CLS 511 Medical Microbiology Unit 13 Fastidious Gram
advertisement

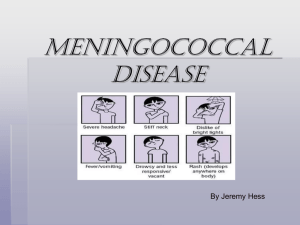
Fastidious gram-negative rods General Information Fastidious Gram-negative Rods Haemophilus, Bordetella, Legionella CLS 511 Medical Microbiology Karen Honeycutt, M.Ed, MT(ASCP)SM Fastidious gram-negative rods Haemophilus influenzae • Haemophilus means blood loving, requires nutrients in blood for growth • Normal flora of respiratory tract • Encapsulated strains – 6 antigen types (a-f) based on capsular polysaccharides – Type b causes most human disease – Systemic and life threatening diseases Haemophilus influenzae Clinical Significance • Respiratory tract infections – Usually determined as pathogenic by predominance or isolation of moderate to p many organisms from sputum culture assocatiated with PMN’s CLS 511 Medical Microbiology Unit 13 Fastidious Gram-negative rods • Gram stain = gram-negative coccobacilli (very small gram-negative rods) • Fastidious = require special nutrient/atmosphere/temperature conditions during specimen transport and for growth • Haemophilus sp., Bordetella sp. and Legionella sp. Haemophilus influenzae Clinical Significance • Respiratory tract infections (often secondary to viral infections) • Meningitis – Dramatic decrease (Hib vaccine) • Otitis media • Conjunctivitis (pinkeye) - contagious (H. influenzae biogroup aegypticus) Haemophilus influenzae Virulence factors • Capsule – most significant role – Most invasive infections caused by encapsulated p strains – antiphagocytic 1 Haemophilus influenzae Prevention – Hib Vaccine • Prevents most systemic disease • See for current vaccine guidelines http://www cdc gov/vaccines/vpd http://www.cdc.gov/vaccines/vpdvac/hib/default.htm#recs Haemophilus influenzae Laboratory Diagnosis Haemophilus influenzae Current treatment • Life threatening disease (meningitis) – Cefotaxime or ceftriaxone – Alternatives: trimethoprimsulfamethoxazole imipenem, sulfamethoxazole, imipenem ciprofloxacin • Non-life threatening disease – Amoxicillin-clavulanate, oral second or third generation cephalosporins or trimethoprimsulfamethoxazole Haemophilus influenzae Susceptibility Testing • Culture appropriate specimen – Organism will grow on chocolate agar, which is usually part of routine cultures where Haemophilus sp. sp is often recovered (respiratory, (respiratory csf, eye) • Direct specimen Gram stain = gram-negative coccobacilli (sometimes reported as gram-negative rods) • Growth within 24-48 hours Fastidious gram-negative rods Bordetella pertussis • Etiologic agent of pertussis • Only human-to-human transfer • Children <1 year of age at risk for most severe disease (nonvaccinated at greatest risk) • Infection initiated when infectious aerosols are inhaled • Bacteria attach and proliferate on ciliated epithelial cells CLS 511 Medical Microbiology Unit 13 Fastidious Gram-negative rods • Non-life threatening disease – Provide beta-lactmase test result • If positive = organism ampicillin/amoxacillin (R) • Life-threatening disease – Provide full susceptibility test results Bordetella pertussis Clinical Disease • 7-10 day incubation • 1-2 wks Catarrhal stage: common cold, very infectious • 2-4 wks Paroxysmal state: repetitive cough, inspiratory whoops, vomiting • 3-4 wks Convalescence/secondary complications 2 Bordetella pertussis Laboratory Diagnosis • Direct specimen detection (results within 2-24 hours) – Antigen testing: Direct fluorescent antibody testing - organism detected directly in specimen • Organism does not need to remain viable for accurate test results Positive fluorescing bacilli in nasopharyngeal specimen Bordetella pertussis Laboratory Diagnosis • Culture – specifically order B. pertussis culture – Best if specimen plated at bedside to appropriate agar (Regan (Regan-Lowe: Lowe: looks black due to charcoal) – Submit inoculated plate to lab immediately – Organism must remain viable – Culture held for 7 days with growth visible at 34 days Bordetella pertussis Susceptibility Testing/Vaccine • No standardized methods available due to fastidious nature of organism • Drug of choice = macrolides (erythromycin, clarithromycin, l ith i azithromycin) ith i ) and d SXT • Prevention: DTaP vaccine (pertussis, diphtheria, and tetanus) See CDC: http://www.cdc.gov/vaccines/vpdvac/pertussis/default.htm CLS 511 Medical Microbiology Unit 13 Fastidious Gram-negative rods Bordetella pertussis Laboratory Diagnosis • Direct specimen detection (results within 24 hours) – Nucleic acid detection (molecular methods) – Appears to be the most sensitive and specific test for B. pertussis – No universal FDA approved test available – Organism does not need to remain viable for accurate test results Bordetella pertussis Specimen of Choice for All Tests • Nasopharyngeal aspirate or swab – Ciliated epithelial cells need to be collected – Press the swab through the nares until resistance is met due to contact with the nasopharynx. – Rotate the swab gently and allow the swab to maintain contact with the nasopharynx for 2030 seconds or until coughing is induced. • A direct specimen technique is usually used in combination with culture Fastidious gram-negative rods Legionella sp. • Etiologic agent of – Pontiac Fever: self-limited, influenzaelike illness – Pneumonia: severe (death in 15% immunocompetent and up to 75% in immunocompromised) • Acquire: inhalation of organism from water source • Person-to-person spread not documented 3 Legionella sp. Legionnaires Disease • At risk: – >40 years-of-age or older – Compromised pulmonary function – Decreased cellular immunity (transplant patients) – Nosocomial pathogen (hospital water system) Legionella sp. Legionnaires Disease - Prevention • Identification of environmental source • Hyperchlorinate water • Maintenance of elevated water temperatures • Immunosuppressed patients – Run water to flush out pipes prior to using (showers) Legionella sp. Laboratory Diagnosis - Culture • Specific Legionella culture must be ordered • BAL fluid inoculated to specific medium: buffered charcoal yeast extract agar Legionella sp. Legionnaires Disease • After 2-10 day incubation – Fever, chills w/pneumonia (multilobar) – Nonproductive, dry cough (sputum not produced) – Multiorgan disease (liver, kidney) Legionella sp. Laboratory Diagnosis • Specimen of choice: bronchial alveolar lavage (BAL) fluid – Sputum p is often not p produced • Direct specimen detection (none are very sensitive, should be paired with culture) – Direct fluorescent antibody – Nucleic acid detection (molecular testing) – Urine antigen detection: antigens of only L. pneumophila serogroup 1 shed in urine for up to 1 year Legionella sp. Susceptibility Testing • No standardized methods available due to fastidious nature of organism • Drugs of choice – macrolides lid (clarithromycin, ( l ith i azithromycin), ith i ) – fluoroquinolones (ciprofloxacin, levofloxacin) – Contains L-cysteine and iron salts required for organism growth • Organism growth detected at 3-5 days, cultured held for 10 days CLS 511 Medical Microbiology Unit 13 Fastidious Gram-negative rods 4 Fastidious gram-negative rods Overview • Most common gram-negative coccobacilli isolated = Haemophilus influenzae – Respiratory infections, conjunctivitis, otitis media – Meningitis (Hib vaccine decreasing incidence) • Bordetella pertussis: pertussis • Legionella sp. – Pontiac fever: self-limited, flu-like – Legionnaires pneumonia: multi-organ involvement, nosocomial pathogen for immunosuppressed CLS 511 Medical Microbiology Unit 13 Fastidious Gram-negative rods 5