Control of Microbial Growth I. Terminology
advertisement
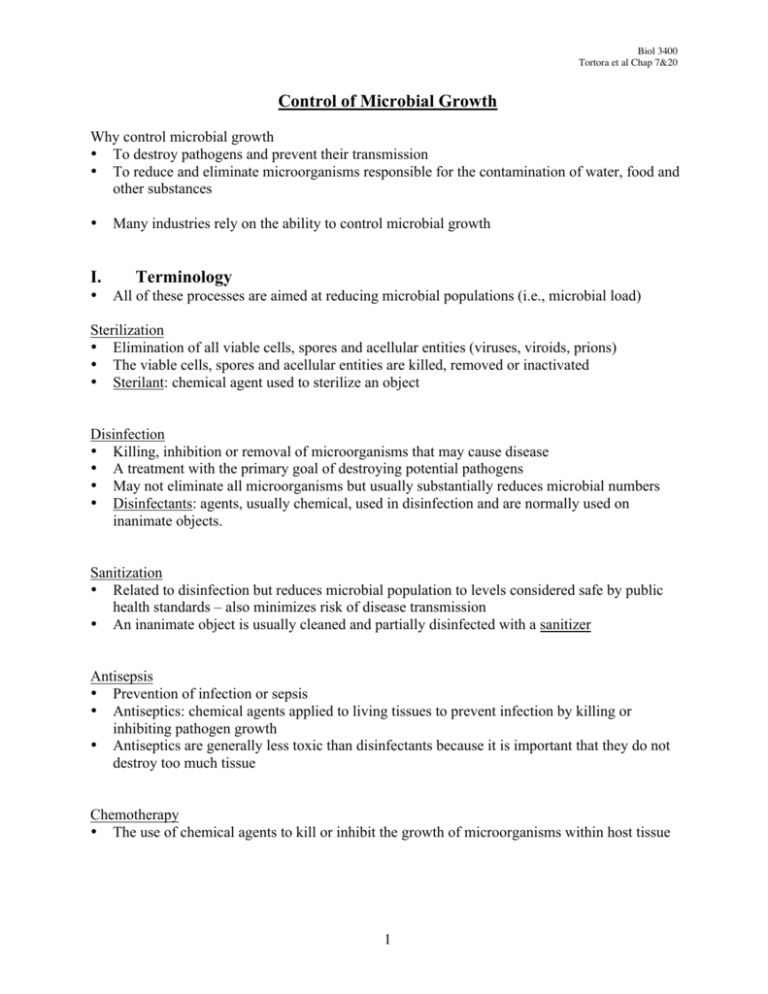
Biol 3400 Tortora et al Chap 7&20 Control of Microbial Growth Why control microbial growth • To destroy pathogens and prevent their transmission • To reduce and eliminate microorganisms responsible for the contamination of water, food and other substances • I. • Many industries rely on the ability to control microbial growth Terminology All of these processes are aimed at reducing microbial populations (i.e., microbial load) Sterilization • Elimination of all viable cells, spores and acellular entities (viruses, viroids, prions) • The viable cells, spores and acellular entities are killed, removed or inactivated • Sterilant: chemical agent used to sterilize an object Disinfection • Killing, inhibition or removal of microorganisms that may cause disease • A treatment with the primary goal of destroying potential pathogens • May not eliminate all microorganisms but usually substantially reduces microbial numbers • Disinfectants: agents, usually chemical, used in disinfection and are normally used on inanimate objects. Sanitization • Related to disinfection but reduces microbial population to levels considered safe by public health standards – also minimizes risk of disease transmission • An inanimate object is usually cleaned and partially disinfected with a sanitizer Antisepsis • Prevention of infection or sepsis • Antiseptics: chemical agents applied to living tissues to prevent infection by killing or inhibiting pathogen growth • Antiseptics are generally less toxic than disinfectants because it is important that they do not destroy too much tissue Chemotherapy • The use of chemical agents to kill or inhibit the growth of microorganisms within host tissue 1 Biol 3400 Tortora et al Chap 7&20 A variety of chemicals can be used to eliminate or reduce the numbers of microbes – these are often referred collectively as antimicrobial agents. Specific suffixes are used to indicate how these agents work. Bactericidal - "cidal" - to kill Bacteriostatic - "static" - to inhibit; if the agents are removed then growth will resume. Bacteriolytic – “lytic” – to lyse suffixes can be applied to all types of agents e.g., II. germicide, fungicide, algicide, viricide fungistatic The Pattern of Microbial Death Analogous to population growth, population death is an exponential process: plotting the log (population) vs time will produce a straight-line plot (Figure 7.1) There is a dilemma associated with determining when a microbe is dead (i.e., VBNC and viruses) It is important to assess the effectiveness of various treatments (i.e., quality control). A variety of methods exist, some of which are described below or later on in these notes • • • 1. Direct Assessment i) Bacterial killing curves • Plot log %survival vs a measure of the sterilizing agent e.g., log % viable Salmonella cells vs [singlet oxygen] ii) Time-dose-rate relationship • The effect of the treatment depends both on concentration used and exposure time. • In order to kill all the cells in a particular culture, one can hold the time constant and vary the dose or keep the dose constant and vary the time. e.g., A high dose for a short time will have the same effect as a low dose for a longer period of time iii) Death point • Treatment dose necessary to sterilize the system in a given amount of time e.g., Thermal death point = temperature necessary to sterilize a culture in 10 min. iv) Death time • Time necessary to sterilize a system with a particular treatment e.g., Time in min. necessary to sterilize the culture when a particular temperature is applied (Thermal death time) 2 Biol 3400 Tortora et al Chap 7&20 v) Decimal reduction time (D value) (Fig 7.1) • Exposure time at a given temperature needed to reduce the number of viable microbes by 90% (1 log). • Most precise way to characterize heat sterilization • Plot of log (number of viable cells) vs. time of heating (min) • Death rate increases with increasing temperature • z value in the change in temperature required to reduce the D value to 1/10 of its value 2. Indirect Assessment i) Sterility indicators • Use certain bacterial endospores • The most durable life forms known. e.g., Geobacillus stearothermophilus spores are capable of surviving 5 min in an autoclave (121°C; 15 psi) III Conditions Influencing the Effectiveness of Antimicrobial Agents The efficacy of antimicrobial agents is affected by at least 6 factors 1. Population size – larger populations require a longer time to die 2. Microbial characteristics – endospores are more resistant than vegetative cells to antimicrobial agents; there are also differences in susceptibility between species (Figure 7.11) 3. Concentration or intensity of an antimicrobial agent, e.g. 70% ethanol is more effective than 95% ethanol – killing activity is enhanced by water 4. Duration of exposure – the longer a population is exposed to a antimicrobial agent, the more microbes are killed 5. Temperature – higher temperature generally enhance the activity of an antimicrobial agent 6. Local environment – The local environment may enhance or diminish the activity of an antimicrobial agent (e.g., heat is more effective at an acidic pH; organic matter can protect cells from heat treatments and chemical disinfectants IV. Actions of Microbial Control Agents Antimicrobial agents kill or inhibit growth of a microbe in several ways 1. Damage to the membrane lipids or proteins cause cellular leakage that has a significant impact on growth 2. Proteins are central to the functioning and structure of cells. Many antimicrobial agents target key enzymes, transport or structural proteins. Agents that affect protein conformation (i.e., disrupt disulfide bridges or hydrogen bonds) inactivate enzymes or transport proteins. 3. Other antimicrobial compounds damage nucleic acids thereby preventing a cell from replicating or carrying out normal metabolic functions such as enzyme synthesis. 3 Biol 3400 Tortora et al Chap 7&20 V. Physical Methods of Controlling Microbial Growth Note: Each method has it limitations, advantages and disadvantages 1. Heat • All microbes have a maximum and a minimum temperature for growth • Almost all macromolecules lose their structure (i.e., denature) and ability to function at very high temperatures • Moist or dry heat is used. Moist heat is more effective than dry heat because • It penetrates cellular structures better • It facilitates unfolding of proteins, degrading DNA and disrupting membranes • It causes hydrogen bond rearrangement Dry heat is basically an oxidative process that • denatures proteins and DNA • disrupts membranes The choice of heat treatment and temperature depends upon material being treated. • Too high a temperature may destroy a food product or render a medium useless. • Wet heat may cause metal instruments to rust • The presence of certain compounds (e.g., protein, sugars and fats) may increase the resistance of cells to heat e.g., Microbial death is more rapid at acidic pH High concentrations of sugars, proteins and fats decrease heat penetration Dry cells and endospores are more resistant than wet cells a. Autoclaving (Fig 7.2) • Exposure of materials to 121°C at 15 psi (1.1 kg/cm2) produces high temperature steam necessary to kill endospores • This processes sterilizes materials • Duration depends on size and bulk of object – heat must be transferred to interior b. Canning • Uses heat under pressure to sterilize and hermetic sealing to drive out oxygen c. Pasteurization • used to kill harmful organisms in food or beverages and to prevent spoilage. • This process does not sterilize; sterilization would destroy desirable properties of many foods and beverages Two pasteurization processes that achieve the same results (more or less) o Low temperature - hold (LTH, also known as bulk pasteurization) - 62.8°C for 30 min 4 Biol 3400 Tortora et al Chap 7&20 o High temperature - short time (HTST, also known as flash pasteurization) 71.7°C for 15s. This method is preferable for milk because it alters the taste less, kills heat resistant microbes more effectively and can be done on a continuous flow bases d. Ultra High Temperature sterilization (UHT) • Sterilizes food and other products • 141°C for 4 - 15 s; allows for a continuous flow system e. • • • 2 • • Dry Heat often requires much higher temperatures and longer exposure times (e.g., 170°C for 2 h) Extreme temperature may damage materials that can resist lower temperature (121°C) Other examples include the flaming of an inoculating loop and incineration of combustible materials Low Temperature Refrigeration (0 to 7°C) and freezing Does not kill all microbes but inhibits growth 3. Radiation • Forms of electromagnetic radiation i) Microwaves • works partially due to heating ii) Ultraviolet radiation • 220 to 300 nm in wavelength • This radiation is energetic enough to cause modifications or strand breaks in DNA that may result in disruption of genetic material and death of the organism • low energy, low penetrating power - surface treatment iii) Ionizing radiation • high energy, high penetrating power that produces electrons, hydoxyl radicals, and hydride radicals → breaks hydrogen bonds, oxidizes double bonds, destroys ring structures, degrade and alter biopolymers • Standard for biological applications is absorbed radiation dose measured as Rad = 100 erg/g (where 1 joule = 10,000,000 erg) Gray (Gy) = 100 rad • A dose providing a 10 fold reduction in numbers is referred to as a D10. A standard killing dose is 12 D10 equivalents • Sensitivity to radiation differs for different microbes Application of radiation • 60Co and 137Cs sources • medical supplies and food industry (spices and fresh meat) 5 Biol 3400 Tortora et al Chap 7&20 4. Filtration • Applicable to liquids and gases • Remove microbes - does not kill them • Types include depth, membrane and nucleopore (Fig 7.4) e.g., Biocontrol hoods & laminar flow hoods - High efficiency particulate air (HEPA) filters are a type of depth filter – remove 99.97% of 0.3µm particles 5. Desiccation • Removal of water - microbes can't grow • Dried fruit, meat and fish • lyophilization - freeze dried food VI. Chemical Methods of Controlling Microbial Growth Classes of Antimicrobial Agents A. Inhibition of microbial growth on inanimate objects or on the exterior of animate objects i. Sterilants • A sterilant destroys all forms of microbial life including endospores • “cold sterilization” often needed for sterilizing and decontaminating heat sensitive materials e.g., ethylene oxide, formaldehyde, H2O2, sodium chlorite (bleach) ii. Disinfectants • kill or inhibit growth of microbes but not necessarily endospores. e.g., ethanol, cationic detergents, chlorine, phenol iii. Sanitizers • A disinfectant that is used to reduce numbers of bacteria to levels judged to be safe by public health officials. iv. Antiseptics • Agents that kill or prevent growth of microbes on living tissues e.g., Alcohol, phenol, iodine, crystal violet Alcohol - dehydrates and denatures proteins and disrupts membranes. Alcohol works best when slightly diluted (70 to 90%). If alcohol is used full strength, then it dehydrates cells before proteins can be denatured. v. Preservatives • agents that prevent microbial growth in foods and other products. e.g., organic acids (propionic acid, lactic acid, citric acid, sorbic acid), NO3-, NO2-, NaCl 6 Biol 3400 Tortora et al Chap 7&20 Assessment of Disinfectant Efficacy 1. Phenol coefficient test – a standard amount of test organisms (Salmonella typhi and Staphyloccous aureus) are added to a dilution series of i) the disinfectant of interest and ii) phenol. The dilutions are placed in a water bath at 20 or 37°C. Samples are withdrawn at 5 minute intervals and inoculated into growth medium. The inoculated medium is incubated for two or more days. The highest dilution that kills the bacteria after a 10 minute exposure, but not after 5 minutes, is used to calculate the phenol coefficient. • Phenol coefficient = reciprocal for the appropriate dilution of the disinfectant being tested reciprocal for the appropriate dilution of phenol • A value > 1 means the disinfectant is more effective than phenol 2. Use-dilution test – cylinders of metal or glass are dipped in standardized cultures of the test organism, removed and allowed to dry. The dried cultures are placed in a solution of the disinfectant and left for 10 minutes at 20°C. The cylinder is then transferred to a suitable growth medium and monitored for growth. 3. Disk diffusion method (Agar-diffusion method) – See below for details B. Inhibition of microbial growth in vivo Chemotherapeutic Agents • Chemical compounds that can be used internally for control of microbes • Synthetic agents and Antibiotics = Antimicrobial agents An antibiotic is a chemotherapeutic compound produced by microorganisms. To be useful in therapy, a chemotherapeutic agent must have selective toxicity e.g., high toxicity towards the microbe but low toxicity towards the host. Selection of Chemotherapeutic Agents • Sensitivities of target microorganism • Side effects of antibiotic • Longevity of antibiotic (e.g., biotransformations) • Chemical properties of antibiotic- affect targeting of antibiotic in the body • Selectivity - broad spectrum vs narrow spectrum of activity (Table 20.2) 7 Biol 3400 Tortora et al Chap 7&20 Assessment of Chemotherapeutic Agent Efficacy i) Agar Diffusion Method (Kirby-Bauer test) • designed for assessing the effectiveness of antibiotics - sensitivity of microbes • Lawn of bacterium in question & disks impregnated with antimicrobial agent • measure clear zone - zone of inhibition • Standardized zone sizes are a measure of sensitivity for chemotherapeutic agents S- susceptible (Ampicillin - 14 mm or more) R - resistant (Ampicillin - 11 mm or less) I - Intermediately sensitive (Ampicillin - 12-13 mm) • • • • Size of zone depends on a number of factors including amount of antimicrobial agent added to the disc, solubility, and effectiveness of agent Conclusion - whether an antimicrobial agent has the potential to control a particular microorganism This test is limited to use with rapidly growing bacteria It is a standardized test not designed for assessing the effectiveness of antibiotics against filamentous fungi, anaerobes or slow growing bacteria, although it is possible to modify test in order to assess these organisms. ii) Minimum Inhibitory Concentration (MIC, also known as tube dilution technique) • Dilutions of antibiotics or other chemical agents are tested for ability to inhibit growth of a microbe in liquid culture • MIC is the lowest concentration of an agent that completely inhibits the growth of the test organism • Determines the minimum amount of antimicrobial agent that must be present at the site of infection to inhibit growth of the pathogen. • Affected by the nature of the test organism, inoculum size, medium composition and other growth parameters (incubation time, temperature, pH, aeration…) • aids in selection of antibiotic and dosage (required to know how antibiotic distributes). Physicians generally add in a safety margin - 10 times MIC • Medium from tubes that do not show growth (i.e., have higher antimicrobial concentration than the MIC) can be used to inoculate broth or on agar plates free of the antimicrobial agent. If growth occurs then the drug was not bactericidal and the minimum bactericidal concentration (MBC) can be determined. VII. A look at chemotherapeutic agents and their mode of action Antimicrobial agents can be categorized based on a number of key characteristics including • Source (synthetic or natural products) • Mode of action (Fig 20.2) • Target microorganism • Chemical structure 8 Biol 3400 Tortora et al Chap 7&20 A. Synthetic antimicrobial agents 1. Growth factor analogs – structural similarity to growth factors Examples, - Sulfa drugs – sulfonamide – analog of p-aminobenzoic acid (part of folic acid). Treatment with sulfamethaxazole/trimethoprim results in sequential blocking of the folic acid biosynthetic pathway (Fig 20.13). Resistance requires a double mutation in the same microorganism - Isoniazid – inhibits mycolic acid synthesis – The genus Mycobacterium has a cell wall different from other bacteria. It contains mycolic acid that influences the staining properties of mycobacteria. A number of important pathogens are found in this genus, including those that cause tuberculosis (Mycobacterium tuberculosis) and leprosy (Mycobacterium leprae). - Nucleic acid analogs – often substituted with fluorine or bromine 2. Quinolones • Not growth factor analogs - interact with DNA gyrase and topoisomerase II (involved in DNA replication – packaging DNA) • Effective against both gram-positive and gram-negative bacteria e.g., B. Nalidixic acid Fluoroquinolone derivatives – norfloxacin and ciprofloxacin are more soluble than Nalidixic acid Antibacterial Antibiotics 1) Cell Wall Inhibitors a) Prevent formation of peptide cross linkages by binding to transpeptidase. β-Lactams • Characterized by β-lactam ring • Transpeptidases are also known as penicillin binding proteins (PBP; FtsI) • Account for over half of the antibiotics produced and used worldwide Ineffective against • bacteria which lack peptidoglycan cell walls - Mycoplasmas • resting or dormant cells β-lactam rings (Figure 20.6) e.g., Penicillin - Penicillium chrysogenum Cephalosporin - Cephalosporium spp. 9 Biol 3400 Tortora et al Chap 7&20 b) Bind directly to peptide portion of peptidoglycan • block action of transpeptidase e.g., Vancomycin – a glycopeptide that is not transported across the outer membrane of many Gram negative cells 2) Protein Synthesis Inhibitors (Fig 20.4) Aminoglycosidses - amino sugars bonded by glycosidic linkages to other amino sugars • Streptomycin, Kanamycin, Neomycin – produced by members of the genus Streptomyces • Not effective against anaerobes or Gram positive bacteria • Bind to small subunit (30S) of the 70S ribosome – prevent protein chain initiation • Not widely used today Macrolides – multi-member lactone ring connected to sugar moieties (Fig 20.12) • erythromycin, tylosin - Streptomyces • act on the 50S ribosomal subunit - prevents peptide bond formation • >10% of world production Tetracyclines - four fused cyclic rings – naphthacene ring system (Fig 20.11) • Broad spectrum – Gram-positive and Gram negative bacteria • Bind to 30S subunit - block the A-site (aminoacyl site) – prevent protein elongation • produced by Streptomyces Chloramphenicol – simple structure makes this antibiotic inexpensive to synthesize (Fig 20.10) • inhibits formation of peptide bonds in the nascent polypeptide by reacting with the 50S subunit • Produced by Streptomyces Rifamycin • block protein synthesis at the transcriptional level - binds to RNA polymerase β-subunit • Best known example is rifampin 3). Membrane Function Inhibitors • Polymyxin - Bacillus polymyxa - changes membrane structure and causes leakage • Daptomycin – cyclic lipopeptide that binds to cell membrane and induces rapid depolarization of membrane potential 4). • • • DNA scission Phleomycin/bleomycin/zeocon Broad spectrum antibiotics that are affectcive against prokaryotes and eukaryotes Cleave DNA 10 Biol 3400 Tortora et al Chap 7&20 C. Antifungal Antimicrobial Agents • Problems associated with host toxicity 1) Ergesterol inhibitors • Polyene - affinity for membrane sterols such as ergesterol - disrupt membrane structure e.g., Nystatin, Amphotericin B (Fig 20.14) 2) Ergesterol synthesis inhibitors • Azoles (Fig 20.15) and allyamines • Inhibit ergesterol biosynthesis - alter membrane permeability e.g., Ketoconazole 3) Cell wall synthesis • Polyoxins - interfere with chitin biosynthesis • Echinocandins – interfere with 1,3 β-D glucan synthase – results in incomplete cell wall 4) Inhibit microtubule assembly • Griseofulvin is produced by Penicillium spp. • Prevents microtubule assembly, interfering with mitosis and thereby inhibiting fungal reproduction D. Antiviral Agents • Problems associated with host toxicity 1) Nucleoside/nucleotide analogs (Fig 20.16) • Acyclovir - Herpes simplex - blocks viral DNA replication • Zidovudine (nucleoside analog) and tenofovir (nucleotide analog) - blocks DNA production (reverse transcription) – effective against retroviruses (HIV) – RNA virus that converts 2) Non-nucleoside reverse transcriptase inhibitors • Bind directly to the reverse transcriptase and inhibit activity e.g., nevirapine 3) Protease inhibitors • HIV requires protease activity in the maturation process • Research has identified peptides that bind in the protease active site and inhibit protease activity • Atazanavir and indinavir and saquinavir are protease inhibitors of 4) RNA polymerase inhibitors e.g., Rifamycin 5) Neuraminidase inhibitors • Neuraminidase is an enzyme on viral surface that is important in releasing virions from host cell e.g., Tamiflu (oseltamivir) – inhibitor of influenza neuraminidase 11 Biol 3400 Tortora et al Chap 7&20 6) Interferon – low molecular weight proteins • prevent viral replication by stimulating the production of antiviral proteins that prevent further viral infection • no clinical use because interferon must be present in relatively high local concentrations VIII. Antibiotic Resistance • 1. Antibiotic producers must protect themselves from the antibiotics that they produce Mechanisms of Antibiotic resistance (Figure 20.20) • The organism lacks the structure that antibiotic acts upon • Impermeable to antibiotic • Decreased transport - β-lactams • Active secretion - Efflux pump - pumps out antibiotic - Tetracycline resistance • Production of modifying enzymes hydrolytic enzymes - β-lactamase addition of chemical groups - acetylation or phosphorylation of macrolides • Modification of site of antimicrobial action - ribosomal modification - streptomycin rpsL • Production of alternate molecules that can replace those disrupted by antibiotics 2. Genetic Basis of Antibiotic Resistance • Antibiotic resistance is coded at the chromosomal or the plasmid level (R-plasmids) • Resistance at the chromosomal level almost always arises due to modification of the target of the antibiotic • Plasmid resistance often results from the production of enzymes that inactivate, prevent uptake or actively pump out the antibiotic 12 Biol 3400 Tortora et al Chap 7&20 3. Spread of antibiotic resistance Overuse and improper use of antibiotics • Treatment of disease • Intensive Livestock production How did antibiotic resistant bacteria come about? Sources of Genetic Variation Mutation high growth rates - production of large populations -7 -9 spontaneous mutation 10 to 10 /generation Recombination • transformation • transduction • conjugation Transfer of antibiotic resistance determinants via • R-plasmids • Transposons • Integrons 13