SSN SBPM WORKSHOP #5 Short Answer Questions & Answers 1
advertisement

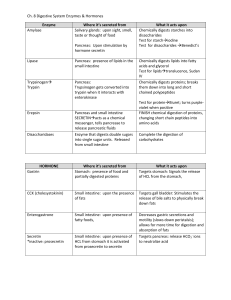
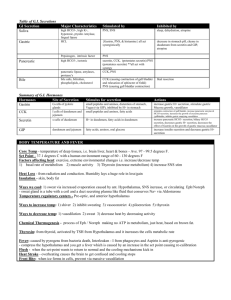
SSN SBPM WORKSHOP #5 Short Answer Questions & Answers 1. What happens in the parietal cells when a person who has fasted begins to eat? After a couple minutes, there is activation of the Hydrogen, potassium ATPase, carbonic anhydrase, and an increase in the production of ATP. 2. Acidification of the duodenal mucosa results in: The main response to acidic fluid in the duodenum is the stimulation of secretin, which stimulates the aqueous component of the pancreas (HC03). It also stimulates pepsinogen secretion as well as release of gastrin. There is some release of CCK which stimulates bile production and contributes to the inhibition of gastric emptying. 3. In the total absence of parietal cells, what would happen to a person? The parietal cells secrete both H+ and intrinsic factor, which is required for the reabsorption of vitamin B12. Without them, there is an elevated level of gastrin, since the normal feedback inhibition of gastric acid secretion has been interrupted. Even though the acidification helps in the digestion of proteins, it is not essential and the proteases within the small intestine will compensate. 4. What metabolic changes would you find in a patient with severe diarrhea? Since diarrheal discharge contains large amounts of HCO3, Na, and K, the patient loses a significant amount of fluid, causing a depletion of the extracellular volume that leads to a decrease in circulatory pressure. The loss of fluid will cause activation of the volume receptors, which leads to an increase in heart rate and activation of the sympathetic nervous system. The loss of potassium causes the patient to become hypokalemic (low potassium). The loss of alkalotic fluid, will lead to metabolic acidosis leading to compensatory hyperventilation to lower the H+ in the blood. 5. Do all seretonin antagonists have the same effect on the GI tract? Why or why not? No they do not. There are a number of different types of 5-HT receptors,and various drugs are selective for one or another type of receptor. Forexample, a 5-HT3 blocker alone will not inhibit the peristaltic reflexes;but this can be accomplished by blocking both 5-HT3 and 5-HT3 receptors simultaneously. The other seretonin receptor involved in GI response is5-HT1P. 6. Describe the process of signal transduction that results in the initiationof the peristaltic reflex. EC cells, the primary sensory cells of the gut, respond to increased pressure or chemical stimulation in the gut lumen by secreting 5HT, aneurotransmitter. 5HT is picked up by submucosal IPAN which are cholinergicneurons with CGRP activity. ACh and CGRP are responsible for fast and slow EPSPs, respectively, in the subsequent neuron. Submucosal IPANs activatethe enteric microsircuits that result in peristaltic and secretory reflexes. 7. How is the existence of receptor subtypes taken advantage of in medications? Mention 5-HT3 and 5-HT4 receptors, specifically. 5-HT receptor antagonists that are specific for 5-HT3 are used to stopsensations of nausea and vomiting from reaching the CNS without affectingperistalsis or secretions because 5-HT3 receptors are not involved ininitiating peristalsis or secretion. Also, 5HT4 receptor agonists are usedto increase peristalsis without causing nausea because there are no 5-HT4 receptors on extrinsic sensory neurons of the gut. 8. A 15 year old diabetic girl is non-compliant with her insulin injections and loves to splurge on sweets. At lunch time she eats a half pound of pure sugar. Which gastro-intestinal hormone will be affected and what effect, if any, will this have on her blood sugar? How would this compare to a normal person's physiology after eating this much sugar? GIP, the only GI hormone released in response to dietary carbs, will be released into the circulation but insulin secretion will not follow. Normally, the secretion of GIP results in the secretion of insulin by the pancreas, lowering blood glucose. In the type I diabetic, however, the beta cells of the pancreas are non-functional or absent. So, elevated blood sugar levels are unopposed by the pancreas (or by the effects of GIP on the pancreas). 9. In a normal individual, how would peak glucose levels differ after injection of glucose compared to drinking soda pop (assuming only glucose in the pop and equal grams of carbs)? The blood glucose curve for injected glucose will be steeper and have a higher peak because it hasn't been processed by the gut (so no GIP secretion occurs). Another reason, although not directly relevant to GI phsyiology, is simply that injection is a faster mode of administration. 10. Describe swallowing: Swallowing is a reflex response that is triggered by afferent impulses in the trigeminal, glossopharyngeal, and vagus nerves; these impulses are then integrated in the nucleus tractus solitarius and nucleus ambiguus. Efferent fibers pass to the tongue and pharyngeal musculature via the trigeminal, facial, and hypoglossal nerves. 11. What can cause a decrease in gastric motility by way of the enterogastric reflex? -products of protein digestion and H+ ions bathing the duodenal mucosa -distension of the duodenum -peptide YY -severing the vagus -fear? 12. CCK exhibits some overlap of function with secretin. How do these GI hormones interact and what might be the purpose of this interaction? The main purposes of CCK are to stimulate the gall bladder to contract, to stimulate the pancreas to secrete its digestive enzymes (trypsin, chymotrypsin, carboxypeptidase, amylase, lipase, etc.), and to stop the stomach from emptying, enabling the small intestine to properly deal with the fats and proteins that are already in its lumen. However, it also potentiates the effect of secretin on inducing bicarbonate secretion by the pancreatic extralobular ductal cells. This synergy between CCK and secretin makes sense because the enzymes that CCK causes to be released require an alkaline environment for their optimal activity. 13. The exocrine pancreas secretes a fluid that is isotonic with plasma. The concentration of bicarbonate in the pancreatic juice, however, is much higher than it is in the plasma. Explain the cellular mechanism in the pancreatic ductal cells responsible for both the increased bicarbonate and the maintenance of isotonicity. The pancreatic ductal cell contains both luminal and basolateral exchangers that allow it to increase the bicarbonate concentration in the pancreatic secretions. On the apical (luminal) surface is a Cl-/HCO3- exchanger that secretes one bicarbonate ion into the lumen for every Cl- ion it brings into the cell (this is thus a non-electrogenic exchanger). On the opposite, basolateral, surface, both H+-ATPase and Na+/H+ exchangers exist to secrete a proton out the other end of the cell, ensuring that acid does not build up inside the cell. There are also apical Cl- and basolateral K+ channels that function in maintaining osmotic balance. Remember, too, that the pancreatic ducts are permeable to water, allowing isotonicity to be maintained between pancreatic secretions and plasma. 14. Trace the fate of dietary triglycerides from ingestion through their storage in adipose tissue. Then trace the fate of triglycerides synthesized in the liver through their storage in adipose tissue. Fatty acids – triglycerides in chylomicrons (small intestine) – lacteals – lymphatic vessels – bloodstream – peripheral tissue capillaries w/ extracellular lipoprotein lipase (LPL) – free fatty acids (adipose tissue). Triglycerides (liver) – Very Low Density Lipoprotein (VLDL) in bloodstream – peripheral tissue capillaries w/ extracellular lipoprotein lipase (LPL) – free fatty acids (adipose tissue). 15 . What happens in reverse cholesterol transport? In short, cholesterol is removed from tissues. Circulating High density lipoprotein (HDL) probably extracts its cholesterol from cell surface membranes and converts it to cholesterol esters via the enzyme lecitin-cholsterol acyl transferase (LCAT). The cholesterol esters are then transferred to Low Density Lipoprotein (LDL) via cholesterol ester transfer protein (CETP). LDL is removed from the plasma by the liver, which excretes the cholesterol in bile. 16. What genetic and epidemiological evidence supports the idea that body weight is regulated? What is the proposed model for this regulation? In twin studies, comparing monozygous versus dizygous twins, the heritability of body fatness is found to be between 65 and 85%. Single gene mutations have been found that produce obesity. Long-term constancy of body weight, and the lack of success of people in maintaining lower body weight. The quantity of stored energy (in adipose) is sensed by afferent systems that feed into the central nervous system, whose efferents act on energy intake systems (feeding behavior) and output to return body weight to its usual level. 17. Why is it so difficult for an obese person to maintain a reduced weight? The body defends a particular weight. An obese person trying to maintain a weight below usual will require a significantly smaller number of calories than predicted solely on the basis of weight loss. Metabolic changes, such as an increase in skeletal muscle efficiency and a decrease in resting energy expenditure, act to oppose the maintenance of the altered weight. 18. What is the final mechanical event of sound transduction in the ear prior to the electrical conduction of sound? What is the series of events of electrical conduction? The movement of the hairs by the basilar membrane in the organ of corti is the final mechanical event, and is absolutely critical to sound transduction. Once the hairs are bent, energy is released in the form of ‘bioelectric potentials’ which leads to excitation of the auditory nerve fibers in the middle ear. These fibers are simply composed of one cytoplasmic process of a bipolar nerve cell. The other pole transmits the electrical impulses to the CNS (as you learned in anatomy) where sound is processed. This pathway proceeds through the cochlear nerve through the spiral ganglion to the brain. 19. Explain how the eye manipulates the lens to focus on near objects and why this ability is diminished with ‘normal’ aging. In order to focus on a near object, the lens must increase in both thickness and in curvature. When your brain decides to look at something close to your eye, the ciliary muscle is contracted, leading to tension on the ciliary body and suspensory ligaments which attach directly to the lens and change its shape. The major age-related change related to loss of near vision is presbyopia. As your parents put on their bifocals to read the map, remember that this is due to hardening of the lens over time, and thus a loss of flexibility, which leads to an inability to change lens shape to see near objects. Other age-related changes include yellowing of the sclera and senile cataracts, which are a result of focal opacities in the lens.