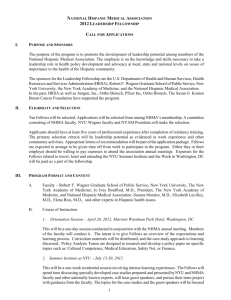
UBIQUS Document - National Hispanic Medical Association
advertisement

NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15th Annual Conference – Health Care Transformation to Expand Prevention and Health Promotion for Hispanic Communities Washington, DC March 18, 2011 Contents A.4. COMMUNITY-BASED PARTICIPATORY RESEARCH AND HISPANI C HEALTH .................................................................................................................... 1 Ubiqus/Nation-Wide Reporting & Convention Coverage 2222 Martin Street Suite 212, Irvine, CA 92612 Phone : 949-477-4972 Fax: 949-553-1302 A.4. Community-based Participatory Research and Hispanic Health [START RECORDING] MALE VOICE: Good afternoon everyone. We’re going to get going. Just so for some logistics if people require CME units please come see me at the end of the workshop. There is a signup sheet for that. My name is - -. I’m a sixth year MD/PhD student from the National - - Latino Medical Student Association. I’m also an NHMA executive board member. Our first speaker up is actually Dr. Vivianne Aponte Rivera. She is the lead psychiatrist and Director of the Hispanic Latino Research Team and Clinic for Depression Study. She completed her medical school and general psychiatric residency at the University of Puerto Rico and her Child and Adolescent Psychiatry Fellowship at Emory University. She’s an Assistant Professor in the Department of Psychiatry and Behavioral Sciences at Emory University School of Medicine in Atlanta, Georgia. Dr. Aponte Rivera is in the board certified child and adolescent psychiatrists, and she is interested in the mental health aspects of immigration and acculturation of the affected children and their families. She is also interested in the impact of cultural differences on the manifestation of psychiatric illness. DR. VIVIANNE APONTE RIVERA: Good afternoon. I’m Vivianne Aponte Rivera, as previously said. I guess I need to click on something here. Is this supposed to be it? Yes. Got it. Basically, I’m going to be talking about how to increase participation of Hispanics within clinical trials and kind of link that a little bit to the topic of community-based participatory research. The objectives of my brief talk would be talk a little bit about the demographics of our clinic. It is a dedicated Spanish speaking clinic for the treatment of Hispanics, and it’s for a depression research clinical trial that we’re conducted at Emory. Besides talking about our patients and our demographics, kind of understand how clinical research studies can help us decrease health disparities, which is one of our main concerns with Hispanic population and minorities overall. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 1 I’ll tell you a little bit about our study. It’s called the Emory PReDICT Study. We like acronyms a lot, so it stands for predicting response and depressions to individual and combined treatment. I’ll tell you a little bit about the study. It’s an NIH funded study. It’s two grants, and it’s a study for major depressive disorder. Our goal is to recruit 600 patients. We already have over 200 patients randomized, but our main goal will be to recruit 600 patients. The purpose of the study is to identify predictors of response to treatment in people who have never been treated before, right? We know we have a lot of treatments in psychiatry and especially for depression that we know they work. We know they’re good. The problem is it’s really hard to figure out what is the best treatment for each patient. Over time, the morbidity and the longer somebody is with depression it has a significant impact in that person’s life. You really want to get them better as quick as possible and avoid those multiple trials of medications until we get the right one. It’s more kind of like this personalized medicine concept. Basically, the first part of the study is a 12 week study. It’s random assignments, so patients are randomized to either medication or therapy. The medications are escitalopram or duloxetine, FDA approved medica tions for depression. We know they work. Cognitive behavioral therapy, which is a type of therapy that is most widely studied. It’s manual-based, manualized so you can do a lot of reliability ratings and adherence, basically, ratings for that. Then, we have an extension study where we can treat people for up to two years after the date of randomization because we do know that depression can be a relapsing illness. Unfortunately, what usually happens is people continue to have episodes over time and the more episodes you have the higher probability of future episodes. That’s one of the parts that I really like about this study, the fact that we’re looking at people two years down the road. It’s very easy to say something was very effective for 12 weeks. What happens two years down the road with that person? That’s sort of like where we’re at. I talked about factors that predict response to treatment. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 2 What are we looking at? What factors are we looking into? I can’t go into a lot of detail about them. I’ll just briefly mention them, but basically we’re looking at a lot of demographic and clinical factors. We gather a lot of information about those patients. We do a lot of self reports and clinician rated evaluations also, very structured rigorous evaluations. We look at brain functioning before, throughout the treatment, and at the end as a factor of prediction of response. We do that through FMRIs. We look at genetics, so we draw their blood and process their blood. We also look at the HPA axis because a lot of work has been done, and the hyperactivity of the HPA axis is part of the etiology for a lot of depression and anxiety symptoms in patients. We also look at immune and inflammatory markers. That is kind of like a new area that has been explored in the last couple of years...well, a little bit more than a couple of years but it has been explored recently about how all these interleukin cytokines, all these substances are related to depression. We look at personality because we do know there are certain personality traits that do predispose for depression. We also look at early life trauma being an important predictor of depression and possibly response to treatment. In our patient population in Georgia it’s mostly recent immigrants, first generation, so there is a lot of trauma history in our patients throughout their immigration process and in their countries of origin. The primary site for this study is located within Emory University in a research clinic that specializes in mood and anxiety studies. It is solely for English speaking patients, so we decided to create Clinica Latina - -. Basically, it’s a satellite research clinic for the Emory study. That’s what I was hired to do to develop this clinic and to run this clinic. We are located within the international medical center at Grady Memorial Hospital, and I’ll tell you a little bit about the center because I think it’s part of the importance of this. It’s very important in the success of our study. Basically, Grady is one of the largest public health hospitals. It’s huge. It’s a tertiary care inner city hospital. It has a lot of components, different satellite NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 3 clinics. It has been around for a very long time in Georgia. Actually, it was a segregated hospital. I’ll say that story. It’s in the shape of an H. It was the white section and the black section, and the corridors were for the nurses and the staff. It has a lot of history to it in terms of talking about health disparities, right? We’re within the international medical center. It’s a health clinic for limited English proficient patients located within Grady, but being Spanish speaking patients, our largest minority group at this time point.... We have African-Americans, but in terms of different other limited English proficient, Spanish speaking would be our main group. All of the staff actually is Spanish speaking and bilingual. Most of the patients seen at that clinic are Spanish speaking. Our clinic is fully bilingual and fully bicultural, and I make a point of that because it has made a difference especially with mental health, the idea that you understand me because we come from a similar place for a lot of our patients. This clinic was fully established 18 months ago. I do have to say it’s a part-time effort. Emory doesn’t do a lot of work with Hispanics, so we’re trying to integrate this type of study to their ongoing research studies. It’s a parttime clinic, so we are only - - two days a week. So far, we’ve had 1295 Hispanic patients call expressing interest in the study. That is a lot of people, especially when you’re doing a depression study. If you were doing diabetes, high blood pressure, or breast cancer you’ll get a lot of people, but depression is kind of one of those things you don’t really talk about within Hispanic culture. We definitely see that there is a need. People want to know about it. People are asking about it. Part of our evaluation...we provide a lot of psychoeducation when they call. We get a lot of calls like well somebody told me I might be depressed. What is that? What is depression? I just feel sad and tired, but it must be because I work a lot. Our screens involve a lot of psychoeducation. In other settings, you have somebody who calls for a study and says I went online and did a ten question screen. I have major depressive disorder. I think I qualify for one of your two FDA approved antidepressants. It’s a very different culture. The people need a lot of psychoeducation during their screening NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 4 process so they can actually make an informed decision about whether they want to participate in the study or not. We’ve tried really hard to network and develop relationships with the limited services we have in Georgia for Spanish speaking patients. In terms o f having a referral, what happens when patients don’t qualify because we do know that for clinical trials a lot of people many times just don’t qualify. We have a lot of requirements and standards. We’ve had so far, and this data is up to February, 146 screens. People have actually showed to our clinic. Once again, it’s two days a week, so that accounts for the number. We’re usually pretty busy. Of those 146, 42 patients have actually been randomized to treatment. We do - - extensive evaluation, basic lab work, EKGs...so they do get some benefit even if they don’t qualify. We might be the first person to tell them I think you might have diabetes. You really need to go to a doctor. These are all the valuable things I see in this clinical trial. Just even if you’re not randomized there is a benefit to it. Our research staff works at the primary English site when they’re not at our clinic. That is a good thing because we’re able to maintain a lot of - - reliability. You have the same people doing the same thing in two sites. Also, it’s a great way to get employment for bachelor’s level by Hispanics. All our staff is actually bicultural, so we’ve been able to provide jobs for these students, too. We do need to have a greater staff to patient ratio. That’s just something you have to understand when you’re working with Hispanics. They need a lot of help navigating the system, understanding it. You want to know that when you’re writing your grant and before you develop your study, right? We worked really hard to incorporate the concept of patient navigators. That has been talked a lot about in a lot of our meetings. Just that person that guides the patient through the system. We can’t tell a patient show up at the MRI building at 9:00 and somebody will do your scan. We really have to tell the person I will meet you here at 9:00. I will walk with you. We’ve even done a contract with a local cab company where they show up to the hospital. We have one staff member who gets in the cab NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 5 with a patient and then they drive to the FMRI because it’s just very complicated, very difficult for them to do. Public transportation is not always great. Many times we have to print out maps, MapQuest, get on bus number X. It leaves at 9:30 and you will be there at 10:00. We have to help them in order to be able to facilitate their participation because they do want to participate. The patients come in. They sign a consent to undergo an initial evaluation, and if they’re eligible they sign our extended consent. We are located within a general medical clinic, which I think has also been very helpful. They don’t go to this mysterious place to do my evaluation. I don’t know. It’s this research study. They actually go to a clinic. They go to a waiting room where there are pregnant women, children, people speaking different languages, and they’re there to get their healthcare. We happen to be in one of those offices. It also adds a little bit to the concept of this is an illness for Hispanics and the fact that you’re not making this up. It wasn’t that you couldn’t handle a situation. It is a real illness. We looked at the questions that came up during our informed consent process with a goal of being able to identify things that could be causing a lot of trouble for the patient in terms of understanding some of the questions. What was difficult for you? Because we really want to use the data we gather from here to make all the changes that we can during the study while adhering to protocol but at the same time be able also to inform future studies about what were the types of doubts and questions and how can we make even better informed consent. There were questions about documentation, legal aspects, and confidentiality, which we sort of expected. There is a lot of concern about what is going to happen. Where is my data going to go? Who are you going to inform? I have a Green Card. I’m working on getting citizenship. How is this going to affect it? That type of concern, right? It was very interesting that they tended to request a lot of further clarification of the protocol and study procedures. I’ve been giving that a lot of thought because people would read something and then they would go okay. They would grab the informed consent and ask you okay so the medicines are X and Y, right? Yes. They are FDA approved, right? NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 6 It almost felt like they needed that personal contact. Here in the US a lot of people are used to just signing documents, and that is even more important - - what people say. I have it written. I need that email so I can certify that you did that. For them, this personal contact was so important. We talked about the fact that yes these are the medications. Yes, these are the side effects. I found myself kind of repeating a lot of the things that were written in the consent. It was only after they heard it from us then they would okay I’m signing. There are also the concerns am I going to be a guinea pig and a lot of concerns about medication side effects. I’ll tell you a little bit about our demographics. What does our clinic look like? In terms of gender, as we know, depression is more prevalent in women. It is kind of like within the expected realm. We have 111 women and 35 males. We looked at the country of origin, too, and it is very consistent with our Hispanic population within Georgia. The majority of our Hispanic population comes from Mexico and mostly Central America. Here we have Mexico, Colombia, that’s the order. We do have quite a bit of Colombia, but they’re the biggest representation from South America. It’s usually Mexico, Colombia, and Guatemala. They go in decreasing order, but it’s a significant difference. Ninety-two of the patients were from Mexico, and then the next category, which would be Colombia, the next Hispanic country there were ten patients. It’s predominantly Mexican, our population. In terms of a little bit more demographic information, their average age is 37, but we went through the whole range. Our study recruits 18 to 65-year-olds. The 66year-old here is because the patient turned 66 during the study. We had the whole range of ages. The average number of years in the US, which I think is very important, too, in terms of considering the population that we had in our study, was 11 years. It was people who had recently came here. Many of them were not born in the US, but it did range from one to 40 years. Their educational level, the majority of them did not finish high school, but in our population we do have people NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 7 even with doctoral degrees, so we were able to capture a more representative population. The marital status, a great majority of them were married, and there were some people cohabitating. We also know that a lot of times couples are separated because one of them is working somewhere else or in another state but they’re still married. There is that stressor, especially for the women, of staying alone with their kids. The number of children because a lot of that is said in terms of depression and the stressors and the number of children you have to take care of...so most of them had children. One...two children is the green one, which is the most number of kids...three, four, but we had patients that had up to nine children. That tends to complicate their ability to have access to medical care. Who is going to take care of the kids so I can come to the appointments? How are we going to make ends meet with nine kids and all of that? I want to talk a little bit about show and retention rates because that is a big concern in trials, right? We get people to come, and once you get them to come how do we get them to stay? We have a lot of baseline data. You don’t have a lot of endpoint data. It’s hard to come to conclusions. Our no show rates for now...it’s really hard to compare the two because the population at the main clinic they’ve been running for two years longer than us and they’ve been running five days a week, so they have been able to recruit more patients, obviously. When we compare the percentages.... Anyway, basically 20% of our patients have not shown for a screening visit versus 28% from the main side. We’ve actually had quite a bit of people show up. People do show up for the study. Our retention rates are a little bit lower, 69. It’s not bad, but we would really want it to be more than that. The main clinic is close to 75%. I mean, we’re very close to them, but we would like our retention rates to be even better. Based on that, we looked at all the reasons for early termination so far with the patients that we have. I do have to say, and going back to the previous slide, in those 18 months basically 20% of the sample is Hispanic. We’ve been able to incorporate a significant amount of Hispanic NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 8 patients to the study versus before this clinic was established it was minimal or next to nothing. Now, 20% of the sample is Hispanic, and we hope to continue increasing it over the next couple of years. Basically, the reasons for early termination in our patients, there was some scheduling conflict. Our patients are the middle column. The main clinic is the column to the right of our 42 randomized and their 163 randomized. There was intolerance to medication. I want to mention intolerance to medication and adverse event. It’s just three patients total among those three, but a lot of times it makes you wonder whether was this termination due to the belief that Hispanics are more somatic and have more significant reactions to illness, or is it that Hispanics do metabolize medicines differently, have more serotonin transporters, and ten milligrams of X medication in them means 30 milligrams rather than blame it on culture or race or things like that, ethnicity. In terms of the study, that’s another important aspect, the fact that we’re looking at genetics, that we’re looking at other data that will help us clarify some of that and will provide significant information about Hispanics that has not been gathered before. My final remarks about this, and you wonder okay so how does all of this fit into communitybased participatory research. I see it as a building block. We don’t have to go around replicating every study. Why can’t we be part of a study and modify it in a way where we still adhere to protocol but we are doing more of a community-based intervention and taking into consideration your population? We’ve proven that you can actually modify a research study while adhering to protocol so that it suits our population. It increases diversity in the study population. I told you - - already mentioned this. We have jobs for Hispanics wanting to go to med school. - - in these 18 months our third...we have two students that are going off to med school, and we have one that was accepted into a psychiatry residency. At least the treatment recommendations that take ethnicity into account not only from a culture and social perspective but also biologically because we’re measuring a lot of biological markers. It leads to more specific and effective interventions. It’s a great way to provide treatment for an underserved population. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 9 Also, what I’ve noticed throughout our study is that we’ve been able really to increase awareness about mental health and depression because we go around promoting our study trying to advertise it. When we go to the radio and we do community shows and the TV we also talk about depression. We demystify this whole depression and mental health thing and try to explain why it is an illness and that there is treatment and there is treatment available for them at no cost through the study and a way to decrease stigma. I know my time is up, but we do have questions at the end I believe, right? Thank you. MALE VOICE: Thank you, Dr. Aponte Rivera. So we’re going to have about a 15 minute question session at the end once we have gotten all the speakers taken care of. Hold onto those questions. Write them. Our next speaker is Dr. Paula Goodwin. She is in the health sciences administrator for the National Institute of Minority Health and Health Disparities at NIMHD. She is primarily responsible for directing the community-based participatory research program, which supports partnerships between academic - research institutes and communities to improve the health of health disparity communities. She completed her doctorate in human development and family studies in 2001 at the University of North Carolina at Greensboro and completed her post-doc fellowship at the University of California LA and the University of North Carolina Chapel Hill. Prior to joining the NIMHD, Dr. Goodwin was a professor in child development and family studies at Purdue University in Indiana. She also worked as a statistician in the Center for Disease Prevention and Control. DR. PAULA GOODWIN: Hi. I’m Paula Goodwin, and I’m from the National Institute on Minority Health and Health Disparities because our acronym is NIMHD. We recently became an institute, so I’m getting used to saying that acronym also. Today, I’m here to talk to you about our initiative in work with communities and how we have a program of community-based participatory research that actually our academic research partners with communities to implement interventions. Also, to talk a little bit about how we specifically with Hispanic Latino populations...some of our CBPR projects that target that specific population. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 10 We were established as a center in 2000 with public law 106525. Part of that law also gave a definition of what health disparity populations were. That defined a health disparity population as a population where there’s a significant disparity in the overall rate of disease incidence, prevalence, morbidity, mortality, or survival rates in the population as compared to the health status of the general population. With that definition, racial and ethnic minority groups including Hispanic and Latino populations were considered health disparities populations. With the passage of the Affordable Care Act in 2010 ten years later we were elevated to an institute, so we’re now the National Institute on minority health and health disparities. With that, we were charged with coordinating health disparities research across the national institutes of health and also supporting research and programs with the goal of reducing health disparities and ultimately eliminating health disparities in the US population. With that in mind, we established programs that had that goal in mind with reducing and eliminating health disparities. We know sort of the traditional research; the traditional approach to research may not be as effective with some of our health disparities communities. That’s why we focused on creating a CBPR, a community-based participatory research program. When we did that, we called upon experts in the field like Dr. Barbara Israel and Dr. Eugene - - and some others as advisors to help us to develop a CBPR program that had the goal...we wanted it to support intervention research. Our CBPR programs, all of our grantees are implementing or are planning to implement interventions to address a disease condition that is of interest to the community. They use the CBPR approach and the principles and methods of CBPR. Again, the goal is to reduce and eliminate health disparities. What’s unique about our program is that, one, we require a partnership, an equal partnership that communities are equal partners in this research grant. We require that there be some partnership that has been developed. Often times, we see where community groups are co-PIs or community groups are key personnel on the research grants. We also require community involvement so that each of our CBPR grants has to have a community NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 11 advisory board. The goal for this, again, is that we want science to be translated and want it to be done in a way that is of meaning to the community and is relevant to the community and also that this is sustained...after the research funding ends that some capacity has been created in the community so that the good that has come from the intervention can be sustained after sort of the academic researchers leave or the funding dries up. With that in mind, our CBPR program is a three phase program. Our first phase is what we call our planning phase. With that phase, it’s three years of support where, again, equal partnership in all phases in all aspects of the research but communities and researchers partner. You have three years to sort of form and really work out the development of those partnerships. There is a community needs assessment done. With input from the community, you identify the disease or condition. The academic researchers are not the ones who say okay we’re going to focus on this particular disease or this particular.... They have to in collaboration with a community partner decide what is the disease or the condition. I can give you an example right now. We have a set of some planning grantees. They start out in writing the grant. They have an idea of what they think the disease or condition may be that they want to focus on, but within these three years and as they develop I get phone calls about the community really took it in a different direction. That’s good to hear because that lets us know that the community is involved and has some say in what’s going to be done and how it’s going to benefit their community. During this three year phase it’s also a time where you really work with your community and plan the methodology for the intervention and also do a pilot intervention. Our next phase is phase II, and that’s what we call our intervention phase. That’s five years of support. Here is where you further define or develop the logic model, the conceptual framework, the research design, and the methodology. You develop evaluation plans. This is the time when you actually...having that planning and solidifying that partnership that you actually have five years to implement the intervention. You do an evaluation study, and then there are plans for dissemination. Again, NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 12 I say this with each phase, at each phase there has to be involvement with the community and you have to have a community partner in these grants. The third phase is a three year phase, and we call this the dissemination phase. These are provided to grantees who have demonstrated effective interventions. This is an opportunity, again, in collaboration with the community disseminate research findings in an effort to improve the health status of underserved populations and eliminate health disparities. Again, in working with the community it’s not always from the academic perspectives about writing research or empirical papers, but the community has an input in what’s the best way that we can disseminate the findings from this research to our communities, to communities like ours. What’s the most effective culturally appropriate way to do that? As you can see, with those three phases...and each one of those phases is a separate competing phase. Just because you received a planning grant, you don’t automatically go to the intervention or the dissemination, but if you’re funded for all three phases that’s 11 years of support in a community working with a community. Again, back to what I said when we decided to sort of develop this program and brought in the experts, we wanted to ensure or to make sure that we had sustainability. That it’s not sort of a drop in for three years in the community and you leave out so that you could actually get funded for 11 years to work collaboratively with communities to implement these interventions. Currently, I can tell you a little bit about our history. Our first planning grant - - started in 2005. We had our second wave of the intervention that started in 2008. Currently, we have 40 intervention grantees that are implementing CBPR products across the country. We were fortunate enough to start a planning phase with ARRA funds, the American Recovery Reinvestment Act funds. Currently, we have six planning grantees. We haven’t yet gone through a full cycle through the dissemination, but our dissemination phase will start in 2013. Afterwards, we will have a full cycle and be able to report on, again, did we reach our goal of eliminating and really building capacity and sustainability in those communities. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 13 NIMHD CBPR grant portfolio. Like I said, Hispanic Latino populations are certainly considered a health disparities population, and our grant portfolio reflects that. Like I said, we have 40 intervention grantees. We have six planning grantees, and of those about a third either exclusively target Hispanic Latino populations or they target Hispanic populations because of the area that they work in that is primarily Hispanic or have a large Hispanic population. We realize and our grants reflect diversity within Hispanic Latino populations, so our grants do reflect that. We have a diversity of target populations when we talk about Hispanic Latino CBPR projects, and just some of the indigenous Mexican farm workers we have a CBPR grant in Oregon that actually works with indigenous Mexican farm workers at nurseries to implement an occupational safety intervention where they’re actually testing for markers of oxidative stress. They actually have an intervention where they have a culturally appropriate...in the indigenous language where they actually do docudramas and also videos and DVDs as opposed to sort of the standard way among nurseries or pesticide workers that you receive a written...something in English that tells about the occupation safety. We have - - grant in Oregon that is actually working with these farm workers to implement a culturally appropriate occupational safety intervention. We have a project in Boston at Tufts University working with Caribbean Latinos. That was one that when I mentioned about the planning, this is a planning grant where originally when the grantees submit it they had some ideas about what issues or diseases they wanted to focus on. When they got there, it wasn’t what they expected. The community said, particularly the young people in the community said, we’re interested in mental health and self esteem and well-being. This particular project, the grantee has youth from middle school and high school that are actually working as researchers on a team...and help developing the intervention. They have a seat at the table, and they’re having a say in the intervention that’s being developed to target their particular population. We have - - populations. We also...a lot of times with CBPR in recruiting, you know, a lot of our grantees have difficulty recruiting males into sort of these behavioral NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 14 interventions. We have a very unique one in North Carolina that targets rural Latino males in HIV prevention and sexual health. It’s unique in an initiative in that they actually go to the soccer leagues, and they recruit men to be sort of the lay health advisors. These males are then the leaders who recruit other team members, and they provide the intervention that way. We work with children. We have a CBPR project in Texas where they actually partner with the Girl Scouts that have a large Hispanic population. They’re working with Girl Scouts and Girl Scouts leaders to implement a physical activity program for overweight and obese Latino adolescents and preadolescents. Again, diversity in terms of the regions in the United States that we focus on, so our projects do reflect the diversity that is within the Hispanic population. We have a number of diseases. Again, these diseases and conditions are collaborative. The community has a say and an input in what is addressed. We have a number...again, from the plenary session and looking at sort of the top diseases and conditions among Hispanics and how Hispanic populations may be overly burdened by particular diseases. Our CBPR projects in the Hispanic populations cover obesity. There are a number that work with physical activity about healthy eating where they have people...lay workers or promoters who go into homes and sort of deliver interventions. Diabetes is one that comes up often that we have a number of programs working with diabetes. HIV and sexual health. The one I mentioned about pesticide exposures. Cardiovascular diseases and then the metabolic syndrome in and of itself. These are just, again, some of the diseases and conditions that are being targeted in Hispanic Latino communities. We have different strategies. Again, the goal and the reason for involving communities is that researchers may bring certain skills. Also, we realize that communities have skills that they can contribute to the research. Part of that is knowing the culture and knowing the people in the community. We want interventions that are developed, that are culturally appropriate, that are effective and that will be adopted by the community. In doing that, a lot of the strategies they’re culturally and linguistically appropriate strategies. They involve community involvement where we have community health workers that are trained, NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 15 people in the community that are trained to educate and carry out interventions and to educate the people that they’re working with. Also, a lot of our grants, like I said, about sustainability and giving something to the community, a lot of them focus on advocacy. We have communities that are working with researchers to advocate for green space, to advocate to their community leaders and politicians for certain things. It’s not just about implementing just an intervention about diabetes, but it’s about building capacity and having sustainability. A lot of our grants do focus on advocacy for community members and how they can sort of get what they need in order to live and lead healthier lives. You can, and I think you’ll have this available to you, but the NIH reporter is a public site. If you want to know more about what are the CBPR programs, and if you want to know who is the PI and how to contact them and what has been published, you can go to NIH Reporter. That’s the website address that will give you more. If you want to know more about our specific programs or about the CBPR program, you can visit our website. You can also contact me. Like I said, I manage the CBPR portfolio at NIMHD, so you’re welcome to contact me if you want to know more about the program or just specifically about some of the programs that we have. Thank you. MALE VOICE: Our last speaker is Sara Tyloski [phonetic]. She has two decades of experience in strategic planning, management, and pharmaceuticals with pharmaceutical and biotech industries. She previously worked both in small and large companies including Intercell USA and GlaxoSmithKline. She provided strategic project planning to launch several new projects focusing on the Hispanic Latino markets...working with advocacy groups for disease awareness campaigns and recruitment. Her passion is working on cross-cultural business goals with particular expertise in helping to accelerate outcomes for product development. She most recently actually organized to spearhead the first ever Hispanic Heritage Conference called - -. Actually, LMSA was invited to this as well as NHMA, so we had about three representatives in that particular conference. They’re going to actually follow up on that. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 16 The conference itself was just focusing on how to reach the Latino community for clinical trials and medical research. Sarah has a BA and an MBA from Florida Atlantic University in Boca Raton, Florida, and travels back and forth between Florida and Mexico. Ms. SARA TYLOSKI: Well, unfortunately, I don’t look like a Latina because my last name is - - Tyloski, so I apologize, per hablo Espanol; yo - - a Mexico. I’m just real curious. I know we only have a few minutes. I think it’s very brave that you guys are hanging in here until 5:00. I’m just real curious. Out of this group here how many of you have been involved in some way in a clinical trial, raise your hand? Have currently or have in the past. So about three. The only reason I was asking is that’s what this whole subject is about. Of course, how do we get you guys more involved? With that, I’ll just get started here. I’m actually representing MMG. They are a full service patient recruitment and retention company, and they basically recruit and retain patients for clinical trial research. Their clients would be people like Emory University. They actually have patients that in NIH studies, people like GlaxoSmithKline...so those that we would be familiar with. That’s their job. Basically, our objectives, it looks hairier than it is. It’s very simple, but what do we know? I think we’ll zip through those slides because I think everybody here knows the basic data about Hispanics and Latinos and their involvement. I would like to share a little bit of a story, a real story about a lady that I met who is in clinical research as a patient. Why are Hispanics and Latinos not involved and how to get involved as a physician? In this group, who has PhDs, MDs, or are on their track? Most everybody...okay so good. I just want to make sure we’re hitting the right target here. What do we know? I’m going to zip through these slides. I think everybody in this group knows this...but background. As you know, in fact, the data has recently been updated. Pew Hispanic Research says that there are now 51 million Hispanics and Latinos in the US, so it’s even probably a little bumping closer to this at 16%. Hispanics and Latinos are the dominant force in the US in terms of impact and influence. I thought it was interesting that the youngest demographic NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 17 group has a median age of 27.4, so it’s a younger population that’s growing in the US. I think everybody knows that here. It’s growing quickly. Probably the biggest thing is that the Hispanics are growing quickly. By 2050 that’s important for clinical research because it takes time to get something to market. The average medication to market is ten to 15 years, eight to ten billion. We’re way behind already. I think the other thing that’s important is that okay who is Hispanic in this room? Raise your hand, if your origin, that is. Everybody? I’m the only one that’s not and you and Dr. Goodwin. I also think it’s interesting the second generation dominates growth. You’re the representation right here, right? That’s people who have been here already for a bit. That’s the big growth group. I know everybody knows this, but just to touch on the fact that if you’re not in California and Texas in the clinical research world you’ve missed the boat. Everybody knows that, right? Interestingly enough, in fact, there was some new data I was just reading the other day. There are some states like Ohio and Idaho and Alabama...they’re really coming up in those areas. I think Alabama had the largest increase in Hispanic growth, so these are great opportunities. I mean, there are 16 states with at least half a million Hispanic Latino residents, so that’s pretty significant. Then, I think the other thing that’s important in terms of clinical research, I think you touched on it a little bit, is what is the economics of Hispanics and Latinos participating in trials specifically? There are a lot of challenges in the United States. This is, again, on census data. You may or may not know this; you probably do, but one in four US Hispanics live in poverty. That definitely affects both the elderly and the younger folks. A lot of Hispanics hold down more than one job, so that makes it difficult for them to get to a trial, as you know. Then, again, the vulnerability is the children and the elderly and then, again, caring for it, as you alluded to in your presentation. That’s a big challenge. Even though the Hispanics and Latinos as a group are a large part of the US population obviously under-represented in trials, there’s actually not even a lot of data out NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 18 there if you go out and look for the data. This is just some summary. In 1995 to 1999 we found only three percent of Hispanics and Latinos were in trials as participants/patients. Then, there is another data point, 3.1. There is some data that shows the National Cancer Institute funded trials it was around 5.6. Even as of 2009, minorities participating in clinical trials have remained lower. We all know that, but if you make that comparison of three to five percent participation versus 16-ish of the population demographics we’ve got a long way to go in a short period of time. Then, this is just an example. Even in something like COPD, which we don’t think about because of that second generation growth. Yet, if you look at the...is it because we haven’t had good diagnoses - - the COPD patient well. Why are they not in trials? We don’t really know. There’s just not that much data out there. I threw this in there because a lot of COPD patients go to the emergency room. They haven’t even probably thought about a trial. They’re usually getting treatment first. Mexican Americans seem to have similar severities of COPD, but we just don’t know that much. That’s the bottom line. We just need to have more people in trials. What does this mean? What it means is that the industry is behind. I think NIH is to be commended for these projects. It’s very exciting what they’re doing at Emory University, but industry, meaning the GlaxoSmithKlines of the world and the Pfizers of the world need to step up. That’s what I’m trying to do with companies like MMG. I’ve talked to physicians. A lot of you are either to be or are physicians. You haven’t seen data on Hispanics and Latinos, right? It’s not out there. Are you comfortable...anybody a practicing physician yet? Do you feel comfortable prescribing....? Here’s a new drug out there that has never been studied in the Latino market. It makes you feel uncomfortable, right? There you go. Of course, I think you know that the FDA is encouraging based on - - data that we do, in fact, try and reach out to these categories of ethnic and race. Therefore, we need more options. Bottom line. We all know this. This is nothing new, but I wanted to share with - - had a chance to meet my friend Gabriella. I’m just going to give you the summary. I met Gabriella at NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 19 the Clinica del Pueblo right here in Washington DC. She’s a 45-year-old Latina who developed HIV from her husband from an extramarital relationship in 1994, and through her husband she also got HIV and passed it on to her daughter. Both her husband and her daughter died within two years of full blown AIDS. It was very sad. In that time period, Gabriella really suffered with anger, depression, frustration, confusion, and of course her own health suffered because she had HIV and was doing nothing about it because her husband and her daughter were dying of AIDS. She ended up having to give up her two sons for adoption, so you can imagine her situation was pretty dire. The thing is that’s not so uncommon. I’m sure all of you have touched lives of people who have had something handed off to them in some way and they didn’t know what to do about it. She went to Clinica del Pueblo, and through an advocacy program that MMG has learned about the opportunity to be in clinical trials. I guess I should say it was pretty severe. We were all crying in that room that day. She ended up in the ER due to complications of tuberculosis - herpes, mouth infections, and eventually had hepatitis C and Parkinson’s, so she was in really bad shape. After five years of psychological therapy - - I was mentioning, she did find out about this program that MMG has. It’s in cooperation with NIH to just basically say hey there’s an opportunity to join a trial. What does that mean? What does that mean to you? She was able to join a trial in 2000 and has been in these studies ever since. Fifteen years later, Gabriella has now started her own group that is basically an advocacy group for Latina woman. I think it’s called Latinas Unida...I forgot what the other one or two were. I wrote it down. I think nuevo. Anyway, the idea was she got together a group of women. They meet every month. It’s growing. There are about 20 women in a group. She is based out of DC, and she said that really her sickness was one of the best things that ever happened to her because through this whole process she has been able to reach out and mentor other younger women to get diagnosed early, to get treatment, to learn about what their health conditions are. The other thing that’s kind of nice is one of her sons that was sent off to adoption is now living with her, taking care of her, and she just hopes NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 20 that we’re going to be able to reach out to more Hispanics and Latinos from her perspective. I think we’ve already moved beyond that with some of these trials that are starting to take place, but we know that we need to do something about it, right? That’s where we’re at. So why are Hispanics and Latinos not involved in clinical research? I think we’ve seen some of the answers. Recently in February we just had a conference called Todos Juntos por la Salud that I helped put together with MMG. Alvaro came. Dr. Elena Rios came. A lot of people were actually at this meeting as the leadership came. What we wanted to find out is what is going on and what can we do instead of just talking about it. What else? What other kinds of initiatives can happen from this? Basically, it was a very short half a day session just to bring leaders together at this point. I think these are things that you guys would all say yeah that’s true, but these are the key issues that we came up with. One of the big ones that we talked about is the lack of a clear message. I know that you probably experience this. People just don’t know what clinical trials are. What does that mean? We’ve got the Tuskegee experience. We’ve got the experience of Guatemala, so it has got a bad rap. It has got a bad name. It certainly has a bad name in the minority community. We have to figure out what is the message. Why are we even having clinical research? We all know why, because we’re in the medical field, but an average patient doesn’t know. Then, of course, there’s a big mistrust in general, especially by Hispanics and Latinos based on their country of origin. White people like me except I’m culturally competent, but white people really don’t get it. They don’t realize that they need more staff...that you need to hug somebody when they come in the front door. Those Latino things that we all know, that language and culture is very important at all levels, and that relationship is key. There is that mistrust. Then, what is the awareness on the patient, physician, community, access to research, access to funding, access to care? A lot of times people end up in the ER because they don’t know where to go. We know the whole lack of insurance story. Then, part of that is lack of training. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 21 Even here at this level I’ve talked to Alvaro. We’re working with the Latino Medical Student Association to create a cultural competency training that could be standard for all people in research. That’s what we need, the nurses straight on from when you walk in the front door right on through the PI right on out the door. I was thinking of a quick story that one of our participants was telling us about a nurse who was in clinical research, and there was a Latino patient who had come in. The nurse said hey you don’t want to be in this study. It’s too much work. Had we trained this nurse about the benefits of research that it’s going to benefit this patient and it’s going to benefit future generations maybe that wouldn’t have happened. Training, would you guys not agree, is a big issue in terms of just overall....? From this conference, actually you guys are the first audience to see the preview of the findings we’ve put together. Again, nothing we don’t know, but we do need to define the story. We’ve created sort of a phase. Phase I is what is the story about clinical research. What does that mean? So talk about...I don’t know. Has anybody heard of the organization called - -? It’s a non-profit, so it’s kind of a small company. They put together educational videos, and they walk you through in language, culturally appropriate, very well done. They have music in Spanish, and it - - a church because the spiritual world is very important in this community. Anyway, it walks you through phase I through IV. What does that mean? A patient can relate to it. These are some of the tools we’re talking about. Discuss stigmas. Use real people. We’ve got lots of people out there in the media who have had certain diseases. Let’s use them. Create access tools like community-based organization ambassadors and online media to disseminate. I was just talking to Alvaro today about the fact that if we can have people, residents for example, coming out of MD program or PhD program you have access to those people. Let’s educate the patient so they understand what those opportunities are when you’re seeing them in that emergency setting at Emory University. Okay, oh we have this asthma study. It becomes our job to educate the patient first so that we can increase participation on the other side. There are the tools. Then, share the benefits of being in NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 22 research, which we talked about the support groups that are out there. That’s phase I. Then, of course, I think everybody knows - identify these groups. It’s eve rybody. It’s basically everybody that’s involved in research in some way. It’s the pharmas and the biotechs. I mean, I think they’re big time guilty personally because I don’t represent any of them so I can say that. Let’s face it; it’s very difficult to get these pharmaceutical companies and biotech companies to recognize the need. I think the census data has really opened up the eyes in the industry. It’s what I’ve seen. PIs, principle investigators, community doctors...those doctors that are out there in the community we need a referring way to get these patients into trials that’s trustworthy. Is that not true? - lots of yes’s there. Even people like Wal-Mart. I have a friend that’s in research at SMU, and she works actually with Walgreens in a very informal way. They do health fairs, and they go out into the community and they just educate what’s going on. Those kinds of low key things - possible grant, I think. Then, so we have to do the education as we’ve talked about this already. Then, I think the other big one is cultural competency training, which we talked about. What does that mean? Put it in simple language. It can’t be in some college level language for a patient. A lot of these patients, as you mentioned, they don’t have a high school education. They need it in simple. I like the docudrama idea. Keep it in a very simple format that a patient who is going to benefit from a trial is going to understand. Then, bring that all together, the phase IV. What does that mean from out Todos Juntos projects? What are the relationships that we have been able to create? Then, what are the tangible things that are going to be out in the marketplace? What projects that are clinical research are going to help bring those new medications to market so that the Hispanic Latino community can benefit and doctors feel comfortable prescribing those medicines that can really make a difference. There are a lot of new diabetic drugs coming out there. I don’t see a whole lot of Hispanics necessarily being studied consciously as part of that. NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 23 So this is something you guys know, but this is just an example of cultural competency. A grandmother from Puerto Rico in New York versus a single man living in rural Texas versus a second generation Cuban student living in Miami is completely different. The white folks don’t understand that necessarily, but I think it’s coming, poco a poco. Then, of course, it’s beyond Spanish. It’s not always the language. It’s also the culture. In fact, most second generation Hispanic Latinos English is their first language. I think everybody knows this. It’s more let’s tell the other people about it. That is let’s connect through food, traditions, and then there was an interesting campaign. I think it was the Susan B. - campaign. They had a Facebook project where they...but they had bras on Facebook and they got people to sign up quick. They appealed culturally to the various groups. Give us something to do, right? Then, I’ve got a little video. Create a message with maybe a little bit of Spanish in there, but it’s really eye catching that makes sense. It’s culturally appropriate. I’m going to show you quick. This is a Spanish language on a VW ad that was viewed about a year ago. So did that resonate with some of you? Yes. Come on, liven up. It’s the end of the day. The point is it doesn’t have to be obvious. It could be just a couple words and there you go. Where was I? I’m almost done guys. What does that mean for you all that are in the research world or PhD or practicing doctors? How can you get involved in research? As PhDs or MDs is anybody involved in research in the room? You are, okay. Would anybody like to be involved in clinical research? Good deal. We got a couple there. You probably know all this. I mean, you probably do know all this, but this is just some basic overviews. I think probably Dr. Vivian Aponte...talk to her. She obviously knows everything about that, but I think this is a really key part. How do you become a principal investigator or subPI for that matter? These are just the basic steps. Obviously, you’ve got to know the regulations and have your site inspected. I like what Emory University is doing where they have a subsite to the university. You’ve got to get your IRB approval, sign a contract, and prepare a visit. I know this is very simple. I know. I’m giving you the very basics. You definitely...I hope you will NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 24 comment on this and build your network. Probably number six is where you have to start, like who is your network first, right? Where are you going and - - relationships? Anyway, I don’t know if you’ve seen this or not. We really weren’t sure what the audience was, but you have to know the regulations. Obviously, who has done GCP here in this group, anybody? So there you go. Well, good clinical practices are just basically international quality and standards for being in clinical research. It goes through a whole compliance...many of the resources are available online. I’ve gone through it. It’s not difficult, but it’s based on providing public assurance that the rights and the safety of the patients are being looked after. It came out of Helsinki. That was a really one second version. Then also, there are a whole set of codes that go along with that, which as you know are quite complicated. That’s basically about how to provide the information to the sponsor of the drug or the university in that process. There are a whole set of regulations that go with that. Part of it is you have to have a site. For community-based physicians, more likely you’ll be referring to a site that’s existing. As Dr. Vivian Aponte...I think this idea of having a subgroup out of a university I bet you could probably get a grant through the NIH and do that. Here we got the nice partnering going on, but you do need to have that site and then, of course, have it inspected. It’s a big long process, but if you have a sponsor who is interested and you have access to Hispanic patients, you probably have a good shot at getting that process going. The IRB is just basically a review board that overviews all your information as far as recruitment, retention, all the information you’re going to provide the patient they have to approve that. The IRB board can be a combination of lots of people, usually academic people, government people, sponsor people...it’s a large group of people, and there are companies that do that. I’m giving the very short version, right? You guys can answer those questions better. Then, you have to sign a contract, which is very important to get proper...because - - talk about your responsibility as a physician, a sponsor’s responsibility, NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 25 when the data is going to be provided, what does it look like, statement of work, what does the followup model look like, how are you being paid per patient per visit per all that? It’s quite complicated, so you probably need a lawyer for that. Then, in the perfect world, all sites have a visit to inspect that you have all the various qualifications that are needed, which are fairly complicated in the study world. The purpose is just to make sure that everything is according to the plan that you’ve put out for the sponsor in order for you to enroll patients and follow the right procedures. For example, you may have to have a refrigerator, and it depends on the study, at a certain temperature. You may have to have a drug room that’s separate from your other drug room. It’s quite complicated. Again, I think for community-based physicians referring to or grouping together as a group in a subarea like with a university...I know Alvaro is involved at the University of California Irvine. I think that’s where there are opportunities that I see that would work for the community-based physicians. Then, I think this is probably the first place to start. Who are your contacts? Who are your people that you want to do a study with? There is a great website that you probably do or do not know about, clinicaltrials.gov. Right now there are about 20 trials that either have happened, are happening, or are going to happen specifically for Hispanics and Latinos. I think Emory...I think your trial is listed there, as a matter of fact, with Emory University, yes? I think it is. GlaxoSmithKline has trials. There is this huge diabetic awareness trial going on, so this might be an opportunity for you to say okay you can go find out what company, who is the contact person, and as a community-based physician or person in research build those relationships. That’s it. The summary is we know Hispanics and Latinos are a very important population. They have a lot of unmet needs. There are unique barriers. We need appropriate outreach and, of course, we hope to help. We’ll save all the comments and questions for the end. Thank you for your time. Gracias por - - tiempo. MALE VOICE: So now I guess we’ll take any questions. Is the NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 26 microphone set up over there? If anyone has a question, just go up to the mic please so that way everybody can hear you. Then, I’ll ask the same of the speakers, whoever the question is referred to. FEMALE VOICE: My question is so we get Latinos into a study, we find a drug. It’s a great drug. It works. Then, they charge five billion dollars for it and they can’t afford it any longer. Now we’ve helped them for like two years, three years, maybe five years. What about the next ten to 15 years when they can’t afford the drug anyways or neither can any of their counterparts, so what’s the use? FEMALE VOICE: I mean that’s a good question. That’s a situation I struggle with. I struggle with my research with even more basic questions. During the screen visit I had a very high blood sugar. The patient doesn’t have insurance. What do I do? I get this lab work and say you have to go to a primary care that they don’t have or they don’t have the money to see. That’s where you have to team up with a lot of agencies in the community. There are physicians. That’s where you also have to become an advocate. There are patient assistance programs where you can try to get them enrolled. You don’t always need a brand medication. A lot of studies are done with medications that don’t have generics available, but there are still some old medicines that do work, too. It depends on your study. It depends if you’re doing a pharma...it’s a clinical drug trial, sometimes they’ll work with a patient to try to figure out what’s the best way to continue the patient on the medication if that’s the only medication that worked. It is very relative, and it’s a concerning topic. At least for us, the two medicines we use in our trial neither has a generic. They’re quite expensive out of pocket, and when people leave the trial or they can’t come to visit us anymore we do work to try to get them.... We usually see them up to three months after the trial. I can continue to treat them. We don’t charge them for doing that. We make sure that they transition to another mental health place within Atlanta where we’re located. I sometimes write prescriptions for them for something as similar as possible. I don’t want to get into all the NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 27 details, but in the study if we’re using escitalopram I can write a prescription for escitalopram. It’s generic. It’s four dollars at the local pharmacy. At least we do some of that. I think it’s a little harder when you’re doing investigational drug studies and new drug studies and that’s the only medicine the patient responded to. We have to abide by all the ethical principles, and we can’t leave a patient unattended because they stop participating in the trial. They need to have services. They need to be transitioned out. At least in our study design, we do take care of that. [inaudible] FEMALE VOICE: He just asked like six months - - how many people - - drug. Actually, we’ve been very surprised. A lot of people said it wasn’t going to work. A lot of people told me that Hispanics are not going to come and that it’s not going to work. It’s working. They’re coming. We just had our first group of patients complete their 18 month visit. Many of them are still on the medicine. Some of them don’t want to stop taking the medicine because they’re feeling so much better, and we’re negotiating about that. Our study is more kind of like naturalistic in nature, so it’s not like you get a medicine for six months and then you stop it. We talk to the patient after a year of treatment and say most studies recommend at least a year of treatment. What would you want to do? Provide education, and if they say I want to continue on the med they do. If they don’t, they don’t. We still follow them because we really want to know what happens down the line with a patient. We’re trying to recreate what would happen in a clinical scenario, so we actually have real live data about relapse and sustained remission and all of these things. Most of the patients are still taking the medicine after a year. It’s an antidepressant. A lot of Hispanics initially were uncomfortable with it, but they find it very helpful. Then, they want to refer other family members. Are there any other...? FEMALE VOICE: I just wanted to make one point. That’s why with our CBPR and with a lot of our grantees - - I talked about advocacy and policy and bridging that. Beyond just the science part but also empowering communities to be NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 28 advocates so that what your question is...after you’re in the science and the science is completed, what next? But leaving something behind in the community so they can advocate and they can help shape policies to get some of those things on the table. Really bridging those two things. FEMALE VOICE: I just want to add a comment that I think those of you that are going in or in Hispanic Latino research or you’re MDs in practice. I don’t think you realize...well maybe you do, but you’re very valuable to research. I think one of the points that I would say if I was a doctor in research today in Hispanic and I had a relationship with a sponsor, I would say what’s going to happen at the end of this study. Can you make drug available through your patient assistance program to my patients? I would demand it. I think that’s something that’s in the planning stages of the protocol that’s missing that pharmas and biotechs are not thinking about. It’s not that they don’t care. They’re not thinking about it. Let’s also recognize that it does take ten to 15 years to bring a drug to trial and ten million dollars and all those things. Obviously, when they bring a drug to market they’ve got to make their money back. At the same time, I know in Brazil they’re doing a program now where it’s a five year extension for those patients...I forget. It was some complicated disease. The point is you have the power as a Hispanic Latino physician to demand that if you’re going to be in a trial because, believe me, you guys are the market. There are pharma companies and biotechs that are dying to get Hispanic doctors into trials. That’s a reality. You need to demand what your plan is, what you see is important, because you’re the one that has a relationship with the patient. Thank you. MR. OLLIE THOMAS: Thank you very much. Ollie Thomas [phonetic]. I’m an internist based in Seattle, and I’m doing a one year fellowship - - at Harvard. I had a question for Dr. Aponte Rivera about the implication of your study. I’m concerned because I really quite appreciate the way you set it up and the qualitative outcomes, but I’m concerned about some of the quantitative implications in terms of what does it mean when you have these differences in treatment dosages if you look at Latino versus majority patients. Just to back up a step, NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 29 I’m an internist. One of the big controversies when I was finishing medical school in 2002 was about the treatment of African-American hypertensive patients. I think there is actually a significant misinterpretation of the literature for treating African-Americans, which has actually increased disparities because it has caused many people to underuse ACE inhibitors for African-Americans who actually have indications. This is the core of what I’m actually going to drive at. I think a very central challenge for research is that we still tend to read biology into race and ethnicity when race and ethnicity aren’t biological. I was really influenced by a talk at Harvard by Dr. - Batista, who founded the UCLA Center for Latino - -. He raises this question because there just aren’t discrete genetic bundles that correlate with phenotype. He pointed out...he looked at the first 41 families that founded Los Angeles. How would you characterize them biologically? You can’t because most of them were interracial couples. If we start to see these outcomes by race and ethnicity, my fear is that we have as Americans always interpreted that as biological as opposed to social and cultural. I’m seeing that we still continue to do this - - the NIH. I think that there’s still the potential for NIH funded research to do that not because of the research being not well done or executed but simply because of how we’re interpreting the findings of the research. DR. APONTE RIVERA: That’s an excellent question that has been brought up many times and is one of the struggles that we do have sometimes. I am a Latina. All the other investigators are Caucasian American, mostly males. It has even been a challenge for a lot of people to understand that Hispanics come from...what you call Hispanic it’s 23 different countries in various continents. I find a lot of value in what we’re doing because we’re going to look at genetics. Maybe that’s what’s going to happen. Our outcomes are going to be...you know what, all these people are Hispanics and they have nothing in common. I think a lot of people confuse and there is...a lot of people use interchangeably ethnicity and race. Those are two very different concepts, NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 30 and we’re piling people from 23 different countries and saying these are the medicines that work for them. We’re on our way. I see this as a step to get there, and we’re going to gather data to say just saying everybody who speaks Spanish comes to the study and you’re one population is not accurate. I think it’s displayed in one of the previous slides where it was how does this Hispanic in this place versus this other Hispanic and these other Hispanics identify. With us, it has been very interesting...where we do our intake packets we ask people about what is their race. We use the ones that have been identified by NIH and NIMH, and they don’t know what to answer. The write other, and then they write Hispanic again because...I don’t know. I think this is going to be very good data for biological scientists to see that we cannot pile groups together. What I was talking about transporters would be we’d be more specific. What if certain groups of people...? It doesn’t necessarily have to be Hispanics, and maybe it sounded like that. If we measure the amount of serotonin transporters and 15 years down the road we can do, well, a very basic blood test and say you’re the person that needs a very low dose of the medication versus you’re the type of person that needs a much higher dose of a medication. I think that’s where it’s going in terms of the personalized medicine. MALE VOICE: I’ll ask a quick followup. Are you also doing any qualitative followups of the very interesting finding that patients needed to have information repeated multiple times because I think that’s an interesting cultural— DR. APONTE RIVERA: sorry. They needed to have what repeated? I’m MALE VOICE: They wanted to have information repeated. Like they wanted to get information from you as opposed to from the piece of paper...because I sometimes sense that in my African-American patients. I just wonder if there is going to be some qualitative study that might follow that up. DR. APONTE RIVERA: Well, we initially started...what we’ve been doing with our trial, actually, I see a little bit of this link with a community-based participatory research is every consent form that is signed has a cover sheet that we’ve developed where every single question that the patient has NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 31 is written and the answer that we’ve given to them. That’s where I got those common themes about the question. It wasn’t like what were my thoughts about what people asked. I actually sat down with hundreds of questions and tried to find themes. I was hoping to find more themes than those because the ones were kind of like the expected ones. We were hoping to see other things. The fact that a lot of people are asking for the verbal...it’s kind of like a verbal consent means more for them than the written consent has been my clinical experience - - talk to the doctor. You’re the doctor, oh and you’re Hispanic, okay so I’m trusting you to make this.... For me sometimes I’ve had patients come up and they say no, no, no. It’s cultural. You are the doctor. If you say I should be in this study then I’ll be in this study. I’m like no, no, no. I want you to understand what this study is about, and then you tell me if you want to be in this study. God put you here for a reason. I’m like well thank you for trusting me, but I need you to understand what the study is about. I won’t enroll you in the study until you do. That is my responsibility rather than just trying to grab patients and get them into a clinical trial. MALE VOICE: A real quick question. - - third year medical student at Drexel in Philadelphia. This question is largely to Dr. Aponte. First of all, thank you to all the presenters here. Dr. Aponte, it seems to me that you’re really a pioneer in - - your own little part in it doing this research in Latinos to a bigger study. I congratulate you for that. My question is what barriers did you find or what barriers did you yourself have to go over and obstacles moved through in order to do this study as part of a larger study professionally in the institution. Can you speak to something that...? DR. APONTE RIVERA: I’m glad that we have medical students here, and I do want to tell you that I was trained clinically. It was clinical training, and as I got involved with other things at Emory over time I realized that I just couldn’t remain quiet. They’re doing all these clinical trials. All this data is coming out. This is what works for this patient. This is what we’re doing, and I’m like but you’re not getting it. The whole thing like all of them are NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 32 Hispanic. They came up with this idea to do the clinic, and I agreed to do it. They hired me to do it, but I was raising all these concerns. I couldn’t believe it. I was at this big meeting. You asked about barriers. I am a young woman, Hispanic; I fit like all the minority categories in many ways. I wasn’t born here. I was raised in a Spanish speaking country. I’ve only been here four years. You don’t know anything about the US...things like that. But it was very interesting for me that they said why are you so concerned about this - -. You go down there, do the same thing you’re doing here in English, but we translate the papers. I was told things like why are you so concerned about getting fully bilingual and bicultural staff members. Why don’t we just buy Rosetta Stone and we train our research interviewers with Rosetta Stone and then they’ll be able to do these interviews. I mean, there has been a lot of...it’s just lack of knowledge. I used to get offended by it, but they don’t know and that is our role to advocate even within PI meetings and research meetings. There have been a lot of challenges, but I do want to encourage all the medical students to do this. You have power. I mean, if in 18 months two days a week we’ve been able to recruit 20% of a clinical sample population. I mean, there’s a lot that can be done. They need you. You are the Hispanic expert, and don’t let them tell you otherwise. You can do it. You can develop a small clinic, and it’s a great way to get involved in research. You’re protected by these people that are the big researchers. You’re trying to develop your career, and that’s kind of like a way to get going within a major institution. MALE VOICE: I just have a comment and a question. One, I guess the question that was asked that was actually my question for my poster downstairs, which was socioeconomic factors playing a role in cardiovascular disease modified by race and ethnicity because often times they are confused. You can say you’re controlling for socioeconomic factors, and then you say that being Latino puts you at a higher risk for cardiovascular disease. Then, is it really the race or ethnicity, or is it the fact there are environmental stress factors living in a neighborhood with a lot of gangs and a lot of violence. It’s very difficult to control for those NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 33 factors, but my poster touches on some of those things. could be interesting to some of you interested in that topic. It My other question is there have been a lot of interesting articles being published involving community participatory research. A couple of years ago there was the Two Feathers paper that came out speaking about promotores as an intervention that was successful in treating diabetes. Recently, about two months ago I think, in the Annals of Internal Medicine there was a very interesting paper that talked about the use of DVDs where patients watched a DVD which was made by somebody in their neighborhood showing them how to take blood pressure medications regularly and in a certain way. These people watched the DVD. That was the intervention, and then their blood pressure was reduced an equal amount as the blood pressure medicines themselves. It showed how that intervention was done. This was done in a black population in the South. I was actually interested in reproducing it in a Latino population, which would obviously be different due to culture and language. I guess my question to you, just a basic question on what type of funding is there available to somebody who would want to do a project like that. This question goes out to anybody. [crosstalk] DR. GOODWIN: Certainly, our institute with the CBPR program that I talked about, that’s what we fund. We have a number of grantees that actually take sort of established interventions and actually work with communities to adopt them to that specific population. There is funding. Like I said, we have planning intervention and dissemination funds. Currently, we don’t have any CBPR - - funding calls at the moment, but certainly we have other funding mechanisms within our institute that would fund research because our goal is to reduce and ultimately eliminate health disparities. We target health disparities population and creating research and interventions to address that. Our institute is an institute...you should definitely visit the website and give us a call and know what funding opportunities are NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 34 available to support that type of research. FEMALE VOICE: Because I’m representing MMG, they’re out here in the exhibit hall area. They are taking names if you will of Hispanic Latino doctors who are interested in being in a database for those exact things because their clients are the pharma and biotechs. If there is something down the pipeline that makes sense to match up, then that’s something that could come together in terms of communitybased as well as education as well as drug development kind of thing, if that helps. MALE VOICE: Now, we’re just going to take one more question and then wrap it up. MS. KIMBERLY NORIAN: Hi. I’m Kimberly Norian [phonetic]. I’m also trained in internal medicine and am one of the health policy fellows - -. Just saying in this vein looking at the social determinants of health, this question is for Dr. Goodwin. I’m wondering how much of the portfolio of your grantees for the CBPR actually do address either environmental or social factors as a means of promoting health equity, or what other avenues are there to do that? DR. GOODWIN: I specifically spoke about our CBPR program, but you mentioned social determinants. This year, last year in 2010 we actually funded R01s, which are sort of the traditional...that actually were focused on the social determinants in health disparities. Our institute certainly realizes the importance of social determinants of health and what role that plays in health disparities. We actually had a specific request for applications to actually study the role of social determinants in health disparities. Many of our CBPR grants because they’re sort of based at the community level do consider the environment and what those influence and those structural influences and address that, like I say, through advocacy and through capacity building. We very much recognize that it’s not all biological. I think that’s what makes our institute unique at the National Institute of Health because we do recognize the social aspect. FEMALE VOICE: I also just want to let you know that there are a lot of different funding opportunities. You just have to go online. I feel like I work for NIH...NIMH now here. I NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 35 mean, there is a big section of pharma that are separate types of clinical trials you can work with. They’re very structured. They’ll give you manuals. They’ll guide you by the hand. I mean, they’re very structured. If you want to go - - NIH...well, we do a lot of mental health - -, but NIH route there are...you can go on the website. There is like a kiosk. You can put like your information and - figure out what would be the best grant for you. You also need to take into consideration that the Hispanic population is increasing, so you can either go through the health disparities route or you can actually go through just the main NIH grants and just say that you want to study a - - population of Hispanics. There also are a lot of K awards. I don’t know how many of you know about K awards, but that is an award that is designed to get you involved in clinical trials and actually it pays part of your salary. Mentorship is a big portion of that award, so that could be a potential place to start. A lot of just general NIH programs are interested in information about Hispanics, so there are a lot of ways to go around it. That doesn’t necessarily have to be...if for some reason there is no funding right now through - - health disparities you can go through another route, but there are a lot of routes and ways to do this. Or join a big study and kind of carve out your little piece and move that way. [crosstalk] FEMALE VOICE: Maybe for the next conference you should have NIH or funding, so that people know because, like you said, you can actually sign up on NIH in the Office of Extramural Research. If you email me, I’ll send you that where you can get every Friday funding opportunities like what funding opportunities. We have 27 institutes and centers at NIH and 24 of them fund. I just represent one, but we also have different institutes that have funding available to address health disparities. Like I said, we coordinate health disparities research at NIH so all our institutes and centers address that. FEMALE VOICE: What was your email address? write it down. MALE VOICE: We’re just going to wrap. We weren’t able to Now, I just want to NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 36 thank the speakers on behalf of NHMA. One more thing before we go is if anyone needs to sign up for CME units you have to come to the front to get the signature. Thank you guys very much. [END RECORDING] NHMA – NATIONAL HISPANIC MEDICAL ASSOCIATION NHMA – 15 t h Annual Conference March 18, 2011 37