties, often without the supervision of a staff nurse, soon after their induction. Besides being in gross violation of the Pakistan Nursing Council’s (PNC) rules, this practice puts patients’ lives at risk. The CHK daily caters to about 3,000 to 4,000 patients in the out-patient department, apart from 800 to 1,000 patients in the emergency section. But despite being a prime healthcare provider in the public sector, the hospital lacks basic facilities and has been facing a severe shortage of staff for over a decade, as there is a ban on recruitments. Though there are 262 nurses for the hospital on paper, many have gone on casual and maternity leave, while others have left for training and post-graduate studies. The nurse-to-patient ratio is as high as 1:50 at the hospital. To bridge this huge gap, trainee nurses are asked to do night duties. Resultantly, the ultimate sufferers are the hapless patients, who have nowhere to report their grievances. It is reported that some first year students had to join night duty as early as the fourth month after joining the school. “Not only this, we are called for night duties on public holidays. In fact, there are no fixed hours. We can even be called at midnight in a crisis-like situation to perform the duty for a staff nurse who, for some reason, has left early or hasn’t turned up. Night duties are also used as a means for punishment,” a student nurse said. This practice violates the PNC rules, which clearly state that there should be no night duty in the first year of general nursing training. However, in the second, third and fourth years, students can work at night for only two months, and that too under the supervision of a senior staff/head nurse. About the risks this practice poses to a patient’s life, a student said that once she gave a higher dose to a patient, which resulted in a sudden rise in his blood pressure. A doctor had to be called to handle the situation. “Taking care of 50 patients’ lives at night, when you have no clue how to administer even an injection or how to give a specific dose, is too much too ask from us. The seniors are not around and at times we have to take the sweeper’s help for simple medical procedures. The doctors, on the other hand, embarrass us by questioning why we are here in the first place, if we don’t know the basics,” said another trainee. The students complained that they are hardly taught anything at the school, and that their entire four-year education depends upon their self-learning at the hospital. “The school lacks competent staff and often, trainee nurses have to perform duties in a specific ward to ask a doctor for a lecture,” they said. 77 Another major concern is the meagre stipend they receive. According to the PNC rules, the stipend of a student will be according to the revised basic pay scale of a staff nurse, in addition to the prescribed mess and uniform allowances. Going by this rule, the stipend of a trainee nurse should be at least Rs4,500, excluding the uniform allowance and mess charges. However, at CHK Nursing School, students get Rs1,500 as a stipend, and that too, often late. “Our colleagues at Abbasi Shaheed Hospital and Jinnah Postgraduate Medical Centre Nursing Schools are getting around Rs3,000. But why are we discriminated against? Until last year, Rs500 were cut as mess charges from our stipend,” they observed. Trainee nurses also complained about the conditions of their hostel and the food they are provided with. “After the girls stopped eating in protest over the quality of food, the administration decided to provide us with food from zakat funds, the same which is prepared for patients. This tasteless food is far better than the unhygienic fare, which often contained insects,” they claimed. After a turbulent training period of four years, most of these students end up in private clinics and hospitals, due to the ban on recruitment. There have been no fresh appointments and promotion of nurses in the CHK for a long time. However, Chief Nursing Superintendent, CHK, Nasreen Gill maintained that the school is providing the best facilities to its students. On the stipend issue, she said that an application is pending with the finance department, and as soon it gets approval, the stipend amount will be raised to Rs4,500. (By Faiza Ilyas, Dawn-17, 05/05/2007) The need to act The Pakistan Pharmacy Council, the National Council for Tibb, the Pakistan Homeopathic Council, the Pakistan Nursing Council and the Pakistan Medical and Dental Council are the regulatory bodies working under the ministry of health. In civilised countries such regulatory bodies do not work under the government. They are independent bodies enjoying autonomous status and have the power to implement rules and regulations in the interest of the profession they are associated with and of the general public. A majority of their members are elected members. They also have representatives from the government, civil society and other stakeholders. In Pakistan the story is different. Every government —democratic or military -- hates autonomous, independent regulatory bodies. It wants them to work under the federal secretary and director-general of health. It does not want them to do things according to rules and regulations. The PMDC is an example in this regard. When this body was first formed, the government did not allow it to work independently. It appointed a secretary in collaboration with council members (95 per cent of whom were govt servants) and used the PMDC to promote the interest of politicians and some individuals. The following are some examples: — The establishment of medical colleges without infrastructure in public and private sectors. — Increase in the number of seats in medical colleges on the order of prime ministers, governors and chief ministers without increasing the required facilities at the centres. — Allowing sons and daughters of political leaders, army generals, judges of high courts and influential people to get admitted to reputed colleges. — Recognising dubious degrees, diplomas and qualifications from other countries. — Recognising medical institutes of foreign countries without proper assessment. Unfortunately it was all done in the presence of principals of medical colleges of Pakistan, provincial secretaries of health, dean of the faculty of medicine and some elected members of the council. The secretary of the PMDC in collaboration with council members and the executive committee did everything possible to destroy medical profession in Pakistan without taking into account the general public’s health, medical education and the training system in Pakistan. The following are the results of such acts: — The establishment of medical colleges and dental colleges in public and private sectors without proper infrastructure, faculty or premises. — The production of hundreds of glorified MBBS quacks. — The promotion of quacks and organised quackery all over the country. — No disciplinary action against unethical and criminal activities of doctors and hospitals in government and private sectors. In our neighbouring country India things are different as far as medical education and training are concerned. They have a very strong, independent and autonomous Indian Medical Council and because of it they now have a system of undergraduate medical education recognised all over the world. They also have a national training programme for postgraduate education and training. There public and private sector hospitals are doing everything which is done in modern countries like the US. Our political leaders and military rulers are ready to compete with India in making atomic bombs, missile systems, submarines and advanced air war fighters, but they are not willing to compete with it in the areas of health, medical education, training of doctors, nurses, midwives and paramedics. The development of healthcare sector in India was made possible because they concentrated on the formation of independent regulatory bodies despite there enormous anti-people defence programme. Another good example is the training of nurses in India. Their nurses are acceptable all over the world. Every year thousands of them are employed in industrialised countries to run their health system. In Pakistan the health department is always found busy controlling regulatory bodies. Because of the unnecessary interference of the health department we have a nursing council which is not able to perform its duties. Like our medical education and training system, nursing education is not good enough. All matters related to nurses’ training and education should be dealt by this body without any interference from politicians or vested interest groups. No different is the situation with Pharmacy, Tibb and Homeopathic councils. 78 All over the world, patients’ care and the health of the nation depend on doctors, nurses, midwives, paramedics, pharmacists and health professionals of alternate medicine. Likewise, we need a system of healthcare in which our people could receive care which should be based on scientific knowledge, honesty and professionalism. We face serious challenges. Our children and women are dying because of unnatural causes. Polio, child blindness, epilepsy, diabetes and many preventable diseases still affect many Pakistanis. Our basic health units, primary health centres and rural health centres are not functional. Our tertiary healthcare hospitals are part-time institutes with part-time faculty members. We have extreme shortage of all kinds of professionals to run our healthcare system. To deal with these challenges we need to have regulatory bodies that can work without any fear. WHAT SHOULD BE DONE — Total independence should be given to regulatory bodies. — There should be democratically elected members of councils and executive bodies to run the affairs of relevant professions. -- There should be representation from government and private sectors to make councils more trustworthy. — There should be representation from civil society. A good government does not work for the benefit of vested interest groups. It is supposed to protect the rights of the common man. It is only possible when the government assumes the role of a monitor to make sure that regulatory bodies are working independently and performing there duties according to the mandate given to them. (By Dr. Shershah Syed, Dawn-The Magazine, Page-5, 06/05/2007) Gastroenteritis on the rise in city KARACHI, May 6: Hospitals and physicians accept that there is an increase in the number of cases of gastroenteritis in the city, but maintain that it is nothing unusual in the hot and humid weather. They said that people should avoid taking spoilt food and drink and exposure to heat for long periods as these could cause diarrhoea and vomiting. Parents should pay special attention to their younger children and restrict them from taking illprepared cold drinks and ice-lollies, they suggested. The medical superintendent of Civil Hospital Karachi, Dr Kaleem Butt, said that his hospital received 864 and 892 cases of gastroenteritis in February and March respectively this year, but the number soared to 1,478 with the advent of summer in April. These days, on average 30-35 patients per day, with the history of diarrhoea and vomiting, are reporting, he added saying that situation was all manageable and could not be attributed to any epidemic outbreak. Gastroenteritis patients are being brought to CHK from areas like Lyari, Chakiwara, Shershah, Keamari, Orangi, Nazimabad, some parts of which have got poor water and sanitation system and experience the episodes of contamination as well from time to time, said another doctor. It was learnt that so far any major collapse in patients had not been witnessed due to gastroenteritis. Doctors who were contacted by Dawn said that most of the gastro-patients were discharged from the hospitals the same day. A medical officer at Abbasi Shaheed Hospital said that there was not any unusual situation as he received 4-5 in his shift of 7 hours, but none in any critical condition. So far we have seen a seasonal situation, he remarked. Dr Iqbal Memon, vice-president of Pakistan Paediatric Association, said that he was in touch with physicians and paediatrics at the CHK and others practicing in Kharadar, Bhempura, Nazimabad and other parts of the city and could say that there was no unusual development. However, he warned that people, among other precautions, should also consume boiled water and not take overripe fruits. Though doctors did not find situation ‘very much alarming’, they suggested the water supply and sewerage agencies to maintain optimum measures for abetting contamination of drinking water at every level. A few of the doctors and specialists blamed that the increase in number of gastro cases in the interior of Sindh was all because people consumed unsafe drinking water. “Careless supply and consumption of substandard drinking water is not an unusual thing in Karachi as well, as we have been reading about the problem in one part of the city or other, which was mainly due to unchecked dilapidated sewer or old eroded and faulty water lines, one of the doctors expressed the view. (Dawn-13, 07/05/2007) Nurses’ complaints THE complaints of trainee nurses at Karachi’s Civil Hospital should not go unheeded. Not only are they indicative of the enormous work pressure and other concerns of the students of the hospital’s nursing school, they are also a reflection of what ails this sector in the country as a whole. Unfortunately, the nursing profession in Pakistan has never been given the kind of importance that it gets in many other countries — which is one of the reasons why there are relatively few entrants in the profession here. Little is done by the state to encourage the profession. In fact, there is far more focus on opening medical rather than nursing schools. Thus, it is not surprising that there is one nurse for 50 patients at the Civil Hospital when the recommended ratio is one nurse for about three patients during an eight-hour shift. Needless to say, overburdening nurses and forcing them to work long hours without relief can take its toll on the health of the patients who, under the prevailing circumstances, are deprived of the care they require. The government must play a pro-active role here by taking steps not only to remove grievances such as long working hours, poor pay and slow promotions, but also to enhance the image of the nursing profession in the eyes of the public. Nurses are often made scapegoats for the mistakes of doctors and are also subjected to the rude and insulting behaviour of both medical colleagues and patients. This attitude is contributing to the dearth of professional nurses, many of whom look out for jobs in countries where they are more respected and better paid. The government would do well to highlight their contributions and encourage more young women to opt for what can be a very rewarding profession under the right conditions. (Dawn-7, 07/05/2007) 79 Overzealous government bleaching water to death KARACHI: Water quality experts have detected excess chemicals in potable water that is being supplied to residents of Chanesar Goth, Mahmoodabad. Each year, as summer approaches, water borne diseases increase in the city and the administration starts using chemicals to purify the water. However, because of the absence of trained staff for the process, the standard measurements are neglected. Residents of unit No. 5 and unit No. 6 in Chanesar Goth have complained that the water they get from the supply lines smells like bleach powder. “It is not possible to consume such water,” said Shahid Husain, a resident of the area, while talking to Daily Times. The residents took samples of the water to Jinnah Postgraduate Medical Centre (JPMC) for analysis. It was discovered that the smell is caused by an excess of chlorine, alum, and bleaching powder, which are all used for the removal of hazardous elements from contaminated water. “We didn’t know exactly why it smelt strange, so we took samples to JPMC and found that it is because of the excess use of chemicals,” said Masoor Khan, an NGO office bearer that has worked on water issues in the area. Dr Huma Ahmed, a microbiologist at JPMC, said that during the purification process if the elements, especially alum and chlorine, are used in excess it could cause a disaster. Experts have expressed their concerns over the excessive use of chemicals to purify water. They said that such practices by the Karachi Water Sewerage Board (KWSB) could lead to epidemics. “The excess quantity of bleaching powder used to purify potable water could prove to be very harmful,” warned water-management expert Prof. Dr Noman Ahmed of NED University. “They could cause stomach disorders, especially in small children and the elderly, by causing diarrhoea.” Furthermore, such practices could also result in skin diseases, hives and rashes for anyone taking a bath in the water. “Bleaching powder could also disturb the secretions of enzymes, thus resulting in interruptions in the abdominal glands,” he said. All of the side effects depend on the quantity of the chemicals used as some amounts are not poisonous. He added that on the international level, the use of chlorine for water purification was prohibited. (By Amar Guriro, Daily Times-B1, 07/05/2007) Environmental pollution triggers asthma Environmental pollution is the major cause of asthma in Pakistan whether it is external pollution such as smoke of vehicles or factories or internal environmental pollution such as dust or cigarette smoke, said Vice Chancellor Dow University of Health Sciences (DUHS), Professor Masood Hameed Khan. While speaking at a seminar on asthma conducted by DUHS in collaboration with the Pakistan Chest Society, Khan also mentioned that celebrating international days for health awareness is good but what is more important is the need for proper planning to control harmful diseases. He said that medical experts, students, social welfare institutions and media can play a vital role in this regard. He suggested that workers of chemical and cotton industries should wear masks to protect themselves from asthma. The Director of Ojha Institute of Chest Disease, Dr Ashfaq Sadiq said that five per cent elders and 10 per cent children are affected by asthma in Pakistan. He said pets in the house, carpets and curtains can be a cause of asthma because they are agents of dust. He said the disease is not curable, however, with prompt treatment it can be treated and controlled effectively. Elaborating on the symptoms of the disease he said that every patient suffers from different ones. “Cough during the night and chest pains are common symptoms of asthma,” he said, adding that the use of the inhaler and nebuliser is beneficial for such patients. Also, a spirometry test to check the function of lungs can be helpful to access the condition of asthma and to control it. Dr Faizullah Shafqat, Dr Nisar Ahmad Rao and Dr Aisha Mehnaz also gave lectures. They mentioned that the smoke of cigarettes and Shisha can be major causes of this disease, while the use of ‘chalia’ is one of the major causes of this illness among children. They stressed that inhalers are crucial for asthma treatment and patients should not be afraid of using them - they are a means of direct delivery of the medicine to the airways. Inhalers are also a must if one wanst to avoid risk factors such as allergens, pollens, pollutants, medications like aspirin and beta-blockers. (The News-20, 08/05/2007) 15 in hospital after drinking well water in Gadap KARACHI, May 8: At least 15 out of 50 people, including women and children, who had complained of diarrhoeal episodes after consuming water reportedly from a seldom used well in Gadap Town, were rushed to the Jinnah Postgraduate Medical Centre (JPMC) for emergency treatment on Tuesday, said health officials. Deputy Director and in-charge of JPMC accidents and emergency department, Dr Seemi Jamali, said on Tuesday afternoon that in all 15 patients of ages between 10 to 60 years, brought to the hospital in the wee hours of Tuesday and the following morning as well, were provided treatment, but none of them was diagnosed as severe case of gastroenteritis. She said that a majority of the patients were given medications, while a very few of them had to be dehydrated. Those who had reported after midnight and the following morning had been discharged, she added, saying all of the patients had the history of vomiting and diarrhoea which they attributed to some wedding meals. The patients given treatment at the JPMC were: Jamila (25), Fauzia (10), Ghulam Ali (22), Sharif (20), Abdul Rashid (22), Mehnaz (60), Abdul Wahid (13), Ahmed Saeed (12), Mohammad (28), Sajid (22), Niaz Ali (28), Salman Mohammad (40), Razia (30), Hamida (20) and Abdul Ghaffar (50). The affected people are the resident of Haji Hussain Jokhio Goth, UC-3, Gadap Town, around 50km off the Super Highway. The health department of the city government has also set up a round-the-clock medical camp in the area since Monday, which provided primary care to people complaining about stomach problems, said a government official. 80 Contradicting the earlier apprehensions about outbreak of any disease due to food poisoning or major drinking water contamination, a source privy to the medical camp said that the area in question sans any piped supply of water mostly relied on 4-5 wells for their needs. In the wake of a marriage ceremony, which was held on Sunday, the area people decided to fetch water from a rarely used or almost abandoned well. Generally, they used water from the fit well, but they also consumed water for drinking and cooking from the faulty well to meet the increased requirement, a health worker quoted an area resident. EDO Health Dr A D Sajnani, who also visited the area of the affected people, said that relevant staffs had collected about 50 samples of water from different well, including the faulty one, nearby ponds, and home water-reservoirs to ascertain the chemical contents and overall quality of drinking water in the locality in question. He said that there was no major medical case and people normally complained about vomiting and diarrhoeal episodes. However, we have placed an ambulance for any emergency shifting to major hospitals in the city, he informed. It was further learnt that some people were also taken to some nearby private hospitals for treatment. (Dawn-18, 09/05/2007) Hospital waste CDGK begins exercise for proper disposal KARACHI, May 8: The City District Government of Karachi has begun gathering data about hospitals, clinics, health centres and laboratories operating in the city to streamline its hospital waste disposal system. Talking to Dawn on Tuesday, Masood Alam, the EDO for Municipal Services, said that at present about 125 hospitals and medical centres were availing of the city government’s incineration facilities for safe collection and disposal of hospital waste, including the hazardous waste. He said the city government wanted that more hospitals and health centres avail the incineration facility to become environment-friendly health facilitators. “At present we have no data about the health establishments and their daily generation of hospital and hazardous wastes,” he said, adding that the new exercise of preparing a union council-wise inventory of hospitals, clinics, healthcare centres, maternity homes and pathological laboratories would surely help the government approach the establishments concerned to observe safe medical practices. Those who are registered with the city government for incineration services are required to pay an amount, fixed against the number of beds they offer to in-house patients, on a monthly basis. However, there are reservations on the private hospital managements’ side about the yearly 10 per cent increase in the waste disposal fee. According to an estimate, there are about 3,500 hospitals, health centres, laboratories, and clinics operating in the city, generating about 25 tons of hazardous waste daily, besides other waste. But only 10-15 per cent of the waste is disposed of scientifically. In addition to those who are registered with the city government incineration facility, there are about 8-10 private and public hospitals which have their own medical waste burning system. The remaining hazardous medical waste is either handled with municipal solid waste or recycled or reused for financial benefits, which is surely an environmental concern. Under the Pakistan Environmental Protection Act, 1997, hospital waste falls within the hazardous waste category, and institutions improperly handling it can be prosecuted. However, EDO Masood is of the view that significant improvement can be made only when the government possesses a complete and reliable data about the hospitals and their waste generations. “We have tasked our field workers and inspectors to collect data, and as soon as the statistics and locations of hospitals and health centres are known, we will first go for counselling and coordination on the waste disposal. And if needed at any stage, we will also take stringent measures against the violators,” he added. (Dawn-19, 09/05/2007) One wedding and 65 sick people KARACHI: As many as 65 people suffered from gastroenteritis-like symptoms from village Haj Hussain in Gadap town reported to different hospitals Monday night, resident Ghulam Haider Baloch confirmed Tuesday. It is believed that they all ate food prepared with contaminated water. A resident of the village said that most people in the area use boring water from up to 500 boring spots in the area. It took 12 to 18 ambulances to transport them; around 20 patients were taken to Naeem hospital, 7 to Nihal hospital and 12 to Ibn-e-Hassan. The JPMC casualty in-charge said that 15 patients came, including children who were sent to NICH. The patients started pouring in at 1:00 a.m. They continued to come till 4:00 a.m. but as none came till Tuesday evening no more are expected. JPMC has been receiving 20 to 24 patients on a daily basis. This was not a gastroenteritis outbreak but a lot of people getting sick at a wedding ceremony, said EDO health Dr. A. D. Sajnani. They drank the bad water and ate food prepared with that water. The severe cases were sent to JPMC, he said, adding that doctors had set up a camp there and no casualties had been reported. Aside from the wedding guest fiasco, there have been fears that the city is faced with a problem. “During the 90 minutes I have received four patients from different areas and all of them are suffering from gastroenteritis due to contaminated water,” said Dr Sham Kumar, on duty at the JPMC causality Tuesday evening. The patients said that they were vomiting and had diahorrea. “My mother was all right till night but suddenly turned sick,” said Mehnaz Maqsood, a resident of Korangi No 3.5 at JPMC. “We took to the nearest hospital where she was given a drip but she couldn’t recover till morning. We then brought her here.” Mehnaz said that out of their family of 13, the children had also fallen sick. 81 Another attendant, Abdul Ghafoor, said that they had been living in the same place for 16 years and his mother got ill last year as well. “After every one or two months we receive water that smells,” he said. “This continued for a week and then my mother got sick.” It is not possible for them to boil enough water for a nine-member family, he said. Civil Hospital Karachi was also busy over the last three months. According to statistics provided by Medical Superintendent Dr Kaleem Butt in February they received 713 such patients, in March 926 and in April 1,324. (By Farhan Ahmed, Daily Times-B1, 09/05/2007) Liver patients face problems at JPMC KARACHI, May 9: People suffering from liver and lower stomach diseases say that the federal government-run centre at the Jinnah Postgraduate Medical Centre is unable to cater out-patients on a large scale. Interviews with patients and other stakeholders at the centre, the Pakistan Medical Research Council Centre for Gastroenterology and Hepatology, revealed that the government was mainly meeting the salary expenditure of 15-20 staff, among whom are researchers, doctors, lab personnel and other supporting staff. It is learnt that mostly the patients come to the centre from Jinnah hospital or other health centres of the city or from the interior of Sindh under a referral system for the specialised diagnostic and clinical and therapeutic procedures that were undertaken at the centre. Patients largely belong to the lower income strata who can not afford treatments at private hospitals. A couple of patients at the centre’s OPD on Wednesday said that they had to wait for a considerable period of time for consultation. “After some interviews, the staff concerned had given me the appointment for today,” said a woman patient, urging the authorities to arrange for a system under which patients could be able to see a doctor on their first visit without wasting time. A staff claimed that the centre was not an open-to-all facility like other OPDs, but a host of patients visited and wanted to be accommodated for a first time consultation which was not possible for the centre as it was not being resourced properly. In the absence of standard procedures and sophisticated equipment at most other government hospitals in the city, the utility and importance of the PMRC Centre cannot be denied, but the system of finalising appointments with doctors in advance helps maintain a discipline and provide sufficient time to a doctor and patient for consultation and examinations, according to another staff member. He expressed the view that a couple of government institutions were provided with state-of-the-art equipment and endoscopes for liver and gastrointestinal diseases procedures but these could not be utilised properly for want of expert hands in a required number. Tracing the history of the centre, a senior staff member said that it had been established under the health ministry as a research cell in 1968 and Prof Sarwar Jahan Zuberi, who also spared some of her personal lab-equipment for the purpose, had put in great efforts in its establishment. It was designated as gastroenterology research unit of the government in 1977 and finally adopted by PMRC. A long-term follow up is done on patients suffering from peptic ulcer disease, inflammatory bowel diseases, including ulcerative colitis, tuberculosis of GI tract, mal absorptive disorders, cancer of the GI tract, gall bladder disease, acute and chronic hepatitis, and complications like portal hypertension, hepatic coma, etc. Medicines are also provided free of cost to the deserving patients while the centre performs different tests and undertakes procedures and treatment at an affordable cost, comparatively much less than what is charged by private hospitals. It gets 1,000 to 1,500 new patients every year, in addition to old patients needing follow-ups. About 70 patients are seen on two out-patient days every week whereas on the remaining working days, therapeutic procedures, diagnostic procedures and biopsies are undertaken. All this involves three-four doctors and a couple of biochemists and microbiologists. Dr Waqaruddin Ahmed, Director of the PMRC centre, said that the centre was established with the aim of organising, promoting and coordinating research in the diagnosis and management of gastrointestinal and hepatobiliary disorders whereas the routine services provided at the centre included diagnostic upper GI endoscopy, therapeutic upper GI endoscopy, placement of plastic or self-expandable metallic stents in the oesophagus, biostatistics and its application in medicine. He said that the centre worked on out-patients basis while long term follow up was done on patients suffering from all kind of liver and GI related disorders. He said that efforts were being made for increasing manpower and introduction of some new machines to ease out the situation. He said that philanthropic support was contributing a lot to the provision of diagnostic and therapeutic procedures to patients from across the province. (Dawn-19, 10/05/2007) Alarming situation in govt maternity homes There are 40 government maternity homes in the sprawling metropolis of Karachi, which are supposed to cater to the needs of the poorest segments of the society. However, barring four or five, doctors are not available in these hospitals in the second half of the day, Dr Shershah Syed, a leading gynaecologist, told the News. Dr Syed, former general secretary, Pakistan Medical Association (PMA), said that if a pregnant woman arrives at the hospital after 1 o’clock, the delivery is conducted by an “aya” and even sweepers. “Seventy per cent of the children across the world are born during the night between 2a.m and 6a.m, therefore, all maternity homes should work round the clock,” he said. Prior to partition in 1947, there was Lady Dufferin Hospital, Sobhraj Maternity Hospital, a maternity home in Soldier Bazaar, Aga Khan Maternity Home in Kharadar, a maternity home in Eidgah, and a maternity home in Lyari. Furthermore, Holy 82 Family Hospital and Seventh Day Adventist Hospital also provided maternity services and they were sufficient to cater to the needs of the then thinly populated city of Karachi, Dr. Syed said. After the creation of Pakistan, the load on maternity homes increased immensely because of the influx of immigrants from India. According to the Government of Pakistan Census Reports, the population of Karachi in 1941 was 435,887. In 1951, it shot up to 1,137,667 indicating an increase of 161 per cent over a period of 10 years. In 1961 it was 2,044,044, and in 1998 it was 9,802,135. Today it has been estimated to be over 15 million. “It must be noted that maternity homes are not run by doctors alone but they need midwives, paramedics, ‘ayas,’ sweepers and security staff besides having basic facilities such as water and electricity. But, gradually, we are witnessing a sharp deterioration in these areas,” Dr Syed pointed out. “It’s the job of the City District Government Karachi to pay heed to these problems but sadly enough the budget is not being diverted to the health sector,” he said. “A society that does not care for pregnant women cannot claim to be civilised,” he said. He said that there should be at least 100 maternity hospitals of 100-beds each in the public sector, but our priority is to build a fountain worth 225 million rupees at Clifton. We have failed, miserably, to provide solace to the down trodden and the lower middle and middle classes. The gravity of the situation in the realm of maternal health in Karachi, as elsewhere in the country, can be gauged from the fact that one woman dies every 20 minutes in Pakistan due to postnatal infections, according to Dr Nighat Shah, a gynaecologist associated with the Aga Khan Healthcare Centre, Kharadar. Statistics indicate that the lifetime risk of maternal death for women in Pakistan is 1 in 31, while roughly 1 out of 10 children born in Pakistan die before the age of five. Among the factors contributing to maternal death and infant mortality, are high fertility rates, inadequate access to quality maternal and child care services, a low rate of skilled birth attendance, inadequate emergency obstetric and newborn care, low female literacy, poverty, and a heavy burden of communicable diseases, according to UNICEF. Professor Sadiqua Jafaray, President National Commission on Maternal Health (NCMH) said: “We don’t know the exact maternal mortality ratio (MMR) but it’s true that it’s very high in Pakistan. For the first time the National Institute of Population Studies is conducting a survey in Pakistan and its findings are expected to reveal the MMR by the end of this year.” She said the medical causes of maternal death in Pakistan include haemorrhage (bleeding), eclampsia (high blood pressure during pregnancy), obstructed labour, and abortion. “There are social and cultural causes of maternal death as well. Poor women are generally illiterate; they don’t know about complications and are malnourished. Anaemia itself can kill. Too many pregnancies during young age can also cause death,” Dr Jafaray, who is a leading gynaecologist, said. (By Shahid Husain, The News-13, 10/05/2007) 343 arrive in city hospitals with gastro symptoms KARACHI, May 10: Sindh Health Minister Syed Sardar Ahmad said that there was a static trend in the reporting of people with gastroenteritis or diarrhoea complaints at the government hospitals in the province, including those at Karachi.Speaking at a press conference at his office on Thursday, the minister said that on average around 1,600 cases of gastroenteritis or diarrhoea had been registered at various Sindh and district government hospitals and health care centres in the recent days. Majority of the patients are discharged after necessary examination and medications same day, he added, saying the problem was overall endemic in nature.He said that increase in vomiting and diarrhoea patients had become routine phenomena of the province during summers for the last few years, which could be attributed to a considerable concentration of contaminants in the Indus river water consumed by people or carelessness observed by them in the health and hygiene practices. The minister said that all government health care centres across the province, including the district hospitals and tertiary care centres had been alerted and equipped adequately in respect of manpower and medicines to handle any situation. Health personnel at all levels are distributing ORS and chlorine tablets in the affected areas in the interior of Sindh, he added and suggested that people should avoid taking improper food and consume boiled water only. Mr Ahmad said that people increased their water intake during summer; it was the prime responsibility of the local governments to ensure a safe drinking water supply to people in all areas, so that chances of spread of diseases could be minimised. He further informed that he asked all the EDOs (Health) in the province to launch a public awareness drive to protect people against possible gastroenteritis. EDOs will ensure that masses are sensitised and motivated for taking preventive measures at their level as well in regard to seasonal ailments, he informed. Giving updates on reporting of gastroenteritis cases from April 23 to May 9, the health minister said that about 18,000 people complaining of vomiting and diarrhoea came to hospitals across the province, out of which 5,500 were admitted for a thorough treatment. During the period in question, only two deaths have been reported from Sukkur district and one from Jamshoro, all children of 4-7 years of age, he informed. According to the data provided to newsmen by Special Secretary (public health) Dr Abdul Majid and Deputy Secretary Dr Shakeel M Mullick, 1,673 patients reported to hospitals and dispensaries of the government in 23 districts of Sindh on May 9, out of which 373 were admitted. 83 As many as 208 patients were received at Thatta district facilities, out of which 33 were retained, followed by Matiari 157 (23 admitted), Sukkur 88 (24), Khairpur 87 (25) and other districts. On May 9, at Karachi 343 cases were reported at government hospitals, including those 81 at the Civil Hospital Karachi. Among others, the town health officer of Lyari reported the registration of 21 patients, while THO Landhi reported 69 cases, THO Malir reported 25 and THO Bin Qasim reported 22 cases, while Sindh Government Hospital New Karachi received 15 and Sindh Children Hospital received 42 patients the same day. (Dawn-19, 11/05/2007) ‘50pc people at risk of iodine deficiency disorder’ KARACHI, May 11: The Sindh government and Unicef have decided to refocus their strategies against iodine deficiency disorders (IDDs), with the realisation that it is a national problem and not confined to the northern areas of the country only. At a meeting on Friday, representatives of the Sindh health department, Unicef, World Food Programme, Micronutrient Unit and NGOs stressed the need to tackle the IDDs issue afresh and effectively in the province. Preparing for a detailed planning and implementation guidelines to control IDD, the participants felt that universal salt iodisation (USI) was an effective measure to increase iodine levels in humans. They resolved that the Sindh government should be moved for the passage of USI legislation in order to ensure the maximum processing of iodised salt for human beings and discourage the common table salt at all levels in the province. A number of serious health problems like preventable mental retardation, cretinism, reproductive failure and deaf-mutism are mainly caused due to iodine deficiency disorders. Of over 2 billion people around the world, who are at the risk of IDD, more than 300 million are believed to be mentally impaired, while about 740 million suffer from goitre; thousands are either still-born or born as cretins. According to Unicef estimates, about 50 per cent of the population in Pakistan is at risk of IDDs. Every second child born is at the risk of IDDs, while 23 per cent of the school aged children and 36.5 per cent of mothers of children under five are severely iodine deficient. So far, only Balochistan and the NWFP have been able to introduce laws for a mandatory salt iodination, a process that is considered cost effective and relatively easy. Salt iodisation involves the addition of small quantity of iodine (30 to 100mg of iodine per kg of salt, or parts per million) in the forms of potassium iodide or potassium iodate.It was noted in the meeting that at present Pakistan was entering into the second phase of activities aimed at controlling IDDs through USI; there was a need to have national level commitment, with a sense of strategic direction, to achieve the targets of USI by year 2010 and IDD elimination by 2013. The Sindh government will launch the IDD control project on May 19 with the conduct of a seminar at Karachi, it was further learnt. Apart from the IDD effects like congenital abnormalities, goitre and its complications, decreased fertility and spontaneous abortions, the loss of IQ points in children living iodine deficient environment was also considered and decided that the point could help a lot in convincing parents to promote the regular consumption of iodised salt. Besides, making the communities at large, families and households realise the importance of regular use of iodised salt, it is also imperative that iodised salt should be made available in the market. Talking to Dawn, one of the participants expressed the view that it cost not more than 20 to 45 paisa per kg extra to the processing organisation for producing adequately fortified iodised salt as they were provided the mineral in question. Earlier, the government with the support of Unicef used to supply iodine to salt producers on subsidised rates and now the Micronutrient Initiative has been made responsible to continue the supply. Universal salt iodisation in Pakistan was launched in 1994, while the responsibility was shifted to the provincial government from the national NGO in August 2000. (Dawn-18, 12/05/2007) Researchers call for precautions to contain water-borne infections There is no virology laboratory in the country, with the exception of one which too is for research purpose, speakers said here on Friday at a press conference organised at Dow University of Health Sciences (DUHS). Vice Chancellor DUHS, Prof Masood Hameed, Prof. Khurshid Hashmi (Sindh Medical College) and Prof. Rafiq Khanani (Dow International Medical College) said the country prone to water- borne infection (bacterial, parasitic and viral) needs to contain it at all levels. Prof Hameed said that hospital culture of majority of stool samples collected from different parts of the province identified these to be bacterial or parasitic in nature. “Pakistan does not have facilities for viral assessment of the samples,” he said mentioning that viral infection as HepatitisA and D, which are also water- borne can, however, be diagnosed. Resource constraints, climatic conditions, poor education makes its necessary that institutions as Dow University of Health Science too play their role in motivating the masses to adopt all precautions. Prevention, he said was the key and simple interventions as conscious efforts to make available water free of germs, through simple and cost effective techniques can largely contain wide range of water- borne infections including gastroenteritis, cholera, dysentery, typhoid, diarrhea, hepatitis- A and E respectively. DUHS realising its responsibility has, in collaboration with Pakistan Infection Control Society, has undertaken a scientific research and identified Solar Disinfection as the most viable option for locals. Copies of a detailed document of the research is being dispatched to the Sindh Health Department as well as to Federal Health Ministry to streamline the experience, he said answering a question. 84 Prof. Masood Hameed also suggested close coordination between the media and health care professionals to sensitise people about personal hygiene, compulsory and proper hand-washing before consuming food, before cooking or getting involved in kitchen chore and before feeding kids. Avoiding consumption of stale food, over ripe fruits, contaminated water is also necessary, he said. Prof. Rafiq Khanani said a large number of people complained of diarrhea and vomiting at local hospitals and it was during last one month that 1400 patients were seen at the OPD of Civil Hospital only. Thirteen deaths due to gastroenteritis were reported during the last two weeks from different hospitals, he said and attributed it to use of contaminated water. Prof. Khurshid Hashmi, a senior office bearer of Pakistan Infection Control Society said boiling is considered to be the most appropriate method to make water safe but in our country boiling can not be simply afforded by many, leaving simple solar disinfectant technique as the alternative. “Pakistan being a hot climate country can benefit by simple intervention of exposing water contained in transparent plastic bottles to sun rays,” Dr. Hashmi said mentioning that it was simple and affordable for all. (The News-20, 12/05/2007) High gastroenteritis cases IT was shocking to hear Sindh Health Minister Sardar Ahmad’s disclosure on Thursday that in the previous few days around 1,600 cases of gastroenteritis were received at various hospitals in the province. Worse, from April 23 to May 9 the number totalled 18,000, of which 5,500 were admitted for treatment. Figures from May 9 show that around 200 patients went to healthcare centres in Thatta, 157 in Matiari, 88 in Sukkur and 87 in Khairpur. In Karachi, on that same day, 343 cases were reported from government hospitals. These are disturbing figures that crop up every year showing that the government has not devised a comprehensive strategy to prevent the outbreak and spread of gastroenteritis. It is not in Sindh alone where gastroenteritis outbreaks are causing misery. On May 7, this newspaper reported that three hospitals in Islamabad were treating 15 to 20 patients a day. The causes are the same: contaminated water and unhygienic food. Mercifully, there have not been a high number of fatalities from this waterborne illness. The health minister says his ministry is working hard, as are authorities in Islamabad, to contain the affliction by treating patients along with handing out chlorine tablets as well as ORS. The government must make sure that treatment facilities are taken to the rural areas where health facilities are inadequate and medicines for gastroenteritis are needed most. What are urgently needed are awareness campaigns in the media highlighting the dangers of contaminated water and the ways to overcome them. For example, it is crucial that people know that they must boil water for drinking and that food must be thoroughly washed before consumption. These messages can help prevent waterborne diseases. (Dawn-7, 13/05/2007) Incinerator needed at civil hospital KARACHI, May 15: Civil Hospital Karachi (CHK) needs a new incinerator for the safe and scientific disposal of medical waste it generates every day, as the existing one involves frequent repairing and high maintenance costs, in addition to falling effectiveness. This was observed at a meeting of the Board of Governors (BoG) of the CHK and Lyari General Hospital (LGH) on Tuesday. Chairman BoG, Abu Shamim M. Arif, presided over the meeting, which, among others, was also attended by newly posted Secretary of the Provincial Health Department, Mumtaz-ur-Rahman. The meeting was informed that the CHK incinerator, which was commissioned 10-12 years back, had almost completed its life and as such, there was a need to purchase another incinerator of international standards in the shortest possible time. At present the hospital charges one rupee per day from every out patient as hospital waste management fee. Since the hospital has no adequate fund for the purpose, the Sindh health department was requested to arrange for a special and bulk provision of funds on a priority basis for the purchase of a new incinerator, it was further said.A member privy to the meeting said that the hospital management has been assured of all possible support on behalf of the health department. The health secretary has also emphasised on proper disposal of hospital waste by the private as well as public sector hospitals. The CHK has over 45 departments and patients’ wards, with a capacity for about 1,900 in-house patients. In addition to patients, doctors and nurses, about 4,000 people attend to patients or visit as out patients every day, who needed a safe and infection-free atmosphere, a participant of the meeting told Dawn. QUALITY OF MEDICINE: The secretary also emphasised on the quality of medicine purchased by the CHK and directed that batch-wise sampling and testing of medicines should be undertaken by involving provincial and federal government laboratories. At present, a random sampling and testing of medicines purchased for the hospital is done either by the provincial or federal lab, said a source privy to the meeting. PURCHASES: In other business, the BoG approved the working paper of the LGH for the re-appropriation of Rs2.4 million for purchase of a telephone exchange, and the amount of Rs0.8 million for the repairs or service of equipment related to the operation theatre. In the case of the LGH it was also decided to grant permission to it for the purchase of equipment and furniture worth Rs21 million. The BoG also approved the decision for purchase of quality medicine on the recommendations of the Dow University of Health Sciences (DUHS) professors. OT COMPLEX: The meeting was also informed that a soft opening of the CHK OT Complex, comprising 14 operation theatres, will be performed on May 22, while the complex will be operational with surgeries on long awaited cases of cleft lip and cleft palate performed by a team of doctors from the plastic surgery department of the CHK and DUHS. Among others, the Vice-Chancellor of DUHS, Prof Masood Hameed Khan, Medical Superintendent of the CHK, Dr Kaleem Butt, MS of LGH, Dr Mukhtar Khawaja and Abdul Sami Khan also attended the meeting. (Dawn-19, 16/05/2007) 85 Inadequate toilet facilities contribute to renal disorders “The delay in passing urine can result in the malfunctioning of kidneys,” says Dr Sohail Ahmed Khanzada. An observation of people’s lifestyles in Karachi reveals that poor sanitary condition in public toilets discourages people from using the bathrooms while they are away from home for long-hours every day. A Karachi University (KU) student, Zufishan Asif, said, “Even if one tries to tolerate the bad smell and filthy conditions, he/she will still be faced with the absence of water facilities.” In some cases, if there are toilets, there will be a large number of users, resulting in long queues. Shopping centres, such as Millennium Mall and Dolmen Mall also lack basic facilities. Also, these bathrooms are not equipped to deal with so many users, which is why they often run of water. Sometimes these bathrooms are also used by the petty staff as a place to sleep. As far as public bathrooms are concerned, the situation is not very different. The toilet at Nipa Chowrangi is a case in point. Women cannot avail this facility because of the mess caused by various construction works in the vicinity. Under such circumstances, people prefer waiting to go home. However, “delay in urinating effects the bladder and disturbs the effectiveness of kidneys,” emphasises a homeopathic doctor, Dr Shahid Latif. Furthermore, extensive delays can cause stones in the kidney and bladder. Ironically, the number of public toilets in the city is inadequate while those available are not in no usable condition, especially for women. Toilets at Malir 15 are another example of why they are not used by the public. Besides being dirty and broken down, some of them don’t even have doors. A little amount is also charged for the use of these toilets but income generated does not seem to be utilised at for maintenance purposes. Toilets built at the Clifton beach also come under the same category. Hundreds of people are using them daily and paying for the services as well but if the money is not being used for maintenance work then where is it going? Doctors who campaign for adopting proper defecation practices seem to forget about the fact that even hospital bathrooms are in a very sorry state. Toilets attached to private rooms are provided with every possible facility but those allocated to general ward patients are intolerably foul. And this situation is not limited to government hospitals; many private hospitals are also found to be negligent towards maintenance and cleanliness. Psychologists believe that people become intolerant or irritable, lazy, morose and physically weak when they don’t make enough trips to the bathrooms. Taniya Khan, a patient, said she suffers extreme headaches after these long but unavoidable gaps. Doctors in Pakistan claim that better facilities of bathrooms across the country — both in the private and public sectors — can help reduce the escalating rate of kidney diseases in the country. Their argument is that the provision of proper facilities is the first step towards preventing kidney problems. It’s necessary to spread awareness regarding this issues amongst the general public, irrespective of their education, class, status or ethnicity, in order to have a healthy nation. The function of kidney is to maintain proper water and electrolyte balance in our body in order to regulate acid concentration and filter the blood of metabolic wastes, which are then passed out as urine. Infections in the kidney, bladder, and adjoining organs can lead to severe medical complications and need quick medical attention. Kidney disorders ultimately affect the whole body. Physicians recommend an intake of 14 to 15 glass of water a day to keep the whole system hydrated as it helps maintain the blood flow in the human body and also removes dirt and other useless particles. (The News-20, 16/05/2007) 50pc population at risk of iodine deficiency KARACHI, May 19: Agreeing that universal salt iodisation (USI) is the fittest line of attack for elimination of iodine deficiency disorders (IDD) in human beings, public and private functionaries at a ceremony here on Saturday pledged to promote active cooperation among themselves for success of iodine supplementation programmes in the province. Like in many other countries, almost 50 per cent Pakistan population is at the risk of IDD. Iodised salt consumption in Pakistan is less than 20 per cent as against 100 per cent in some other countries of South East Asia like Bhutan and Nepal, followed by Bangladesh (75 per cent), Sri Lanka (75 per cent), Maldives (66 per cent), India (60 per cent). Speaking as chief guest at the launching of the provincial IDD/USI project, Sindh Minister for Health Syed Sardar Ahmad described the IDD threat as alarming, stressing that the issue needed to be addressed genuinely at all levels. He promised that legislation for USI would be made soon to ensure 100 per cent use of iodised salt and ban the noniodised salt. He said EDOs health could play an important role in the implementation and execution of relevant laws and rules at grass-root level. He was critical of many of the federal health initiatives, saying that health was a provincial subject and federal government should minimise its role as far as the functioning of the sector at provincial level was concerned. “Every now and then, provincial health officials are summoned to Islamabad for meetings which don’t prove helpful in resolving health issues, rather result in wastage of time and money.” Deputy Director General, Health (Nutrition), Zahid Larik suggested phasing out subsidies for salt processing, pointing out that salt producers were provided iodine at lower prices by the government for iodisation of salt but the iodine was sold away to other parties illegally. Prof Zulfiqar Bhutta of the Aga Khan University said that majority of the rural and urban population did not use iodised salt because it was either expensive or not available in their areas. They also feared adverse effects of its use. On the basis of the findings of his research survey conducted in Matiari, Khairpur and Bilal Colony (Karachi), he said only 20 per cent of population in Sindh used iodised salt adequately. One major concern appeared to be fake iodised salt as well, he added. According to Prof Bhutta, 30 per cent of rural and 74 per cent of urban areas told surveyors that they had heard about iodised salt. He also stressed the need for compliance and quality control on the part of the industry, increased advocacy, massive media campaign and consistency in the relevant policy to achieve the desired results in promoting use of iodised salt. 86 Dr Ayub Rose of the Micronutrient Initiative, Islamabad, said that IDD was one of the major micronutrient problems affecting about 1.65 billion people – 655 million with goiter and 11 million with cretinism – in the world. According to a survey conducted in 2001-2002, prevalence of goiter among women was 21 per cent and school-age children 6.7 per cent in Pakistan, he said. He was of the view that the national IDD control programme launched with the assistance of Unicef in 1994 had a limited impact. Dr Mazhar Alam of Unicef, Sindh, said iodine was an essential element for the functioning of human body and also helped address the problems like mental retardation and brain damage. In Pakistan, about 23 per cent school-age children and 36.5 per cent mothers of small children (less than five years) had severe iodine deficiency, he stated. Special Secretary (Public Health), Sindh, Dr Abdul Majid said that in Sindh, consumption of iodised salt had decreased due to various reasons, but now the health department had already started working on a comprehensive strategy for reaching all stakeholders. The ceremony was organised jointly by the Sindh health department and Unicef, Sindh. Dr Asif Aslam of Unicef, Dr Shakeel A. Mullick, Dr Jamaluddin, Dr Nadeem Shaikh and Dr A. D. Sajnani also spoke on the occasion. (Dawn-18, 20/05/2007) ICU patients flee fire at heart hospital KARACHI: A fire erupted in a hospital in Federal B Area, Sunday night, causing wide-spread panic and chaos. The fire, which started in the angiography room of the Institute of Heart Diseases, created pandemonium throughout the hospital. Patients were seen gasping for air as they desperately made their way outside. The police finally managed to control the fire after breaking into the locked angiography room. According to initial investigations, the fire seemed to have been sparked by an electrical short-circuit. Patients in the departments next to the angiography room, such as those in the Intensive Care Unit (ICU), suffered the most as smoke quickly spread to all the nearby rooms. The hospital administration was quick to act as it called the police, the fire brigade department and KESC. “Within 45 minutes, we had broken into the angiography room and controlled the fire,” said DSP Azizabad, Ejaz Hashmi. “The fire itself wasn’t really a problem, however, the smoke created some serious issues. We had also asked KESC to disconnect the power supply temporarily so that we could carry out our operation.” Hashmi mentioned that six patients had been moved to the ICU because of excessive smoke exposure, whereas 20 other patients were shifted to the hospital’s gardens, on the directives of doctors, to allow them to get fresh air into their lungs. Furthermore, 80 other patients managed to exit the hospital’s building on their own. Meanwhile, fires broke out in a private school and a warehouse Sunday in two other incidents in the city. A fire erupted at the Ahmed Grammar School, Ittehad Town, inside Mochko police limits, and destroyed school records and furniture. The school owner, Waseem Ahmed Abbasi, has filed an application at the police station stating that he suspects that the fire was started intentionally. The police, however, believe that the fire was accidental. In another incident, Al-Noor Enterprise’s warehouse in Machar Colony caught fire. According to the fire brigade’s spokesman, two fire fighters managed to put out the flames after a two-hour struggle. The police said that Mushtaq Pani Wala owns the warehouse and that it is reportedly insured. The owner has claimed that more than nine thousand plastic drums worth 2.2 million rupees have been burnt. (Daily Times-B1, 21/05/2007) ‘22pc suffering from hypertension in Pakistan’ HYDERABAD: Experts at a seminar said on Monday that high blood pressure is a curable disease and when it is 140/90 or higher it must be treated timely. The seminar titled “Complications of Hypertension & Its Management” was orgnaised at the Isra University Hospital here to mark World Hypertension Day. Renowned professors Dr Feroz Memon and Dr Abdul Rasheed Shaikh, the cardiologist and the nephrologist, respectively, addressed the seminar. The professors elaborated that 33 per cent of people all over the world were patients of hypertension (blood pressure), while 22 per cent of the people in Pakistan had that medical condition. However, they said, only three per cent of people of the country are able to control their Hypertension. They told the seminar that high blood pressure could be a major risk for other diseases such as heart stroke, blindness (retinopathy) and renal diseases if no treatment was availed of by patients timely. They said about 50 million people suffered from high blood pressure in the United States alone and blood pressure of 140/90 or higher on two or more occasions must be treated timely, otherwise it could be a major risk for other diseases like heart problems, including heart stroke, blindness (retinopathy) and renal diseases. The speakers gave lectures on different aspects of hypertension and its renal complications, cardio vascular complications and its treatment plan. They emphasised lifestyle modification and continuation of medical treatment. They further said that hypertension was on the rise due lack of proper awareness. In fact, only three per cent of the patients of hypertension were able to keep their blood pressure under control in Pakistan. The speakers strictly advised people not to ignore this disease because high blood pressure can cause fatal diseases such as heart attack, paralysis, kidney failure and brain haemorrhage, adding that the patients of high blood pressure should keep bodyweight normal, take regular exercises, have half an hour daily walk, use less salt, avoid fatty foods and smoking. Dr Abdul Ghani Kazi, Director Isra University Hospital, talked about exercise, dietary plan and put emphasis on the treatment of hypertension properly and timely. However, he advised the participants to be more focused on lifestyle modification. A large number of professors, postgraduates, students, nurses, paramedical staff and general public attended the seminar. (The News-3, 22/05/2007) 87 Weight loss pills: Drop in weight, or loss of health? The advent of the ‘instant’ culture in society means that everything has been made more convenient for the consumer who is short on time. Companies have made attempts to make everything ‘instant’ and ready to use, without causing any delays. While this may work for fast food, the same cannot be said for medication. More serious is the issue of medicines being sold in the market, which are not only advertised, but are also marketed with “instant” solutions. In most cases, the purposes are not achieved but they play with the consumers’ psychology, and may even cause serious and chronic side effects. One of these instant solutions are weight loss pills. These concentrate on a person losing weight without any exercise, in an average of a couple of months, only by taking pills or drops. The market for weight loss pills is not small, and there are many who are attracted by the tempting posters that are plastered along walls and the banners all over the city, which show before and after images of people. These claims are also questionable. Since the problem of obesity is on the rise, especially with the advent of the fast food culture, this is an increasingly “expanding” market. It is a golden opportunity for companies to introduce ‘magic pills’, which will help obese or fat people in losing weight. One of the most major results of this is that people have altogether stopped exercising because they feel that a medicine will work better and faster. Former Additional Medical Superintendent of Civil Hospital, and now a private practitioner, Dr Munawwar Qureshi, while highlighting the problems of these pills, said that cardiac problems are one of the worst side-effects of using them. Other effects include palpitation, tumors, slowing down of mental capabilities, with the patient generally feeling weak and dizzyness. “Any good doctor will never prescribe these pills for weight loss,” he said, condemning the drugs. “These can only be prescribed by quacks and frauds, who only want to make easy money.” Qureshi, instead, recommends a brisk walk everyday, a serious reduction in the consumption of fatty, oily and sweet foods, and a cut down of starch and carbohydrates by at least one half. He also strongly discouraged the consumption of bakery products as the oil used is mostly unsuitable for health purposes. “Every doctor should be registered by the Pakistan Medical Association, with a registration number and they should put their degrees up in their offices, for the patient to know. It is because of unregistered doctors and quacks that today pills of these kinds, which are more for profit rather than curing problem, are being sold in the market.” Out of the pills being sold, most are homeopathic. One of these is manufactured by Schwabe, a well known German company, and the medicine is known as Phytolacca Berry sold mostly in a 20 gram bottle. The prescription says that the medicine will help by ‘dissolving excess fat’, and ‘reducing hunger’ but it does not say how. All it guarantees is ‘results in two to three months’, and that it has ‘no side effects’. Another very commonly-sold drug is called ‘Slim Drops’ manufactured by Mektun Homeo-Pharma, in Karachi. The ingredients for this medicine includes not only phytolacca berry, but also fucus, asafetida, Abis can, graphites, and helianthus. A cardiologist at Civil Hospital, Dr Afzal Qasim says that the main function of weight loss pills is to increase metabolism, but eventually, long term usage of these pills affects the function of the pulmonic valve, resulting in valvularpathy. According to the opinion of a ‘herbal doctor’ or hakim, Syed Zohair Ahmed, people have now become materialistic and are attracted by superficial ideas, and therefore, are easily persuaded by advertisements and marketing campaigns. “These are all tactics to fool the consumer who spend so much money only to gain a certain status in society, by looking good.” Ahmed thinks that these medicines and others similar to these are supported by authorities and the government, which is why they are still available in the market. The shopkeepers who sell these medicines say that the customers not only buy these medicines once but they keep coming back for more. They also say that many show prescriptions for these pills, which mean that there are doctors out there who are supporting the usage. Qureshi echoes Zohair’s thought in saying that the only way in which these medicines can be stopped from entering the market is by strengthening the writ of the government’s health department. The Ministry of Health, both federal and provincial, should not be allowing these medicines in the market, irrespective of them being imported, or of being allopathic or homeopathic in nature. There should also be strict control on the advertisement of pharmaceutical drugs, and also on pressuring consumers to resort to unhealthy means of losing weight or solving other physical ailments and problems. For the consumers, they should realise that there is no magical way to lose weight, and that they should recognise their right to be informed about a particular product before purchasing it, and not fall prey to the power of persuasion of advertisements. (By Xari Jalil, The News-20, 22/05/2007) Three-day workshop begins 9,000 born with cleft lips, palates every year KARACHI, May 22: Nine thousand children are born with cleft lips or palates every year in the country and their proper rehabilitation remains difficult in view of the availability of a few plastic surgeons and lack of team approach for multidisciplinary management. These facts were highlighted at the inaugural ceremony of a three-day workshop ‘Recent Trends in Cleft Lip and Palate Management’, which was held at Arag Auditorium, Dow University of Health Sciences. The workshop was organised by the plastic surgery department in collaboration with the professional development centre of the university. 88 Giving details of the cleft lip/palate incidence in the world and Pakistan, DUHS plastic surgery department’s head Dr Mohammad Ashraf Ganatra said 132 million babies were born with cleft lip/palate or both in the world annually. Its incidence rate in Pakistan is one such patient in 400 births. Twenty five babies are born with cleft lip and/or palate daily out of 10,000 babies and that makes 9,000 new clefts just in a year. “According to a rough estimate, there are around 1.2 million untreated cleft patients in the world, of which around 300,000 are in Pakistan. In Sindh, their number is estimated around 50,000 to 60,000,” he said. In an ideal situation, he said, cleft surgeries should be conducted by plastic surgeons. But, he said, there was a dearth of plastic surgeons in the country. “There is no plastic surgeon outside Karachi and Hyderabad,” he added. Dr Ganatra said paediatric surgeons working in the interior areas of Sindh were doing a great job. But, he said it was necessary for doctors to learn new techniques to avoid complications and secondary surgeries. “A single operation if done properly can change the life of a child,” he said. Stressing the need for creating awareness, he said there were misconceptions about the birth defect as many people still linked it to lunar or solar eclipse. He said all such misconceptions needed to be removed. He underlined the importance of timely medical intervention and said that in cases of cleft palate, delay in treatment could cause irreversible damage to speech. Cleft patients were as common in urban localities as in rural areas. The only difference was that there was no awareness and facilities for treatment in villages, he said. Apart from physical disabilities, he said, people with this birth defect go through a lot of psychological and social problems which are more severe in cases of girls. About the causes of this deformity, he said that genetic factors were thought to play an important role. He said genetic influence was more common in cleft lip/palate combined, then in cleft lip or cleft palate alone. “The risk of a cleft lip or palate is increased if the mother takes alcohol or certain medicines during pregnancy, such as the anticonvulsant or steroids. Other factors include folate deficiency, exposure to radiation and cigarette smoking during pregnancy,” he added. In international studies, he said, clefts were found to be more common in oriental group, medium in caucasians and the lowest in blacks. In Pakistan, there was no study conducted to identify particular groups with this deformity. “However, cleft lip/palate seem more common in males and cleft palate alone seems to be more in females,” he added. In the last three years, he said, a team of doctors and technicians from the Civil Hospital Karachi and the Services Hospital, Lahore, had organised cleft camps in Sukkur, Nausheroferoz, Hyderabad and Tando Adam in different hospitals where 160 operations were conducted free of cost with philanthropists’ support. “The oldest patient treated in the camps was a 52year-old man with bilateral cleft lip,” he added. Dr Ganatra stressed the need for establishment of a cleft centre having all disciplines involved in the management under one roof. Underlining the need to adopt a team approach for complete rehabilitation of cleft patients, Dr Ghulam Qadir Fayyaz from the Services Hospital, Lahore, said cleft surgery needed multidisciplinary management which might involve assistance of pediatrician, ENT surgeon, maxillo-facial surgeon, orthodontist, speech therapist and psychologist. “Unfortunately, there is no concept of this strategy in Pakistan,” he said. Dow varsity vice-chancellor Dr Masood Hameed Khan said the country had an excellent pool of doctors and there was a dire need that they should make combined efforts to transfer their skills to junior doctors. Training workshops, he said, should be held every three months to bridge the gaps in professional development. Medical Superintendent Dr Kaleem Butt also addressed the participants of the workshop. Five medical and health experts will give lectures and training to 73 postgraduate doctors and consultants during the three-day workshop. (By Faiza Ilyas, Dawn-18, 23/05/2007) ‘More surgeons needed for cleft lips and palate patients’ There is a great need to increase the number of plastic surgeons as the number of children born with cleft lips or palates in the country is increasing. This was stated by the Vice Chancellor of Dow University of Health Sciences (DUHS), Professor Masood Hameed Khan at the inaugural ceremony of the three-day workshop on recent trend in cleft lip and palate management. This workshop has been organised with the cooperation of Plastic Surgery Department (PSD) and Professional Development Centre of Dow University. He said that establishing of Professional Development Centre at the university is to increase the number of experts in the medical field. For this purpose seminars and workshops are held under the umbrella of the centre where the medical students, postgraduates, nurses and technical persons are trained. Khan assured that DUHS will extend its fullest cooperation to train surgeons and doctors. He also announced that in the second week of June the classes of Dr Ishrat-ul-Ibad Institute of Oral Health Sciences will commence. Medical Superintendent (MS) of Civil Hospital, Dr Kaleem Butt in his speech said that city’s public sector hospitals have most of the expert doctors and surgeons. Moreover, 110,000 patients get treatment at the Out Patient Departement (OPD) of Civil Hospital annually. He said that the patients with cleft lips and palates are provided free treatment at the hospital whereas private hospitals charge Rs60,000 to Rs80,000 in this regard. The head of department of plastic surgery of Civil Hospital, Ashraf Ganatra said that main reasons behind the children born with cleft lips and palate are environment and genetics. “Beside cousin marriages, unnecessary use of medicines during pregnancy and deficiency of Folic Acid in the body are the other reasons,” he said. 89 Ganatra rejecting the misconception attached to the disease said that lunar and solar eclipse has no involvement in developing cleft lips and palates. He said that Pakistan ranked fourth in the world regarding children born with clef-lips. However, these children can be cured through plastic surgery and they can lead a normal life. He added that free plastic surgeries will be performed on patients with cleft-lips and palate on May 23 to 24 in the Plastic Surgery Department of CHK. (The News-19, 23/05/2007) City hospitals short of ventilators, says PMA KARACHI, May 23: There are only 150 ventilators in government and private hospitals in the city, according to healthcare experts, who said that Karachi, with a population of around 18 million people, requires a minimum of 2,000 to 2,500 ventilators. A medical ventilator is a device designed to provide mechanical ventilation to a patient. Ventilators are chiefly used in intensive care units, home care, and in emergencies. A dire need for ventilators was felt during the May 12 violence in Karachi, when hundreds of people were rushed to hospitals for medical treatment.“Patients with an emergency need to be put on a ventilator at least for 24-48 hours,” Dr Qaiser Sajjad, PMA Karachi General Secretary, told PPI. He said that only because of a shortage of these machines some causalities occurred, which otherwise could have been avoided. The situation is particularly serious for newborns with respiratory complications. Paediatricians believe that prolonged labour or delayed delivery affects the respiratory centre in the brain and the infant can’t breathe normally. Such a baby should immediately be put on a ventilator. However, owing to the limited number or even lack of ventilators in many hospitals, these infants’ lives are in danger. Some hospitals claiming to have the facility reportedly charge patients without actually using the ventilator, while some others which have ventilators lack the back-up support, said Dr Sajjad. This is more common in public sector institutions where ventilators are often out of order due to a lack of maintenance, and the lack of required support such as oxygen supplies and monitoring equipment, including cardiac monitors. A dearth of trained staff, technicians and doctors to operate ventilators is also a major issue in the ICUs of hospitals. Although 10 new ventilators have been placed in Abbasi Shaheed Hospital, more are needed as the hospital caters to the needs of a large population. The number of ventilators in Civil Hospital and JPMC is also very little as compared to the number of patients. (Dawn-18, 24/05/2007) Kidney trade: hospital owners, doctors held LAHORE, May 25: Police on Friday detained two owners of private hospitals and some doctors in Lahore for their alleged involvement in illegal kidney trade, besides ‘recovering’ 10 victims (donors). Though a senior police officer has shown reluctance to divulge their names saying that it will be premature to do so without carrying out thorough investigation, sources privy to the investigation say that managements of Masood Hospital at Kalma Chowk, Rashid Hospital in Garden Town and Shafi Hospital in Iqbal Town have been accused of running the heinous business. Capital City Police Officer Malik Iqbal told Dawn that on a tip off a police team raided a house in Liaquatabad and recovered 10 people who were detained there for the purpose (removal of their kidneys). Two of them had already been operated upon, he said, adding that two people who were guarding them had also been arrested. “We hope that with the help of the arrested guards we will soon reach the perpetrators.” Mr Iqbal said the police had taken the owners of the private hospitals and doctors into custody on the complaints of the victims. “It is a very serious matter and we can't arrest the (accused) doctors formally without solid evidence,” he added. The victims, most of them from Sheikhupura and Nankana districts, told police a man had promised to get them work in Lahore. On their arrival, he along with his accomplices detained them in a house in Liaquatabad. They took two of them to the said hospitals and got removed their kidneys. Earlier, the accused had promised to pay Rs65,000 each of the two ‘unwilling donors’ but they did not give them a penny. The CCPO said that Shekhupura SP (investigation) Zaeem Iqbal had been made an OSD in connection with this trade. The illegal organ trade is on the rise in Punjab. Private hospitals and clinics involved in the removal and transplant of kidneys are making millions daily without any hindrance. The health ministries have so far been expressing their inability to initiate action against unscrupulous elements in the absence of any legal framework. On the other hand, extreme poverty is compelling people to sell their organs. Private hospitals offer between Rs50,000 and Rs100,000 to each donor. Such health facilities charge between Rs250,000 and 600,000 from a recipient for transplantation. They charge up to Rs1 million and above in case the recipient is a foreigner. Such hospitals reportedly do not even have trained staff, proper theatres and latest instruments, which often result in creating post-operation complications in the recipients. No renal status and other diseases of a donor have been investigated before removing his kidney. If a donor is not medically fit, his kidney cannot be removed for transplantation but this fact holds a little importance for the people involved in this business. (By Zulqernain Tahir, Dawn-1, 26/05/2007) 90 NICVD & state of cleanliness I HAVE on several occasions been to the emergency department of NICVD for self and friends and have always been impressed at the streamlined approach to attending the patients. Although the wards are packed, it does not seem ‘rushed’ and the patients are satisfied with the attendant and treatment. Even when you lose a patient, you know that they have done their best for the patient. Some time ago a close friend phoned me about 3am, informing me her husband had a heart attack and was being admitted to NICVD. She asked me to bring our parish priest along to anoint him. I picked up the priest and took him over to the hospital, and was told that our friend was on the 5th floor. I approached the lift operator and told him we had to go up to the 5th floor but he ignored us. However after arguments he took us up. As no private room was available, we got our patient on to the bed which was a bit small and he could not lie completely straight. Anyway the doctor started to examine him. Suddenly the doctor disappeared, so we went looking for him. Across the corridor was the ladies’ ward and a patient had taken a turn for the worse. The doctor was pumping her chest and doing everything else to revive her. This was being watched by us, through the glass window, the patients in the room and several relatives of hers. The reason being there was no curtain to pull around the patient, in fact there were no curtains at any of the beds in both the wards. The poor lady finally died and losing interest we went back to our own patient, where we were horrified to see several cockroaches crawling on him. The cabinet near the bed was filthy so we used a newspaper to line the cabinet. This of course attracts more cockroaches. The doctor asked for some medicine, so the patient’s brother, also a heart patient, had to walk down to the ground floor to buy the medicine and walk back up the stairs as the lift operator refused to bring him up. This was experienced by most of the attendants who had to go down to get medicines. I was taking a turn sitting near our patient’s bed, swatting cockroaches and thoroughly bored, when I noticed the oxygen outlet near his side. Some one was being provided oxygen, I started with shock and glanced at our patient, heaving a sigh of relief when I saw it was not for him. I took a look at the patient on the other side of him, no oxygen there either, losing interest I was thinking of ways to keep myself awake, when someone came in rolling a trolley for one of the patients to have some test done. Suddenly there was a commotion as the trolley had pulled out some tube from another patient. This vetted my interest and I started watching the patient and the attendants right across on the other side of the ward. The oxygen supply had been pulled out and they were replacing it. The mystery had been solved. The oxygen supply at the side of our patient’s bed went across the floor of the ward right down to the other side. When the breakfast trolley came around, this was repeated, as the tube came out again. I can’t understand why there was no supply closer to the said patient. Next afternoon we finally got permission to move our patient to the CCU on the second floor, a cleaner place but the bed a tight squeeze. There should be some way to clean up the wards. The hospital may seek volunteers from the general public to assist them and also ask some industry to donate curtains. Metal rods are in place, just no fabric. Of course, the reluctance of the lift operator to take passengers can mean more business for the hospital. This is just one experience and I pray that no one should have to go through this experience. YVETTE FRANKLIN, Karachi (Dawn-6, 26/05/2007) State-run leprosy hospital a picture of neglect KARACHI: The agony of Gregor Samsa in Franz Kafka’s The Metamorphosis of being rejected by his loved ones for no fault of his own, but due to a deformity that suddenly emerged out of nowhere, touched the hearts of many. The misery of being an outcast is traumatic in itself and is precisely what many lepers, admitted to the only city government-run leprosy hospital in Manghopir, feel. But their despair has multiplied owing to the dilapidated condition of the hospital building and inefficient management. Leprosy is a contagious disease. According to the annual report of the Marie Adelaide Leprosy Centre, there are 700 new cases of the disease found annually in Pakistan. “Furthermore, those infected with the bacteria called Mycobacterium leprae, develop signs and symptoms of the disease in 3 to 40 years. It is transmitted from an infected and untreated patient through droplets (mucus), from the nose and mouth,” says a World Health Organisation (WHO) report. “Once the patients are administered even a single dose of multi-drug therapy (MDT), comprising three medicines -dapsone, rifampin and clofazimine -- there are no chances for the disease to be transmitted or its reoccurrence,” the report adds. Located in a far-flung area of the city, the leprosy hospital was built in 1896 by a philanthropist, Dr B.L. Roy. However, after being run by various NGOs it was handed over to the now defunct Karachi Municipal Corporation in 1960. There is no prize for guessing what happened to the facility afterwards. According to the Medical Superintendent (MS), Dr Mohammad Abbasi, 180 patients are under treatment in this healthcare unit. However, this scribe could see not more than 80 to 100 patients at the time of the visit. Currently there are six doctors working at the hospital, out of which two work in the OPD till 1.30pm. The other doctors visit the hospital occasionally but are basically called when there is an emergency. The same is the case with the nurses and ward boys, (there are only two of each) and although they live on the premises, they too leave at 1.30pm. The statements of the MS about the state of the hospital are quite quizzical. He says that most of the in-house patients have been cured and are staying there as they have no other place to go. He also claims that the majority of the lepers came when MDT was not introduced (before 1985) by the WHO, as earlier the disease was considered incurable. Nonetheless, when this reporter mentioned that a patient had been living there for not more than six years, he had no answer. 91 Thirty-six acres of the hospice’s land have been encroached upon and the administration says that they cannot do much about it. The hospital, which appears quite presentable whenever high-ups of the government have to visit it, in reality has a suffocating environment. Walls in the ward have cracks running through them and paint flakes off due to dampness. When there is an electricity breakdown patients are seen lying on the floor to beat the heat. Bed sheets and pillows are stained and it seems that they haven’t been changed in ages. In addition to this, the patients have to wash their clothes themselves, while they have no access to recreation facilities. Proper medicines are not visible on the bedside table. Instead, one can see cooking utensils as the patients have to cook their own food, as there are no cooks in the hospital. It is simply horrific to even imagine what will happen if any of the patients injures or burns themselves while cooking. But the management seems to be in no particular hurry to appoint cooks. The MS maintains two reasons for this. “The old cooks have retired and the city government has to allow (us) to appoint new ones,” he says, adding that the other reason is that “no one wishes to work among lepers.” The city government has sanctioned 100 employees, but the administration says they only have 80 people working for them. Forty patients are also employed as gardeners, gatekeepers, watchman etc. Though 30 of them draw their salary from the city government, the remainder are paid by some NGOs. It is worth pondering whether these men and women, who have lost parts of their hands and feet to leprosy, can perform the job, for example, of a watchman satisfactorily? A recent incident quite clearly illustrates the pathetic situation. A few men from the nearby colony entered the hospital, as there is no significant boundary wall to stop anyone, and proceeded to beat and rob one of the patients. The watchman tried, to the best of his ability, to stop the intruders but couldn’t do much. Dr Abbasi himself admits that he was helpless to prevent the incident. On one hand the authorities claim they have no money to improve the conditions of the hospital. However, the administration has spent millions on the construction of a molecular laboratory, tuberculosis centre and dental healthcare unit. Then why are funds not being allocated for the uplift of this facility? It is not difficult to understand why these patients are forced to live there. Abandoned by their families, they have no other place to go. Some of the women even have their children with them in the hospital. Male patients voice their concerns about food. It seems that they want to complain about other things as well, but the presence of the MS prevents them from doing so. However, the female patients are more careful in this respect and say that they do not have any complaints. Talking to these patients, one senses an air of melancholy about them. Not being accepted by society they are confined to the hospital, while the attitude of their relatives has shattered them. Thirty-eight-year-old Najibur Rehman has been living in the hospital since he was a young boy. His family found out about him being infected with the disease when he was 9. They tried to have him treated by various hakims and doctors, but it was all in vain. His mother, brother and family visit him once in a while. On the other hand Anwer Hussain says that he hates his family. When asked why, he says that “when I was diagnosed with leprosy, my mother did not come close to me.” He adds that “not even my dad or brothers bothered to come and see me.” He also criticises the hospital administration for not taking care of the patients. All the patients agree when he says that the hospital gives one piece of bread per meal, which is not enough for them. Hailing from Chitral, Mirsawat, 70, sits on the floor of the hospital. He lost half of his foot and both of his eyes due to this bacterium. He doesn’t know what has happened to his family as he has not been in touch with them for ages. In fact, he has also lost track of the time when he first came here. He used to work as a street vendor in a nearby area and when he was diagnosed with leprosy, he moved to the hospital. The situation in the female ward is no different. Bibi Khatoon, 70, sitting on the edge of her bed complains about the poor provision of electricity to the hospital. She reveals that she had to come here as most of her family lives in India. “After my husband died some years ago, I was left with no option,” she says. As she has no children of her own, her brother-in-law’s kids, living in Karachi, visit her. She very innocently says that her nieces and nephews do love her, “but they never take me home and therefore, I no longer insist.” Sara, 30, had to leave her infant girl in Afghanistan seven years ago. She still remembers how her daughter looked like then. She says that the clothes she and the others wear are donated by charities. She thinks it is best for her to stay in the hospital so as to not infect any others with the disease. It seems extremely unfair for these patients to suffer further due to the incompetence and neglect of the hospital staff. The city government should try to improve the living standard of these people. If they are cured, they should be shifted to a place where they can settle down and rejoin the fabric of society. (By Meera Jamal, Dawn-17, 26/05/2007) Ice manufactured under unhygienic conditions The Civil Hospital Karachi (CHK) has not reported any new cases of gastroenteritis up till now, but doctors do fear an upsurge in cases in the coming summer months. Dr Samiullah a junior doctor at the CHK, echoes his concerns, which have also been corroborated by other senior doctors, when he states that, “the main cause of gastroenteritis is the consumption of contaminated drinking water.” In fact, he says, not only does contaminated drinking water cause gastroenteritis, it can also cause several other diseases such as typhoid, diarrhea, hepatitis etc. However, contaminated drinking water is not the only source of water-borne diseases in Karachi, as ice too, sold in the market and consumed by the public is a major source of contamination, especially due to the unhygienic conditions under which this ice is manufactured, stored and transported. According to Abdul Razzak, who owns a shop in a slum area of Patel Para, ice factories are concentrated in three main areas namely: Korangi, Banaras, and Jamshed Road, where several ice factories are situated. Being a retailer, Razzak, 92 purchases his ice blocks from all three areas, and stores it in a room with a low ceiling; this room is built of thick walls and is insulated with a layer of wood. Here, the blocks of ice can be stored for 20 to 22 hours before it starts to melt. According to the All Karachi National Ice Dealers Association, the wholesale rate is fixed at Rs104 per kilogramme, and the retail price is Rs120. The ice is mainly used for commercial purposes; it is used in storage facilities where meat, cold drinks, milk and other perishable items are stored. In the blistering summer months, many people consume this ice with spurious cold drinks sold on pushcarts all over the city. The problem is that this ice is manufactured without treating the water first. According to Haji Mohammad Yusuf Paracha, a manufacturer, and the owner of Lasbela Ice and Cold Storage, the water is supplied by Karachi Water and Sewerage Board (KWSB) and is ordinary tap water. Due to scarcity of drinking water he uses water bored out from the ground, which is saline and brackish, for manufacturing his ice blocks. Paracha says that around 160,000 kilogrammes of water is used for producing one block of ice, and Paracha’s factory has the capacity to produce 450 blocks of ice. One block of ice measures 2x1x4 feet in size. It takes upto 48 hours for the water to become a solidly frozen block of ice. Paracha says that the amount of water used to make a block of ice if properly treated would cut into his profits. Therefore, using water treated for contaminants is out of the question. “We really don’t have the means of purifying water in a costeffective way,” he says bluntly. “In Japan, and Europe, however, there is a system of blowing oxygen into water as it is processed into ice. This process makes the water more transparent, and thus makes it look cleaner and clearer.” Another contributing factor is that ice is made in large steel dyes, which too, contributes to the unhygienic process of manufacturing. The water to be frozen is mixed with salt, at a temperature of at least 1160 degrees centigrade, in order to help the ice remain frozen, and not melt easily. Apart from this, chemicals are also used in a layer on the steel dye for insulation purposes. After a time span of a year, however, these steel dyes become laden with rust and salt sediment, and the steel dyes have to be discarded, as the ice produced in these steel dyes makes it salty. Paracha’s factory mainly supplies ice to Karachi’s five star hotels, but not for consumption purposes. Rather, it is used to store perishable items. Much of the ice blocks are sold to Karachi’s fisheries for storage of seafood and to abattoirs. Taking into consideration the unhygienic conditions that ice is prepared under and its various uses and forms of consumption, it is vital that a method be derived by authorities in the interest of public health in collaboration with the ice manufacturers to introduce technology to make water fit for human consumption before it is frozen into ice blocks. (By Xari Jalil, The News-20, 26/05/2007) Fighting Aids PARTICIPANTS in a workshop on Aids held recently in Quetta have stressed the need for creating greater awareness about this incurable disease. Pakistan is lucky in that it has a low prevalence rate of HIV/Aids at the moment. The National Aids Control Programme has registered approximately 800 Aids cases so far. However, the fear is that the actual figure is much higher. For lack of awareness about the disease and poor access to proper clinics and hospitals, many HIV/Aids cases are not diagnosed. Besides, the social stigma attached to the disease (transmitted mainly through sexually aberrant behaviour, the sharing of contaminated needles among drug addicts and their use in hospitals) prevents many patients from reporting their illness. In fact, according to the UN, the number of cases of HIV/Aids in Pakistan could be as high as 85,000. This means that the government cannot afford to be complacent and must take effective steps to reduce the incidence of the disease and put to effective use the sizable aid provided by international donors for the control of Aids in the country. In doing so, the government’s main focus must be on spreading information about Aids. Greater efforts are needed to disseminate information, especially to high-risk groups and school-going children, who must be made to understand that the only way to combat the disease is through prevention. Such an effort to provide information and to encourage a public debate on Aids can only be promoted through proper planning and coordination among various government departments and NGOs. The task, though daunting, would be much easier to do now than later when cultural conservatism, coupled with the government’s negligence, make the problem spiral out of control. Pakistan would then have to pay a heavy price in trying to control Aids. (Dawn-7, 28/05/2007) $35m Norwegian grant for health KARACHI, May 29: Sindh has been selected for a grant of $35 million from the Norwegian government for initiating a fiveyear programme towards the improvement of health status of women, neonates and children in the province, said a source in the health department. A decision pertaining to the grant was reached at a workshop held recently at Islamabad under Norwegian-Pakistan Partnership Initiatives (NPPI) aimed at addressing the millennium development goals relevant to the improvement of mother and child health and reduction of mortality rate by two third of under five children and mothers by 2015. The source said that the provincial health department would submit a logical framework addressing the clause 4 and 5 of MDG in a month or so to the federal government for materialising the foreign fund to be released in five equal instalments in five years. To finalise the modalities in question a Norwegian mission will also visit Sindh soon, the source added. The grant will be in addition to what the federal government had promised to provide for improving the indicators of mother, neonatal and children health (MNCH) in the shape of projects. The federal government’s funding is likely to come in January next, it was further learnt. The Norwegian fund is likely to be utilised in areas which will not be covered through federal funding. Sindh will spend the foreign grant on developing a separate block of monitoring and fortification of patient referral system, besides engaging community workers for strengthening the lady health workers’ networks and basic health units, said another source. As announced about a year back, Rs32 billion national MNCH programme is to be implemented by the federal government over a period of five years for improving the health of mothers and children, the obligations to be met so as to fulfil the MDGs. (Dawn-18, 30/05/2007) 93 World No-Tobacco Day today Ban on smoking at public places not enforced KARACHI, May 30: Like elsewhere across the globe, World No-Tobacco Day will be observed on May 31 in the city where health practitioners will highlight the hazards of tobacco consumption in various programmes planned for the day. It is felt that the government and other stakeholders have been unable to make concerted efforts against the widespread use of tobacco that causes preventable diseases and death in many cases. Though the rules prohibiting smoking at public places, indoor workplace and public buildings, educational institutions and in public transport as well as sale of tobacco to children exist on paper, they remain largely unimplemented. According to a senior doctor at Jinnah Postgraduate Medical Centre, cigarettes and other tobacco products have nothing positive. Today tobacco is considered second major cause of death in the world and half of the regular smokers are at the risk of premature deaths.Equally alarming is the fact that hundreds of thousands of people die each year from diseases caused by passive smoking, says a WHO document. In view of the adverse results of increased public addiction to tobacco, the member states of the World Health Organisation planned a World No-Tobacco Day in 1987 to draw global attention to the tobacco epidemic and preventable deaths. The WHO’s theme for the day is “smoke-free environment” this year. About the diseases caused to smokers or those exposed to smoke, health experts say it is unfortunate that once a person takes up the first pack of cigarette, he is left with no choice, he gradually becomes addicted to nicotine. Pakistan should exercise an effective control on tobacco products in the country, because it is a signatory to the international convention on the prohibition of smoking, they observe. Quoting some international findings, an expert says smoking causes 40 per cent of heart diseases and 90 per cent of lung cancers. He says tobacco companies in Pakistan are given a freehand to promote a powerful addictive substance to the population. According to a study conducted some years back in Karachi, the prevalence of tobacco use was 32.7 per cent. The prevalence of smoking in Karachi has not declined in the past few decades and requires attention of researchers to explore smoking related issues. A research conducted by students of Aga Khan University Hospital says that 62 per cent of high school adolescents included in the survey reported their reasons for smoking as enjoyment, while 18 per cent claimed to have been influenced by advertisements. Majority of them (61.3 per cent) started smoking with their friends. Boys who spent most of their leisure time outside their homes were more prone to smoke cigarettes, adds the research report. A community-based study, undertaken in 2005, about awareness and practices regarding tobacco consumption and passive smoking in Gadap Town says that high proportion of people smoked and other people who lined with them shared the environment as passive smokers. The study shows that only 22 per cent individuals were aware of the adverse effects of passive smoking. A total of 157 subjects were studied of whom 110 (70 per cent) were tobacco consumers. In this group, 42 per cent chew tobacco in betel leaves, 39 per cent smoke cigarettes and 19 per cent hookah. About 89 per cent people started use of tobacco under 20 years of age and the reasons given for adopting this habit were social peer pressure (64.5 per cent), depression (22.7 per cent) and pleasure (12.7 per cent). These statistics and other relevant studies though help chalk out a comprehensive plan to spread awareness among youth regarding adverse effect of smoking, the authorities fail to implement the same in letter and spirit. Chest physicians, pathologists, ENT specialists and members of medical practitioners’ bodies and the civil society forums have long been voicing their concern over the increasing trend of smoking. They stressed the need for discouraging smokers, particularly children and teenagers. The Prohibition of Smoking and Protection of Non-smokers’ Health Ordinance was promulgated in 2002 under which smoking at workplaces or in public transport was banned. The aim was minimising the effects of smoking on non-smokers’ health, but defiance could never be averted as one can see even students smoking in the school and college premises. The executive officer for college education had issued a letter in March 2005 informing the head of institutions of colleges, higher secondary schools and technical education institutions that their institutions had been declared as no-smoking zone. The heads and principals were told that storage, sale, distribution and use of drugs, cigarettes, gutka, supari and any other material or substance considered injurious and hazardous to public health had been prohibited in the government education institutions. Ironically, smoking besides students is common even in the ranks of teaching and non-teaching staff in government institutions. A provincial government’s anti-smoking task force in February 2007 had also resolved that there would be a complete ban on the sale of cigarettes in educational institutions and its surrounding areas. In line with the anti-smoking ordinance, the task force decided that the CCPO and other senior officials would be urged to cooperate in the implementation of the decision. Regarding effectiveness of tools against the ban of smoking at public places and transport, a source in the provincial health department said the task force on curbing smoking was reactivated three and a half months back, but things could not go beyond a meeting involving high-ups from various departments and agencies. (By Mukhtar Alam, Dawn-18, 31/05/2007) Poor healthcare for children ALTHOUGH the mortality rate for children under five years of age has been slowly declining over the years, it is still a cause for concern and is indicative of the deficiencies in the government’s overall policies relating to child health. Currently, the infant (up to one year of age) mortality rate is 80 per 1,000 live births while the figure for the under-five category is 101. This is disappointing, because, as pointed out by speakers at a workshop held in Karachi the other day, a majority of children die from preventable illnesses. Hygiene, proper sanitation, clean drinking water, adequate nutrition and routine immunisations can avert a number of deadly infections that claim thousands of infants every year. However, these remain 94 unavailable to large sections of the population who live far away from medical centres and whose poverty and ignorance about disease is largely responsible for their offspring dying young. The male bias in society also has a role to play in this, for families prefer to concentrate on the health of their sons often at the cost of their daughters. Many of these shortcomings could be rectified if the government attached greater priority to the welfare of the young population. Health, like education and all other sectors affecting children, has been denied the required priority, and improvement will be slow as long as the government does not revamp existing medical centres and build new ones throughout the country, besides increasing the number of doctors and nurses there. Moreover, regular programmes on educating mothers about the basics of hygienic living and routine vaccinations should be conducted in remote villages where the situation is particularly grim. Malnutrition and disease can only be contained through preventive and curative measures and the political will to deliver on the various promises made on children’s health from time to time. (Dawn-7, 31/05/2007) JUNE World No-Tobacco Day Demand for enforcement of law against smoking KARACHI, May 31: Speakers at seminars and meetings on ‘World No-Tobacco Day’ observed on Thursday said that tobacco even in small doses was harmful and there was a need to motivate public against its consumption. They also expressed concern over the increase in the trend of smoking among adolescents and women and clarified that tobacco was wrongly related to heroism, body strength, creativity and smartness. Speakers at a seminar organised by the Aga Khan University Hospital (AKUH) demanded for strict enforcement of the Prohibition of Smoking and Protection of Non-smoker Ordinance, 2002. They said that smoking was the single largest preventable cause of deaths in Pakistan. Some details from the US Surgeon General’s report were also referred to during the seminar. According to the report, the environmental tobacco smoke had been found to cause premature death and disease in children and non-smoking adults. Prof Dr Javaid Khan, head of AKUH pulmonary section and also president of Pakistan Chest Society, Sindh, said that some of the multinational tobacco firms were openly flouting the Pakistani ordinance on smoking in defiance of Supreme Court’s directives and used “all possible means to make the Pakistani public addicted to tobacco”. Dr Khan said that smoking caused over 90 per cent chronic obstructive lung disease cases, whose treatment was very difficult, with most patients ending up with respiratory failure. Dr Nadeem Rizvi, head of chest diseases department at the JPMC, said that as a result of aggressive marketing, “an estimated 1,500 children were taking up smoking everyday, in Pakistan.” He urged pro-active measures by city governments in terms of removing tobacco-related signboards from shops and for a youth education campaign in educational institutions and called for a sponsorship ban on sporting and other events. Dr Suleman Haque of the AKUH dismissed the notion of countering stress through smoking. A surgeon at the AKUH, Dr Shehzad Ghaffar, reported on tobacco use in the form of ‘gutka’ and ‘pan masala’ and warned that there was an increasing trend amongst children. He said that Pakistan currently topped the list in the incidence of oral cancer. Senior nurse at the AKUH, Humaira Waheed, suggested making all public places and public transport smoke-free by strict enforcement of the Anti-tobacco Ordinance. A scholar, Engineer Naveed Ahmad, reiterated scientific confirmation on the serious harm to passive smokers through release of toxins from smoking. Dr Aamir Hameed said that sheer will-power, modern medication and counselling could enable most patients to kick the habit of smoking altogether. A video demonstrated that tobacco was the first step towards other addictions and must be controlled at all costs. Meanwhile, Dr Abdul Wahid Bhurt, WHO Operation Officer in Sindh, in a communication said that World No-Tobacco Day was observed annually on May 31 to highlight hazardous effects of tobacco smoking and to remind and help colleagues around the world for taking effective legislative and executive measures against it in order to safeguard health and happiness. “There is no safe level of exposure of tobacco smoking. Active smokers as well as passive smokers (apparently non-smokers) are becoming victims of dangerous diseases of lung, including cancer, tuberculosis, heart and others, including obesity, diabetes, liver and GIT diseases. “In addition to it, we are wasting millions and billions of rupees on purchase of tobacco products and minimising already limited resources that can be better utilised for improving health, education and other aspects of life”, he added. Referring to the theme of this year, ‘smoke-free environment’; a senior doctor at the Civil Hospital Karachi said that policy makers and the public should be informed about the adverse effects of exposures to second hand smoking. He also laid emphasis on a consistent communication campaign about health rights and elimination of tobacco smoke, a toxin air contaminant. Finding no significant development against tobacco on ground, the Pakistan Medical Association, Karachi, said that the prohibition of smoking ordinance could not be implemented so far in true sense due to lack of interest on the part of government functionaries. 95 More than 100,000 people died every year in the country only due to cigarette smoking. They suffer from carcinoma of oral cavity, tongue, lungs, larynx, blood pressure, heart diseases, oesophagus, stomach, pancreas, kidney etc, the association added in a statement. It also referred to Sheesha smoking offered in different restaurants and demanded a ban on this bad habit. The PMA also appealed to the general public to make their homes and offices smoke free. A survey aimed at knowing the attitude of Karachi-based medical students towards smoking revealed that incidence of smoking was greater among male students (17 per cent) than females (4 per cent). The average age of initiation of smoking was 17 years and the major influence was friends. (Dawn-18, 01/06/2007) Hazards of smoking SMOKING — both inhaling directly and breathing in exhaled smoke — is injurious to health but the government is doing precious little to drive home the point. There could be many reasons for this. The authorities may simply lack the will to enforce anti-smoking rules or are reluctant to lose the billions of rupees earned from the sale of cigarettes. Whatever the case, one thing is clear: at least 100,000 people die of tobacco-related causes in the country every year while the consumption of this lethal substance is on the rise. Even children are increasingly among the smokers. According to doctors, more than 1,000 children between the ages of six to 15 years take up the habit every year, indicating that shopkeepers continue to flout the 2002 ban on the sale of cigarettes to anyone below 18 years. As a result, smoking has become a common sight in schools. This factor is worrying, for unless the young population is educated on the health hazards of smoking, how can it be expected to refrain from the habit? How can it learn not to associate smoking with the world of glamour since that is what has been projected all along? And most importantly, how can it be taught to respect the preferences of non-smokers who, because of the government’s failure to crack down on those smoking in public places, are forced to breathe in carcinogenic fumes? Each year on World No-Tobacco Day, top doctors in the country and international organisations come out with alarming statistics on smoking while reiterating all the hazards of this habit. But such an exercise becomes meaningless unless there is follow-up action to ensure that laws already in place are being observed strictly and awareness is being enhanced. On both counts, Pakistan has put up a disappointing performance so far. (Dawn-7, 01/06/2007) Global drug menace THE production and trafficking of heroin and cocaine have assumed the dimensions of a global problem and figure in the list of major challenges requiring the participation of all governments. As nearly 90 per cent of the world’s opium, the source of heroin, is produced in Afghanistan, there is considerable smuggling through the tribal areas of Pakistan. We are, therefore, prominent among the list of countries that need to give special attention to this problem. Since the instability and conflict in Afghanistan started in 1979, when even the CIA encouraged opium cultivation during the Soviet occupation of the country, Pakistan has suffered from the culture of drugs and Kalashnikovs. Today, some of Pakistan’s major problems can be traced to this scourge. The country is awash with illegal weapons that have contributed to crime, political violence and terrorism. As for drugs there are an estimated four million drug addicts. Half a million are addicted to heroin. Drug addiction, apart from ruining the lives of addicts and that of their families, is also a source of crime and contributes to poverty and backwardness. Those affected need care and attention, though in many cases, they become outcasts and end up dying miserable deaths. During British times, there were licenced sellers of opium, and addiction did not generate crime or violent tendencies. The introduction of hard drugs, such as heroin derived from opium and cocaine that is made from the coca plant, found mainly in South America, is a more recent phenomenon, and is linked to the spread of prosperity in industrial societies in Europe and North America. With affluent youth discovering the thrill and elation of hard drugs the habit has spread and demand has led to production of crops from which these substances, i.e. heroin and cocaine, can be made with the help of certain chemicals. The post Second World War period during which industrial societies became enormously wealthy saw a phenomenal increase in demand, matched by supply mostly from backward countries. In Asia, opium was grown in the Golden Triangle in Southeast Asia and parts of Southwest and Central Asia. The price paid at the consumer end was over a thousand times higher than at the source, and drug money provided a short-cut to wealth, not so much for the growers as for middlemen, transporters and sellers. As both the production and consumption of drugs grew, the UN became involved and the matter was entrusted to the Economic and Social Council (Ecosoc), which established a UN Drug Control Programme (UNDCP). An International Narcotics Control Board was also set up to coordinate the operations of narcotics control authorities in various countries. In Pakistan, a Narcotics Control Board was set up as a part of the police. Later, a separate ministry was set up to deal with the problem. The Narcotics Control Board was succeeded in 1994 by the Anti-Narcotics Force which has a working relationship with 27 other countries where narcotics are a major source of concern. Pakistan’s drug problems relate mainly to Afghanistan. As that country has experienced internal turmoil, external military intervention and widespread civilian suffering over the past three decades, poppy cultivation has taken root in anarchic conditions. Through active collaboration between the UN and Pakistani authorities, poppy production (concentrated in the NWFP) went down from 800 metric tons in 1979 to 10 metric tons in 2000. However, as we have a 2,500km long border with landlocked Afghanistan, there has been considerable smuggling of heroin with Pakistan providing the shortest transit route to the sea. The quick wealth generated by drug trafficking has created a drug mafia. Between 1976 and 1989, life in Pakistan became complicated as criminals became billionaires and sought to join the power elite. Apart from trafficking, the drug mafia encouraged drug addiction within the country. 96 The Taliban government in Afghanistan successfully banned poppy cultivation between 1996 and 2001 but after 9/11 and the consequent military occupation of the country by the US-led coalition, the former warlords rose to power again and were joined by others. Total poppy production is currently estimated to be 6,100 tons that amounts to 92 per cent of the world production. Though the heroin produced is going abroad through many routes, including Iran, Central Asia and the Middle East, 40 per cent transits through Pakistan. Unfortunately, the so-called democratic reforms in Afghanistan since 9/11 have enabled the warlords to dominate certain areas and to enrich themselves by resuming poppy production. Though the foreign forces and UN agencies make serious efforts to discourage this trend, their writ does not prevail much beyond Kabul and a few other cities. There is so much poverty and deprivation in the absence of reconstruction in the war-ravaged country that poppy cultivation has spread to practically all the provinces. The international community has pledged billions of dollars for the rehabilitation of the devastated country, but the occupation forces have concentrated on the use of force and done very little to provide shelter, employment and other amenities either to the returning refugees or the local residents who are among the poorest people anywhere. Coming to the other hard drug, the main growers of the coca plant are to be found in some countries, including Colombia, in the north of Latin America that share one characteristic: the huge gap between a small number of wealthy people and the mass of the common people who can barely eke out a living. The social and political turmoil is exploited by the drug mafia. Though the US extends liberal assistance to the central government and has even stationed some troops to back the government forces, several billion dollars worth of cocaine enters the US every year. The growing, transporting and sale of drugs is now recognised as major crimes in many countries among which some like Saudi Arabia, Malaysia and Singapore have imposed the death penalty. In the affluent and sophisticated countries of Europe, many make allowances for drug addicts, such as the Netherlands, Denmark and Germany. In the US, hospitals allow the provision of narcotics to addicts. This liberal approach towards drugs brings to mind the concept of same sex marriages. Since drug addiction flourishes in societies with wide gaps between the rich and the poor a twin approach is needed. On the preventive side it is essential to treat drug production and trafficking as major crimes. However, the long-term solution lies in addressing the problem of economic deprivation and poverty affecting developing countries. Both the political causes and the economic roots need to be tackled. (By Maqbool Ahmed Bhatty, Dawn-7, 04/06/2007) Misconceptions about hepatitis rejected KARACHI, June 3: Misconceptions about hepatitis are as damaging as the disease itself. While there is a dire need for doctors to educate themselves about the disease and adopt safe medical practices, the government must also fulfil its responsibility by creating awareness and regulating blood screening practices. This was stated by speakers at a public awareness programme organised by the Pakistan Medical Association in collaboration with the Pakistan Society of Gastroenterologists on World Hepatitis Day at the PMA House on Saturday. Giving a presentation on hepatitis C, Dr Saad Khalid Niaz, consultant gastroenterologist and hepatologist, said that hepatitis had become a major problem in this part of the world and the public’s miseries were being compounded by the hazardous practices of quacks, openly doing business in every part of the city. In this situation, he said, it’s all the more necessary for the public to have the basic information about the various forms of hepatitis, their treatment and diagnosis so they can seek the right treatment. “There are about seven to nine million hepatitis carriers in the country. Most of them don’t know they have the disease and that they are a risk for themselves as well as for others. Hepatitis C is a slow, progressive disease and can take from 10 to 40 years to affect the liver. It can damage the liver, but the damage can range from minimal to liver failure,” he said. About the misconceptions about hepatitis C, he said the disease does not spread by physical contact like touching and hugging etc., or through using the bed sheets, towels, plates, cutlery etc., of an infected person. There is no harm in maintaining a conjugal relationship, but those with more than one partner are at risk. Breast-feeding is safe and should be encouraged and treatment should be started after the mother stops nursing the baby, he added. People who are at risk include those who have received blood transfusions, especially before regular blood screening for hepatitis C was started in the mid-90s. Patients on haemodialysis, medical professionals and anybody who uses nonsterile/reused injections, especially drug addicts, are also at risk. Only 20 per cent of hepatitis patients get serious liver disease. Also, there are no dietary restrictions, except for those with very severe and complicated liver disease, he said. He dispelled the impression that liver biopsy causes the spread of the virus and said that it’s necessary, since it is the only way to know the severity of the disease. In diagnosis, ultrasound is reliable only when the disease is at an advanced stage and to pick up complications. “Not everybody needs treatment or is suitable for treatment. The only scientifically proven treatment of any benefit for eradicating the hepatitis C virus is an injection, Interferon, which is taken with tablets (Ribavirin). It can cure 60 to 80 per cent of patients. Treatment for the majority of patients in our country is for 6 months but can be for one year,” he said. He also urged the government to play an active role in ensuring safer blood screening practices, while asking doctors to avoid blood transfusions if possible and the unnecessary use of injections. “If needed, use only properly screened blood and disposable syringes,” he said. Dr Badar Faiyaz Zuberi, gastroenterologist and hepatologist, Dow University of Health Sciences, gave his presentation on hepatitis B. He said that the disease is preventable through vaccination and there are no side-effects of it. The acute case fatality rate from hepatitis B is 0.5 to 1 per cent, while the premature mortality rate from chronic liver disease is 15 to 20 per cent. Nine out of 10 adults naturally get rid of the hepatitis B virus in their bodies after a few months. Up to 9 out of 10 babies born to infected mothers will end up being hepatitis B carriers for the rest of their lives if they do not get the shots. Nineteen out of 20 babies who get the shots will be protected for life. Dr Hasnain Shah, Dr Abdul Rauf Memon and Dr Abu Talib, took part in the panel discussion. (Dawn-14, 04/06/2007) 97 Smoking law An anti-smoking law is in existence in Pakistan. The country is a signatory to the WHO Framework Convention on Tobacco Control, and ratified it in July 2003. But from the increasing number of smokers, the legislation is mostly confined to the statute books and doesn’t extend to streets, public transport, workplaces and homes. Thursday was World No-Tobacco Day and this year’s slogan for the event sponsored by the World Health Organisation was “Fight the Tobacco Epidemic”. Pakistan has hardly put up a fight against the menace which is killing or affecting scores of millions around the world. There have been some successes in this fight in Pakistan, though not as a direct result of the law. Our airline flights are now free of the weed, for example. More important, cigarette ads have nearly vanished from Pakistani newspapers and magazines and from radio and television, all of which were a big boost to the hazard despite the feeble warnings accompanying the advertisements. There has been another refreshing change in recent years: More and more private companies are making their buildings entirely or mostly no-smoking. On the other hand, however, the practice is sharply increasing among young people, especially young urban women. This last group has become a particular target of western tobacco companies in their dumping tactics in the Third World, their getting increasingly unpopular in the developed countries. Smoking was always trendy with young people, a false sign of independence and maturity. The unfortunate recent phenomenon is its becoming a symbol of gender equality among educated Third World woman. The habit goes unchallenged among the less educated and illiterate, as well as among teenagers and minors. The sale of cigarettes to children under 18 is banned under the law, which also prohibits the sale and storage of tobacco within 50 metres of educational institutions – a cynical joke when the prescribed restrictions are compared with the actual situation. Stopping cigarette advertisements is certainly good, but it’s only half the battle. The need is for an effective, sustained advertising against smoking, with the ads clearly specifying all its harms. In Pakistan few people know about the injurious effects of passive smoking. This aspect alone could persuade many smokers to stop, because of the ill effects their habit could have on their families. But the bottom line is for the government to enforce the law. It must fight the tobacco epidemic in earnest, not merely mark no-smoking days every year. The fact that not a single violator has been punished in these four years is proof that the legislation is just there. (The News-7, 04/06/2007) How safe are our vaccines? A Canadian aid agency Friday last pledged $1.2 million (about Rs62m) grant for eradication of polio in Pakistan which had already contributed $3.5 million to our polio eradication campaign. But two recent events have raised a big question mark about the safety of vaccines being administered to infants and children across the country. A week ago, the Pakistan Medical Association and the Saarc Medical Association had asked the health ministry to withdraw from the market a stock of Hepatitis B vaccine manufactured in a country in the Far East which is said to have claimed many lives in Bangladesh, Vietnam, Philippines and Russia. An outright denial by the ministry the next day that any such suspect batch of Hepatitis B vaccine had been supplied to Pakistan, was hardly any consolation to the public. Just before this incident, the safety of the polio vaccine was questioned in the Peshawar High Court where a member of the public had filed a writ petition claiming that polio drops contained substances that weakened the reproductive system besides causing some other diseases. Although the Peshawar High Court had dismissed the petition — based on technical reports on polio drop samples conducted by a hitherto unheard of local facility called the National Control Laboratory — and ruled in favour of continuation of the polio vaccination drive in the country, the case has nevertheless drawn attention to the existence of anti-vaccination movements in other countries like Nigeria and even in the US itself, where there has been longstanding concern about the safety of polio and other vaccines being administered to American infants and children. In Pakistan, objections to the polio vaccine — that they contain substances that could cause sterility — have usually been portrayed as the paranoia of some religious clerics who believe that WHO’s polio eradication programme is a plot by westerners to depopulate Pakistan. However, Pakistani clerics are apparently not the only ones who harbour this conspiracy theory. As was told to the Peshawar High Court, an anti-polio campaign in Nigeria, the most populous country in Africa, had resulted in a boycott of the vaccination in 2003 which reportedly resumed many months later only after WHO apparently agreed to the condition that the polio vaccine administered in Nigeria would be manufactured in Indonesia and nowhere else. Other countries where WHO’s vaccines have reportedly also been found suspect are Mexico, Nicaragua and the Philippines. In these countries, tetanus vaccines were alleged to contain substances that could cause miscarriage and sterilisation. There are countless books, reports and websites that purport to document the intentional (as well as nonintentional) contamination of vaccines with disease-causing viruses and the alleged relation of these vaccines to diseases like AIDS and cancer. Conspiracy theories aside, it is an established fact that serious concern about the safety of vaccines, particularly about the presence of thimerosal (a mercury-based preservative used in vaccines), exist in the US itself, where anti-vaccination organisations have been trying to educate and inform the public about the risks associated with vaccinations. While adverse reactions to vaccines in general has been a concern in the US since the 1980s, the dangers of mercury poisoning from vaccines was first raised in the US Congress in 1999 when an investigation was initiated into this problem. Countless studies and reports have emerged in the US about the presence of toxic substances like mercury (a neurotoxin), formaldehyde (a known carcinogen) and aluminium in vaccines like polio, Hepatitis B, DPT and MMR. These toxic substances have been linked to sharply rising incidences of autism (a neurological disorder) in American children as well as other diseases including Sudden Infant Death Syndrome, allergies/asthma, leukemia (especially leukemia in infants and children), lymphoma, cancer, tumours and other diseases. Eventually in 2003, the US Congress investigation report specifically identified thimerosal in childhood vaccines as the cause for the huge jump in the cases of autism and other related neurodevelopmental disorders in the US, where some 30 over childhood vaccinations are mandatory, most of them made mandatory during the 1980s. 98 The result of this campaign on the safety of vaccines is that today vaccines in the US are supposed to contain no trace of thimerosal. Besides, oral (live) form of the polio vaccine (OPV), which some studies found to be directly responsible for the majority of new polio cases in the US as well as the major increase in childhood leukemia, was removed from the US market in January 2000, it being replaced by the inactivated and killed polio virus vaccine (IPV). Said to be a less potent vaccine than OPV and a very costly injection, IPV apparently does not contain thimerosal. As for the Hepatitis B vaccine, it was recommended for newborns in the US in the second half of the 1990s and made mandatory in 2000 for infants aged two months, but concern has been raised about the thousands of averse reactions to the vaccine with hundreds of deaths which have been reported in the country since the vaccine was made mandatory (figures which some claim are only the tip of the iceberg). Why are vaccines being introduced in the US one after the other when the risks apparently far outweigh the benefits? Why are the defects in the vaccines and their adverse reactions not usually reported well in time? Some writers have termed this phenomenon a corrupt public policy stemming from financial conflict of interests and scientific fraud involving the drug manufacturers, the disease control centres as well as the food and drug authorities. The question that we in Pakistan should ask is: Are the vaccines being supplied to Pakistan and being administered to our infants and children free from anti-fertility substances as well as from toxic substances (like mercury) and unwanted contaminant viruses (like SV40) that cause cancer, HIV, etc.? Also, why are we and many other developing countries still being given the apparently less safe OPV when this form, which is capable of causing, though rarely, paralytic polio, has already been removed from the market in the US? (The official argument being given for continuation of OPV in developing countries like Pakistan is its low cost, ease of administration and superior capacity to provide the population immunity.) As for the Hepatitis B vaccine in Pakistan, although our ministry of health has claimed that they are not suspect, organizations like the PMA and the SMA have a moral and ethical duty to continue to pursue this case to ensure that the Hepatitis B vaccines, as well as all other vaccines, supplied to us are really safe for the public. While vaccinations have certainly saved many Pakistanis from the sufferings of several diseases like smallpox and polio, a key part of our vaccination programme should be to do everything possible to ensure that the vaccines are as safe as possible and that adverse reactions are fully disclosed. The total number of confirmed polio cases in Pakistan dropped from thousands in the 1980s to 558 in 1999, 98 in 2002, 40 in 2006 and eight so far this year, but do we know for sure that these handful of new polio cases have not contracted polio from the polio vaccination itself? Have we ever studied the possible correlation of this vaccine with rising infant and childhood diseases, like for instance lymphoma, leukemia and other forms of cancer or with infertility problems? Whether or not drug manufacturers and promoters of vaccines like WHO and other foreign aid agencies have a hidden or secret agenda, on our part we should build up our capacity to conduct tests that would reveal whether the vaccines supplied to us contain unwanted contaminants. Our scientists and researchers can also be encouraged to engage in studies to find out whether these vaccines cause other diseases. (By Aileen Qaiser, Dawn-2, 05/06/2007) 800 community-based midwives to be trained KARACHI, June 6: Sindh Health Minister Syed Sardar Ahmed has approved a training programme for 800 communitybased midwives under the Maternal, New Born and Child Health Programme of the provincial health department. In a meeting held on Wednesday, it was decided that advertisements inviting applications for the proposed training would be published in all major newspapers in July. The health minister said the department was taking a number of steps aimed at improving the health status of the masses. He said the training programme for community-based midwives was meant to improve maternal and infant health standards and life quality. Sindh Mother and Child Care Project Director Dr Sahab Jan said the Maternal, New Born and Child Health Programme was being funded by the governments of Pakistan and Norway. She said the federal government would provide Rs3.246 million and the Norwegian government would offer 37 million dollars. Dr Sahab Jan said Rs1.937 billion funds were being given for emergency obstetric and neo-natal; Rs0.840 million for community-based midwifery training; Rs0.030 million under the head of family planning; Rs0.016 million for nursing examination board; Rs0.128 million for printing and advocacy; Rs0.154 million for contingency and Rs0.159 million for other related utilities. The minister was informed that the funds to be provided by Norwegian government would be in accordance with the “Need Base Assessment”. A committee, headed by Special Secretary for Public Health Dr Abdul Majid, would put forward recommendations. The committee comprising Prof Sadqa Jaffery, Prof Zulfiqar Bhutta, Dr Shershah Syed, Prof Iqbal Memon, Dr Sahab Jan, Dr Khalid Shaikh and Dr Shakeel Malik was said to be in the process of finalising their recommendations. Sindh Health Minister Syed Sardar Ahmed directed the special secretary for health to ensure provision of estimated expenditure on an yearly basis so that the money was arranged for the required year before hand preventing any delay or difficulty in sustenance. (Dawn-18, 07/06/2007) Lack of burn units THERE is an urgent need to build burn units at hospitals in Karachi especially since the city has only two (one at the Civil Hospital and the other for children at NICH). This was stressed at an on-going conference on the subject on Tuesday where participants said that because of an increase in industrial units and chemical warehouses, as well as an increase in buildings without adequate security systems for fire control, chances of people getting burned had also increased. There is also a rise in number of cases of domestic violence against women, particularly the horrific crime of throwing acid on them which heavily disfigures their faces and requires extensive care. In view of all this, it is depressing that there are only two 99 places to go in the city to get treatment for burns. What makes it worse is that there have been demands from the medical community for building burns units across the country. Five years ago we noted that despite making funds available for burn units across the country, there was no progress and it seems nothing has changed since then. Where have those funds gone, especially those donated by foreign countries specifically for setting up burn units? The health ministry must look into this and expedite matters, if it has not done it already, or do whatever is needed to set up the required units and make them functional. Too many people succumb to burn-related injuries many which are avoidable if adequate burn care was available. The government’s negligence in this regard is deplorable and must be rectified. At the same time, it is imperative that doctors in all hospitals are trained to deal with burn cases as not everyone can go to specific burn treatment facilities, especially when only two exist in Karachi. (Dawn-7, 07/06/2007) Nurses and the mullah in Lahore The Jinnah Hospital administration and School of Nursing decided Tuesday to make their nurses attend Islamic classes that will keep them “pure and clean”, and help develop in them a sense of “love and care” for patients. But if the nurses thought this was coming free they were mistaken. A sum of Rs 300 will be deducted from the salaries of the nurses to pay the man of God. The administration is convinced that this price for the achievement of spirituality is a just price. Nursing is tough profession. It is tough because it goes against the cleric-dominated tenet that woman should not been seen in places where men roam around. Unfortunately, men are poor nurses and hospitals can’t do without female nurses. But nurses are poorly paid and are in the profession because of economic compulsion. The cruel irony in the latest case is that some unthinking administrator is ready to deliver the poor creatures into the hands of the very entity that damns them. The administrator is a very ordinary male who erroneously wants to tackle problems of discipline through religiosity. He should be seriously advised against it. (Daily Times-A6, 07/06/2007) One doctor for 1,254 patients ISLAMABAD: Pakistan's public health sector confronts considerable scantiness, as there is one doctor for 1,254 persons, one dentist for 20,839 people and one nurse for 2,671 patients, yet the government is spending a meagre 0.57 percent of the GDP (or Rs50 billion) on health sector. There is one midwife for 6,235 and one Lady Health Visitor for 18,318 patients, according to the Economic Survey 2006-07 released here on Friday. Although the ratio between available health facilities and the population has recorded a slight improvement over last year and the number of doctors has increased, yet it is minimal to provide health coverage compared to the population growth. In 2006-07, health sector allocations increased by $50 billion from $40 billion in the corresponding year. In 2006, there 122,798 MBBS doctors, 7,388 dentists, 57,664 nurses, 24,692 midwives, 8,405 LHVs while in 2005, there were 118,062 doctors, 6,734 dentists, 51,270 nurses, 23,897 midwives, and 7,037 LHVs. Pakistan is still lagging behind compared to other Asian countries such as China, Thailand, Indonesia, India, Sri Lanka and Bangladesh in terms of the human welfare indicators. Among these countries, Pakistan depicts a grim picture regarding health facilities. Mortality rate under five year per thousand in Pakistan is highest 101, compared to India 85, Bangladesh 77, Nepal 76, Sri Lanka 14, China 31, Thailand 21, Philippines 34, Malaysia 12 and Indonesia 38 per 1000. Infant mortality rate is also highest in Pakistan at 70 per 1,000 which is 62 in India, Bangladesh 56, Nepal 59, Sri Lanka 12, China 26, Thailand 18, Philippines 26, Malaysia 10 and Indonesia 30 per thousand births. This poor situation could be attributed to unequal dis-tribution of health facilities, malnutrition, poverty and inadequate allocation for the health sector. The survey, however, says that during 2006-07, 63 basic health units and 24 rural health centres were constructed while 20 rural health centres and 45 basic health units were upgraded to cover the deficiencies. But, still it looks minimal for the population of 160 million. (By Israr Khan, The News-4, 09/06/2007) Proposal on medico-legal departments pending KARACHI, June 9: A government proposal about conferring medico-legal status — ie the legal cover to attend to trauma cases — on private sector hospitals has been pending for two years, Dawn has learnt. On the one hand, there has been a delay in appointing medico-legal officers (MLOs) to private hospitals. On the other, private hospitals are reluctant to attend to injuries that have subsequent legal implications, such as gunshot wounds or accidents, and refer such patients to public sector tertiary care units where MLOs are present. Currently, no private hospital in the city has medico-legal facilities and while nine public sector hospitals have the required departments, only three of these are functional since the others lack the resources to entertain medico-legal cases. This is grossly inadequate in a city of 16 million people where at least 550 people die every year from road accidents alone. “We will appoint medico-legal officers without delay once private sector hospitals are ready to provide the necessary space and apparatus,” said Dr Abdul Majid, the government of Sindh’s Special Health Secretary (Public Health). He told Dawn that private hospitals are willing to accept a medico-legal status, as long as the government builds a separate building containing the emergency operation theatre, apparatus and even appoint the doctors. This, he said, would create a hospital within a hospital, which was not feasible. However, private hospitals point out that the government has taken no steps to improve emergency centres at established hospitals that already have medico-legal facilities. 100 In cases where legal proceedings are likely, such as accident or assault, the law of the country requires that an MLO examine the patient before treatment and issue a medico-legal certificate that records the nature, cause and gravity of the wounds. After this, the victim is attended to by the hospital’s regular staff of doctors and surgeons. Where a victim dies an unnatural death, the post-mortem examination to ascertain the cause of death is carried out by an MLO. The city’s expansion and increased traffic congestion in recent years means that the closest medico-legal hospital is often relatively far. According to sources in public tertiary care hospitals, a large number of people injured in accidents, terrorist attacks or clashes die on the way to a public sector hospital where medico-legal facilities are available. Private hospitals, conversely, are spread across the city. Medico-legal departments exist in the following nine hospitals: Civil Hospital in Saddar Town, Abbasi Shaheed Hospital in Nazimabad, Jinnah Post-graduate Medical Centre (JPMC) in the Clifton Cantonment Board, Qatar Hospital (Orangi), Government Hospital Korangi, Lyari General Hospital, Sindh Government Hospital Liaqatabad, Government Hospital New Karachi and Government Hospital Saudabad. Of these, only Civil Hospital, JPMC and Abbasi Shaheed Hospital have functioning medico-legal departments. The rest lack the resources and equipment to carry out these duties. This means, for example, that a patient injured in Malir or its adjoining areas has to be taken to the JPMC, which is at least an hour away, instead of the nearby Government Hospital Saudabad. Similarly, there is a medico-legal department in Government Hospital Korangi, but all such cases are referred to the JPMC. Doctors point out that the implications of this increased distance, particularly in life-threatening injuries, are obvious. According to Dr Seemi Jamali, deputy director JMPC, most medico-legal cases arrive at JPMC and almost all neurologyrelated cases – such as head injuries – are referred here since it is the only public sector hospital that has the required equipment. “We have a heavy load of emergency and trauma patients who need medico-legal certificates,” she said, proffering the view that other hospitals should share this burden and the government should develop policies in this regard. Hospital sources told Dawn that the five inoperative centres lack the resources to treat emergency cases. The problem has been compounded, they said, by a new system introduced in 2002, under which the presence of a forensic expert and a judicial magistrate is mandatory during the post-mortem examination of custodial deaths. They said the autopsy is usually delayed since both officers are often not available simultaneously. Even where medico-legal departments are operational, the situation remains grim. An investigation conducted by Dawn revealed that inadequate allocation of funds and the lack of proper facilities are impeding the performance of medico-legal doctors at the JPMC, Civil Hospital and Abbasi Shaheed Hospital. Doctors complained that they lack the apparatus to properly examine the nature and extent of wounds, particularly where invasive measurements are required. The accuracy of such data is crucial in subsequent legal proceedings. They said that modern techniques and equipment, such as electrically-operated cutters for bone, have not been introduced and MLOs have to perform post-mortem examinations with crude and obsolete apparatus. (By Arman Sabir, Dawn-17, 10/06/2007) Rs265m spent daily on smoking In the span of a single day, Pakistanis smoke cigarettes worth Rs265 million and their children, being exposed to passive smoking, directly affects their IQ level, senior medical professionals revealed on Saturday. Prof Nadeem Rizvi (Head of Chest Medicine Department ñ JPMC), Prof. Sirajud Daula (Pathology Department - Dow University of Health Sciences) were addressing a seminar, jointly organised by the Pakistan Medical Association (PMA) and Pakistan Society of Chest Medicine, in connection with World No-Tobacco Day. The speakers maintained that parental smoking enhances the risks of abortion, premature deaths, still births as well as diminished intelligence capacities among young children, who are either directly exposed to passive smoking or inhale the smoke in phase of foetus through their mothers. The scenario is quite grim in Pakistan, the experts warned, mentioning that the menace of smoking was getting equally severe in rural areas. A study published some times back in the Journal of Pakistan Medical Association (JPMA) reflected that 30 per cent of the daily earning of the country dwellers was spent on smoking alone. Another research study published in the same journal in 2003 had revealed that more than 23 per cent of the drivers running inter-city buses were chain smokers who smoked while driving the packed to capacity buses. (The News-14, 10/06/2007) The drug law of demand and supply Karachi has been revolutionized in recent times. Various development projects have been introduced, some of which have been completed and are functional. Karachiites are working harder by the day to make their city a better place to live in; is the city going in the right direction? As with all urban centers in the world, there are vices that enter through some back door in some nether region. Drug addiction is the most insidious of these. In Karachi, the frequency of drug abuse is highest amongst the skilled and unskilled labour categories (47 per cent), followed by business people (16 per cent), agricultural workers (5 per cent) and students (3 per cent). With the cloud of drug abuse ballooning rapidly, research finds that hashish is the most commonly used. Known in local parlance as charas, it seems to be the drug of choice in Karachi in terms of lifetime use and prevalence. While hashish is categorized as a drug, most users do not perceive it as a cause of social upheaval. However, in some areas, hashish related troubles have been reported. Karachi is a big city, one of the most sprawling and populated in the world. With the growing rate of drug abuse, it is difficult for administrators to track down the dealers and know their hiding places and costumers. Add to that a high level of corruption in the police force and you have an environment in which the drug trade can flourish easily. 101 Students form a large part of drug consumers in Karachi. We caught up with MYC ,an engineering student, whose middle name is Yasir. He told us: "There are a lot of places here where you can find people selling charas. Once you get into smoking this stuff, you can easily track down the dealers of different areas." Yasir, who will be 24 soon and lives in North Nazimabad. "We don't have to go to places far from ours," he says. "There are dealers who live near Pahaar Gunj (a hilly sort of area located behind North Nazimabad). Once you get into the smoking circle, you make contacts and then start buying stuff for yourself. Areas behind the Intermediate Board office, Block P, Q, R and S have many dealers living there who can be contacted by a phone. You can go to their places, but that's dangerous; you might bump into mobile snatchers or even policemen." MZA, 22, works as a medical representative and is also a resident of North Nazimabad. He tells Kolachi about his connections: "Stuff (charas) has become quite common. Youngsters are going for it because it is easily available. Many of the dealers live in the behind our block. They have different hideouts so it is difficult to track them but once you find their agents, you can easily buy stuff from them". Dealers in the areas around North Nazimabad are in big numbers as well. MZA, tells us about the areas near his locality where drug selling is at its peak. "The nearest place to find charas and its dealers here is behind Shadab Ground". He also told us about a place near the Tahir Villa roundabout in FB Area. "The dealers live behind the cricket ground. It is easy to locate the dealers, as everybody around knows them. You pay them, take the stuff and go home". But sometimes it's not that easy to go there and make a comfortable exit as Zeeshan discovered. "Policemen are also involved with dealers," he warns Kolachi. "If you are a regular customer and the dealers know you, it's alright. But if you are a new face they won't give you charas. Even if they do, the police would know that a new customer has arrived in the market. The dealers are in contact with the police and they inform them about any new customers that they get. The police will track you down after that and will only let you go once you've paid a bribe to free yourself. Oh and they will also take the charas from you". Kolachi managed to trace out a drug dealer, who did not tell us his original name but spoke about the drug dealing in Karachi. Mr D (pseudonym), 32, lives in Yasrab Colony near Super Highway; it's quite far away from the main city, near Baqai Medical College. When asked about his trade Mr. D said: "Though this area is quite far from the city, people come in large numbers because we sell the best quality charas there is." For Mr D, this knowledge is a source of great pride. Asked how he gets charas himself, he said it isn't difficult to have it sent here. The usual way of trading charas from different areas of Pakistan or neighbouring countries like Afghanistan is via buses and trucks. As the Super Highway is the main route, it is easy for Mr. D to have it sent to him. "Usually the stuff comes from Peshawar and Quetta where they grow it," says Mr D. "There are areas called Ilaqa-e-Ghair in the NWFP. That stuff is also exported. There is a huge market of hashish smokers so I am not sure if the amount grown here in Pakistan is sufficient but even if it isn't, they can always import it from our neighbours." So how dangerous is the job of selling charas in Karachi? Mr. D calmly replies: "Very. Sometimes you have to run for your life. But when you get into the groove and start making contacts, it becomes easy. Connections with the police and other agencies are very necessary otherwise we would be doomed. A friend of mine has been to jail twice." Another student, FAR, who is doing his Masters in Business Administration from a reputable institute, has been smoking dope for the last four years. He smokes everyday. How does he manage to buy so much stuff on regular basis? Isn't it a waste of money as well as an adverse effect on one's health? Disappointingly enough FAR is well aware of these things. "Yeah! It is. But it is getting out of control. I need it every hour of the day. Though it has affected both my mental and physical health I can't stop smoking weed. It sure is a waste of money though". How expensive is the drug in Karachi? FAR replies: "There are different rates at different places. It also depends upon the quality of the stuff. Sometimes you buy stuff for around 2000 rupees for 50 grams. You can even find people selling it at around 800 rupees for 50 grams but it is of very low quality". Charas is not the only drug being infused in our society. There are other substances available which are far more harmful to the users health and his environment; namely heroin, ecstasy and crack cocaine. These substances are regularly imported on a large basis and their dealers are making big bucks. With the involvement of law-enforcing departments making their job easier, they roam Karachi streets. One has to take notice of this trend to control it. Parents should be aware of their children's activities. School, college and university administrations should be watchful of their students and employees who are sometimes involved in distributing drugs on campus. Acknowledging the existence of this issue and being vigilant about it is an important measure to take if we want to keep Karachi from being permanently immersed in a vicious drug culture. (By Muhammad Shahbaz Zahid, The News-42, 10/06/2007) City govt hospitals need 900 doctors KARACHI, June 11: The city government needs another 700 to 900 doctors — both general physicians and specialists — to make 61 new health facilities functional, besides running the existing hospitals and dispensaries efficiently. The city government manages 271 hospitals and dispensaries and 13 of them are major facilities having a total of 1,843 beds. For them, 2,432 posts of doctors and 3,712 of paramedics have been budgeted. However, 15-20 per cent of the posts of doctors and paramedics are lying vacant since the retirement or death of the personnel. The prolonged ban on recruitment has kept these post still vacant. As many as 61 health care units, including hospitals, maternity homes and dispensaries, constructed over a couple of years in different towns of Karachi, are lying non-functional mainly for want of staff and the required funds. 102 According to an estimate, there is one doctor for every 5,000 patients and one paramedic for every 3,000 patients living within the jurisdiction of the city district government. The reality of ‘ghost employees’ is another factor aggravating the situation. Talking about inadequate furniture, a source said that doctors at 90 per cent of the city government health facilities could be seen sitting on the benches meant for patients. It is further learnt that 45-50 of the old health units in different towns are either non-functional or under-utilised for various reasons, mainly non-availability of doctors and paramedics, technical staff, medicines, equipment and furniture. Referring to the inoperative newly-constructed health care units, the source said no staff could have been appointed so far owing to the ban on recruitment, adding that due to the paucity of funds, medicines and other support facilities couldn’t also be made available there. A big population in Shah Faisal, Malir, Orangi, Baldia, Gadap, Landhi, Nazimabad, Bin Qasim, Korangi, Jamshed, Site and Keamari towns is deprived of the vital health care facilities which would, otherwise, have been available very close to their respective areas of residence. A source in the Sindh health department said that a request for the approval of the SNE for the 61 health care facilities was under consideration and allocations in this regard would hopefully be made in the coming budget. It is believed that staff for the CDGK-run health facilities, as well as those run by the other district governments, would be appointed on a contract basis till the availability of the permanent staff recommended by the Sindh Public Service Commission, the source added. (By Mukhtar Alam, Dawn-19, 12/06/2007) Celebrating the potential to save lives KARACHI: On World Blood Day, this year’s theme being ‘Safe Blood for Safe Motherhood”, the World Health Organisation (WHO) is to launch an initiative to improve the availability of safe blood for women who suffer child-birth complications. A noble task, yet convincing people to actually roll their sleeves up remains a challenge for people such as Dr Syed Abdul Mujeeb, Associate Professor, Blood Bank, Jinnah Postgraduate Medical Centre (JPMC). He blames not attitudes but a lack of awareness about the great need for blood donors. The question is, how to convert a potential donor’s good intentions into action. And, what do you do when women in need of blood are accompanied by queasy relatives? This becomes particularly important because the lack of donors forces blood banks to ask for blood to replace that being released. Last week, for example, Shazia (not her real name) came to the JPMC. She was in the eighth month of her third pregnancy and suffering severe bleeding. Had it not been for her husband’s friends, who donated blood to replenish the hospital bank’s stocks, she may well have lost her life. Asked why her husband did not donate his own blood, Shazia hesitated and then said, “He can’t, since he’s very weak.” Such an attitude has been observed frequently by Dr Shireen Bhutta, professor of obstetrics and gynaecology at the JPMC. “Many women refuse to let their husbands donate blood, citing his ‘weakness’”, she says. Even when such decisions can be the difference between life and death, “there are times when men fear the prick of the needle or refuse to countenance the sight of blood.” Her view is endorsed by Mohammad Jawaid, a senior technician at the hospital’s blood bank. However, he points out that while the JPMC blood bank tries to maintain a balance through the blood replacement system, “in emergencies the patient’s need always takes precedence over the need to replenish the blood bank.” The JPMC is a tertiary hospital and emergency obstetrics service is available round the clock. According to Dr Bhutta, this means that the hospital often gets the complicated cases and of the 35 deliveries daily, her department deals with 2 or 3 cases of postpartum haemorrhage (PPH) – the loss of over 500ml of blood after delivery. PPH is often related to multiple pregnancies or unsafe deliveries, while another major cause is chronic anaemia because of poor dietary practices. “The loss of 500-800ml need not be too dangerous for a healthy, well-nourished mother,” explains Dr Mujeeb, “but it can lead to disastrous consequences for anaemic women.” Of Pakistan’s 145 million strong population, 33 million women are of childbearing age and it is estimated that a woman dies from childbirth complications every 20 minutes. One-fourth of the preventable deaths among these are due to haemorrhaging, which Dr Mujeeb terms “cold-blooded murder.” The maternal mortality rate is officially estimated to be 533 per 100,000 live births. “This year’s theme highlights how voluntary blood donation can play a pivotal role in saving the lives of thousands of mothers and their babies,” says Dr Mujeeb. This would help Pakistan meet the Millennium Development Goals by 2015, he adds, pointing out that this seminal aspect of development has be completely missed by those working to meet the millennium challenge. After all, blood transfusion is one of the eight key life-saving interventions in healthcare facilities that provide emergency obstetric care. Countrywide, registered blood banks collect approximately 300,000 voluntary donations a year. The requirement is put at 34.5 million. “Only two people of every 1,000 donate blood voluntarily,” estimates Dr Mujeeb, calculating that if a mere two percent of the population gave a single unit of blood on their birthday, no citizen would die for want of a timely blood transfusion. So why don’t people donate blood? Dr Mujeeb believes that many people are not aware of the dire need. “It’s not that charitable feelings have been snuffed out within us,” he says, “we saw donors thronging blood banks after the 2005 earthquake and people come willingly during emergencies. But why do people wait for emergencies?” According to Dr Mujeeb, the failure lies in converting potential blood donors between the ages of 17 and 60 into regular voluntary donors. Referring to the blood replacement system, Dr Mujeeb points out that on many occasions, patients’ family members are 103 unable to provide safe blood. “Often, poverty and malnutrition renders men unfit to donate blood, while sometimes the potential donors are fewer than the blood bank’s requirement,” he commented, emphasising the need to develop a voluntary donation system. It all boils down to institutionalising the blood banking system. “A centralised system is needed and this is possible given developments in information technology,” believes Dr Mujeeb. “We could develop satellite centres where blood is collected and then preserved at a central place from where it can be distributed according to need. Given that the shelf-life of blood is 35 days, this would be cost-effective since less blood would be wasted. Usually, we give whole blood since the various components have not been separated, but if it were, one unit of blood could fulfil the needs of multiple patients.” Dr Mujeeb also believes that donors should be made to feel special for their act, which is after all a noble one. As an incentive, he suggests free diagnostic facilities for regular voluntary donors. (By Zofeen T. Ebrahim, Dawn-17, 14/06/2007) World Blood Donor Day The annual requirement of blood in Sindh is approximately 4.5 million bags (500 ml each) but only 1.7 million of these can be acquired through voluntary donation, according to statistics of the SBTA (Sindh Blood Transfusion Authority). Third world countries strive to address the issue of obtaining safe blood for recipients. Increasing spread of communicable diseases, ignorance and laxity on administrative fronts in identifying carriers of communicable diseases, and illiteracy are all playing havoc with the procedure of blood transfusion. On the occasion of World Blood Donor Day on June 14, the SBTA aims to encourage greater voluntary blood donation, assuring that donating blood at least once a year is a perfectly safe practice for healthy males and females. Provincial Secretary of the Sindh Blood Transfusion Authority since November 2005, Dr Zahid Hasan Ansari strongly believes that increasing numbers of people should be convinced to donate blood, and this message should translate into a chain reaction. He stated that this day must be taken as an opportunity to increase awareness about blood donation, which is not only a healthy practice for the donor and a life saving act for the recipient, but it could also serve as an effective way of identifying individuals carrying communicable diseases. Thus, if organised better, blood donation could help curb the spread of these diseases. “When an individual donates blood at any of the registered blood banks, complete information about him is recorded on the official Performa that has to be filled before donation. The blood is screened for communicable diseases which include HIV, Hepatitis B and C, and Malaria absolutely free of cost. If a person is found positive in any of these tests, he or she is informed in full confidence in order to protect his or her privacy,” said Ansari. He also stated that people carrying communicable diseases don’t realise the jeopardy they may cause in the lives of those around them. “There is an urgent need to put in place an organised system of blood screening to avoid serious repercussions for the whole world,” he said. The SBTA is working vigorously to ensure the establishment of as many blood banks as possible across the province. Ansari proclaimed that since he undertook his current office as secretary, he has established 45 blood banks, whereas only 38 blood banks were established by the SBTA between 1998 and 2006. “We are trying to make sure that every district in the province has its own facility so that people don’t have to run to the metropolis in each and every emergency. Out of 23 districts in Sindh, only eight have no registered blood banks and these are Matiari, Tando M. Khan, Ghotki, Jamshoro, Kashmore, Umerkot, Noshehro Feroz and Shehdad Pur. We are trying to establish one in each of these districts in the near future,” he said. In keeping with the criteria outlined by the World Health Organisation (WHO), ideally all blood banks should contain four rooms for each department. Furthermore, every blood bank should have a collection area, donor area, screening and laboratory area, and a reception room. Ansari claims that the blood banks endorsed by the SBTA strictly conform to these requisites. He stated that people will feel comfortable donating their blood at any of the registered blood banks. “It is a priceless gift of life and any commercial concerns that certain people derive out of it must be strongly condemned and curbed by all means,” he said. There are 85 registered and licensed blood banks endorsed by the SBTA all over Sindh, of which Karachi alone has 47. These figures include both public and private banks, although a majority of these are public blood banks. These blood banks are inspected and supervised by the SBTA under the guidelines of Safe Blood Act of 1997. Moreover, the SBTA ensures adherence to the WHO guidelines and ethical concerns. People are strongly encouraged to donate blood at any of these banks. (By Asra Pasha, The News-20, 14/06/2007) Promoting safe blood donations ONE of the concerns cited by Pakistani doctors on the occasion of World Blood Donor Day that was observed on Thursday, was the absence of the culture of voluntary blood donation in the country. Statistics show that 300,000 voluntary donations are made every year to registered blood banks. However, this figure falls far short of the required number. What we see, instead, are donors who are required to give blood to replace what has been given to a relative in need of a transfusion. They constitute the majority of blood donors. There are also a substantial number of paid donors, many of them drug addicts whose use of shared needles may have infected their blood. This is frequently unscreened and can be a source of disease when it enters the bloodstream of a patient. While the health authorities have lately woken up to the problem of contaminated blood donation, and have undertaken periodic campaigns to seal blood banks storing expired or unscreened blood, they have not done enough to address the need for encouraging voluntary donations. It has been observed that the blood of regular voluntary donors is generally safe. It is properly screened and the volunteers’ medical history is carefully noted to ensure that they are suitable candidates for 104 donating blood. This is a trend that must be encouraged so that the need for paid donors can be gradually eliminated and voluntary donors can become the main source of blood supply. At the same time, health authorities must ensure that donors themselves are not at risk from unsafe medical practices in hospitals and that no more than the specified amount of blood is taken from them. In the absence of these safeguards, those willing to give blood might think twice before coming forward to donate. (Dawn-7, 15/06/2007) Not enough drops to go around? The drive to eradicate polio in Sindh has begun to show symptoms of what health planners described as ‘donor fatigue’, as the forthcoming Sub-National Immunisation Days (SNIDs) in July will exclude five of Karachi’s eighteen towns on account of the paucity of funds, sources said. Doctors involved in the campaign have lately learnt that the Expanded Programme of Immunisation (EPI) has cut grants for special immunisation days geared towards polio eradication on the pretext of a shortage of funds. Consequently, provincial health planners have been compelled to drop five towns from the next round of SNIDs. Instead, resources will be mobilised to focus attention on other neglected areas of Hyderabad, Matyari and bordering areas of Balochistan, where health planners believe the risk of transmission of wild polio virus to be growing larger with the frequent movement of people from one province to another. However, the EPI-Sindh has expressed willingness to go an extra mile and cover all five towns of Karachi during the forthcoming SNIDs if only the federal government could provide extra doses of oral polio vaccines (OPV). “Provided OPVs, we can run the immunisation drive in all 18 towns of Karachi,” stated project director EPI-Sindh, Dr Salma Kausar Ali. Efforts to eradicate polio from Pakistan are considered to be in their final phase with only nine polio cases so far confirmed from the length and breadth of Pakistan. However, international donors including Global Alliance for Vaccine Initiative and Rotary International seem disappointed with the performance on the immunisation front. Poliomyelitis is an acute viral infection of the nervous system. More than half of the infections are found among children under five years of age. One in two hundred infections leads to permanent paralysis, usually of the legs. In 5-10 per cent of these cases victims die when breathing muscles are paralysed. “Since the launch of the Global Polio Eradication Initiative in 1988 the number of reported cases worldwide has fallen from 350,000 to 1968, a decrease of over 99 percent,” the World Health Organisation (WHO) says in its latest report. “Today it remains endemic in four countries; Nigeria, India, Afghanistan and Pakistan.” According to health managers, Sindh like the rest of the country has just marked 67th round of national immunisation days (NID) for polio. June and July are traditionally considered the peak months for transmission of the polio virus. “We opt for the SNID to bolster our efforts to contain the polio virus circulation,” another doctor explained. While underscoring the critical nature of arresting polio virus, special secretary public health in Sindh, Dr Abdul Majid Lyari, wised up/(informed?) Karachi’s 18 town health officers that the shortcomings of polio eradication campaigns have been frustrating donor agencies resulting in cost reduction measures at the critical juncture when the ‘crippling virus deserves the last push’. “We will not be marking SNID in Bin Qasim, Malir, Landhi and Jamshed Town, because we are not given enough funds to replicate the immunising exercise all over the province,” Lyari maintained while speaking at a meeting of town health officers last Saturday. “We need to gear our efforts to raise the 80 per cent immunisation coverage to 90 per cent and beyond, for results.” The EPI has documented 8 new cases of polio from all over Pakistan. Of these, four have been reported from Sindh: two from Jacobabad and one from Karachi and Khairpur each. The child from Karachi was found infected with polio-1 or P1 virus whereas the remaining three were infected with the P3 virus. Lyari also emphasized the importance of enhancing routine immunisation coverage besides going out for special rounds of polio immunisation. He minced no words reminding town health officers that Sindh has somewhat low routine immunisation coverage, ranging from 42 to 45 per cent. “We have to bring our routine immunisation coverage at par with 80 per cent coverage during the NIDs.” Furthermore Lyari expressed the belief that Karachi district has shown no indigenous circulation of poliomyelitis. According to him, Karachi has reported a single confirmed case of polio caused by P-1 virus. “We know that the very type of virus is circulating amongst the moving population and Karachi is a melting pot for the rest of the country.” On the other hand, Dr Salma Kausar Ali not only agreed with Lyari’s assertions but elaborated that northern Sindh is a reservoir of P-3 virus, and therefore requires special focus. She hoped that the strengthened immunisation drives would soon deliver results. “We are in the last phase of eradication when we need an all out effort,” she said. (By Asadullah, The News-20, 15/06/2007) Rs1.4bn for 80 health schemes KARACHI, June 15: The Sindh government has allocated Rs1,400 million for 19 new and 61 ongoing health schemes under the Public Sector Development Programme in the next financial year (2007-08). The new schemes likely to be initiated in the new financial year include establishment of a bone marrow transplantation unit at the Sindh Institute of Urology and Transplantation. The total cost of the project is Rs500 million of which the government will release Rs83 million in the new fiscal year. Besides, Rs46 million has been allocated for up-gradation of radiology department and medical and surgical units, construction of general canteen at the Civil Hospital Karachi and construction of an OPD Block at Lyari General Hospital. 105 Under the ongoing schemes, the government has allocated Rs50 million for the establishment of cardiac surgery, paediatric cardiology and other services at the Karachi Institute of Heart Diseases. The total cost of the project, as estimated by the government, is Rs399.679 million. According to the budget documents, funds have also been allocated for fresh initiatives like improvement of Liaquat University Hospital, Jamshoro; construction of 40-bed wards for the ophthalmology department of Chandka Medical Hospital, Larkana; construction of an accident and emergency centre at DHQ hospitals; incinerator for the Institute of Chest Disease, Kotri; establishment of a cardiac emergency centre in Landhi, Karachi; and for the construction of a trauma centre on the Indus Highway at Amri, Jamshoro. In the medical education sector, the government has planned establishment of a library as well as purchase of equipment and furniture for second and third professional departments at the Ghulam Muhammad Mahar Medical College, Sukkur. The ongoing projects, which will continue to get funds in the new fiscal year, include establishment of a cardiology department at Lyari General Hospital, Karachi; renovation of the emergency department, ENT wards and CCU department at the CHK; expansion of Chandka Medical College Hospital, Larkana; an extension project of Behbhani Hospital, Saudabad, Karachi; improvement of the Institute of Skin Diseases Hospital, Karachi; upgrade of Taluka Hospital, Gambat, to the level of an institute; and repair and renovation of primary health care facilities in nine districts. Since no funds were previously provided for the establishment of a vaccine laboratory for anti-snake venom/ rabies at Tharparkar, the financial managers of the provincial government have made an allocation of Rs20 million for the project this year. The total cost of the project is estimated at Rs200 million. The budget documents also indicate that no substantial progress was made regarding the establishment of a general nursing and midwifery training school at Liaquatabad Government Hospital in Karachi. Under the preventive programme, no new scheme has been introduced. However, a sum of Rs164.864 million has been allocated in the budget for the nine ongoing projects under the preventive programme of the health department. (By Mukhtar Alam, Dawn-17, 16/06/2007) Medical training in Pakistan Michael Moore has scandalised America again. He did it first with Fahrenheit 9/11, arguably the most famous US documentary film of all times. Now he has produced another which has received raves at the Cannes film festival. Sicko savages the US healthcare system and extols the Cuban healthcare system. I have not seen it yet, but it can’t be all that bad and may even have some grain of truth if so many US commentators, especially from the right, are so incensed by it. As a part of the US healthcare delivery system for over thirty years, I have seen the best and the worst of it. But for all its faults, the quality of care most US citizens got was always of a reasonably good standard. This of course does not mean that every body gets equally good treatment. The real problem is that of access. There’s much about healthcare delivery in the US that can be criticised. What is admirable, though, is the almost universally comparable quality of programmes that train physicians. Graduates from medical schools in the US, like most other places including Pakistan, are smart, committed and relatively idealistic individuals. What turns these young men and women into good doctors is the postgraduate training they receive. Of the thousands of training programmes in the US that prepare these young physicians to take care of patients in the real world, national oversight committees and specialty boards enforce a certain basic standard. If a doctor wants to practice internal medicine, general surgery or any of the specialties, he or she must go through a similar basic training programme and then sit for the identical specialty board examination in that discipline. In short, every surgeon in practice has undergone similar if not identical training and has taken the same examination as any body else in that specialty at that time. I started to think about all this stuff because of a controversy that recently surfaced concerning different levels of specialty training for different physicians. What made the situation more piquant for me was the fact that the controversy surrounded my alma mater, King Edward Medical College (Now University). At odds are two competing concepts. One view is that all specialists in a particular discipline within medicine must be equally well trained and possess the same basic qualifications; the other view is that we need less trained physicians since they will opt to work in lesser-developed areas. Perhaps the Pakistani hang up about different levels of training for different classes of people is a leftover from the days of the Raj when most specialties were not as advanced as they are today — a year or two of postgraduate training was usually enough to get the hang of things. The controversy is, should the King Edward Medical University, successor to KEMC also be offering different sub-specialty diplomas. In principle, KEMU has the right to provide whatever type of medical education it decides. But as somebody who trained in the entirely egalitarian system of US training programmes, I personally find the multi-tier system of specialisation, as it exists in Pakistan, entirely counter-productive. Whether Kabirwala deserves the same level of trained physicians as Lahore is not a medical question but rather a political one. What comes first, well-trained doctors or well-equipped medical facilities? It might sound like a chicken or the egg question but in my opinion well-trained physicians inevitably help to create well-equipped facilities. Presently, in Pakistan, there are three types of postgraduate medical qualifications available to physicians. At the top is a fellowship from the College of Physicians and Surgeons of Pakistan (CPSP) in almost very specialty. This is a reasonably standardised postgraduate training system. Yes, it has many inadequacies but these can be improved upon and in my opinion that is the way to go. After the fellowships awards by CPSP (FCPS) come the Master of Surgery (MS) and Doctor of Medicine (MD) degrees 106 awarded by different universities. The clinical training and the level of expertise acquired by physicians who obtain these degrees vary extremely. Most young physicians today prefer to enrol in the CPSP programmes rather than pursue an MS or MD. These degrees will in time hopefully become what they should be — post-fellowship degrees for people who wish to pursue an academic career. At the bottom of the specialist heap are the diploma holders. The justification for producing such less trained specialists is that by virtue of not being trained well enough they will not mind working in less developed areas. This is not only discriminatory to the candidates themselves but also creates the pernicious impression that people living in less developed areas do not deserve first-rate medical care. What I find most bothersome about this approach can be put simply: what would a person preparing for a diploma not be taught compared to someone preparing for a fellowship? For instance, in the field of cardiac medicine, will the diploma candidate not be taught the latest treatments for heart attacks since these are too expensive to ever become available in small towns? For all the policymakers and especially the politicians, the question then is, do they want to have a semi-trained specialist come treat them if they have a heart attack while visiting their hometowns or campaigning in their constituencies during the upcoming elections? Finally, I want to see the KEMU become a great medical university like some in the US and elsewhere. I hope that it will provide the best possible training to CPSP candidates through its faculty and affiliated teaching hospitals. Perhaps one day it will become the obvious first choice for graduates from any medical college in Pakistan who wish to pursue sub-specialty training. (By Syed Mansoor Hussain, Daily Times-A7, 18/06/2007) 4 out of 10 people at madrassas suffer diabetes KARACHI: Four out of every ten people who are overweight and above the age of 30 are diabetic or very close to having the disease because of a lack of exercise, according to results of a study conducted by the Baqai Institute of Diabetology. The study was conducted with a sample of 1,000 people under the supervision of Secretary General Diabetic Association of Pakistan Prof. Abdul Samad Shera and Director Baqai Institute of Diabetology Prof. Abdul Basit and Dr Muhammad Zafar Iqbal Hydrie. Camps were set up at four religious seminaries where Baqai hospital teams conducted the survey. The study was carried out in collaboration with Oslo University and aims to create awareness about diabetes and preventive measures that can be used, such as a more active lifestyle. “Public awareness could save fifty percent of vulnerable people from the disease,” said Program Coordinator Dr Zafar Iqbal Hyderi. “An imbalanced diet and sedentary lifestyle are its main causes. The disease has serious consequences, and even affects the eyesight and kidneys.” The Baqai Institute of Diabetology and Endocrinology is organizing a food festival on June 23 to help create awareness about diabetes and its related diseases. Sugar and cholesterol tests will be offered free of charge and experienced medical experts will be available for advice. The festival will be held from 10:00 am to 3:00 pm. Entry costs Rs 20, and children under 12 have free admission. (Daily Times-B1, 19/06/2007) PM’s hepatitis control scheme Over 2,000 patients await free treatment KARACHI, June 19: Some 2,440 patients registered under the Prime Minister’s Programme for the Prevention and Control of Hepatitis in Sindh are still awaiting the promised free treatment, Dawn has learnt. Meanwhile, patients currently under treatment are suffering because of the slow supply of medicines. According to a source in the programme, an additional 2,750 healthcare workers and citizens were screened for Hepatitis-B and -C at the Civil Hospital Karachi and the Jinnah Postgraduate Medical Centre (JPMC) up to April 15, 2007, of which about 300 tested positive. Currently, 11 designated centres – including one in Karachi – are dispensing free treatment to hepatitis patients in Sindh under the programme. Launched in August 2005, the five-year programme was allocated Rs2.52 billion at the country level. During the first phase, which was supposed to continue till June 2006, Sindh was promised resources – including the vital Interferon injection – for the treatment of 1,740 Hepatitis-C patients. The programme also stipulated measures to ensure safe blood transfusions, syringes and sterilised medical equipment in government and private hospitals. The matter is one of serious import since sources quote a Ministry of Health study which estimates that about 3.6 per cent of Sindh’s population is infected with Hepatitis-B, while 5.4 per cent suffers from Hepatitis-C. The incidence of Hepatitis-A, a self-limiting virus, is at least one episode suffered under the age of 15 by 97 per cent of the population. Under the mechanism evolved by the Prime Minister’s Programme for the Prevention and Control of Hepatitis, committees have been formed in chosen hospitals of the provincial health departments and the federal government in Sindh. These determine patients’ eligibility and register them for free treatment. The programme’s provincial coordinator, Dr Zulfikar Ali Gorar, conceded that there had been delays in the delivery of medicines to registered patients but “things are now under control.” He said that supplies of the injection Interferon and the capsule Ribavirine will shortly be delivered to Sindh’s director-general health, after which the needs of patients awaiting treatment would also be catered to. Dr Gorar informed Dawn that the province’s 11 centres have been functional since July 2006 and 526 patients have so far completed the treatment, which comprises 72 Interferon injections and other medication administered over six months. The treatment of 98 out of 235 registered Hepatitis-B patients is underway, while about 2,100 registered Hepatitis-C patients are on the waiting list. Referring to the incidents when patients have quarrelled with doctors, Dr Gorar said that a break of up to one month in the administration of Interferon would not harm Hepatitis-C patients. 107 Meanwhile, Prof. SM Munir, point-person for the PM’s programme at the JPMC, told Dawn that the hospital has registered about 1,000 patients, of which 127 had completed treatment. The treatment, raging from one to four months, of another 700 patients is currently underway. Referring to the estimated 100 registered patients who have not contacted the hospital for medicine, Dr Munir said that the supply was delayed for about two months, during which some patients stopped coming to the centre. He said that these people must be informed that medicines are now available and that they should report immediately. (By Mukhtar Alam, Dawn-17, 20/06/2007) Woes of hepatitis patients FREE treatment for almost 2,500 patients of hepatitis in Sindh has been held up because of delays in the supply of medicine. The patients are registered under the Prime Minister’s Programme for the Prevention and Control of Hepatitis that was launched in 2005 and which also aims at providing potable water, Hepatitis B vaccines and Hepatitis C medication. Unfortunately, so far the programme has not proved very effective in Sindh or elsewhere in the country for that matter. Not only does the provision of medicines leave much to be desired, little headway has been made in creating awareness about the two blood-borne diseases. While definite figures for hepatitis (B and C) patients in the country are not available, the World Health Organisation fears that this could be as high as 10 million. This is not surprising considering that most people have not been vaccinated against Hepatitis B and are exposed to dangerous medical practices, such as the reuse of syringes, which could cause the hepatitis virus to enter their bloodstream. This concern is exacerbated by the knowledge that Pakistan has one of the highest use of injections worldwide, and doctors here administer these to even those who do not need them. There is need for greater research on the incidence of the disease to get a clearer picture of what kind of health strategy should be employed to treat the patients. Similarly, a greater check must be kept on hospitals and clinics to ensure that contaminated medical equipment is not used on patients. Educating the public about the modes of transmission of bloodborne hepatitis and of its health implications is also necessary to prevent their going to quacks or doctors with doubtful qualifications. Meanwhile, the government must step up the supply of medicine to contain the suffering of patients registered under its hepatitis control programme. (Dawn-7, 21/06/2007) Protecting children WHEN it comes to the state of health, there is never any good news. A new report by the Society for the Protection of Rights of Children is no different. It says that every one minute, a child in Pakistan dies from EPI disease, diarrhoea or acute respiratory diseases. We have known for some time that the infant and maternal mortality rates are very high in the country but according to Sparc, they are the highest in South Asia. This is particularly depressing given that the mortality rate for children under five years had declined over the last few years and now stands at 101 per 1,000 births. But this figure is just one out of other very gloomy figures on children’s mortality and health. Sparc reports that nearly 20 per cent of children are born with low weight. Almost 40 per cent are under the age of five suffer from malnutrition and 13 per cent of them severely underweight. Then there are horrifying figures on the abuse children faced last year at home, school or at work. That an estimated ten million children are working is sad in itself, as is the figure of over six million children not going to school. This report is an eye-opener and should prompt the government into taking immediate action to protect the welfare of children. Existing laws on the issue need to be effectively implemented. Children should not be dying of diseases that can be easily prevented with access to clean drinking water, and proper sanitary conditions, nutrition and immunisation. The nasty campaign against polio vaccine did a lot of harm in the NWFP which must be tackled without delay. It is the government’s responsibility to ensure that they are at school where they can have a chance at bettering their lives. (Dawn-7, 22/06/2007) 4 percent of Sindh’s women die during pregnancy or delivery KARACHI: Sindh has a four percent mortality rate in women during pregnancy mainly because there are not enough doctors, the Sindh government told the provincial assembly Thursday. Provincial minister for health Syed Sardar Ahmed provided this information while responding to a supplementary question during question hour on the health department. He said that the government was working to overcome the shortage of doctors and has planned to recruit at 450 of them at the local level. Answering different questions from Opposition members, Ahmed said that during the years 2003-2004 and 2004-2005 about 14 women expired in district Sanghar during their pregnancies or deliveries. Similarly, 21 women died in district Mirpurkhas during the same period, four in district Umerkot and 49 in district Badin. According to him, district Hyderabad had the most casualties as 156 women lost their lives during their pregnancies. In another written reply, the minister told the assembly that there were no MRI and CT Scan tests available in any Hyderabad government hospital. Ahmed also said that there had been no incident of anyone leaving any surgical instruments in a patient in any government hospital of Hyderabad during January to September 2006. However one incident took place in 2004 in which a patient was brought to Liaquat University Hospital on February 2, 2006 to be operated on for the removal of scissors left in her abdomen two years earlier. She did not survive. In another query, he said no new hospital or dispensary has been sanctioned for Hyderabad district in the current financial year. However, he added, they have successfully upgraded and improved existing health facilities in the district hospitals and health centers, including the district government hospital, Qasimabad, district government hospital, Pareetabad, basic health units at the Latifabad No.10 and Liaquat Colony. To another question, the minister disclosed that at present no standard procedure was available to open a private medical centre in the province. However, he added, an Accreditation and License Ordinance/Bill for private hospitals and clinics was being formed. (Daily Times-B1, 22/06/2007) 108 Quintuplets born to Afghan woman QUETTA, June 24: An Afghan woman gave birth to five children, four boys and one girl, in the Bolan Medical College Hospital early on Sunday morning. “It was a normal delivery,” gynaecologist Dr Mahrukh said. The woman, Ruqaiya, was brought to the hospital by her husband Maulvi Ahmed Jan from the suburban Pashtoonabad area. It was the first delivery of quintuplets in Quetta, hospital sources said. “The mother and the babies are in good health,” Dr Mahrukh said. Maulvi Ahmed is an Afghan refugee living in Quetta for a long time. He owns a grocery shop in Pashtoonabad. Before the God’s gift of the quintuplets, he had three children, one of whom had died some time ago. (By Saleem Shahid, Dawn-1, 25/06/2007) New record at JPMC Saturday’s storm created a new record for the emergency ward of Jinnah Postgraduate and Medical Centre where a very large number of patients were brought in for medical treatment. The fire at a shopping mall in Clifton also put pressure on the limited services available at city hospitals as many people turned up for medical treatment. While on an average, 500 to 550 patients are handled daily at the emergency ward of JPMC, on Saturday around 1,250 patients were brought to the emergency ward. Some time back 1,100 patients were admitted to emergency ward of JPMC in a single day due to outbreak of Dengue fever in the city. This was the previous record. However, this record was broken due to Saturday’s higher number of rain’s victims that were provided treatment at the emergency ward. In charge of Emergency at JPMC, Dr Seemin Jamali, said that 13 dead bodies were brought into the hospital due to incidents that occurred due to rain. Moreover, she said 70 persons were admitted in the emergency ward for variius injuries due to rain. She said injured patients had a variety of injuries like head injuries and fractures on hands and legs. She said some patients were injured due to the hoardings and electric poles that collapsed in parts of the city. Some patients got injuries due to road accidents. Dr Jamali said that some patients got injured due to collapse of roofs and walls. “Saturday was an exhausting day for me and for other staff of emergency ward. We handled 17 injured of firebreak of Clifton, 40 patients of heatstroke, 250 patients of gynecology and there were also patients of routine casualties at the emergency ward,” Dr Jamali said. She said the staff of emergency who had come to the hospital to work for the morning shift had been working during the evening shift as well to deal emergency like situation in the city on Saturday. Medical Superintendent of Civil Hospital, Dr Kalim Butt said due to heavy rain and speedy winds, five dead bodies and around 60 injured persons were brought to his hospital. He said two teenage girls namely Chanda and Anita expired due to electric shock from a cable that had broken and fallen on the ground from an electric pole. He said two dead bodies brought into the hospital due injury from falling roofs. He said one man expired after falling from a rooftop and he got severe head injuries. Dr Kalim Butt said majority of injured persons that were admitted suffered minor injuries. He said most of these patients got bruises on different parts of their bodies. He said, as their condition was not bad so they were discharged from the hospital after providing them first aid. (The News-13, 25/06/2007) Alarming rise in gastroenteritis cases after rains KARACHI, June 28: A surge in cases of gastroenteritis or diarrhoea arriving at various hospitals and other health care facilities has been reported over the past few days and health experts are attributing the trend to the deteriorating quality of drinking water following the rains as well as carelessness on the part of its consumers. Medical Officer of the Civil Hospital Karachi Dr Kaleem Butt said that as many as 82 children and 41 adults were brought to the Diarrhoea Treatment Centre and the Emergency Section of the hospital on Thursday. A 40-year-old resident of Sultanabad died from diarrhoea at the hospital at around 2.30 pm, he added. Most cases reported at various hospitals are children. According to another report, an eight-year-old boy, reportedly a gastroenteritis patient, died in a village in Gadap Town on Wednesday. A doctor at the Emergency Section of the National Institute of Child Health said that about 20 children aged one to eight years were brought there after 3pm with the history of loose motions and vomiting. However, after necessary medication, all of them are now in a stable condition, he added. He observed that the number of gastroenteritis cases had registered a rise from Wednesday. A house officer at the Diarrhoea Treatment Unit of the NICH told Dawn that about 50 children up to the age of 12 were treated since Thursday morning and 20 of them had to be admitted. An official of the Sindh Health Department said that the number of patients with symptoms of gastroenteritis arriving at the government hospitals in the city after rains was increasing gradually. On Wednesday and Thursday alone, as many as 1,571 patients were brought to various hospitals in the province, he said, adding that in Karachi, 700 cases were reported at the hospitals and health care facilities managed either by the Sindh government of the City District Government Karachi. 109 According to a break-up, the CHK received 72, the Saudabad Government Hospital 48 and Qatar Hospital Orangi 90 patients. As many as 61 patients with the symptoms of diarrhoea and vomiting were taken to the New Karachi Hospital, another 31 to Abbasi Shaheed Hospital, 45 to North Karachi Children Hospital and 50 to Landhi Hospital over the past 24 hours, according to the reports received by the health department by noon on Thursday. The number of gastroenteritis cases registered at different hospitals in Karachi on June 20-22 was between 350 and 450. A senior official at the Jinnah Postgraduate Medical Centre said that the number of such patients arriving there was not alarming. Experts view that gastroenteritis is caused mostly by substandard water and food prepared or stored unhygienically. The factors involved include absence of electricity for long hours as this renders refrigerators and freezers inoperative. Food and other eatables kept in the appliances go bad and become unfit for human consumption. The experts advise people to avoid consuming such dicey food items and ensure the quality of food available at food outlets in this season. A doctor advised parents to start administering ORS or some home-made solutions to their children upon detecting symptoms of diarrhoea and vomiting immediately. In case of deterioration in the condition, a patient must be rushed to a competent doctor. Healthcare professionals also advise people to consume boiled water in view of the possibility of piped water getting mixed with rainwater or sewage during and after rainfall. (By Mukhtar Alam, Dawn-17, 29/06/2007) Two die, over 700 admitted for gastro KARACHI: Two people died of gastroenteritis Thursday and there were reports that over 700 people suffering from it were admitted to hospitals throughout the city. This was confirmed by Public Health Sindh Deputy Secretary Dr Shakeel Malik. He said that one unidentified eight-year-old boy died in Gadap Town. The other was 40-year-old Sarwar, a resident of Saeedabad, who died at Civil Hospital Karachi. He said that the most patients (90) are currently admitted at Qatar Hospital in Orangi Town. And 72 people have been admitted to Civil Hospital in the last 24 hours. APP reported that children from different parts of Balochistan and the interior of Sindh were arriving with Malaria as well. The CHK Pediatrics Department has registered a surge in the cases of malaria, both falciparum and cerebral, during the last few days, according to chief Prof. Ayesha Mehnaz. Children are coming from Lasbella, Hub and Thul with cerebral malaria. “These were the cases which were besides falciparum malaria, which is also caused by the bite of a mosquito that breeds in stagnant and dirty water,” she said. She strongly recommended the need to massage children with mustard oil or make them sleep under mosquito nets, also recommended for adults. Also, children under two in particular have been reporting with gastroenteritis as well as other viral infections at the National Institute of Child Health since Wednesday evening. “Since Thursday morning more than 20 cases of gastro were brought to NICH and a few had to be admitted due to severe dehydration,” a doctor on duty said. Another senior doctor said children of up to 12 years were being brought directly by their parents or were being referred by GPs with varied viral infections. “We do fear a surge in the next few days - perhaps by early next week,” Prof. Ayesha Mehnaz added. The Pediatrics Department at Lyari General Hospital has also registered a marked increase in the incidence of gastroenteritis among children brought to its OPD since Thursday. Dr Mushtaq Memon told APP Thursday evening that more than 30 percent of all cases reported to the department were either severe diarrhoea or gastro ones. There were 100 cases of the two inter-linked ailments brought Thursday, he said, mentioning that most of the children were below six months of age. “25 percent of these children were dehydrated,” he said. Memon said he and his team of doctors preferred to give ORS to the patients followed by drips. (Daily Times-B1, 29/06/2007) Over 670 gastroenteritis patients land in govt hospitals KARACHI, June 29: Another 675 patients suffering from gastroenteritis or diarrhoea were brought to government hospitals from different parts of the city on Friday, out of which 80 were admitted. A deputy secretary of the public health department of the Sindh government, Dr Shakeel A. Mullick, said on Friday evening that a total of 1,512 patients, including 562 of Karachi, were brought to government healthcare facilities across the province during the last 24 hours, ending at 12 noon. Besides the Civil Hospital Karachi and New Karachi Hospital, 482 patients were rushed to city government hospitals and clinics, out of which 39 were retained for further treatment. “In all 44 patients, mostly children, were admitted to government hospitals who have been reporting on the subject to the Sindh health department for some time,” Dr Mullick added, saying that no deaths were reported on Friday. Lyari General Hospital Dr Khawaja Mukhtar, Medical Superintendent of Lyari General Hospital, which caters to people in the low-lying areas, said that though the reporting of gastroenteritis and diarrhoea at his hospital had increased there was no emergency-like situation. “After the rains the average per day intake of children and infants with a history of diarrhoea and vomiting ranged from 15-20, while the nature and degree of infection was not so severe,” he added. National Institute of Child Health About 50 patients were brought to the casualty section or OPD of the National Institute of Child Health (NICH) till 8pm on Friday. A doctor on duty at the diarrhoea treatment centre said that as many as 20 patients had been admitted since morning for further treatment and assessment as they were relatively serious cases. A doctor at the casualty and emergency section of the NICH said that the number of patients complaining of vomiting and diarrhoea increased on Friday in comparison to Thursday’s figures. “Some patients are brought in the night also,” he added, saying that the total number of gastroenteritis patients could go up to 60 for Friday. 110 Jinnah Postgraduate Medical Centre Dr Seemi Jamali, Deputy Director and in-charge of Emergency and Accidents at the Jinnah Postgraduate Medical Centre, said in the night as many as 25 patients, both men and women, including senior citizens, were rushed to the hospital for gastroenteritis interventions, out of which two were admitted for comprehensive treatment. “The remaining patients with a history of diarrhoea, vomiting and fever were sent back after some treatment and rehydration,” she added, saying that so far the situation had not reached epidemic proportions. PMA’s appeal Meanwhile, the Pakistan Medical Association (PMA) has once again reminded people to take extreme preventive measures to avert gastroenteritis, waterborne diseases and ailments such as conjunctivitis, flue, sore throat and skin diseases. “The only remedy to prevent these diseases is to take preventive measures. People should always use boiled water, take plenty of water during the day, use ORS in case of diarrhoea and vomiting, and if it is uncontrollable, a qualified doctor should immediately be consulted,” the PMA statement said. (Dawn-17, 30/06/2007) Heroin-addicts fixing electricity faults Believe it or not but it is a daily happening in various localities of the megapolis where people are hiring private electricians, skilled or semi-skilled persons and even drug-addicts. These hired technicians risk their lives for repairing and fixing hightension electricity wires and other faults so as to restore power supply in their respective areas in the absence of help from the city’s power utility, KESC. One such event occurred in UC-7 of Gulberg Town, behind Karachi Institute of Heart Diseases (KIHD), where some young men - highly disappointed by performance of KESC staff and annoyed with 24-hour power breakdown — hired a drug addict to repair jumpers of a PMT to restore electricity in the area. “My younger brother Naeem, 21, along with his friends, was cursing KESC at a playground near our house located adjacent to Masjid Ghufran in UC-7 Gulberg when one of his friends noticed some heroin addicts in the park and humorously suggested that they may be asked to repair the faulty PMT jumpers,” Shamim, an office worker, told The News on Friday. He said the fault in their area’s PMT had occurred on Tuesday last and they were told by the KESC’s complaint centre that the jumpers in their area (a kind of connecter that joins 11KV power line to the PMT) had been damaged and these would be repaired as soon as staff was available. According to him, the said heroin-addict demanded Rs. 600 from them and a plier for repairing the damaged jumpers. “He (heroin-addict) climbed on the pole without any ladder or wearing any protective gear, fixed the fault, probably by joining the 11KV line directly with the PMT and asked them to check out whether electricity had been restored or not,” he said. Shamim said when he was told that electricity had been restored, the addict who was probably under the influence of heroin climbed down and demanded the money. The boys collected Rs. 20 from each house in two to three lanes of their area where electricity was disconnected and paid the money to the “electrician”. “I came to know about the said event after my brother asked me to give him Rs. 20 as he had to pay to the heroin-addict for his job. I was quite relived over the restoration of electricity but was annoyed at the same time as to why my brother and his friends managed to get the job done at the risk of the life of a person,” he added. When Executive Engineer KESC Muhammad Siddique was asked as to whether it was possible for anyone, other than qualified staff of the KESC, to fix damaged jumpers of PMT, he informed that it was possible but that was highly risky and dangerous job for the person doing so. “An electrician or any other person having some know-how of electricity transmission system can do so but that is extremely dangerous and life-threatening job. Our staff performs the job by taking several precautionary measures to ensure their own safety,” he mentioned. Siddique informed that as per Standard Operating Procedure (SOP), a shutdown was initially carried out in the entire area to protect the lives of linemen and later several other precautionary measures were adopted to ensure safety of the staff. The technician who fixes the problems also uses gloves and other equipment to carry out the job safely,” he added. During investigation for this news story, it transpired that a number of people were adopting the same exercise almost in every locality of the city by hiring private electricians and skilled or semi-skilled workers to fix faults in the electricity transmission system of their areas. Azhar, another resident of F.B Area, informed that last Saturday’s gale-force winds had broken several electricity wires in their neighborhood and despite lodging several complaints with KESC, nobody came to fix the problem and restore the electricity. “We hired an electrician who fixed snapped electricity wires and restored electricity in our area. We paid him after pooling the money from all houses in the area,” he informed. Alamgir, a shopkeeper in the vicinity of Arambagh, told this scribe that they too had hired the services of an electrician to maintain and restore electricity to the market where his shop was located. (By M Waqar Bhatti, The News-13, 30/06/2007) 111