MRSA Care Plan
advertisement
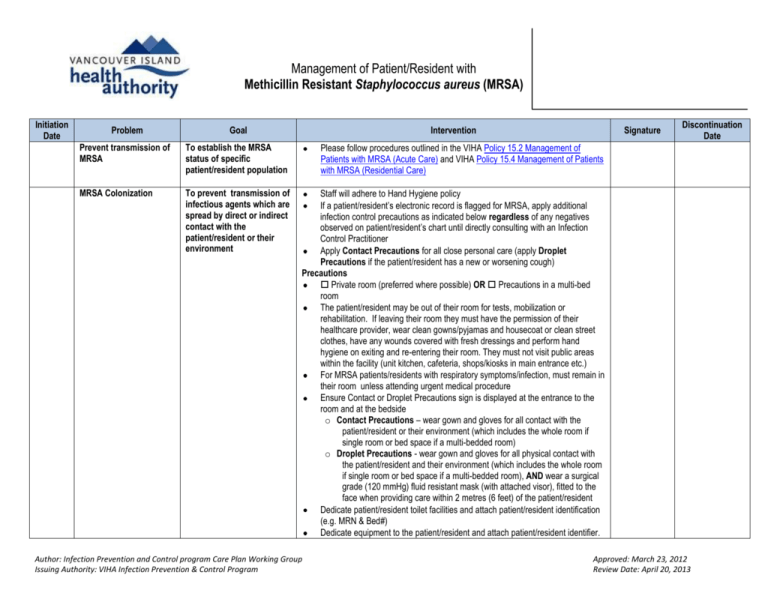
Management of Patient/Resident with Methicillin Resistant Staphylococcus aureus (MRSA) Initiation Date Problem Goal Intervention Prevent transmission of MRSA To establish the MRSA status of specific patient/resident population Please follow procedures outlined in the VIHA Policy 15.2 Management of Patients with MRSA (Acute Care) and VIHA Policy 15.4 Management of Patients with MRSA (Residential Care) MRSA Colonization To prevent transmission of infectious agents which are spread by direct or indirect contact with the patient/resident or their environment Staff will adhere to Hand Hygiene policy If a patient/resident’s electronic record is flagged for MRSA, apply additional infection control precautions as indicated below regardless of any negatives observed on patient/resident’s chart until directly consulting with an Infection Control Practitioner Apply Contact Precautions for all close personal care (apply Droplet Precautions if the patient/resident has a new or worsening cough) Precautions Private room (preferred where possible) OR Precautions in a multi-bed room The patient/resident may be out of their room for tests, mobilization or rehabilitation. If leaving their room they must have the permission of their healthcare provider, wear clean gowns/pyjamas and housecoat or clean street clothes, have any wounds covered with fresh dressings and perform hand hygiene on exiting and re-entering their room. They must not visit public areas within the facility (unit kitchen, cafeteria, shops/kiosks in main entrance etc.) For MRSA patients/residents with respiratory symptoms/infection, must remain in their room unless attending urgent medical procedure Ensure Contact or Droplet Precautions sign is displayed at the entrance to the room and at the bedside o Contact Precautions – wear gown and gloves for all contact with the patient/resident or their environment (which includes the whole room if single room or bed space if a multi-bedded room) o Droplet Precautions - wear gown and gloves for all physical contact with the patient/resident and their environment (which includes the whole room if single room or bed space if a multi-bedded room), AND wear a surgical grade (120 mmHg) fluid resistant mask (with attached visor), fitted to the face when providing care within 2 metres (6 feet) of the patient/resident Dedicate patient/resident toilet facilities and attach patient/resident identification (e.g. MRN & Bed#) Dedicate equipment to the patient/resident and attach patient/resident identifier. Author: Infection Prevention and Control program Care Plan Working Group Issuing Authority: VIHA Infection Prevention & Control Program Signature Discontinuation Date Approved: March 23, 2012 Review Date: April 20, 2013 Initiation Date Problem Goal Intervention Signature Discontinuation Date Equipment not dedicated must be thoroughly decontaminated before being removed from the patient/resident’s bed-space to be used by another patient/resident Linen, garbage and dishes are treated as routine Ensure patient/resident information leaflet: MRSA is given to patient/resident/visitors Housekeeping On discharge or transfer from the room, or discontinuation of precautions, notify housekeeping that a terminal clean must be completed Housekeeping shall remove Precaution sign on completion of terminal clean To prevent spread of MRSA and reduce the risk of transmission associated with out of room procedures or tests A diagnosis of MRSA must not delay or inhibit any procedure or test required for the care of the patient/resident (discuss with Infection Control Practitioner if the patient/resident has respiratory symptoms/infection) Identify additional precautions required on the test/procedure requisition form Notify the receiving department in advance of the type of additional precautions and cleaning required Notify transport staff of additional precautions required Encourage patient/resident with hand hygiene Hand washing is extremely important for staff, visitors and patients/residents, especially before meals and after using the toilet. Regular soap and water or alcohol based hand rub is recommended Teach patient/resident correct procedure to wash hands and when to perform hand hygiene Ensure patient/resident information leaflet: Hand Hygiene is given to patient/resident/visitors To prevent spread of MRSA and reduce the risk of transmission associated with visitors Provided visitors of patient/resident are healthy, there is no restriction on visiting Visitors must be directed to wash their hands with soap and water or use alcohol based hand rub on entering and leaving the patient/resident room Visitors must use gown and gloves in addition to hand washing only if they are providing close personal care. Guidance must be given by the Most Responsible Nurse Visitors will not be required to wear PPE for social visits (i.e. Saturday chat with the patient, etc) Visitors must not visit public areas within the facility (unit kitchen, cafeteria, shops/kiosks in main entrance etc.) and SHALL NOT use the patient/resident bathroom To decolonize the The decision to use decolonization therapy will be made in accordance with Author: Infection Prevention and Control program Care Plan Working Group Issuing Authority: VIHA Infection Prevention & Control Program Approved: March 23, 2012 Review Date: April 20, 2013 Initiation Date Problem MRSA Infection Goal Intervention patient/resident of MRSA VIHA’s Policy 15.2 - Management of Patient with MRSA in Acute Care and/or Policy 15.4 – Management of Patient with MRSA in Residential Care Decolonization therapy must be ordered by the Most Responsible Physician (MRP) Treatment and eradication of MRSA infection To assess the MRSA status of the patient/resident following treatment The Most Responsible Physician to coordinate treatment regime Signature Discontinuation Date Colonized: Wait 7 days following completion of any antibiotic treatment (topical, oral or injectable) or following decolonization therapy then take first set of swabs Two sets of swabs must be taken, 7 days apart If the first set of swabs are positive, wait 7 days before doing another set of swabs Infection: Wait 30 days post completion of any antibiotic treatment (topical, oral or injectable) then take first set of swabs Two sets of swabs must be taken, 7 days apart If the first set of swabs are positive, wait 7 days before doing another set of swabs Date of antibiotics and treatments discontinued: _____________________________ Dates of cultures (at least 7 days apart; must include nares, groin and other sites previously positive) Discontinuation of precautions #1_________________ Nares MRSA positive MRSA negative Groins MRSA positive MRSA negative Other site MRSA positive MRSA negative #2_________________ Nares MRSA positive MRSA negative Groins MRSA positive MRSA negative Other site MRSA positive MRSA negative To discontinue precautions at the appropriate time Author: Infection Prevention and Control program Care Plan Working Group Issuing Authority: VIHA Infection Prevention & Control Program Please refer to Table 10: Procedure for Discontinuing Additional Precautions in the Infection Prevention and Control Manual and discuss potential removal of ARO flag with Infection Control Practitioner Most Responsible Nurse notifies Housekeeping a clean is required according to Approved: March 23, 2012 Review Date: April 20, 2013 Initiation Date Problem Goal Intervention Signature Discontinuation Date current VIHA Guidelines If precautions are discontinued prior to patient/resident discharge, ensure: o Patient/resident is helped into a clean gown/pyjamas and housecoat o Hand hygiene is performed and the patient/resident brought out of room o The bedspace/room has a terminal clean o If possible, the patient/resident is showered or bathed and clean gown/pyjamas and housecoat is donned and the bathroom is terminally cleaned o Patient/resident is helped into a clean gown/pyjamas and housecoat Once bedspace/room has been cleaned by housekeeping in a timely manner, precautions can be formally discontinued, sign will be removed from entrance to room and at bedside by housekeeping and the patient/resident may return Discharge Planning Ensure discharge of the patient/resident is done in a manner to ensure the risk of transmission is reduced, and the receiving facility is fully aware of the patient/resident’s diagnosis May discharge home or transfer to another facility Must inform Infection Control Practitioner of any transfers/discharges Must inform receiving caregivers or receiving agency of additional precautions if required and course of treatment Must inform any transport services of additional precautions if required See also the Infection Prevention and Control Manual Author: Infection Prevention and Control program Care Plan Working Group Issuing Authority: VIHA Infection Prevention & Control Program Approved: March 23, 2012 Review Date: April 20, 2013