Dr Adrian Massey – Creating a link between good management and
advertisement

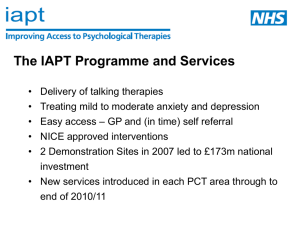
Doctors or Managers – Who has the solutions for workplace wellbeing? IOSH : Wellbeing – That Works! 23 September 2015 Dr Adrian Massey MRCP FFOM Doctors or Managers? Doctors or Managers? Doctors or Managers? Doctors or Managers? The temptation to medicalize life The dangers of medicalizing life Why it is becoming harder to hold the line The potential of people Summary The temptation to medicalize life Tempting to see health as a commodity we buy rather than something we do Perhaps this is because it is – • Easier to take a pill than take responsibility for lifestyle changes • Lack of health can then be politicised – it implies social/economic injustice rather than personal fallibility • Easier subject matter for a wellbeing conference! The temptation to medicalize life We are increasingly treating life as a medical problem - The dangers of medicalizing life Medicine can be dangerous! (pharmakon) Misdiagnosis, missed diagnosis, treatment errors and side-effects are inevitable because clinicians, as humans, are fallible When an illness is diagnosed where no illness exists, any level of treatment risk is unacceptable When life is made a medical problem there is an opportunity cost to society as enormous resources are directed to fashionable illnesses People like easy solutions that don’t require effort… People like easy solutions that don’t require effort… But these solutions can be dangerous…. People like easy solutions that don’t require effort… But these solutions can be dangerous…. …this puts an important social duty on doctors to curtail the aspirations of their franchise. The dangers of medicalizing life Examples – • A 19 year old lady attends her GP very distressed having found out her first long-term boyfriend has been having an affair. 7 minutes is allotted for the appointment. She is told she is depressed, prescribed citalopram and asked to come back in a month… • A 27 year old production manager has fallen out with his new area manager over time-sheets and has become tearful, anxious, has stopped sleeping and going out. His GP tells him he is depressed, prescribes citalopram (!), commiserates with him about his treatment at the hands of his employer, signs him off for 2 months and writes to the employer to say they must not contact his patient… The dangers of medicalizing life What kinds of medical harm arise in situations of this kind? Disempowerment Dependence Alienation Distraction from practical interventions to a circumstantial problem Side-effects of unnecessary treatment “The first duty of the physician is to educate the masses not to take medicine.” Sir William Osler (1849 – 1919) Why it is becoming harder to hold the line Medicalization facilitated in modern times by – Move from a disease model to an illness model Increasingly unrealistic expectations of human life IT and social networking (normalising irrational, unscientific beliefs) Democratization of opinion in modern times (the ‘Balance Fallacy’) Reduced deference to professionals (post-Shipman) These have undermined the physician in their socially important role of normalising rather than pathologizing the experiences of their patients Why it is becoming harder to hold the line That is not to say that medicine is never good But the study of interventions in illness models is necessarily less objective than for disease models and must be interpreted with scepticism Why it is becoming harder to hold the line That is not to say that medicine is never good But the study of interventions in illness models is necessarily less objective than for disease models and must be interpreted with scepticism This includes consideration of the vested interests of those offering to sell the ‘solution’! My butcher says – “Eat More Sausages!!” The potential of people The observable evidence is that as a species, throughout human history, we are very resilient When problems are presented in a human context people feel able to apply a wide range of human qualities – Practical Emotional Philosophical Religious/spiritual We should not underestimate the power of social/cultural factors as means of helping people to cope with, and make sense of, the existential challenges of their life The potential of people “Medicalisation constitutes a prolific bureaucratic programme based on the denial of each man’s need to deal with pain, sickness and death.” (Extract from ‘Limits to Medicine’, Ivan Illich) The potential of people Medical interventions have a declining marginal utility There is an opportunity cost to excessively medicalised wellbeing solutions Organisations have less time and less money for other activities that are actually more useful – Having time for one another Embodying a culture of interest and care rather than ‘outsourcing’ these Building mutually supportive teams and networks Improving the physical environment, pay & rations, social activities Investing in training to improve manager skills The potential of people What is ‘good’ management? The potential of people What is ‘good’ management? Why would you ask a doctor? The potential of people What is ‘good’ management? Why would you ask a doctor? ….perhaps because we are regularly spectators to the consequences of ‘bad’ management and may have some useful observations to make? Honesty Expectations for role, consequences of underperformance: the existence of a contract! Consistency Resisting the temptation to make promises that can’t be cashed Integrity Say what you mean and mean what you say Engagement Whether the employee’s expectations are realistic or not, you can’t hope to manage them if you don’t know what they are Demonstration of care Time, verbal/non-verbal communication, actions The potential of people There is no evidence that people who are vulnerable to mental health problems, or who have a mental health problem, need a fundamentally different kind of management to anyone else But they are less resilient to poorer management Summary There is little evidence of effectiveness for workplace medical interventions intended to reduce the risk of people developing MHPs It is intuitive that how well people fare in work depends heavily on the quality of their line manager interactions There are evidence-based medical treatments for people who have developed clinically-recognised MHPs Summary Managers should not under-estimate how important their own interactions with employees are as a means of helping them to keep well and helping them to recover if they have become unwell Well-meaning (or avaricious) doctors and HCPs should leave well people alone!