36k doc - UCLA.edu
advertisement
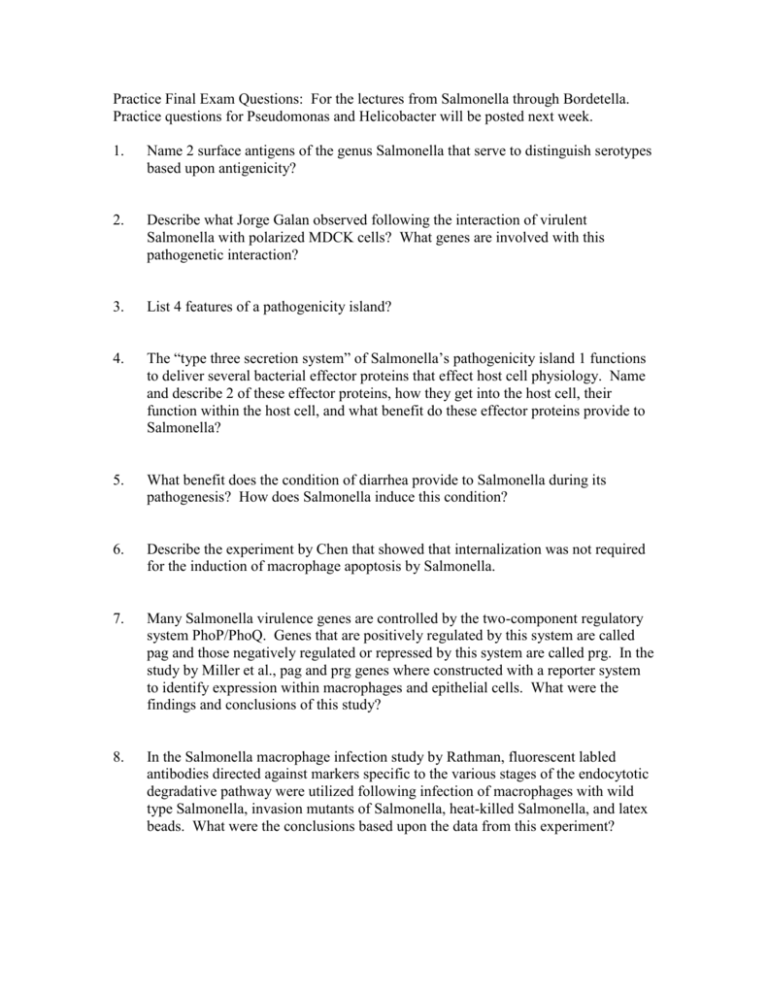
Practice Final Exam Questions: For the lectures from Salmonella through Bordetella. Practice questions for Pseudomonas and Helicobacter will be posted next week. 1. Name 2 surface antigens of the genus Salmonella that serve to distinguish serotypes based upon antigenicity? 2. Describe what Jorge Galan observed following the interaction of virulent Salmonella with polarized MDCK cells? What genes are involved with this pathogenetic interaction? 3. List 4 features of a pathogenicity island? 4. The “type three secretion system” of Salmonella’s pathogenicity island 1 functions to deliver several bacterial effector proteins that effect host cell physiology. Name and describe 2 of these effector proteins, how they get into the host cell, their function within the host cell, and what benefit do these effector proteins provide to Salmonella? 5. What benefit does the condition of diarrhea provide to Salmonella during its pathogenesis? How does Salmonella induce this condition? 6. Describe the experiment by Chen that showed that internalization was not required for the induction of macrophage apoptosis by Salmonella. 7. Many Salmonella virulence genes are controlled by the two-component regulatory system PhoP/PhoQ. Genes that are positively regulated by this system are called pag and those negatively regulated or repressed by this system are called prg. In the study by Miller et al., pag and prg genes where constructed with a reporter system to identify expression within macrophages and epithelial cells. What were the findings and conclusions of this study? 8. In the Salmonella macrophage infection study by Rathman, fluorescent labled antibodies directed against markers specific to the various stages of the endocytotic degradative pathway were utilized following infection of macrophages with wild type Salmonella, invasion mutants of Salmonella, heat-killed Salmonella, and latex beads. What were the conclusions based upon the data from this experiment? 9. In the above question #8, what role does Salmonella pathogenicity island 2 play in this mechanism? 10. What unique cell wall associated feature does Listeria monocytogenes possess that is not found associated with the cell walls of other gram positive bacteria? 11. Listeria monocytogenes is an intracellular pathogen that is capable of multiplying inside resting macrophages. How does Listeria avoid the phagolysosomal killing mechanism of this phagocytic cell? 12. In the study conducted by Bielecki et al., the hlyA gene of L. monocytogenes that encodes listeriolysin O was mutated. Describe how this gene was mutated, the resulting 2 phenotypes that were looked at following mutation, and the conclusions based upon these data. 13. Listeriolysin O is a member of a family that contains several other cholesteroldependent cytolysins secreted by gram positive pathogens. However, Listeriolysin O is the only one that functions within the vacuole whereas these other cytolysins function extracellularly. Name 2 properties of Listeriolysin O that are different from the properties of these other cytolysins and how is this important to successful Listeria pathogenesis? 14. Kocks et al. compared macrophage infection using wild type Listeria, Listeria with a transposon mutation of the hlyA gene, wild type Bacillus subtilis, and a B. subtilis strain transformed with the Listeria hlyA gene. What parameters did they address in this study and what were the conclusions drawn from the data? 15. What do Listeria monocytogenes and Shigella flexneri have in common with regard to their pathogenic strategies? 16. Theriot et al. used a phalloidin-rhodamine conjugate to observe intracellular Listeria monocytogenes. What does the phalloidin-rhodamine conjugate bind to, what was the observation made in this study, and what was the conclusion drawn from the data? 17. Theriot et al. used caged-resorufin bound to G-actin which was micro-injected into potoroo kidney epithelial cells to investigate actin filament dynamics within the actin tail formed by Listeria moncytogenes during infection of these cells. How was caged-resorufin used in their study and what observation was made? 18. In Listeria monocytogenes, actin polymerization mediated by the gene product ActA has been shown to be polar resulting in unidirectional movement. Design an experiment to show that actin polymerization is polar because ActA is polar. 19. How did Smith and Portnoy use the Streptococcus pneumoniae protein LytA, and living S. pneumoniae to demonstrate that polarized localization of ActA was sufficient for unidirectional movement? 20. What is the primary symptom that gave bubonic plague the name ‘Black Death’? 21. Listeria produces a toxin called listeriolysin O (LLO). LLO is a UNIQUE member of a family of pore-forming toxins called cholesterol dependent cytolysins (CDC’s). Another CDC, streptolysin O (SLO), is produced by Streptococcal species. In an experiment using Yersinia, it was determined that YopB and YopD produce SMALL pores in the plasma membranes of target-cells in the specific instance when Yop effectors are deleted. The size of the pores was determined to be small by showing that a small dye (Lucifer yellow) could enter cells while a larger dye (Texas red phalloidin) could not. As a control, researchers used SLO to show that Texas red phalloidin could enter cells. What property of LLO would make this toxin a pore choice to replace SLO in this experiment. 22. What does the “low calcium response” in Yersinia refer to? 23. The proteins involved in interaction between Y. pseudotuberculosis and Y. entercolitica with host cells were analyzed using an invasion assay. a. What is the invasion assay? b. What types of host and bacterial cells were used and why? c. What does the result of the assay tell you about the host proteins that interact with the bacterial cells? d. From this assay, they found four proteins important in adherence. What would have been the results if Y. pestis was used in the initial assay? 24. What are three traits that Y. pestis satisfies to classify it as a Category A biological weapon by the National Institute of Health (NIH)? 25. Two Yersinia adhesins, inv and ail, were identified using a similar assay. Which of the Molecular Koch’s Postulates were used to identify these adhesins? (no numbers – fully state the postulate) Are these adhesins important for Y. pestis virulence? Why? 26. What is the primary purpose of the type III secretion system in Yersinia? What host cell types are targeted by the Yop/Ysc/Lcr type III secretion system? How would you identify effectors? 27. What conditions are required for Y. pestis Type III secretion in vitro? 28. Bordetella pertussis is the human adapted pathogen that causes the disease known a “whooping cough”. B. pertussis is a non-invasive, extracellular pathogen that colonizes the upper respiratory tract (URT) during pathogenesis. a. Name 2 innate immune mechanisms that B. pertussis must evade in order to successfully colonize the URT. b. Name 2 secreted products expressed by B. pertussis during URT colonization that knockout the above 2 innate immune mechanisms that you listed. 29. B. pertussis infection is viewed as a two stage pathogenesis process involving first colonization of the URT and second toxin mediated tissue damage. Name two virulence factors that are expressed by B. pertussis that are responsible for toxin mediated tissue damage. 30. BvgAS, the virulence gene regulation locus of pathogenic Bordetella, is a 2 component sensory transduction system. How was BvgAS implicated in phase variation that occurs with Bordetella pertussis with respect to the virulence phenotype? 31. In a study designed to determine whether BvgAS of B. pertussis is responsible for phenotypic modulation of virulence, Miller et al. designed an experimental approach to find mutants that were insensitive to environmental modulators of BvgAS. a. In the genetic construct generated for the above goal by Miller (strain VIR102 of B. pertussis), why was the pertussis encoding toxin gene fused with the gene encoding chloramphenicol acetyltransferase that confers resistance to the antibiotic chloramphenicol? b. Why was hemolytic activity also assayed along with chloramphenicol resistance? c. Why in the genetic construct that they generated (VIR102) did they delete the wild type BvgAS from the chomosome and then integrate back into the chromosome a plasmid vector containing wild type BvgAS? How did this allow them to prove that BvgAS mediates phenotypic modulation? 32. The apparent function of BvgAS in Bordetella pathogens is to determine if Bordetella is within or outside a mammalian host. The Bvg minus phase in B. bronchiseptica results in the expression of several products required for survival of B. bronchiseptica when it is free living in the environment. What is the function of the Bvg minus phase products expressed by B. pertussis? 33. During B. bronchiseptica infection of rabbits, serum from the infected rabbits have antibodies against FHA, fimbriae, adenylcyclase, but not flagella. What conclusion can you draw from this finding with respect to BvgAS? 34. In the “skinny pig” (the ugly hairless guinea pig) aerosol transmission model it was found that B. bronchiseptica having a wild type BvgAS locus, but not those having a Bvgc (constitutive Bvg+ phase) locus were transmission competent. Given that Bvgc is as virulent as wild type, and Bvg- is avirulent, what conclusions were drawn from this observation?